Abstract
The objective of this study was to evaluate the survivorship of revision TKA and determine the reasons and predictors for failure. Between January 1999 to December 2005, 499 total knee arthroplasty revisions were performed on 474 patients. There were 292 (61.6%) women and 182 (38.4%) men. The average age at the time of index revision was 63.9 years. Revision was defined as surgery in which at least one component (tibial, patellar, femoral, or polyethylene) required exchange. At an average follow-up of 64.8 months (range, 24.1–111.6), and considering reoperation or re-revision as failure, there were 102 failures (18.3%). Infection was the major cause of failure (44.1%) followed by stiffness (22.6%), patellar or extensor mechanism problems (12.8%), periprosthetic fracture (5.9%), loosening (4.9%), haematoma formation (3.9%), malalignment (2.9%), and instability (2.9%). A total of 83% of failures were early (less than two years). Infection was the most common mechanism of failure of revision TKA. The majority of TKA revision failures tend to occur in the first two years after revision. The mode of failure of revision TKA appears to differ from the failure of primary TKA to some extent. Better understanding of current modes by which TKA revisions fail may enable surgeons to prevent these problems and improve outcomes for revision TKA.
Introduction
Primary total knee arthroplasty (TKA) is a successful operation associated with dramatic improvements in quality of life and restoration of function for the patient. Primary TKAs are durable procedures with survivorship exceeding 90% in the second decade. However, failures of TKA may occur, leading to a need for revision arthroplasty [1–6]. Despite the low percentage of primary TKA failures, it is reasonable to expect an increase in the annual number of revision TKAs as the number of primary TKAs performed continues to increase annually [7].
Revision TKA is generally considered as a reliable procedure with predictable outcome [8, 9]. However, the outcome of revision TKA is not as successful as primary TKA due to a multitude of factors including the complexity of the procedure associated with bone loss and soft tissue, the need to use larger and more constrained prostheses, and so on [8–10]. On the other hand, the cost of TKA revisions is approximately double that of a primary procedure because of the increased technical demands (implants and allografts), length of hospital stay, higher complication rate, and lengthier period of convalescence [11–14]. Considering the technical complexity and economic burden of the revision TKA procedure, it would be advantageous to investigate current mechanisms and the predictors for TKA revisions failure, thereby focussing future efforts to address these mechanisms of failure and improve the ultimate outcome of TKA revisions.
The objective of this study was to evaluate the survivorship of revision TKA and to determine the relative contributions of different mechanisms in the failure of revision TKA. We also sought to determine the potential predictors of failure after TKA revisions.
Materials and methods
After obtaining institutional review board approval and patient consent, patients undergoing revision TKA were identified from the institutional prospective database. There were 503 patients undergoing 517 revision TKAs between the dates of January 1999 and December 2005. Twenty-nine patients died prior to completion of a two-year follow-up, leaving 474 patients (499 knees) to be included. The primary TKA in 165 (33%) revisions was performed at our institution while the remaining 334 knees (67%) were referred to our institution for revision. The average follow-up was 64.8 months (range, 24.1–111.6). The average age at the time of index revision was 63.9 years (range, 33–94 years) of which 292 (61.3%) were women and 182 (38.7%) were men. The average height, weight, and body mass index (BMI) for the male patients were 180.4 cm (range, 156.8–248.9), 99.7 kg (range, 66.2–150.0), and 30.3 kg/cm2 (range, 19.0–45.9), respectively. Similarly, the average height, weight, and BMI for the female patients were 164.20 cm (range, 150.1–237.3), 89.8 kg (range, 52.9–147.5), and 33.7 kg/cm2 (range, 17.7–62.1), respectively.
Revision was defined as the need for exchange of at least one component (femur, tibia, patella or tibial polyethylene liner). Multi-stage revisions were treated as a single procedure. Revision failure, used as the endpoint, was defined as need for reoperation when general or regional anaesthesia was required. Of the 499 included knees, 102 patients (102 knees) required reoperations. The cause of failure was determined by the treating surgeon and categorised into one of nine modes of failure: infection, stiffness, aseptic loosening, extensor mechanism dysfunction, instability, fracture, malpositioning/malalignment, wear, and wound related problems (haematoma formation or persistent wound drainage). When applicable, multiple modes of failure were noted but categorised by the predominant modality for analysis. Aseptic loosening of either the tibial, femoral, and/or patellar components was always treated as a secondary mode of failure when found in conjunction with another failure mechanism, while loosening of only the patellar component was considered primarily as an extensor mechanism problem and secondarily as aseptic loosening. Infection was always considered as primary mode of failure if present. In assessing the mode of failure, preoperative history, physical examination and radiographic findings, along with the analysis of intraoperative findings including examination under anaesthesia, gross inspection of the components, and fluid and tissue cultures were considered. Failures were subdivided into an early group whose reoperation was performed less than two years from the index revision, and a late group whose reoperation was performed more than two years after index revision. These failure groups are consistent with previously published criteria [15].
Indications for revision
The predominant indication for revision of the primary TKA in this cohort of 474 patients (499 knees) was aseptic loosening (153 knees, 30.7%) followed by infection (101 knees, 20.2%) and wear (66 knees, 13.1%). Stiffness (52 knees, 10.5%) and extensor mechanism dysfunction (52 knees, 10.5%) were the next common reasons for index revision, followed by instability (40 knees, 8%), periprosthetic fracture (21 knees, 4.2%) and malalignment/malpositioning (14 knees, 2.8%). Periprosthetic joint infection was diagnosed based on the presence of one of the following criteria: (1) abscess or sinus tract that communicated to the joint space, (2) positive growth on solid medium from joint aspiration fluid or intraoperative culture, (3) purulence detected intraoperatively, or (4) an elevated cell count and differential of the aspirate fluid, and abnormal erythrocyte sedimentation rate (>30 mm/hr) or C-reactive protein > 10 mg/dL. At the time of revision for infections, patients were treated according to the appropriate protocol for their clinical presentation. For acute haematogenous infections, patients underwent irrigation and debridement along with polyethylene exchange. For chronic infection, patients usually receive two-stage exchange. The majority (88%) of patients with primary TKA infection were treated by two-stage exchange arthroplasty. Eight patients (9%) were treated with irrigation and debridement along with exchange of the tibial polyethylene insert. Three patients (3%) underwent debridement, removal of prosthetic components and bone cement and insertion of new prosthesis using antibiotic-impregnated cement. All patients undergoing revision surgery at our institution receive prophylactic antibiotics within 30 minutes of tourniquet inflation. Cephozoline is the antibiotic of choice; however, for patients with penicillin allergy, history of infection with resistant staphylococcus, healthcare workers, and institutionalised patients, vancomycin is the preferred prophylactic antibiotic. All antibiotics are continued after revision TKA until the results of culture are obtained.
Statistical analysis
All data were analysed using standard descriptive statistics, and parametric and nonparametric two-tailed tests for comparisons (Fisher’s exact and Student t tests). Using an unadjusted logistic regression, all covariates were tested. We report the corresponding odds ratios, 95% confidence intervals, and p values. Any p value of less than 0.05 was considered significant. Multivariate logistic regression analysis was used to model the effects of different patient- or procedure-related factors on the risk of failure following index revision TKA. Kaplan-Meier survivorship analysis was calculated for the entire patient cohort, as well as septic and aseptic modes of failure.
Results
Modes of revision failure
Of the 499 index revisions performed, 102 patients (102 knees) required reoperation yielding a 20.4% failure rate. The primary modes of TKA revision failure were infection (44.1%), followed by stiffness (22.6%), extensor mechanism problems (12.8%), fracture (5.9%), aseptic loosening (4.9%), haematoma (3.9%), misalignment/malpositioning (2.9%), and instability (2.9%). Wear was not found to be a mechanism of failure in any index revision patient in this group. The most prevalent organism isolated from infected revision operations was Staphylococcus aureus (27.3%), followed by Staphylococcus epidermidis (16%), Streptococcus group B (4.6%), Proteus mirabilis (4.6%), Streptococcus mitis (2.2%), Pseudomonas aeroginosa (2.2%), Citrobacter spp. (2.2%), and Enterobacter faecalis (2.2%). Out of 19 staphylococcal organisms, 11 were methicillin-resistant. In 16 (36.5%) patients with infected TKA revisions, no organism was identified.
Among the 102 patients who failed, the indication for index revision was infection (31.4%), followed by aseptic loosening (19.6%), stiffness (13.7%), extensor mechanism problems (10.8%), wear (8.8%), instability (5.9%), fracture (5.9%), and misalignment/malpositioning (3.9%).
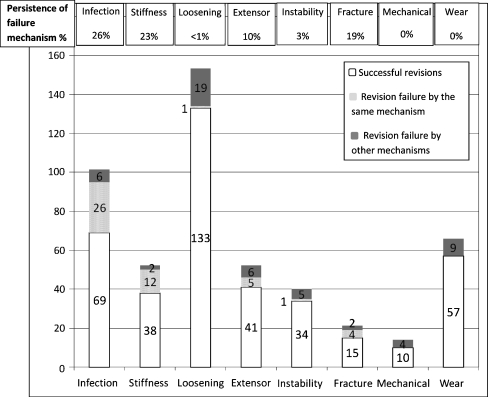
Persistence of failure
The data was then evaluated to discover if the indication for index revision and the reason for reoperation or re-revision were the same. Among 101 patients who underwent revision for infection, 26 patients (27%) failed again because of infection; in other words, diagnosis of infection at the time of index arthroplasty was the most important predictor for later failure as a result of further infection. The reverse was true for aseptic loosening, as among 153 patients undergoing revision TKA, one patient (<1%) failed again because of aseptic loosening (Fig. 1).
Fig. 1.
Persistence or recurrence rate of different failure mechanisms (columns indicate the number of knees)
Predictors of failure
Using univariate analysis for different potential patient- and surgery-related factors, body mass index, comorbidities, presence of respiratory disease, hypothyroidism, time from the primary to revision, indication for revision, revision for wear or infection, and transfusion were found to be significant predictors of failure (Table 1). Considering all potential variables, multivariate analysis using hypothesis-driven modelling revealed infection to be the only independent predictor of failure after allowing for all potential confounders including age, gender, BMI, the underlying joint disease and comorbidities (using Charlson Index [16]). Patients with infection as the cause of failure were 1.71 (confidence interval, 1.1–2.94) times more likely to fail than patients who underwent revision for aseptic reasons (p < 0.05).
Table 1.
Descriptive and unadjusted univariate analysis comparing cases with failure to controls who did not fail
| Characteristic | Failure (n = 102) | No failure (n = 397) | Odds ratio (95% CI) | P value |
|---|---|---|---|---|
| Age | 66.31 (10.66) | 66.65 (11.18) | 1.00 (0.98, 1.02) | 0.78 |
| Male sex | 41 (40.20%) | 145 (36.52%) | 1.17 (0.75, 1.82) | 0.49 |
| BMI (continuous) | 32.04 (8.46) | 33.36 (8.22) | 0.98 (0.95, 1.01) | 0.17 |
| BMI≥25 | 76 (80.85%) | 312 (88.64%) | 0.54 (0.29, 1.00) | 0.05 |
| ASA (continuous) | 2.41 (0.78) | 2.36 (0.77) | 1.10 (0.83, 1.46) | 0.51 |
| Charlson (continuous) | 3.49 (2.37) | 2.78 (1.60) | 1.22 (1.09, 1.37) | <0.01 |
| Charlson > 3 | 44 (43.14%) | 109 (27.46%) | 2.00 (1.28, 3.14) | <0.01 |
| Dx other than OA | 10 (9.80%) | 19 (4.79%) | 2.16 (0.97, 4.81) | 0.06 |
| Inflammatory arthritis | 13 (12.75%) | 29 (7.30%) | 1.85 (0.93, 3.71) | 0.08 |
| Heart | 32 (31.37%) | 112 (28.21%) | 1.16 (0.73, 1.86) | 0.53 |
| HT | 61 (59.80%) | 207 (52.14%) | 1.37 (0.88, 2.12) | 0.17 |
| DM | 27 (26.73%) | 92 (23.17%) | 1.21 (0.73, 1.99) | 0.45 |
| Vascular arterial | 12 (11.76%) | 71 (17.88%) | 0.61 (0.32, 1.18) | 0.14 |
| Respiratory disease | 28 (27.45%) | 61 (15.37%) | 2.08 (1.25, 3.48) | 0.01 |
| GI | 32 (31.37%) | 92 (23.17%) | 1.52 (0.94, 2.45) | 0.09 |
| Renal | 3 (2.94%) | 6 (1.51%) | 1.97 (0.49, 8.03) | 0.34 |
| Liver | 6 (5.88%) | 15 (3.78%) | 1.59 (0.60, 4.21) | 0.35 |
| Thyroid | 20 (19.61%) | 39 (9.82%) | 2.24 (1.24, 4.04) | 0.01 |
| Vascular venous | 8 (7.84%) | 28 (7.05%) | 1.12 (0.50, 2.54) | 0.78 |
| Stroke | 3 (2.94%) | 8 (2.02%) | 1.47 (0.38, 5.66) | 0.57 |
| Cancer | 10 (9.80%) | 49 (12.34%) | 0.77 (0.38, 1.58) | 0.48 |
| Bilateral | 12 (11.76%) | 39 (9.82%) | 1.22 (0.62, 2.43) | 0.56 |
| Primary TKA done at our Institute | 38 (40.20%) | 127 (33.25%) | 1.35 (0.86, 2.11) | 0.19 |
| Duration primary to secondary | 3.69 (3.50) | 4.90 (4.64) | 0.93 (0.88, 0.99) | 0.02 |
| Indication | 0.01a | |||
| Stiffness | 14 (13.73%) | 38 (9.57%) | 1.50 (0.78, 2.90) | 0.22 |
| Extensor | 12 (11.76%) | 40 (10.08%) | 1.19 (0.60, 2.36) | 0.62 |
| Fracture | 5 (4.90%) | 16 (4.03%) | 1.23 (0.44, 3.43) | 0.70 |
| Instability | 6 (5.88%) | 34 (8.56%) | 0.67 (0.27, 1.64) | 0.38 |
| Mechanical | 3 (2.94%) | 11 (2.77%) | 1.06 (0.29, 3.88) | 0.93 |
| Wear | 7 (6.86%) | 59 (14.86%) | 0.42 (0.19, 0.95) | 0.04 |
| Infection | 33 (32.35%) | 68 (17.13%) | 2.31 (1.42, 3.78) | <0.01 |
| Loosening | 22 (21.57%) | 131 (33.00%) | 1.17 (0.75, 1.83) | 0.49 |
| OR time | 148.65 (49.25) | 148.07 (46.13) | 1.00 (1.00, 1.01) | 0.92 |
| Unit transfused | 1.00 (1.05) | 1.09 (1.10) | 0.92 (0.72, 1.18) | 0.52 |
| Transfusion | 42 (41.18%) | 256 (64.48%) | 0.39 (0.25, 0.60) | <0.01 |
CI confidence interval, BMI body mass index, ASA American Society of Anesthesiologists, Dx diagnosis, OA osteoarthritis, HT hypertension, DM diabetes mellitus, GI gastrointestinal, OR operating room, TKA Total Knee Arthroplasty
a Chi-squared overall
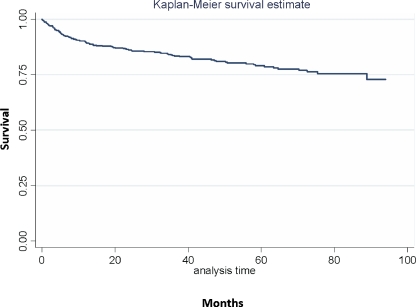
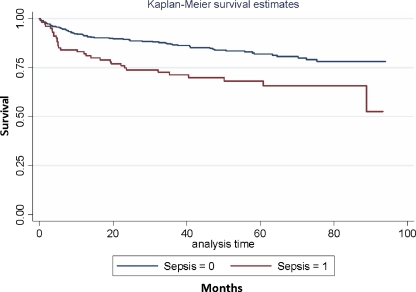
Survivorship
Using reoperation as an endpoint, the mean survival of the index revision for the entire cohort was 86.1% at 30 months, 79.2% at 60 months, and 72.9% at 90 months (Fig. 2). The survival of the index revision for aseptic modes of failure was 88.3% at 30 months, 82% at 60 months, and 78.2% at 90 months. For septic modes of failure the mean survival of index revisions were 73.4% at 30 months, 68% at 60 months, and 52.4% at 90 months (Fig. 3). Using time to event analysis where patients were followed until failure or censorship (due to death or loss of follow-up), patients with septic revision had higher risk of revision failure than subjects who had an aseptic indication for revision. The hazard ratio adjusted for age, sex, and other possible confounders was 2.24 (95% CI 1.31–3.82), where p < 0.01.
Fig. 2.
Kaplan-Meyer survivorship: total cohort
Fig. 3.
Kaplan Meyer survivorship: septic vs. aseptic modes of failure
Time to failure
Of the revisions which had failed, 68 (67%) occurred within the first two years of index revision, while the remaining 34 (33%) occurred more than two years later. The mean time to failure was 21.5 months (range, 0.1–110 months). Table 2 shows the percentage of early and late revision groups for all modes of failure. No statistical significance was found in comparing the mode of failure to the categorical time of failure (early or late group). Failure because of infection and stiffness tended to occur early when compared to other mechanisms (p = 0.04).
Table 2.
Early versus late failures
| Diagnosis | Total | Early revision | Late revision | Mean time to failure (months) | ||
|---|---|---|---|---|---|---|
| Infection | 45 | 32 | 71% | 13 | 29% | 20.4 |
| Stiffness | 23 | 18 | 78% | 5 | 22% | 15.1 |
| Aseptic loosening | 5 | 2 | 40% | 3 | 60% | 49.9 |
| Extensor mechanism problems | 13 | 6 | 46% | 7 | 54% | 30.5 |
| Instability | 3 | 2 | 67% | 1 | 33% | 17.3 |
| Fracture | 6 | 3 | 50% | 3 | 50% | 21.1 |
| Misalignment/malposition | 3 | 1 | 33% | 2 | 67% | 32.4 |
| Hematoma | 4 | 4 | 100% | 0 | 0% | 0.4 |
| Total | 102 | 68 | 67% | 34 | 33% | 21.5 |
Discussion
TKA revision is an effective treatment for most patients with failed primary TKA, evidently with less favourable outcome than primary TKA [8]. In previous series, the average survivorship of TKA revisions has ranged from 58% to 89% at five years [17–23], which is significantly lower than that of primary TKAs [1–6]. The available literature, however, is difficult to interpret due to the fact that most of these studies are different in nature (evaluating different outcome points), the varying time span of the studies, the variation in definition of success and failure between the studies, and most importantly the inclusion of the septic and aseptic failures in the same group for the purpose of determining the survivorship [18].
Studies have attempted to determine the reason for reoperation or re-revision following revision TKA. Goldberg et al. reported instability (three knees), patellar problems (two knees), and infection (four knees) as the main reasons for reoperation following 65 consecutive aseptic revisions [18]. Major reoperations for loosening (8%) and manipulation under anaesthesia (15%) were the most common failure mechanisms in the study by Rand et al. in a series of 54 aseptic revisions [20]. Stuart et al. reported on the reasons for reoperation after 655 revisions, including extensor mechanism or patellar problems (41%), component loosening (22%), deep infection (20%), wound problem (20%), tibiofemoral instability (17%), limited range of motion (8%) and particulate debris synovitis (2%) [23]. Peters et al. reported instability and extensor mechanism problems as the main causes of failure [19].
This study was conceived to determine the mode of failure, time to failure, and the predictors of failure of revision TKA attempting to address some of the shortcomings of the available literature. The findings of our study resembled those of previous studies in some aspects and differed from them in other aspects. The main finding of this study was that infection was the most common cause of failure of revision TKA. This finding is similar to the finding of the study performed by Suarez et al. when infection at 46% was found to be the main cause of failure in 508 patients undergoing revision TKA [24]. We deliberately included revisions performed for infection and aseptic reasons. This study found deep periprosthetic infection (PJI) to be the major reason for reoperation or re-revision, accounting for 44.1% of the failed TKA revisions in this series. Not surprisingly, 58% of these knees (26 of 45) had been revised due to infection of the primary TKA, which may be an indication of persistence of infection or reinfection. The data indicated an overall 25.7% recurrence rate for infection following treatment of infected primary TKAs (26 of 101). Previous studies have shown that the rate of failure following treatment of infected TKAs depends on the treatment strategy. While the failure rate following open debridement and retention of the prosthesis has been reported as 60–80% [25–27], studies have reported a 27% failure rate following one-stage reimplantation and less than 10% failure rate following two-stage reimplantation [28–35]. Our 23% failure rate is comparable with these reported results, considering open debridement and polyethylene exchange with retention of prosthesis was used in some of our patients.
The outcomes of treatment methods for infected TKAs have been evaluated by their ability to eradicate infection, which is obviously the most important objective of different treatment options. However, as our data has shown, 22.6% of patients with failure following septic revision failed as a result of other mechanisms like periprosthetic fracture, extensor mechanism problem, and stiffness even in the presence of successful eradication of infection.
Reoperation rates for deep infection after revision TKA in patients with no history of infection have ranged from 2 to 4.5% in different series [18, 23, 36]. Sierra et al. compared the cumulative risk of reoperation for deep infection after index aseptic revision in three consecutive decades and found a trend toward a higher reoperation rate for infection in patients revised in more recent decades. They also concluded that the rate of reoperation for infection in patients who had a revision TKA was approximately two times higher than that reported for patients having had a primary TKA. Infection rates after primary TKAs have been reported to be less than 1% in high volume centres to 2% overall [15, 37–41]. Our data showed a 4.4% reoperation rate for deep infection in those patients with no history of infection. Thus, the risk of reoperation for infection after aseptic revision is four times greater compared to the risk after primary TKA, which reveals the significant risk of infection following revision for aseptic reasons. This increased risk is often attributed to a combination of the poorly vascularised tissue commonly encountered after multiple operations, the increased operative time for revision surgery, prior wound healing, and the increased age and a compromised metabolic state of the patient population [42, 43]. Alternatively, a possible explanation is the fact that our conventional diagnostic modalities for diagnosis of infection are not 100% sensitive, which increases the probability that some of these so-called aseptic cases were actually infected TKAs that escaped detection by usual diagnostic tests. The indolent infection could be hidden in the context of other modes of failure.
Several limitations of this study must be acknowledged. While the data revealed a reliable profile of various mechanisms leading to early failure of TKA revisions, appropriate verification of the mechanisms of late failure after revision TKA demanded longer follow-up. The other limitation of this study is the fact that we did not take into account functional failure, which includes patients with low functional and clinical scores for the operated knee who did not have any further intervention requiring some kind of anaesthesia. Additionally, different types of surgery for revision of infected TKAs were not considered in separate categories, so the overall success rate in the treatment of infection includes the less successful irrigation and debridement and polyethylene exchange strategy as well as the more predictable two-stage reimplantation.
The annually increasing number of TKA revisions and the high economic burden of the revision procedure necessitate improvement of the outcome of this procedure through recognition, modification, and resolution of the most significant contributory factors. Infection remains the most important factor compromising the outcome of revision TKA. Hence, further improvement in prevention and management of this dreaded complication is warranted.
Acknowledgments
Conflict of interest The authors do not have any conflicts of interest with regard to this research.
References
- 1.Weir DJ, Moran CG, Pinder IM. Kinematic condylar total knee arthroplasty. 14-year survivorship analysis of 208 consecutive cases. J Bone Joint Surg Br. 1996;78:907–911. doi: 10.1302/0301-620X78B6.6678. [DOI] [PubMed] [Google Scholar]
- 2.Emmerson KP, Moran CG, Pinder IM. Survivorship analysis of the kinematic stabilizer total knee replacement: a 10- to 14-year follow-up. J Bone Joint Surg Br. 1996;78:441–445. [PubMed] [Google Scholar]
- 3.Font-Rodriguez DE, Scuderi GR, Insall JN (1997) Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res 345:79–86 [PubMed]
- 4.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish knee arthroplasty register 1975–1997: an update with special emphasis on 41,223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 5.Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB (1994) Long-term survival analysis of a posterior cruciate-retaining total condylar total knee arthroplasty. Clin Orthop Relat Res 309:136–145 [PubMed]
- 6.Stern SH, Insall JN. Posterior stabilized prosthesis. Results after follow-up of nine to twelve years. J Bone Joint Surg Am. 1992;74:980–986. [PubMed] [Google Scholar]
- 7.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B, Cross WW 3rd, MacDonald RM, Rutks I (2003) Total knee replacement. Evid Rep Technol Assess (Summ) 86:1–8 [PMC free article] [PubMed]
- 8.Saleh KJ, Dykes DC, Tweedie RL, Mohamed K, Ravichandran A, Saleh RM, Gioe TJ, Heck DA. Functional outcome after total knee arthroplasty revision: a meta-analysis. J Arthroplasty. 2002;17:967–977. doi: 10.1054/arth.2002.35823. [DOI] [PubMed] [Google Scholar]
- 9.Saleh KJ, Rand JA, McQueen DA. Current status of revision total knee arthroplasty: how do we assess results? J Bone Joint Surg Am. 2003;85-A(Suppl 1):S18–S20. doi: 10.2106/00004623-200300001-00005. [DOI] [PubMed] [Google Scholar]
- 10.Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ. Current etiologies and modes of failure in total knee arthroplasty revision. Clin Orthop Relat Res. 2006;446:45–50. doi: 10.1097/01.blo.0000214421.21712.62. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 12.Rorabeck CH, Murray P. Cost effectiveness of revision total knee replacement. Instr Course Lect. 1997;46:237–240. [PubMed] [Google Scholar]
- 13.Healy WL, Finn D. The hospital cost and the cost of the implant for total knee arthroplasty. A comparison between 1983 and 1991 for one hospital. J Bone Joint Surg Am. 1994;76:801–806. doi: 10.2106/00004623-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Lavernia CJ, Guzman JF, Gachupin-Garcia A (1997) Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res 345:134–139 [PubMed]
- 15.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13 [DOI] [PubMed]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Friedman RJ, Hirst P, Poss R, Kelley K, Sledge CB (1990) Results of revision total knee arthroplasty performed for aseptic loosening. Clin Orthop Relat Res 255:235–241 [PubMed]
- 18.Goldberg VM, Figgie MP, Figgie HE 3rd, Sobel M (1988) The results of revision total knee arthroplasty. Clin Orthop Relat Res 226:86–92 [PubMed]
- 19.Peters CL, Hennessey R, Barden RM, Galante JO, Rosenberg AG. Revision total knee arthroplasty with a cemented posterior-stabilized or constrained condylar prosthesis: a minimum 3-year and average 5-year follow-up study. J Arthroplasty. 1997;12:896–903. doi: 10.1016/S0883-5403(97)90159-5. [DOI] [PubMed] [Google Scholar]
- 20.Rand JA, Bryan RS. Results of revision total knee arthroplasties using condylar prostheses. A review of fifty knees. J Bone Joint Surg Am. 1988;70:738–745. [PubMed] [Google Scholar]
- 21.Sheng PY, Konttinen L, Lehto M, Ogino D, Jamsen E, Nevalainen J, Pajamaki J, Halonen P, Konttinen YT. Revision total knee arthroplasty: 1990 through 2002. A review of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2006;88:1425–1430. doi: 10.2106/JBJS.E.00737. [DOI] [PubMed] [Google Scholar]
- 22.Sierra RJ, Cooney WPt, Pagnano MW, Trousdale RT, Rand JA (2004) Reoperations after 3200 revision TKAs: rates, etiology, and lessons learned. Clin Orthop Relat Res 425:200–206 [PubMed]
- 23.Stuart MJ, Larson JE, Morrey BF (1993) Reoperation after condylar revision total knee arthroplasty. Clin Orthop Relat Res 286:168–173 [PubMed]
- 24.Suarez J, Griffin W, Springer B, Fehring T, Mason JB, Odum S. Why do revision knee arthroplasties fail? J Arthroplasty. 2008;23:99–103. doi: 10.1016/j.arth.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Hartman MB, Fehring TK, Jordan L, Norton HJ (1991) Periprosthetic knee sepsis. The role of irrigation and debridement. Clin Orthop Relat Res 273:113–118 [PubMed]
- 26.Schoifet SD, Morrey BF. Treatment of infection after total knee arthroplasty by debridement with retention of the components. J Bone Joint Surg Am. 1990;72:1383–1390. [PubMed] [Google Scholar]
- 27.Tattevin P, Cremieux AC, Pottier P, Huten D, Carbon C. Prosthetic joint infection: when can prosthesis salvage be considered? Clin Infect Dis. 1999;29:292–295. doi: 10.1086/520202. [DOI] [PubMed] [Google Scholar]
- 28.Zywiel MG, Johnson AJ, Stroh DA, Martin J, Marker DR, Mont MA. Prophylactic oral antibiotics reduce reinfection rates following two-stage revision total knee arthroplasty. Int Orthop. 2010 doi: 10.1007/s00264-010-0992-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bengtson S, Knutson K. The infected knee arthroplasty. A 6-year follow-up of 357 cases. Acta Orthop Scand. 1991;62:301–311. doi: 10.3109/17453679108994458. [DOI] [PubMed] [Google Scholar]
- 30.Booth RE Jr., Lotke PA (1989) The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop Relat Res 248:57–60 [PubMed]
- 31.Goldman RT, Scuderi GR, Insall JN (1996) 2-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res 331:118–124 [DOI] [PubMed]
- 32.Haleem AA, Berry DJ, Hanssen AD (2004) Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res 428:35–39 [DOI] [PubMed]
- 33.Insall JN, Thompson FM, Brause BD. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983;65:1087–1098. [PubMed] [Google Scholar]
- 34.Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81:1434–1445. doi: 10.2106/00004623-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Park SJ, Song EK, Seon JK, Yoon TR, Park GH. Comparison of static and mobile antibiotic-impregnated cement spacers for the treatment of infected total knee arthroplasty. Int Orthop. 2009 doi: 10.1007/s00264-009-0907-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jacobs MA, Hungerford DS, Krackow KA, Lennox DW (1988) Revision total knee arthroplasty for aseptic failure. Clin Orthop Relat Res 226:78–85 [PubMed]
- 37.Grogan TJ, Dorey F, Rollins J, Amstutz HC. Deep sepsis following total knee arthroplasty. Ten-year experience at the University of California at Los Angeles Medical Center. J Bone Joint Surg Am. 1986;68:226–234. [PubMed] [Google Scholar]
- 38.Johnson DP, Bannister GC. The outcome of infected arthroplasty of the knee. J Bone Joint Surg Br. 1986;68:289–291. doi: 10.1302/0301-620X.68B2.3958017. [DOI] [PubMed] [Google Scholar]
- 39.Rand JA, Bryan RS, Morrey BF, Westholm F (1986) Management of infected total knee arthroplasty. Clin Orthop Relat Res 205:75–85 [PubMed]
- 40.Windsor RE. Management of total knee arthroplasty infection. Orthop Clin North Am. 1991;22:531–538. [PubMed] [Google Scholar]
- 41.Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR. The microbiology of the infected knee arthroplasty. Int Orthop. 2010;34:505–510. doi: 10.1007/s00264-009-0797-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hanssen AD, Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999;48:111–122. [PubMed] [Google Scholar]
- 43.Garvin KL, Cordero GX. Infected total knee arthroplasty: diagnosis and treatment. Instr Course Lect. 2008;57:305–315. [PubMed] [Google Scholar]