Abstract
Purpose
The purpose of this study was to assess, in anterior cruciate ligament (ACL)-injured and -uninjured population, tibial plateau anatomic variables [medial and lateral tibial plateau slopes (MTPS and LTPS) and medial tibial plateau depth (MTPD)] on conventional magnetic resonance imaging (MRI) using a novel combined method and to determine whether these variables are risk factors for ACL injury.
Methods
Seventy-three isolated ACL-injury patients (20 women and 53 men) were compared with 51 control group patients (19 women and 32 men).
Results
The combined method had very high interrater and intrarater reliability compared with previously described methods. LTPS was significantly steeper in the overall injured group and injured men compared with the control group, with odds ratio (OR) of 3.031 and 5.89, respectively. Women with ACL injury had significantly shallower MTPD than uninjured women, with OR of 4.13.
Conclusions
We conclude that the new combined method is accurate and reproducible for assessing the tibial plateau anatomy. Women with shallower MTPD and men with steeper LTPS are at higher risk of sustaining ACL injury. Overall, steeper LTPS is a significant risk factor for sustaining ACL injury.
Introduction
Anterior cruciate ligament (ACL) injury is a major problem worldwide and is more common among people involved in high-impact sports activities and in women. Osteoarthritis prevalence following ACL injury is as high as 80% [1], and most young patients suffers from early-onset osteoarthritis with associated knee pain and reduced quality of life between 30 and 50 years of age. Identifying risk factors for sustaining an ACL injury or a contralateral ACL injury has been the focus of many recent studies. Several risk factors have been proposed, both internal (anatomical, hormonal, neuromuscular, and familial) and external (type of sports, footwear, and environment) [2–4]. Among anatomical risk factors, most studies have been conducted on the size of intercondylar notch [5–8], but recently, posterior tibial slope (PTS) has also been identified as an important risk factor [9–19]. Tibial plateau slopes, medial plateau (MTPS) and lateral plateau (LTPS), independently are important determinants of knee biomechanics. Many reports note increased tibial anterior translation in the knee with greater PTS [9], resulting in increased joint contact force, specifically its anterior shear component, leading to substantially increased strain on the ACL [10–12]. Lately, shallower medial tibial plateau depth (MTPD) has also been recognized as a risk factor [13]. Together, these tibial plateau anatomic variables are gaining more attention, and magnetic resonance imaging (MRI) has become the study of choice for their measurement. Our study further contributes to the understanding of these variables and their association with ACL injury and describes a new method of measurement, with verification of methods previously mentioned in the literature.
We hypothesized that: (1) MTPS and LTPS would be steeper in the ACL-injured group than in the control group, (2) MTPS and LTPS would be steeper in both men and women patients with ACL injury compared with their uninjured counterparts, and (3) MTPD would be shallower in ACL-injury patients, in both men and women compared with uninjured men and women.
Methods
We performed a case control study to compare MTPS, LTPS, and MTPD in men and women with and without ACL injury. Hospital records of large group of patients, from 2004 to 2009, were reviewed. Patients with surgically confirmed isolated ACL tear, with no lesions of collateral ligaments, posterior cruciate ligament, or other bony abnormality and who had undergone preoperative MRI were included in the injured group. There were 73 ACL-injury patients (20 women and 53 men), with mean age 30.5 (range 14–54) years. In the control group, patients whose knee was screened due to minor trauma or bruises or due to other medical reasons were included. Patients with patellofemoral pain were excluded. There were 51 patients in this group (19 women and 32 men), with mean age 28.4 (range 16 to 49) years. Patients with meniscal injury were excluded from both groups. No patient had osteoarthritis. This study was approved by our Institutional Review Board.
All patients underwent MRI according to the standard protocol in our institution. Patients were placed supine with their legs extended and in neutral position by keeping the patella facing toward the roof. The involved knee was placed in a knee-extremity coil with the patella centered in the coil. After procuring a three-plane localizer scan, an axial scout scan was acquired. The sagittal slice imaging was aligned perpendicularly to a line tangential to the posterior margins of the posterior femoral condyles. Sagittal sections were secondarily aligned parallel to the femoral diaphysis on the coronal scout scan. This standard protocol ensured obtaining true sagittal images in all patients.
We first conducted a pilot study to determine the intrarater and interrater reliability in the measurement of MTPS and LTPS by using the new combined method and method described by Hashemi et.al. [12] (hereafter called method 1 in this study). Ten patients were randomly selected from control and injured groups (five men and five women from each group). Reliability in measurement was assessed by using intraclass correlation coefficient (ICC). Intrarater and interrater reliability was calculated on these random sample of 20 patients, with measurements performed at two different sessions, three weeks apart, by two observers. Each observer was blinded to the initial findings. We found that the combined method had a much higher intrarater and interrater reliability (Table 1), and this method was adopted for all final measurements, which were done by single author (M.S.K.).
Table 1.
Interrater and Intrarater reliability of the two methods
| ICCa values | ||||
|---|---|---|---|---|
| Method 1 | Combined method | |||
| MTPS | LTPS | MTPS | LTPS | |
| Observer 1 | 0.73 | 0.85 | 0.91 | 0.92 |
| Intrarater | ||||
| Observer 2 | 0.71 | 0.77 | 0.93 | 0.90 |
| Interrater | 0.73 | 0.80 | 0.93 | 0.94 |
ICC intraclass correlation coefficient, MTPS medial tibial plateau slope, LTPS lateral tibial plateau slope.
aAll values are significant (p < 0.05)
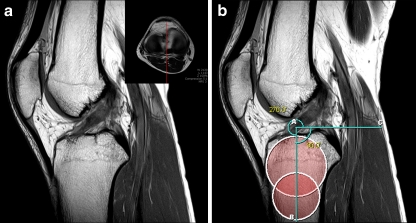
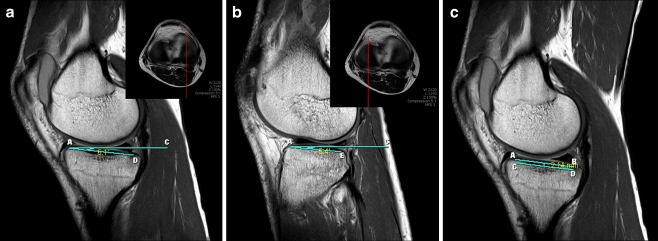
Briefly, MRI measurement consisted of identifying the most proximal transverse image of the tibia, immediately distal to the femur at the tibiofemoral joint. Using this axial cut as scout image, the central sagittal plane was identified [12] (Fig. 1a). Two circles were applied in the proximal tibia, with the proximal circle touching the anterior, posterior, and most proximal cortex and the distal circle touching the anterior and posterior cortex and its center lying in the circumference of the proximal circle [20]. The longitudinal tibial axis (TA) was defined as the line connecting the center of the two circles. A line perpendicular to this axis was drawn (Fig. 1b). Using the transverse scout image, the midarticulating portion of medial plateau was identified and the corresponding sagittal image selected. On this image, a line connecting the peak anterior and posterior points on the medial plateau was drawn, which defined the slope of the medial plateau. The perpendicular line to the TA was reproduced in this image, and the angle between the two was calculated, which gave the value of MTPS (Fig. 2a). In the same way, the central articulating region of the lateral plateau was identified and the LTPS calculated (Fig. 2b). If the posterior peak point was superior to the anterior peak point, the angle was measured as a negative value. The MTPD calculation was done by the method described by Hashemi et al. [12] (Fig. 2c). All measurements were done using the annotation tools on the Picture Archiving and Communication System (PACS), Marosis m-view 5.4 (Marotech, South Korea), which reports all angular measurements up to one decimal point value with a sensitivity of 0.1°, thus ensuring accurate measurement.
Fig. 1.
Assessment of tibial longitudinal axis (TA). Sagittal plane, at the center of the tibial plateau, used for assessing the TA (a). Inset shows the scout axial image used for determining the location of corresponding sagittal planes. Two circles drawn on the proximal tibia in this image and line connecting the centers of these circles, AB, is the TA (b). AC line perpendicular to the TA
Fig. 2.
Measurement of medial (MTPS) and lateral (LTPS) tibial plateau slopes and medial tibial plateau depth (MTPD). Line AC reproduced in midarticulating sagittal images of medial and lateral plateau and calculated MTPS (a) and LTPS (b). MTPD measured on the same image as used for MTPS measurement (c)
Statistical analysis
Independent samples Student’s t test was used to compare the MTPS, LTPS, and MTPD between the two groups and between the sexes. A two-way mixed ICC was used to access the interrater and intrarater reliability. A p value <0.05 was considered significant for all t tests and ICC analysis. To discern the relationship between the variables and ACL injury, a discriminant analysis was performed. Odds ratio (OR) was calculated for MTPS, LTPS, and MTPD to assess the association of these factors and ACL injury in overall patients and in men and women separately. All statistical calculations were done with PASW Statistics 18 software (IBM SPSS, Chicago, IL, USA).
Results
The intrarater and interrater reliability of the combined method was considerably higher than method 1 (Table 1). ICCs were excellent for both the intrarater and interrater comparisons in MTPS and LTPS measurement by the combined method (> = 0.9), whereas it was only good by method 1 (< = 0.73 and < = 0.85, respectively). MTPS, LTPS, and MPTD values for different groups and sexes are provided in Table 2. The injured group, comprising both men and women, had increased LTPS compared with the control group (p = 0.0001) (Table 3). There was no significant difference in MTPS and MTPD. Men with ACL injury had steeper LTPS (p = 0.0001) compared with men in the control group. Women with ACL injury had significantly shallower MTPD than women in the control group and men with ACL injury (both p < 0.05). Uninjured women had steeper MTPS and LTPS and shallower MTPD than uninjured men (p < 0.05 in all three measurements). Women in the control group had steeper MTPS values than women with ACL injury, but the result was not significant (p = 0.18).
Table 2.
Mean, standard deviation (SD), and range of medial (MTPS) and lateral (LTPS) tibial plateau slopes and medial tibial plateau depth (MTPD) in control and injured patients (group and sex distribution)
| Control group | Injured group | |||||||
|---|---|---|---|---|---|---|---|---|
| No. of individuals | Mean | SD | Range | No. of individuals | Mean | SD | Range | |
| MTPS (°) | ||||||||
| Men | 32 | 4.17 | 2.38 | 0.5–8.0 | 53 | 5.16 | 2.44 | 0.7–9.6 |
| Women | 19 | 5.9 | 2.52 | 1.7–11.8 | 20 | 4.78 | 2.57 | −0.2–9.7 |
| Total | 51 | 4.81 | 2.55 | 0.5–11.8 | 73 | 5.06 | 2.46 | −0.2–9.7 |
| LTPS (°) | ||||||||
| Men | 32 | 2.04 | 2.28 | −2.5–7.5 | 53 | 4.5 | 3.01 | −1.04–11.6 |
| Women | 19 | 3.67 | 2.54 | −0.6–8.8 | 20 | 4.82 | 3.21 | 0.6–10.8 |
| Total | 51 | 2.65 | 2.48 | −2.5–8.8 | 73 | 4.6 | 3.04 | −1.4–11.6 |
| MTPD (millimeter) | ||||||||
| Men | 32 | 2.4 | 0.78 | 1.07–3.76 | 53 | 2.45 | 1.2 | 0.31–6.6 |
| Women | 19 | 1.94 | 0.64 | 0.94–3.45 | 20 | 1.41 | 0.6 | 0.31–2.83 |
| Total | 51 | 2.23 | 0.75 | 0.94–3.76 | 73 | 2.17 | 1.16 | 0.31–6.6 |
Table 3.
Independent samples Student’s t tests results for medial (MTPS) and lateral (LTPS) tibial plateau slopes and medial tibial plateau depth (MTPD) between groups and sexes
| P values | |||
|---|---|---|---|
| MTPS | LTPS | MTPD | |
| Injured (I) vs. Control (C) | 0.56 | 0.0001* | 0.726 |
| Male (I) vs. female (C) | 0.27 | 0.29 | 0.08 |
| Male (I) vs. female (I) | 0.56 | 0.687 | 0.0004* |
| Female (I) vs. female (C) | 0.18 | 0.22 | 0.011* |
| Male (I) vs. male (C) | 0.07 | 0.0001* | 0.813 |
| Male (C) vs. female (C) | 0.0188* | 0.023* | 0.038* |
*Significant difference
Injured and control group (men and women combined) comparison revealed that LTPS had the highest predictive value [sensitivity 53.4%, specificity 72.5%, positive predictive value (PPV) 73.6%, negative predictive value (NPV) 52.1%], with OR of 3.031 [95% confidence interval (CI): 1.406–6.533, p = 0.005] for ACL injury. LTPS also had the highest association for ACL injury in men, with sensitivity and specificity of 62.3% and 78.1%, respectively, and PPV and NPV of 82.5% and 55.6%, respectively, with OR of 5.89 (95% CI: 2.156–16.10, p = 0.003). In women, MTPD had the highest predictive value, with sensitivity and specificity of 75% and 58%, respectively, and 65.2% PPV and 68.7% NPV, with OR of 4.13 (95% CI: 1.057–16.097, p < 0.04). No calculation of OR for other variables was significant.
Discussion
The results of studies measuring PTS, LTPS, and MTPS in the normal population are quiet varied. Roentgenographic studies measuring PTS [9, 14–16] report average values ranging from 8.5° to 10°. MTPS and LTPS, measured in MRI studies [12, 17–21], have been reported ranging from (mean values) -2.9° to 10.7°and -1.8° to 7.52°, respectively. Hashemi et al. [13] reported steeper MTPS and LTPS in ACL-injury patients compared with noninjured controls, whereas other studies [17–19] reported only steeper LTPS in ACL injured patients. Stijak et al. [17] reported steeper MTPS in uninjured populations compared with LTPS, with this finding being in total contrast to the study by Hashemi et al. [13]. We believe the great variation in values and results obtained between different studies is due to the method of choosing the TA and selecting sagittal images.
The PTS is calculated by measuring the angle between perpendicular to the TA and tangential to the medial and lateral plateau. For using the method described by Dejour and Bonnin [9], also used by Hashemi et al. [12] , at least 150 mm of bone below the joint gap should be available for assessing the longitudinal axis [22], and conventional MRI of the knee does not provide this adequate tibial length. The method described by Hudek et al. [20] is more appropriate for conventional MRI, but their selection of sagittal images was ambiguous. We combined the two methods: choosing the central sagittal image and midarticulating sagittal images of the medial and lateral tibial plateau, as described in method 1, and then drawing the TA using the method of Hudek et al. [20]. We called this the combined method, which overcomes both shortcomings and provides simple and reliable measurement of these variables. Using this method, we conducted the study with the purpose of comparing the MTPS, LTPS, and MTPD between the ACL-injury population and uninjured controls.
Stijak et al. [17] described a method using radiography, but this method is subject to a high error level [23] and requires additional investigation. The method described by Simon et al. [19] uses three-dimensional MRI and advanced software, which is not suitable for conventional MRIs and routine use. Our combined method had excellent (>0.90) interrater and intrarater ICC. Hashemi et al. [12] had an ICC of 0.88 with their method, and Bisson et al. [18], using the same method, reported an ICC of 0.85–0.88 for LTPS measurement.
Our first hypothesis that patients with ACL injury will have steeper MTPS and LTPS was partly correct, as LTPS in ACL-injury patients was significantly steeper than in controls. Other studies [13, 17, 19] also collaborate this finding. However, we were unable to find any significant difference between MTPS in control individuals and injured patients. This finding is supported by other studies [17–19] but is in contrast to the findings of Hashemi et al. [13]. Our second hypothesis is also partly correct, as we found significantly steeper LTPS in ACL-injury men than in uninjured men. This finding is also supported by other studies [13, 17–19]. Only the study by Hashemi et al. [13] reported significantly steeper MTPS in injured men. Our third hypothesis, that MTPD would be shallower in ACL-injury patients, in both men and women, again is partially correct, as we found significantly shallower MTPD in ACL-injury women compared with uninjured women and ACL-injury men. Only one study prior to ours assessed MTPD as a risk factor for ACL injury [13], and that study reported significantly shallower MTPD in the injured group and in men and women with ACL injury. Their finding can be attributed to a higher number of women in their study population. Our study had a much higher number of men. A study with strict matching regarding sex of the study population in assessing MTPD is required to remove this confounding variable. Bisson et al. [18] conducted a matched study, but they defined MTPD as the greatest distance from anterior to posterior on the medial tibial plateau and measured it in axial images. This measurement does not reflect true MTPD and is only the anteroposterior length of the medial tibial plateau.
The results from our study attest to the hypothesis that increased LTPS is an important risk factor for ACL injury. Increased posterior slopes lead to increased anterior tibial translation and increased anterior shear force, leading to increased strain on the ACL [10–12]. Steeper posterior slopes combined with shallower MTPD further facilitate the anterior translation of tibia. Steeper LTPS and shallower MTPD will result in external rotation of the femur under joint loading conditions, which will put the ACL under excess strain [24]. This external rotation movement may be further facilitated by normal MTPS or even aggravated by less steep MTPS. These factors might explain the increased incidence of ACL injury in female patients, as we found decreased MTPS and increased LTPS in ACL-injury women (although not significant) and significantly shallower MTPD. Sjitak et al. [17] also reported steeper MTPS in ACL-intact patients. In men, steeper LTPS and normal MTPS seems to play a significant role in ACL injury. OR values in our study also suggest the same, with MTPD in women and LTPS in men and in overall patients being the most important factors associated with ACL injury.
Our study had several strengths. We used a measurement method with a high reliability. All the final measurements were conducted by a single observer. Patients with isolated ACL injury only were included in injury group; patients with meniscal injury were also excluded. In the control group, no patient had prior knee complaints. Thus, confounding variables from both groups were minimal. This study is not without limitations, however. The primary limitation was unmatched injury and control groups and the retrospective nature. Another limitation is that with conventional MRI, rotational malalignment of the tibia could not be assessed, which may affect the measurements. We calculated knee rotation in all patients using the method described by Yagi et al. [25] and found the values within normal limits (mean values: control group 5.8° ± 7.54°; injured group 4.96° ± 6.7°), with no significant difference between groups. Thus, measurements between the two groups were comparable. Furthermore, all patients in this study were young, with no osteoarthritis and no history of fracture or knee complaints, and all MRIs were obtained using a standard protocol. Thus, the error resulting from this anatomic variability seems to be low and would not have affected the results of this study.
Although we calculated the OR for different variables, this only provides a model for risk analysis based on steeper slopes or shallow medial tibial plateau, without providing any definitive values. For true analysis of individuals at risk for ACL injury, a strictly matched and large prospective study is required, which can provide a cutoff value for these variables above or below which a person can be categorized into high risk. Future studies can focus on this aspect, but the high range of values and variability in these anatomic variables, even among uninjured individuals, would be a major hindrance.
Conclusion
We describe and recommend the combined method of measuring the LTPS and MTPS on conventional MRI, which is much simpler and more reproducible than the methods previously described. Steeper LTPS is an important risk factor for sustaining ACL injury, especially in men. Women with shallower MTPD are at increased risk of sustaining ACL injury. Measurement of these variables may prove useful in preventing contralateral ACL injury and improving prognosis of ACL reconstruction, but a prospective study with a large cohort is required to determine values of these variables, which may categorize an individual as high risk for ACL injury.
Acknowledgments
Conflict of interest statement The authors declare that they have no conflict of interest. The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.
References
- 1.Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP. Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture–is sports activity a determining variable? Int J Sports Med. 2001;22(4):304–309. doi: 10.1055/s-2001-13823. [DOI] [PubMed] [Google Scholar]
- 2.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Pećina M, Bajok I, Pećina HI. Tuberculum Intercondylare Tibiae Tertium as a Predictive Factor in the Anterior Cruciate Ligament Injury. Am J Sports Med. 2001;29(6):709–711. doi: 10.1177/03635465010290060601. [DOI] [PubMed] [Google Scholar]
- 4.Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International olympic committee current concepts statement. Br J Sports Med. 2008;42:394–412. doi: 10.1136/bjsm.2008.048934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am J Sports Med. 1988;16:449–454. doi: 10.1177/036354658801600504. [DOI] [PubMed] [Google Scholar]
- 6.Shelbourne KD, Facibene WA, Hunt JJ. Radiographic and intraoperative intercondylar notch width measurements in men and women with unilateral and bilateral anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 1997;5:229–233. doi: 10.1007/s001670050055. [DOI] [PubMed] [Google Scholar]
- 7.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears A prospective study. Am J Sports Med. 1998;26:402–408. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 8.Domzalski M, Grzelak P, Gabos P. Risk factors for Anterior Cruciate Ligament injury in skeletally immature patients: analysis of intercondylar notch width using Magnetic Resonance Imaging. Int Orthop. 2010;34(5):703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture Two radiological tests compared. J Bone Joint Surg Br. 1994;76:745–749. [PubMed] [Google Scholar]
- 10.Li G, Rudy TW, Allen C, Sakane M, Woo SL. Effect of combined axial compressive and anterior tibial loads on in situ forces in the anterior cruciate ligament: A porcine study. J Orthop Res. 1998;16:122–127. doi: 10.1002/jor.1100160121. [DOI] [PubMed] [Google Scholar]
- 11.Torzilli PA, Deng X, Warren RF. The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med. 1994;22:105–112. doi: 10.1177/036354659402200117. [DOI] [PubMed] [Google Scholar]
- 12.Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90:2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC, Jr, Dabezies E, Beynnon BD. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 14.Meister K, Talley MC, Horodyski MB, Indelicato PA, Hartzel JS, Batts J. Caudal slope of the tibia and its relationship to noncontact injuries to the ACL. Am J Knee Surg. 1998;11:217–219. [PubMed] [Google Scholar]
- 15.Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22:894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 16.Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63–67. doi: 10.1177/0363546509343198. [DOI] [PubMed] [Google Scholar]
- 17.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 18.Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy. 2010;26(7):901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. doi: 10.1016/j.jbiomech.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. doi: 10.1007/s11999-009-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuda S, Miura H, Nagamine R, Urabe K, Ikenoue T, Okazaki K, Iwamoto Y. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12:165–168. [PubMed] [Google Scholar]
- 22.Brazier J, Miguad H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. Evaluation of methods for radiographic measurement of the tibial slope. A study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200. [PubMed] [Google Scholar]
- 23.Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB. [Development of a 3-dimensional method to determine the tibial slope with multislice-CT] [in German] Z Orthop Ihre Grenzgeb. 2003;141:143–147. doi: 10.1055/s-2003-38658. [DOI] [PubMed] [Google Scholar]
- 24.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 25.Yagi T, Sasaki T. Tibial torsion in patients with medial-type osteoarthritic knee. Clin Orthop Relat Res. 1986;213:177–182. [PubMed] [Google Scholar]