Abstract
The objective of this work was firstly to evaluate the long-term results of medial opening wedge high tibial osteotomy (HTO) and secondly to evaluate the tolerance and integration of a Biosorb® wedge (β Tricalcium Phosphate, SBM Company, Lourdes, France). The series consisted of 124 knees in 110 patients, 74 men and 36 women, with mean age of 53.23±10.68 years (range 32–74) and treated between June 1995 and November 2000 for medial compartment knee osteoarthritis by the senior author. The mean preoperative Lysholm and Tegner functional score was 65.44±13.32 (range 27–80) and the preoperative HKA angle was 172.51°±3.8° (range 162–179°). According to the modified Ahlbäck classification there were 27 stage I, 42 stage II, 44 stage III and 11 stage IV knees. All patients were reviewed clinically and radiologically with a mean follow-up of 10.39±1.98 years (range 8–14 years). Immediate postoperative complications consisted of nine undisplaced lateral tibial plateau fractures of no clinical significance, two deep vein thromboses and three pulmonary emboli which resolved with appropriate treatment. At a later stage, there were seven delayed unions without development of pseudarthrosis, and three screw breakages when the AO T-plate was used, leading to a secondary angulation in one case, requiring revision by femoral osteotomy. Postoperative mean weightbearing HKA angle was 182°±1.8° (range 178–186°) and 73.4% of axes were 184°±2°. Fifteen knees (12.1%) underwent total knee arthroplasty (TKA) after a mean delay of 8.87±3.04 years and were excluded from the final analysis. Concerning the long-term results (n = 107 knees), the mean Lysholm-Tegner score was 88±12.7 points (51–100) and the KOOS score was 86±14.6 points (25–100) with 94 patients satisfied or very satisfied (87.85%). In terms of the HTO survivorship curve, with failure consisting of revision to TKA or another operation, survival was 88.8% at five years and 74% at ten years. Concerning Biosorb®, this was completely integrated in 100% of cases and there was complete resorption in 12.1% of cases and greater than 50% resorption in 52.3% of cases.
Introduction
Medial opening wedge high tibial osteotomy was first described in the 1950s [15, 17] for the surgical treatment of osteoarthritis of the knee with varus deformity. Since then, several publications have shown consistently pleasing results [1, 2, 6, 8, 11, 13, 16, 19, 22, 26, 31]. Lateral closing wedge osteotomy, popularised by Coventry in the Anglo-American literature [5] and by Judet in France [17] was the technique of choice for many surgeons. However, although this technique seems easy to perform, it carries with it a number of issues such as the need to perform a fibula osteotomy, the risk of compartment syndrome or injury to the common peroneal nerve, malunion of the proximal tibia and the potential of inaccurate bony resection resulting in a failure to achieve the preoperative objective of correcting the deformity with acceptable precision [35]. The opening wedge medial osteotomy, described in France by Debeyre and Artigou in 1972 [7], avoids the majority of the issues associated with closing wedge osteotomy. However, its popularity was limited for a long time by the need to fill the osteotomy site with bone graft harvested from the iliac crest with its associated morbidity. To address this problem, Goutallier et al. [10] proposed a wedge of bone cement to fill the osteotomy, but this modification of the technique has not gained the support of many surgeons. In the 1990s, plates with integrated metal wedges [9] and biomaterials designed to fill the osteotomy site became available. We performed lateral closing wedge osteotomies for many years but then started to use Biosorb® wedges (β tricalcium phosphate, SBM Company, Lourdes, France) in 1993, initially intermittently, then routinely from 1995. To date, in our department, we have used these wedges in nearly 600 cases with much success.
Following this experience, the objective of this work was firstly to evaluate the long-term results of medial opening wedge high tibial osteotomy (HTO) and secondly to evaluate the tolerance, integration and resorption of Biosorb® wedges.
Material and methods
The series consisted initially of 132 knees in 118 patients operated upon by a single surgeon (DS) between June 1995 and November 2000. Eight knees were excluded (two died and six were lost to follow-up) such that our series was reduced to 124 knees (110 patients). It consisted of 74 men (87 knees) and 36 women (37 knees) with mean age of 53.23±10.68 years (range 32–74). We operated on 57 right knees and 67 left knees. Mean body mass index (BMI) was 27.1±4.37 (range 19.47–44.44).
For functional assessment, we used the Lysholm–Tegner score [34] to evaluate patients, both preoperatively and postoperatively. We felt this scoring system was better adapted than the IKS score usually used to evaluate surgical treatment for knee osteoarthritis. Preoperative mean score was 65.44±13.32 points (range 27–80).
For radiological evaluation, we routinely used AP and lateral standing views, a Schuss view (single leg flexed standing view), a patella skyline view and weight-bearing long-leg alignment views. We measured the angle of axial deformity (HKA angle) and evaluated the degree of arthritis according to the modified Ahlbäck staging system [29]. We operated on 27 stage I knees (22%), 42 stage II (34%), 44 stage III (35%) and 11 stage IV knees (9%). The mean HKA angle using the Ramadier protocol [25] was 172.51°±3.8° (range 162°–179°).
The Biosorb® wedges used in this series are composed of beta tricalcium phosphate with purity of greater than 95%, porosity of 30% total volume and with pores of diameter between 140 and 400 microns. The load to failure in compression is 80 MPa. They are wedge shaped (Fig. 1) with a base width ranging from 6 to 17 mm.
Fig. 1.
Biosorb® wedges
With regard to operative technique, the objective was to obtain an HKA angle of 184°±2°. To attain this goal, we routinely simulated the medial opening with tracing paper superimposed over long-leg alignment radiographs (100% magnification was used at the time of the study), which permitted us to estimate the size of the wedge required. In addition, we were able to monitor the correction intraoperatively having identified the position of the centre of the femoral head using an image intensifier and marking it by placing an adhesive ECG electrode on the overlying skin. This allowed us to control the axis relatively easily, by holding a large suture proximally over the electrode palpable through the drapes, stretching down across the knee to the distal end overlying the centre of the ankle joint. In general, we used a wedge which corresponded to the degree of opening required; for example, a wedge of base 6 mm to create 6° opening or a 10 mm wedge to open 10°. The technique of the opening osteotomy itself is still the same as we use today and we have described this in detail previously [28, 29]. In addition to the Biosorb® wedge, we used a two- or three-hole AO T-shaped plate and screws to stabilise the osteotomy.
All patients were contacted by telephone and asked to complete a questionnaire to establish a postoperative Lysholm–Tegner score and a KOOS score [27]. In addition, they all had AP and lateral knee radiographs to evaluate the integration and resorption of the Biosorb® wedge. We considered the wedge to be completely integrated when there was no lucency between the wedge and the bone and the impression of bone penetration into the wedge (Fig. 2). With regard to its resorption, we tried to quantify it by comparing the state of the wedge in comparison to the immediate postoperative film. Thus, we have been able to define six stages of resorption: stage 1, with less than 20% resorption; stage 2, with between 20 and 40% resorption; stage 3, with between 40 and 60% resorption; stage 4, with between 60 and 80% resorption; stage 5, with between 80 and 100% resorption; and stage 6, for 100% resorption.
Fig. 2.
Integration and resorption of the Biosorb® (D + 7 years)
For statistical analysis, we used the chi-squared test or Fisher’s exact test to compare the qualitative variables and the Mann-Whitney test to compare quantitative variables. The level of significance (p value) was 0.10. Statistical analysis was performed using SPSS (version 13.0; SPSS Inc., Chicago, IL, USA) including analysis of long-term survivorship. Univariate survivorship analysis was done according to the Kaplan-Meier method. We considered all surgical revisions either by total knee arthroplasty (TKA) or another operation (e.g. new osteotomy) as failures.
Results
In terms of complications, per-operatively there were nine lateral tibial plateau fractures without impact on either the postoperative rehabilitation or final result. We had no infection in this series. Two patients developed postoperative deep vein thrombosis (DVT) and three patients, a pulmonary embolism (PE). These complications resolved after appropriate treatment with anticoagulation. Three other patients had failure of fixation (screw breakage) following premature weight-bearing. One of them had a secondary loss of angulation (high BMI) and required revision two years later with a new osteotomy at the femoral level to correct the deformity. All osteotomies united completely. However, seven knees had delayed union which required deferring weight-bearing for a few weeks. Full weight-bearing was allowed, in general, on or around the 60th postoperative day (mean delay of 8.3±2.2 weeks; range 3–17).
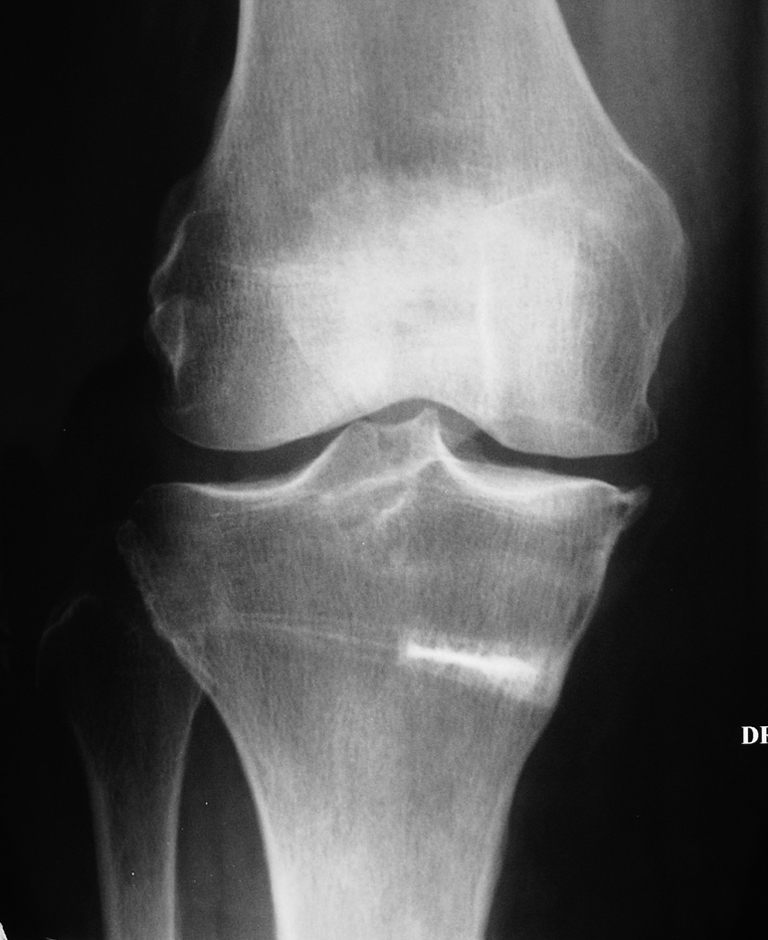
Fifteen knees (12.9%) were revised by total knee arthroplasty (TKA) at a mean of 8.87±3.04 years postoperatively. This secondary intervention was uneventful and the wedge did not hinder the implantation of the prosthesis (Fig. 3).
Fig. 3.
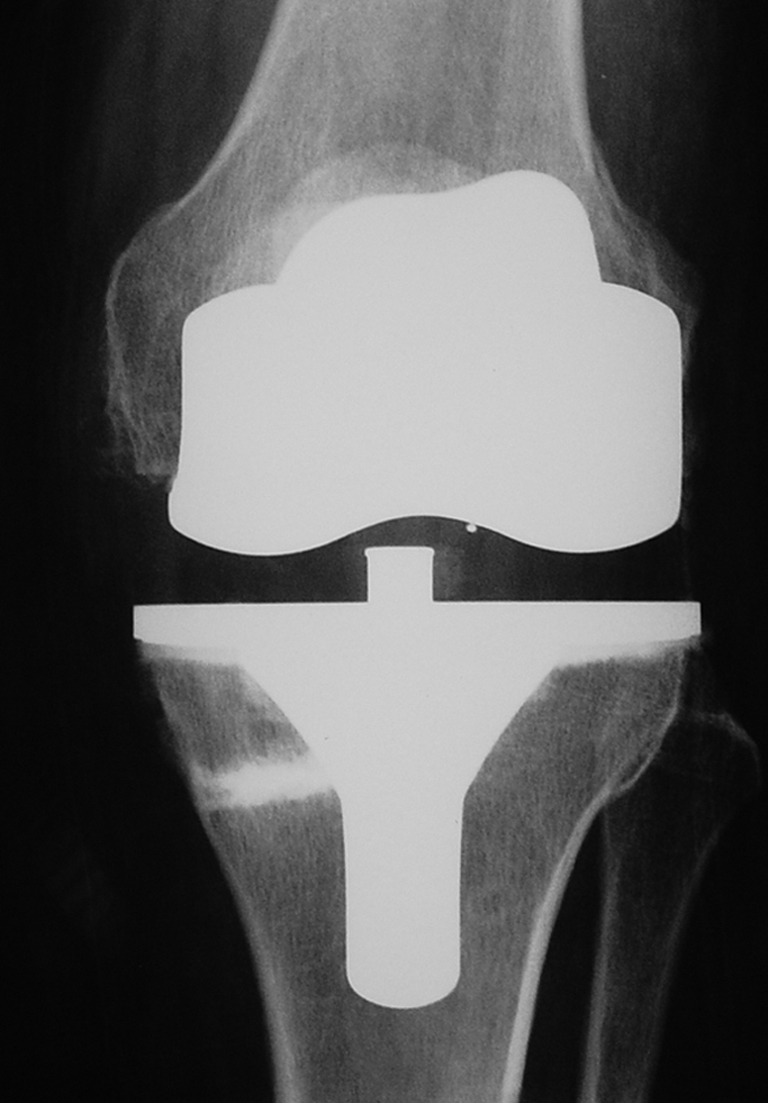
Total knee arthroplasty (TKA) after failure of OWHTO using Biosorb®
In terms of postoperative radiological results at three months, the mean HKA angle was 182.03°±1.8° (range 178°–186°) such that the objective of 184°±2° was achieved in 73.4% of cases.
At mean follow-up of 10.39±1.98 years (range 8–14 years), the mean KOOS score of unrevised patients (n = 107 knees) was 86±14.6 points (range 25–100) and the Lysholm–Tegner score was 88±12.7 points (range 51–100). Thus, 94 patients were either very satisfied or satisfied with the intervention (87.85%).
As for the fate of the Biosorb® wedge, its tolerance and integration was perfect in all cases. The resorption was complete in 12.1% of cases and less than 20% in 23.4% of cases (Table 1).
Table 1.
Stages of resorption of the Biosorb®
| Stage of resorption | Number of cases (N = 107) | Percentage |
|---|---|---|
| Stage 1 | 25 | 23.4% |
| Stage 2 | 13 | 12.2% |
| Stage 3 | 28 | 24.3% |
| Stage 4 | 20 | 20.5% |
| Stage 5 | 8 | 7.5% |
| Stage 6 | 13 | 12.2% |
The survivorship curve, with surgical revision as failure, demonstrated 88.6% survival at five years and 74% survival at ten years.
Discussion
Medial opening wedge high tibial osteotomy (HTO) represents the gold standard treatment for medial compartment osteoarthritis of the knee in a young person. The alternative is arthroplasty, most notably unicompartmental knee arthroplasty (UKA). In our opinion, the choice between HTO and UKA is not competitive but rather complementary. In effect, for the same stage of arthritis, we would offer an HTO to patients less than 65 years old, while offering, with some exceptions, a UKA in older, more sedentary patients. Our ten year results are inferior to some [2, 8, 19], similar to some [1], or better than other series published in the literature [6, 11, 13, 14, 16, 22, 24, 26]. The satisfactory outcome rate varies from 45% to 95% [19], which poses a problem for outcome analysis. In practice, it is difficult to compare different series, firstly because they are not matched, secondly because the evaluation criteria are not the same and finally because the principal outcome measure is level of pain which is very variable on both an individual and cultural level. On the other hand, the five-year results in all the series describe a satisfaction rate of around 90% regardless of evaluation method used, which corroborates our results (88.6%).
We have used surgical revision as the criterion of failure for osteotomy as in the evaluation of TKA. This end-point is disputable, as certain patients will have started to suffer with their knee again without considering further intervention. With this in mind, the postoperative Lysholm–Tegner and KOOS scores used to evaluate patients who had not undergone revision are certainly impressive (86±14.6 points [range 25–100] for the KOOS, and 88±12.7 points [range 51–100] for the Lysholm–Tegner) and put the disputable nature of this choice of end-point into perspective. We have used these scores previously, as they are much more sensitive than the IKS score in the evaluation of moderate osteoarthritis (in the absence of stiffness, instability, or major contractures, etc.) as is the case when one considers HTO. As is to be expected, our study, despite showing very encouraging ten-year results, also confirms, as with the majority of other studies, a worsening outcome with time.
With regard to factors likely to influence the longevity of the osteotomy, we recognise the importance of over-correction rather than under-correction as is described in the literature [11, 16, 31]. Patients who underwent revision were statistically significantly more likely to have an HKA angle less than 182° than those not revised (p < 0.001). However, excessive hypercorrection advocated by certain authors [8, 31], even if contributing to a good result, is not well tolerated in our present society, attributable mainly to the non-aesthetic deformity it produces and also the malunion that it leads to at the proximal tibia [30]. We think that an HKA angle of 186° is the maximum that one should tolerate and this is an argument for the routine use of surgical navigation systems [28–30] to facilitate achieving the preoperative goal of an HKA angle of 184°±2°. We also recognise the importance of age in predicting longevity of the osteotomy. This notion was previously raised by Flecher et al. [8]. Essentially, the older the patient is at the time of the osteotomy, the more likely the revision will be premature (p < 0.001). However, it is important to put this into perspective, as the mean delay to revision in this series was 8.87±3.04 years, which would justify an osteotomy in a very active patient up to the age of 65 at least. On the other hand, we have not found a correlation between the stage of osteoarthritis and the longevity of the osteotomy. This is contrary to the work of Jenny et al. [16], which showed that the less developed the arthritis, the more durable the osteotomy. This statement is certainly logical and has previously influenced our practice. It would probably require a much larger series with more failures to be able to demonstrate a difference.
In this series we had 7.25% fractures of the lateral plateau per-operatively without any consequences in terms of union and stability of the osteosynthesis. This fracture can occur when the osteotomy line is not extended up to the lateral edge of the tibia. In this case, when one tries to open the line with two Pauwel’s chisels the fracture can occur. Usually, the risk is less when the surgeon is well trained (less than 2% in the current experience of the senior author based on 350 cases more).
As for the use of a Biosorb® wedge to fill the osteotomy site, we have never regretted this choice, as firstly the tolerance has been perfect in all cases, and secondly the bony integration has not posed a problem and finally resorption has been greater than 50% in more than 50% of cases at ten-year mean follow-up. Similarly, performing a TKA has never been a problem either for performing the tibial cut or in the preparation for the stem of the tibial component (Fig. 3), as has been equally described by Kraal et al [19]. This good tolerance has also been underlined by other authors [3, 12, 20, 21] who have used either a plate and screws, or staples. Some authors use hydroxyapatite wedges [18], porous alumina ceramic wedges [4] or acrylic cement wedges [10]. In principle, if hydroxyapatite wedges do not pose a problem for revision to TKA (or new osteotomy), then the same should apply for alumina ceramic and acrylic cement wedges. Other authors use neither bone substitutes nor bone graft and put their confidence in a relatively large, rigid locking plate [32, 33] or a plate with an integrated metal wedge built in [9, 23]. These alternatives could be acceptable, provided they offer the same possibilities as our technique, notably, a minimally invasive incision (5–6 centimetres), immediate rehabilitation, full weight-bearing between 30 and 45 days, absence of collapse or pseudarthrosis and no problems following metalwork removal at the request of the patient or following symptoms (pain, infective problems, intolerance, etc). This does not seems to be the case with some integrated metal wedge plates as shown by Nelissen et al. [23].
In this series, we used AO T-plates with non-locking screws, initially two-hole plates and subsequently three-hole plates. We had three screw breakages, which in one case (2 hole plate) was associated with a loss of correction following premature weight-bearing in an obese patient. Since 2002, we use a C-shaped relatively rigid locking plate, which not only makes the construction more rigid, but also permits a very short incision, similar to that required when using staples, and allows an earlier return to full weight-bearing without collapse (between 30 and 45 days).
Conclusion
Medial opening wedge high tibial osteotomy using a Biosorb® wedge together with plate and screws is an excellent alternative to iliac crest bone graft. Union of the osteotomy occurs without problem, tolerance and integration of the bone substitute is excellent and revision to total knee arthroplasty is straight-forward. The long-term results are entirely satisfactory (74% good results at ten years post-surgery) and provided the chosen operative technique is reliable and reproducible in all hands, it should be extensively used as treatment of choice for medial compartment knee osteoarthritis in adults less than 65 years old.
References
- 1.Aglietti P, Buzzi R, Vena LM, Baldini A, Mondaini A. High tibial valgus osteotomy for medial gonarthrosis : a 10 to 21-year study. J Knee Surg. 2003;16:21–26. [PubMed] [Google Scholar]
- 2.Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H. The long-term outcome of high tibial osteotomy. A ten to 20-year follow up. J Bone Joint Surg Br. 2008;90:592–596. doi: 10.1302/0301-620X.90B5.20386. [DOI] [PubMed] [Google Scholar]
- 3.Bonnevialle P, Abid A, Mansat P, Verhaeghe L, Clément D, Mansat M. Ostéotomie tibiale de valgisation par addition médiale d’un coin de phosphate tricalcique. Rev Chir Orthop. 2002;88:486–492. [PubMed] [Google Scholar]
- 4.Bove JC. Utilisation d’une cale en céramique d’alumine poreuse dans l’ostéotomie tibiale de valgisation par ouverture interne. Rev Chir Orthop. 2002;88:480–485. [PubMed] [Google Scholar]
- 5.Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg Am. 1965;47:984–990. [PubMed] [Google Scholar]
- 6.Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical long-term study of eighty-seven cases. J Bone Joint Surg Am. 1993;75:196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Debeyre J, Artigou JM. Résultats à distance de 260 ostétomies tibiales pour déviation frontale en varus du genou. Rev Chir Orthop. 1972;58:335–337. [PubMed] [Google Scholar]
- 8.Flecher X, Parratte S, Aubaniac JM, Argenson JN. A 12–28-year follow-up study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006;452:91–96. doi: 10.1097/01.blo.0000229362.12244.f6. [DOI] [PubMed] [Google Scholar]
- 9.Franco V, Cerullo G, Cipolla M, Gianni E, Puddu GC. Open wedge high tibial osteotomy. Tech Knee Surg. 2002;11:43–53. doi: 10.1097/00132588-200209000-00006. [DOI] [Google Scholar]
- 10.Goutallier D, Juliéron A, Hernigou Ph. La cale de ciment remplaçant les greffons iliaques dans les ostéotomies tibiales d’addition interne. Rev Chir Orthop. 1992;78:138–144. [PubMed] [Google Scholar]
- 11.Hernigou Ph, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity : a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–354. [PubMed] [Google Scholar]
- 12.Hernigou Ph, Roussignol X, Flouzat-Lachaniette CH, Filippini P, Guissou I, Poignard A. Opening wedge tibial osteotomy for large varus deformity with Ceraver™ resorbable beta tricalcium phosphate wedges. Int Orthop. 2010;34:191–199. doi: 10.1007/s00264-009-0875-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holden DL, James SL, Larson RL, Slocum DB. Proximal tibial osteotomy in patients who are fifty years old or less. J Bone Joint Surg Am. 1988;70:977–982. [PubMed] [Google Scholar]
- 14.Insall JN, Douglas MJ, Msika C. High tibial osteotomy for varus gonarthrosis. J Bone Joint Surg Am. 1984;66:1040–1048. [PubMed] [Google Scholar]
- 15.Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43:746–751. doi: 10.1302/0301-620X.43B4.746. [DOI] [PubMed] [Google Scholar]
- 16.Jenny JY, Tavan A, Jenny G, Kehr P. Taux de survie à long terme des ostéotomies tibiales de valgisation pour gonarthrose. Rev Chir Orthop. 1998;84:350–357. [PubMed] [Google Scholar]
- 17.Judet R, Dupuis JF, Honnard F, et al. Désaxations et arthroses du genou. Le genu varum de l’adulte. Indications thérapeutiques, résultats. Rev Chir Orthop. 1964;13:1–28. [Google Scholar]
- 18.Koshino T, Murase T, Saito T. Medial opening-wedge high tibial osteotomy with use of porus hydroxyapatite to treat medial compartment osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85:78–85. doi: 10.1302/0301-620X.85B1.12468. [DOI] [PubMed] [Google Scholar]
- 19.Koshino T, Yoshida T, Ara Y, Saito I, Saito T. Fifteen to twenty-eight years follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee. 2004;11:439–444. doi: 10.1016/j.knee.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Kraal T, Mullender M, Bruine JH, Reinhard R, Gast A, Kuik DJ, Royen BJ. Resorbability of rigid beta tricalcium phosphate wedges in open-wedge high tibial osteotomy : a retrospective radiological study. Knee. 2008;15:201–205. doi: 10.1016/j.knee.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Lascard T, Favard L, Burdin P, Traoré O. Utilisation du phosphate tricalcique dans les ostéotomies tibiales de valgisation par addition interne. Ann Orthop Ouest. 1998;30:137–141. [Google Scholar]
- 22.Lootvoet L, Massinon A, Rossillon R, Himmer O, Lambert K, Ghosez JP. Ostéotomie tibiale haute de valgisation pour gonarthrose sur genu varum: à propos d’une série de 193 cas revus après 6 à 10 ans de recul. Rev Chir Orthop. 1993;79:375–384. [PubMed] [Google Scholar]
- 23.Nelissen EM, Langelaan EJ, Nelissen RGHH. Stability of medial opening wedge high tibial osteotomy: a failure analysis. Int Orthop. 2010;34:217–223. doi: 10.1007/s00264-009-0723-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papachristou G, Plessas S, Sourlas J, Levidiotis C, Chronopoulos E, Papachristou C. Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int Orthop. 2006;30:406–408. doi: 10.1007/s00264-006-0098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramadier JO, Buard JE, Lortat-Jacob A, et al. Mesure radiologique des déformations frontales du genou. Procédé du profil vrai radiologique. Rev Chir Orthop. 1982;68:75–78. [PubMed] [Google Scholar]
- 26.Rinonapoli E, Mancini GB, Corvaglia A, et al. Tibial osteotomy for varus gonarthrosis. A 0 to 21-year follow-up study. Clin Orthop. 1998;353:185–193. doi: 10.1097/00003086-199808000-00021. [DOI] [PubMed] [Google Scholar]
- 27.Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee Injury and Osteoarthritis Outcome Score (KOOS): validation of a Swedish version. Scand J Med Sci Sports. 1998;8:439–448. doi: 10.1111/j.1600-0838.1998.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 28.Saragaglia D, Pradel Ph, Picard F (2004) L’ostéotomie de valgisation assistée par ordinateur dans le genu varum arthrosique: résultats radiologiques d’une étude cas-témoin de 56 cas. E-mémoires de l’Académie Nationale de Chirurgie 3:21–25. Available at http://www.bium.univ-paris5.fr/acad-chirurgie
- 29.Saragaglia D, Roberts J. Navigated osteotomies around the knee in 170 patients with osteoarthritis secondary to genu varum. Orthopaedics. 2005;28(suppl 10):1269–1274. doi: 10.3928/0147-7447-20051002-13. [DOI] [PubMed] [Google Scholar]
- 30.Saragaglia D, Mercier N, Colle PE. Computer-assisted osteotomies for genu varum deformity: which osteotomy for which varus? Int Orthop. 2010;34:185–190. doi: 10.1007/s00264-009-0757-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty two years. J Bone Joint Surg Am 469–474 [PubMed]
- 32.Staubli AE, Simoni C, Babst R, Lobenhoffer P. Tomofix a new LCP-concept for open wedge osteotomy of the medial proximal tibia: early results in 92 cases. Injury. 2003;34(suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 33.Staubli AE, Jacob HAC. Evolution of open-wedge high-tibial osteotomy : experience with a special angular stable device for internal fixation without interposition material. Int Orthop. 2010;34:167–172. doi: 10.1007/s00264-009-0902-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tegner Y, Lysholm J, Lysholm M, Gillquist J. A performance test to monitor rehabilitation and evaluate anterior cruciate ligament injuries. Am J Sports Med. 1986;14:156–159. doi: 10.1177/036354658601400212. [DOI] [PubMed] [Google Scholar]
- 35.Tunggal JAW, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34:255–261. doi: 10.1007/s00264-009-0819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]



