Abstract
Most surgeons believe that Asians have a low risk of developing venous thromboembolism (VTE) and routine thromboprophylaxis therapy is not required after major orthopaedic trauma. This study evaluates the postoperative risk of VTE in Indian patients sustaining pelvi-acetabular injury. Fifty-six patients with pelvi-acetabular injury, who underwent open reduction and internal fixation, were prospectively evaluated for VTE in the postoperative period. They were evaluated, both clinically and radiologically (pulmonary CT angiography and indirect venography of lower limb and pelvis veins), until six weeks after surgery. A total of 16 patients developed VTE, of which 12 had proximal deep vein thrombosis (DVT), ten had pulmonary embolism (PE) and only two had distal DVT. Six patients with proximal DVT had associated PE. The risk of development of VTE among Indian patients after pelvi-acetabular injury is high (28.6%) with increasing chances of proximal DVT and PE; hence, administration of routine thromboprophylaxis is fully justified in them.
Introduction
Venous thromboembolism (VTE) is a broad term that encompasses both deep vein thrombosis (DVT) in extremities/pelvic veins and pulmonary embolism (PE). Major orthopaedic trauma is a high risk factor for development of VTE. The reported incidence of DVT and PE in these patients varies from 30 to 80% and 0.5 to 2% depending on the type of injury, patient profile and diagnosis [8, 15, 23, 28]. However these studies are mainly based on western literature. The few studies available on Asian populations show a wide variation in the incidence of VTE (0–72%). While few studies on Asians patients undergoing high risk operations (total hip replacement, total knee replacement, hip fractures) report incidence of VTE equivalent to western literature (up to 62.5%), most studies report a very low incidence and advise against routine chemoprophylaxis in this population [1, 2, 4, 6, 20, 22, 29]. Some workers have shown that even established thrombi in Asian patients resolve spontaneously without any long-term consequences [13, 14]. Some recent studies report an increasing incidence of VTE in the Indian subcontinent [11, 16]. The increased incidence is attributed to increased life expectancy, changing lifestyle and better methods of diagnosis [16].
A study based on VTE risk associated with major trauma in Asian patients is lacking and most of the centres still do not provide routine thromboprophylaxis in these patients [35]. This prospective study evaluates the risk of VTE after pelvi-acetabular surgery in the Indian population.
Materials and methods
A two-year (from January 2008 to December 2009) prospective study was performed in our level I trauma centre to evaluate the risk of development of VTE in the postoperative period among Indian patients (<65 years) sustaining pelvi-acetabular injury. Patients with renal failure, allergies to dye, high risk candidates for VTE such as myocardial infarction, nephritic syndrome, hormone replacement therapy or oral contraceptive pills, underlying malignancy and systemic vascular diseases were excluded. The patients with associated femur, tibia or spine injury or vascular injury receiving heparin therapy were also excluded. A total of 56 patients were included in this study. Eleven of these had 13 associated injuries (two clavicle fractures, two humerus fractures, two Galleazi or Monteggia fracture dislocations, one both-bone forearm fracture, one scapula fracture, one shoulder dislocation, two metatarsal fractures, and two patella fractures).
As soon as these patients arrived at our emergency service, adequate resuscitation and haemodynamic stability was achieved. They were closely monitored for their vital parameters (blood pressure, pulse rate, respiration rate, and urine output). Those patients who had fracture dislocations underwent urgent reduction followed by skin/skeletal traction. Early active and passive physiotherapy was started as tolerated by the patients. Routine investigations (full blood counts, renal and liver function tests, coagulation profile, and arterial blood gas analysis) were performed. A detailed history was taken and clinical and specific laboratory investigations were conducted to exclude any risk factors of VTE. After obtaining their consent, these patients were enrolled into the study.
The patients were operated upon as soon as they were fit for the surgery. No mechanical or chemical prophylaxis was administered in the postoperative period. They were evaluated daily for signs and symptoms of VTE, during their course in hospital. Clinical evaluation for DVT was done with particular attention to recent onset lower limb swelling, calf tenderness and Homan's sign. Similarly, patients with breathing difficulty, pleuritic chest pain, and pleural rub were evaluated for underlying PE.
Those patients having no clinical evidence of VTE were evaluated by pulmonary angiography and indirect CT venography on the fifth (±2) day after surgery for radiological evidence of VTE. A contrast study using 16-slice spiral CT (Siemens-Sensation) and 130 ml of non-ionic dye infused at a rate of 2 ml per second was performed. A venous phase study was obtained after a total delay of 180 seconds. Films were evaluated by expert radiologists for any evidence of VTE. Those patients having evidence of VTE were treated as per American College of Chest Physicians (ACCP) guidelines [9].
Patients suspected of VTE on clinical grounds underwent pulmonary angiography and indirect CT venography on the same day and those found positive were treated as per the above guidelines.
All these patients were discharged after suture removal and complete stabilisation. Patients were followed up by direct questioning over telephone up to six weeks after hospital discharge with regard to any complaint suggestive of VTE. When VTE was suspected from history, patients were evaluated clinically and by colour Doppler (Philips ALT) in the out-patient department as early as possible. Patients not having any complaint suggestive of VTE were routinely evaluated by colour duplex at the end of six weeks from hospital discharge for evidence of DVT in bilateral calf, thigh and pelvic veins. The same protocol was used to monitor response to therapy in patients diagnosed with VTE during initial screening. All the radiological investigations were performed and assessed by a senior radiologist. Those patients found to have radiological evidence of DVT were treated as per ACCP guidelines [12].
Results
The average age of the patients was 36.42 years (range, 17–61). There were 48 males and eight females. The fracture distributions of the patients were as noted in Table 1. The acetabular fractures were also classified as per Letournel; and on frequency distribution, bicolumnar fractures (28.6%) and transverse with posterior wall fractures (21.4%) were found to be most frequent types. The mean delay between injury and surgery in this study was 12.2 days.
Table 1.
Comparison of frequency of different acetabular fractures in this study to that reported by previous studies using Letournel classification for acetabular fractures. We observed similar frequency of different fracture types as reported by Montgomery et al. and Fishmann et al. [7, 25]
| Fracture pattern | This study | Montgomery et al. [25] | Fishmann et al. [7] |
|---|---|---|---|
| Posterior wall | 7 (12.5%) | 15 (15%) | 18 (12%) |
| Posterior column | 3 (5.35%) | 3 (3%) | 1 (0.67%) |
| Anterior wall | 0 | 0 | 4 (2.7%) |
| Anterior column | 1 (1.8%) | 5 (4%) | 18 (12%) |
| Transverse | 2 (3.57%) | 0 | 3 (2%) |
| Posterior column and posterior wall | 4 (7.14%) | 7 (7%) | 3 (2%) |
| Transverse and posterior wall | 12 (21.4%) | 23 (23%) | 29 (19%) |
| T-shape fracture | 7 (12.5%) | 12 (12%) | 13 (8.7%) |
| Anterior wall and posterior hemitransverse | 4 (7.14%) | 11 (11%) | 16 (10.8%) |
| Bicolumnar fracture | 16 (28.6%) | 22 (22%) | 42 (29%) |
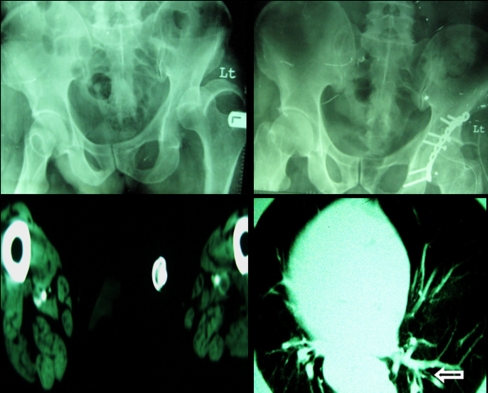
During the course in hospital, six patients had clinical evidence of VTE (one chest pain, two calf tenderness, two thigh tenderness and one fever) and 15 patients (26.8%) had radiological evidence of VTE. The thrombi were classified to be proximal if they were found in the popliteal or more proximal vein and distal if they involved tibial or calf muscle veins. Two patients had distal DVT with associated proximal DVT and only one had associated PE. A total of 11 patients had acute proximal DVT (19.6%) and six of these had PE (54.5%) (Fig. 1). Three patients had bilateral proximal DVT with presence of thrombus also in the uninjured limb. However, none of the patients had thrombus in the isolated uninjured limb. Pulmonary embolism was detected in ten out of 56 patients (17.85%) (Fig. 2). In four cases of PE, no DVT locus was identified; two of these cases had clinical evidence of distal DVT.
Fig. 1.
Radiographs of a 58-year-old male showing left posterior wall acetabulum fracture that was treated by open reduction and internal fixation with recon plate. Postoperative CT pulmonary angiography and indirect venography shows bilateral femoral vein thrombi and pulmonary embolus in left lung segmental artery (arrow)
Fig. 2.
Radiographs of a 42-year-old male showing left acetabulum fracture that was treated by open reduction and internal fixation with recon plates. Postoperative CT pulmonary angiography and indirect venography shows saddle embolus at the left pulmonary trunk compared with normal pulmonary trunk on right side
In between hospital discharge and six weeks follow-up, only one additional patient had radiological and clinical evidence of proximal vein DVT. One other patient with limb oedema on clinical examination did not have colour Doppler evidence of DVT.
In total, 16 cases of radiologically proved VTE were observed during the study period (28.6%). Clinical VTE was seen in six of these cases (37%). Complete resolution of thrombus was noted in all patients undergoing evaluation by colour Doppler at six weeks and no death occurred during the study period from any cause. There was no difference among the two groups in relation to age, sex, and duration between injury and surgery (P = 0.471).
Discussion
VTE after major trauma is the most common cause of morbidity and mortality in patients who survive the first 24 hours [8, 28]. Though routine chemoprophylaxis is provided to all such patients in western nations, its use in the Asian population is still lacking because a proper study on these populations has not been performed to date. With increasing incidence of high velocity injuries, the numbers of pelviacetabular fractures are also rising in Asian countries. These cases are now increasingly being treated surgically [10, 17]. However, no one has ever estimated the risk of VTE in this population after surgery. This is the first study based on VTE in pelvi-acetabular injury among the Indian population.
ACCP reports that prevalence of VTE in trauma is higher than arthroplasty [9]. Furthermore, the pathophysiology of VTE in trauma is different from elective surgery and most thrombi in these patients are proximal [8, 24, 28]. Pelvi-acetabular fractures result from high velocity trauma, associated with injury to vascular structures around the hip and require prolonged immobilisation [8, 24]. Subsequent manipulation during surgery causes further insult to the vascular endothelium [8]. According to western literature, the incidence of DVT in pelvi-acetabular injuries varies from 10 to 60% and about 50% of these thrombi involve proximal veins [8, 23, 24, 28, 32–34]. As 95% of pulmonary emboli originate in proximal veins and more than 50% of patients with proximal thrombosis develop pulmonary embolism, pulmonary embolism is more likely with pelvi-acetabular injuries when compared to general trauma patients [27]. Incidence of PE in pelvi-acetabular injuries ranges from 2 to 10% compared to an overall incidence of 0.5 to 2% in trauma patients and is the most common cause of death in the postoperative period [37].
Patients with associated injuries which are independent risk factors for VTE [8] (long bone lower limb injuries, spinal injuries and blunt trauma to abdomen or chest) and predisposing medical conditions [9] have been excluded from this study. Therefore we expect that our results reflect the true risk of VTE attributable to pelvi-acetabular trauma and consequent surgery per se. The results of our study have been compared to other major studies of VTE in pelvi-acetabular trauma patients (Tables 1 and 2). Comparison with other studies is however challenging due to differences in patient profiles, diagnostic modality used and aspects of VTE studied. Even after excluding all other risk factors of VTE, the demographic profile of patients in our study is not different from other studies. The mean age of patients in our study is similar to those of patients in other studies. Compared to other studies we have fewer females in this study, but sex of the patient has not been shown to be a factor influencing the rate of VTE. Unlike other studies no prophylaxis was administered in our patients, and hence it truly reveals the incidence of VTE in these particular patients.
Table 2.
Comparison of this study with other major studies on venous thromboembolism (VTE) in pelviacetabular trauma
| Study | This study | Montgomery et al. 1997 [25] | Geerts et al. 1994 [8] | Fishmann et al. 1994 [7] | Stannard et al. 2001 [33] | Steel et al. 2005 [34] |
|---|---|---|---|---|---|---|
| Number of patients | 56 | 101 | 100 | 197 | 107 | 103 |
| Mean age (years) | 36 | 42 | 39 | 40 | - | 37 |
| Male :female | 48 :8 | 69 :42 | - | 105 :45 | - | 83 :20 |
| Associated injuries | 11(19%) | 66 (66%) | - | 120 (61%) | - | 77 (76%) |
| Medical comorbidities | 0 | - | - | - | - | - |
| Prophylaxis | No | Heparin + IVC filter | No | Mechanical + Warfarin | Mechanical | LMWH |
| Radiological screening | CTVPA | MRV | Conventional Venography | Colour duplex | MRV | Colour duplex |
| Proximal DVT | 11 (19.6%) | 37 (37%) | 29 (29%) | 20 (10%) | 15 (14%) | 10 (10%) |
| PE | 10 (17.8%) | 1 | - | 2 (1%) | 1 | 5 (5%) |
| Total acute VTE | 15 (27%) | 38 (38%) | 61% | 20 (10%) | 16 (15%) | 10 (10%) |
| Clinical VTE | 6 (40%) | 0 | - | 0 | 0 | |
| Number of Death | 0 | 0 | - | 2 | 0 | 2 |
| Late DVT | 1 | - | - | 1 | - | |
| Nature of study | Postoperative | Preoperative | Postoperative | Postoperative | Postoperative | Preoperative |
DVT deep vein thrombosis, PE pulmonary embolism, IVC inferior venacava, LMWH low molecular weight heparin, CTVPA CT pulmonary angiography and indirect venography, MRV magnetic resonance venography
Colour Doppler as the diagnostic modality has been observed to be insensitive in diagnosing pelvic thrombi [3, 25, 26]. Most thrombi occurring after pelvi-acetabular injuries are proximal and up to 30% of thrombi in these patients involve pelvic veins [8]. Both Fishmann et al. and Steel et al. used colour Doppler, and low rate of VTE reported in their studies may be due to this factor [7, 34]. Geerts et al. used conventional venography, though considered to be the gold standard in diagnosis of DVT, it has been found to be false negative in 58% of cases of pelvic thrombi [25]. Magnetic resonance venography (MRV) is a non invasive test with sensitivity and specificity of 100% and 97%, respectively [3]; however, it can detect very small thrombi which may not be clinically significant [32]. When using any of the above modalities, a second test is required to diagnose PE. None of the previous studies used routine screening of patients for PE. Since some of the thrombi can form in pulmonary artery [36] and PE frequently remains asymptomatic, it is likely that some important VTE events have been missed by all the previous studies.
CT pulmonary angiography and indirect venography (CTVPA) is a new protocol introduced in 1998 [18]. It has been shown to be highly sensitive and detects both pulmonary embolism and deep venous thrombosis using same contrast in the circulation. The method is being increasingly used as a ‘single stop’ investigation for VTE [12]. Though it has never been compared to conventional venography (rarely performed today), compared to lower limb sonography it is 97% sensitive and 100% specific in detecting femoral-popliteal thrombus [19]. In addition, it detects pelvic and venacaval thrombi which are not detected by sonography. This technique has not been used earlier to study VTE in pelvi-acetabular injury patients. Using this method in this study, we diagnosed 15 cases of acute postoperative VTE (11 cases of proximal DVT, 19.6%; and ten cases of PE, 17.8%). VTE was suspected clinically in only six of the 15 patients (40%) and was confirmed in all of them by radiological study.
Presence of proximal DVT is of more significance because of its potential to cause pulmonary embolism [27]. The rate of proximal DVT in this study (19.6%) was slightly less than that reported by Geerts et al. and Montgomery et al. (29% and 34%, respectively) [8, 25]. This difference can be due to risk stratification used in our study. However, 54.5% of these patients had associated PE, which is almost equivalent to that reported by Moser and Steel [27, 34]. Three patients with proximal DVT had bilateral thrombi, with unilateral limb injury, and no case of isolated thrombi to uninjured limb was found in this study. In a study of Montgomery et al., 12% of the thrombi were bilateral and 12% of thrombi involved only the uninjured limb [25]. Thrombus formation in uninjured limbs is due to procoagulant environment in post trauma patients, contributed by release of tissue factors, decreased Antithrombin III, release of acute phase reactants from liver and unregulated Thrombin formation [21, 24, 31].
Diagnosis of PE in previous studies was mainly based on clinical features and had reported lower incidence (0–2%). The apparently high rate of PE in this study (17.85%) could be explained by the universal screening of all patients with CT angiography. Out of ten cases of PE diagnosed in this study, only one had a clinical sign (chest pain). Routine screening of patients for PE led to diagnosis of nine clinically silent PE and hence avoided mortality. Four cases of PE had isolated involvement without any evidence of DVT, which would have been missed with routine screening of lower limb only. Using CT pulmonary angiography and indirect venography, Velmahos et al. reported 19% incidence of PE and 7% incidence of DVT in 247 patients sustaining major trauma [36]. They suggested that some of the thrombus in pulmonary circulation are not related to DVT and may arise denovo.
DVT can occur up to six weeks after hospital discharge [9] and some studies suggest that most DVT occur after discharge from hospital [5, 30]. We evaluated all our patients until the end of six weeks with colour Doppler, as it is an ideal diagnostic tool for out-patients. Late onset DVT has not been studied before by any other study on pelvi-acetabular trauma patients. Stannard et al. reported one case of late onset DVT developing after negative postoperative MRV; however, they did not screen patients routinely for DVT after hospital discharge [32].
Sensitivity of clinical signs for VTE in this study (37%) is similar to other studies on trauma patients [28]. None of the patients in the study of Montgomery et al. had clinical signs of DVT and one patient was suspected to have PE on pulse oxymetry [25]. Geerts et al. reported clinical VTE in only 1.5% of their cases [8]. The absence of symptomatic VTE in the study of Montgomery et al. could be due to use of thromboprophylaxis. It is also likely that clinical signs such as limb tenderness and chest pain would have been masked by associated injuries in some of their patients.
We did not find any association between delay in surgery and the risk of VTE (P = 0.471), a finding similar to Steel et al. [34]. However, Montgomery et al. and Stannard et al. reported significant association of VTE with prolonged period of immobilisation, which fits with current understanding of VTE pathogenesis [24, 33]. Our findings cannot be compared to those of Montgomery et al. as they studied VTE rates in the preoperative period. The surgery and subsequent manipulation in trauma patients increases the VTE risk [28]. We also did not find any correlation between VTE and age and sex.
A limitation of this study is the small sample size. However, as a pilot study, we conclude that Indian patients sustaining pelvi-acetabular trauma have significant risk of postoperative VTE, even in the absence of any associated injury or predisposing medical condition. Most of these are located in proximal veins which have high propensity to develop PE. Administration of routine thromboprophylaxis is fully justified in these patients.
References
- 1.Agarwal S, Bhagwat AS, Modhe J. Deep vein thrombosis in Indian patients undergoing major lower limb surgery: Distribution of thrombi and its significance. Indian J Surg. 2003;65:159–162. [Google Scholar]
- 2.Atichartakarn V, Pathopchotiwang K, Keorochano S, Eurvilaichit C. Deep vein thrombosis after hip surgery in Thai. Arch Intern Med. 1988;148:1349–1353. doi: 10.1001/archinte.148.6.1349. [DOI] [PubMed] [Google Scholar]
- 3.Carpenter JP, Holland GA, Baum RA, Owen RS. Magnetic resonance venography for detection of venous thrombosis, comparison with contrast venography and duplex ultrasonography. J Vasc Surg. 1993;18:734–741. doi: 10.1067/mva.1993.49364. [DOI] [PubMed] [Google Scholar]
- 4.Chan YK, Chiu KY. The incidence of DVT in elderly Chinese suffering hip fracture is low. J Orth Surg. 2004;12(2):178–183. doi: 10.1177/230949900401200208. [DOI] [PubMed] [Google Scholar]
- 5.Dahl OE, Andressen G, Aspelin T, et al. Prolonged prophylaxis following hip replacement surgery. J Thromb Haemostat. 1997;77:26–31. [PubMed] [Google Scholar]
- 6.Dhillon KS, Askander A, Doraisamy S. Postoperative deep-vein thrombosis in Asian patients is not a rarity. J Bone Joint Surg Br. 1996;78:427–430. [PubMed] [Google Scholar]
- 7.Fishmann AJ, Greeno RA, Brooks LR, Matta JM. Prevention of deep vein thrombosis and pulmonary embolism in acetabular and pelvic fracture surgery. Clin Orthop. 1994;305:133–137. [PubMed] [Google Scholar]
- 8.Geerts WH, Code KI, Jay RM, Chen E. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–1606. doi: 10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 9.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edn) Chest. 2008;133:381–453. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 10.Gupta RK, Singh H, Dev B, Kansay R, Gupta P, Garg S. Results of operative treatment of acetabular fractures from the Third World—how local factors affect the outcome. Int Orthop. 2009;33:347–352. doi: 10.1007/s00264-007-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kakkar N, Vasishta RK. Pulmonary embolism in medical patients: An autopsy-based study. Clin Appl Thromb Hemost. 2008;14(2):159–167. doi: 10.1177/1076029607308389. [DOI] [PubMed] [Google Scholar]
- 12.Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians evidence-based clinical practice guidelines (8th edn) Chest. 2008;133:454–535. doi: 10.1378/chest.08-0658. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Kim JS. Incidence and natural history of deep-vein thrombosis after total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 2002;84:566–570. doi: 10.1302/0301-620X.84B4.12330. [DOI] [PubMed] [Google Scholar]
- 14.Kim YH, Oh SH, Kim JS. Incidence and natural history of deep-vein thrombosis after total hip arthroplasty. A prospective and randomised clinical study. J Bone Joint Surg (Br) 2003;85:661–665. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 15.Knudson MM, Collins JA, Goodman SD, Mc Crory DW. Thromboembolism following multiple trauma. J Trauma-Inj Infect Crit Care. 1992;32:2–11. doi: 10.1097/00005373-199201000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Lee AD, Stephen E, Agarwal S, Premkumar P. Venous thrombo-embolism in India. Eur J Vasc Endovasc Surg. 2009;37:482–485. doi: 10.1016/j.ejvs.2008.11.031. [DOI] [PubMed] [Google Scholar]
- 17.Liu X, Xu S, Zhang C, Su J, Baoqing Y. Application of a shape-memory alloy internal fixator for treatment of acetabular fractures with a follow-up of two to nine years in China. Int Orthop. 2009 doi: 10.1007/s00264-009-0867-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loud PA, Grossman ZD, Klippenstein DL, Ray CE. Combined CT venography and pulmonary angiography, a new diagnostic technique for suspected thromboembolic disease. Am J Roentgenol. 1998;170:951–954. doi: 10.2214/ajr.170.4.9530042. [DOI] [PubMed] [Google Scholar]
- 19.Loud PA, Katz DS, Klippenstein DL, Shah RD, Grossman ZD. Combined CT venography and pulmonary angiography in suspected thromboembolic disease: Diagnostic accuracy for vein evaluation. Am J Roentgenol. 2000;174(1):61–65. doi: 10.2214/ajr.174.1.1740061. [DOI] [PubMed] [Google Scholar]
- 20.Mavalankar AP, Majmundar D, Sudha R. Routine chemoprophylaxis for DVT in Indian patients. Indian J Orthop. 2007;41(3):188–191. doi: 10.4103/0019-5413.33680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller RS, Weatherford DA, Stein D, Crane MM, Stein M. Antithrombin III and trauma patients: factors that determine low levels. J Trauma Inj Infect Crit Care. 1994;37:442–445. doi: 10.1097/00005373-199409000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Mitra AK, Khoo TK, Nagan C. Deep-vein thrombosis following hip surgery for fracture of proximal femur. Singapore Med J. 1989;30:531–534. [PubMed] [Google Scholar]
- 23.Montgomery KD, Geerts WH, Code KI. Thromboembolic complications in patients with pelvic trauma. Clin Orthop. 1996;329:68–87. doi: 10.1097/00003086-199608000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Montgomery KD, Geerts WH, Potter HG, Helfet DL. Practical management of venous thromboembolism following pelvic fracture. Orthop Clin North Am. 1997;28(3):397–404. doi: 10.1016/S0030-5898(05)70297-2. [DOI] [PubMed] [Google Scholar]
- 25.Montgomery KD, Potter HG, Helfet DL. The detection and management of proximal deep venous thrombosis in patients with acute acetabular fractures: A follow-up report. J Orthop Trauma. 1997;11(5):330–336. doi: 10.1097/00005131-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Morgan SJ, Jeray KJ, Laura SP. Attitude of orthopaedic trauma surgeons regarding current controversies in management of pelvic and acetabular fracture. J Orthop Trauma. 2001;15(7):526–532. doi: 10.1097/00005131-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Moser KM, Lemoine JR. Is embolic risk conditioned by location of deep venous thrombus? Ann Intern Med. 1981;94:439–444. doi: 10.7326/0003-4819-94-4-439. [DOI] [PubMed] [Google Scholar]
- 28.Napolitano LM, Garlapati VS, Heard SO, et al. Asymptomatic deep venous thrombosis in the trauma patient: is an aggressive screening protocol justified? J Trauma. 1995;39:651–657. doi: 10.1097/00005373-199510000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Piovella F, Wang CJ, Lu H, Lee K, et al. Deep venous thrombosis rates after major orthopedic surgeries in Asia. An epidemiological study based on postoperative screening with centrally adjusted bilateral venography. J Thromb Hemostat. 2005;3:2664–2630. doi: 10.1111/j.1538-7836.2005.01621.x. [DOI] [PubMed] [Google Scholar]
- 30.Planes A, Vochelle N, Darman JY. Risk of deep-vein thrombosis after hospital discharge in patients having undergone total hip replacement. Lancet. 1996;348:224–228. doi: 10.1016/S0140-6736(96)01453-5. [DOI] [PubMed] [Google Scholar]
- 31.Selby R, Geerts W, Ofosu FA, Craven S, Dewar L, Phillips A, et al. Hypercoagulability after trauma: hemostatic changes and relationship to venous thromboembolism. Thromb Res. 2009;124(3):281–287. doi: 10.1016/j.thromres.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Stannard JP, Singhania AK, Lopez-Ben R. Deep-vein thrombosis in high energy trauma despite prophylaxis. J Bone Joint Surg Br. 2005;87:965–968. doi: 10.1302/0301-620X.87B7.15989. [DOI] [PubMed] [Google Scholar]
- 33.Stannard JP, Riley RS, McClenney MD, Lopez-Ben RR, Volgas DA, Alonso JE. Mechanical prophylaxis against deep-vein thrombosis after pelvic and acetabular fractures. J Bone Joint Surg Am. 2001;83:1047–1051. doi: 10.2106/00004623-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Steel N, Dodenhoff RM, Ward AJ. Thromboprophylaxis in pelvic and acetabular trauma surgeries. J Bone Joint Surg Br. 2005;87:209–212. doi: 10.1302/0301-620X.87B2.14447. [DOI] [PubMed] [Google Scholar]
- 35.Todi SK, Sinha S, Chakraborthy A, Sarkar A, Gupta S, Das T, et al. Utilisation of deep venous thrombosis prophylaxis in medical/surgical intensive care units. Indian J Crit Care Med. 2003;7(2):103–105. [Google Scholar]
- 36.Velmahos GC, Spaniolas K, Tabbara M, Abujudeh HH, Moya M, Gervasini A, et al. Pulmonary embolism and deep venous thrombosis in trauma: are they related? Arch Surg. 2009;144(10):928–932. doi: 10.1001/archsurg.2009.97. [DOI] [PubMed] [Google Scholar]
- 37.Webb LX, Fuller SB, Menedith JW. Greenfield filter prophylaxis of pulmonary embolism in patients undergoing surgery for acetabulum fracture. J Orthop Trauma. 1992;6:139–145. doi: 10.1097/00005131-199206000-00002. [DOI] [PubMed] [Google Scholar]