Abstract
Osteosynthesis of comminuted posterior acetabular wall fractures is a challenging task for surgeons. We report a series of eight cases of such fractures where the comminuted fragments were excised and the defect in the posterior acetabular wall was reconstructed with iliac crest strut graft. The graft was buttressed with a reconstruction plate on its posterior aspect. The patients were followed up every week until radiological signs of union were seen. Subsequent follow-up was after six months, one year and annually. Patients were evaluated clinically by Merle d’Aubigne and Postel score and radiologically by Matta score at their final follow-up. All fractures united radiologically after an average follow-up of 3.2 months. The clinical outcome after mean follow-up of 3.34 years (minimum two years and maximum five years) was as follows: two (25%) were excellent, two (25%) were very good, three (37.5%) were good and one (12.5%) was fair. Radiological grading at last follow-up showed excellent in one (12.5%), good in four (50%) and fair in three (37.5%) patients. No complication in the form of infection, heterotopic ossification, neurovascular injury or graft resorption was noticed. To conclude, excision of the small comminuted fragments and reconstruction of the wall using iliac crest strut graft is a viable alternative technique for reconstruction of the comminuted posterior acetabular wall fracture. The medium-term clinical and radiological results of this technique are satisfactory.
Introduction
Posterior wall acetabulum fractures are the most common type of acetabular fracture [1]. Only 30% of these fractures involve a single large fragment. The majority are multifragmentary or have areas of impaction. Reconstruction of these comminuted or impacted posterior acetabular wall fractures is difficult; the problem is compounded when the posterior wall involvement exceeds 50% of the surface area and leads to hip joint instability [1, 13]. The usual treatment method as described in literature includes articular fragment reduction and bone grafting with buttress plating to support the elevated and comminuted fragments [1, 2]. Some surgeons prefer to buttress the small fragments with spring plates [4, 6, 10]. Recently, Giannoudis et al. have described a two-level reconstruction technique using subchondral miniscrews for the stabilisation of comminuted posterior-wall marginal acetabular fragments before applying lag screws and a buttress plate to the main overlying posterior fragment [5]. These levels of management demand extreme surgical skill, accuracy and infrastructure, which may be a limiting factor in many centres [7]. Again the orientation of the small fragments is sometimes difficult to assess [1, 13]. In this situation reconstruction of the wall with iliac crest autograft (after excising the comminuted fragments) seems to be a viable option. This technique was described as early as 1993 by Daum in two case reports [3]. We present the medium-term result of eight cases of severely comminuted posterior acetabular wall fractures (Letournel type 2 or 3, AO type A1 fracture) that were reconstructed with iliac crest strut graft.
Materials and methods
From 2003 to 2008, eight patients (seven males and one female) with severely comminuted posterior wall acetabular fractures (Letournel type 2 or 3, AO type A1) were treated surgically where the posterior acetabular wall had been reconstructed with iliac crest autograft. The mean age of the patients was 36.6 years (range 22–48 years). The demographic profile and clinical/radiological outcome of the surgery is cited in Table 1.
Table 1.
The demographic profile and clinical/radiological outcome of the patients with comminuted posterior wall fracture where the posterior wall was reconstructed with iliac crest strut graft
| Surgery number | Age/gender | Associated injuries | Surgical approach | Follow-up (y) | Merle d’Aubigne and Postel score | Radiological score |
|---|---|---|---|---|---|---|
| 1 | 28/M | Abdominal injury | Kocher-Langenbeck | 5 | Excellent | Good |
| 2 | 36/M | Medial malleolus fracture, knee ligament injury | Kocher-Langenbeck | 3.5 | Fair | Fair |
| 3 | 33/F | Patella fracture | Kocher-Langenbeck | 2.5 | Very good | Good |
| 4 | 48/M | Both bone forearm fracture, tibial plateu fracture | Kocher-Langenbeck | 3.5 | Good | Fair |
| 5 | 22/M | Head injury (AISS < 3), femur head fracture (Pipkin type I) | Ganz surgical dislocation | 3 | Very good | Good |
| 6 | 39/M | Blunt trauma chest | Kocher-Langenbeck | 4 | Good | Good |
| 7 | 44/M | – | Kocher-Langenbeck | 3.2 | Excellent | Excellent |
| 8 | 43/M | Abdominal injury, knee ligament injury | Kocher-Langenbeck | 2 | Good | Fair |
M male, F female, AISS abbreviated injury severity score
These patients were resuscitated and haemodynamic stability was achieved immediately after their arrival to our emergency services. They were managed for the associated life-saving emergencies. The hip joint dislocation was reduced and the limb was put on traction. Once the condition became stable, antero-posterior and oblique radiographic views of the pelvis and computed tomography scan (3-mm cut sections) of the pelvis were obtained (Figs. 1 and 2). Surgical treatment of the posterior wall acetabular fracture started as soon as they were fit. The average delay between injury and surgery was five days (range two–14 days).
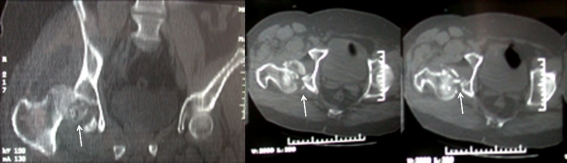
Fig. 1.
Radiograph shows posterior dislocation of hip with posterior acetabular wall fracture
Fig. 2.
Coronal and axial cut section of computed tomographic scan showing hip dislocation with comminuted posterior acetabular wall fracture (arrow) and femoral head fracture (Pipkin type I)
Seven out of eight patients were operated upon through the Kocher-Langenbeck approach. The only patient with associated femur head fracture (Pipkin type I) was approached through Ganz surgical dislocation which allowed us to deal with both fractures. The intra-operative findings showed severe comminution of the posterior wall of the acetabulum; the surrounding muscles were severely contused with disruption of the capsule. Most of the fragments were detached from the soft tissues. The sciatic nerve was identified and was found to be intact in all these cases. Traction was applied to the lower limb and intra-articular fragments were extracted. The small comminuted fragments were difficult for fixation and without any soft tissue attachment. The orientation of the fragments was difficult to appreciate. These were debrided (Fig. 3a). A large void or defect was noticed after removal of the fragments and the joint was unstable on examination.
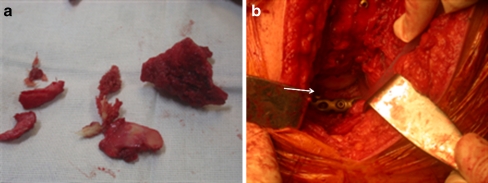
Fig. 3.
The infero-medial femur head fragment was excised. Because of severe comminution and difficulty in assessing the orientation of small fragments in this displaced comminuted acetabular fracture, fixation was not possible. The small fragments were discarded (a) and iliac crest strut graft was used for reconstruction of the posterior acetabular wall. The graft (arrow) was well supported with a reconstruction plate on its posterior aspect (b)
The posterior acetabular wall defect was reconstructed with a strut of iliac crest graft taken from the same side. The opposing surfaces of the graft and posterior acetabular wall were prepared in a step cut/oblique manner so that no step or protrusion on the posterior inner acetabular wall was created. This also improved the stability of the graft which was then fixed temporarily with K-wires. The femoral head acted as a mould for the posterior acetabular wall shape. The graft was fixed to the remaining acetabular wall by small fragment (3.5 mm) cancellous screws. It was then buttressed by a 3.5-mm reconstruction plate on its posterior aspect (Figs. 3b and 4a). The torn capsule was repaired and sewn over the graft or to the overlying soft tissues. A plate could not be placed in one patient so the iliac crest autograft in his case was fixed with screws only. However, he was immobilised for a long period (about six weeks) in the postoperative period.
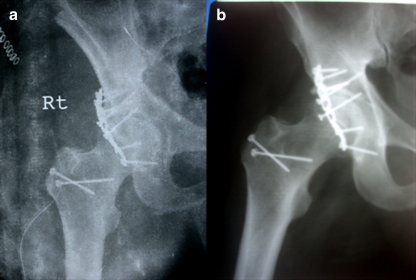
Fig. 4.
Immediately after the operation, a radiograph showing osteosynthesis of comminuted posterior acetabular wall fracture with iliac crest strut graft (a). Three months later the graft had completely united (b)
In the postoperative period prophylaxis for deep vein thrombosis (Enoxaparin 40/60 mg/day) and heterotopic ossification (Indomethacin 25 mg tid) was administered. Postoperatively traction was applied to the lower limb for a period of three weeks. Isometric quadriceps exercises, ankle pump and active flexion of the hip joint under the traction were carried out during this period. After three weeks traction was removed and mobilisation on the bed was allowed. Toe touch walking with crutches was started after six weeks. Complete weight bearing on the affected limb was restricted until the period radiological signs of union were noticed.
The patients were followed up weekly after their discharge from the hospital until the radiological signs of union were noticed. Then they were followed up at six months, one year and annually thereafter. All patients were evaluated for osteonecrosis with magnetic resonance imaging during these follow-up evaluations (at the end of three months, six months, one year and two years). We had an average follow-up of 3.34 years (minimum two years and maximum five years). The clinical (Merle d’Aubigne and Postel score) and radiological evaluation (Matta score) at the final follow-up was noted [11, 12]. According to this clinical grading system, pain, gait, and range of motion of the hip are each assigned a maximum of 6 points. The three individual scores are summed to derive the final score. The clinical result was classified as excellent (18 points), very good (17 points), good (15 or 16 points), fair (13 or 14 points), or poor (<13 points). The radiographs were graded according to the criteria developed by Matta [11]. In this grading method, excellent is given to a normal appearing hip joint, good denotes mild changes with minimal sclerosis and joint narrowing (<1 mm), fair indicates intermediate changes with moderate sclerosis and joint narrowing (<50%) while poor signifies advanced changes. A computed tomogram was performed to look for the graft incorporation and the posterior acetabular wall anatomy.
Results
No intra-operative and perioperative complications were observed. Radiological signs of union were noticed after an average period of 3.2 months following surgery (Fig. 4b).
The clinical outcomes according to the modified Merle d’Aubigne and Postel scoring systems at final follow-up were as follows: two (25%) were excellent, two (25%) were very good, three (37.5%) were good, and one (12.5%) was fair. None of the patients had a poor outcome. No complication in the form of neurovascular injury, heterotopic ossification or infection were noticed. One patient had evidence of avascular necrosis after one year of surgery. He was treated with core decompression at that time and he is able to manage to date with out any further intervention. No evidence of osteonecrosis was observed in other cases (Fig. 5). Radiological grading at last follow-up showed excellent in one (12.5%), good in four (50%), fair in three (37.5%) and none had a poor outcome (Fig. 6). Computed tomogram at final evaluation showed complete incorporation of the graft without any signs of resorption (Fig. 7).
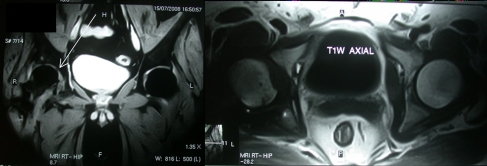
Fig. 5.
Magnetic resonance imaging after one year shows no evidence of osteonecrosis
Fig. 6.
Radiographs after three years show no evidence of avascular necrosis and mild degeneration in hip joint (good outcome as per Matta radiological score)
Fig. 7.
Coronal and axial images of computed tomographic scan showing complete incorporation of the graft after three years of surgery (arrow)
Discussion
Baumgaertner has postulated that operative management of posterior acetabular wall fracture offers the best chance of long-term joint function if an anatomically reconstructed acetabulum can be achieved without complication [1]. However, reconstruction of an anatomical acetabulum is difficult to achieve in a grossly comminuted posterior acetabular wall fracture. Letournel found good results in only 35% of patients in his series with comminuted posterior acetabular fractures [9]. Though the bone grafting technique in metaphyseal comminution, spring plate support, and mini screw fixation along with reconstruction plate support have been described in such comminution [1, 2, 4–6, 13, 14], these techniques may not always be possible. The anatomical orientation of the fragments is difficult to assess and the detachment of the soft tissues (either during surgical handing or injury per se) further devascularise the fragments [1, 13]. The general consensus among surgeons is that the soft tissue injury around posterior acetabular wall fracture is minimal because of its indirect nature of injury (dashboard injury) [1]. However our experience in severely comminuted wall fracture was completely different. The soft tissue had been severely damaged in these cases and the fragments were easily detached from the soft tissue even with careful handling.
Posterior acetabular wall reconstruction demands stable fixation considering the amount of force delivered to it, especially during the immediate postoperative period and the early part of rehabilitation when movement is started [4]. Goulet et al. [6] have demonstrated that fixation with spring plates and reconstruction plates have a higher load to failure than reconstruction plates alone, especially in concentrically comminuted fractures. Im et al. [8] found good results in posterior wall fractures with single fragment or moderate communition, fixed with screws only. However a description of the exact percentage of communition or the minimum size of the fragments amenable to screw fixation was not reported in their study. They also emphasised that using screws alone can prevent early weight bearing in comparison to buttress plate fixation. One patient with a large acetabular defect in the series had iliac crest graft fixation with screws only. The patient was advised a prolonged period of immobilisation in the postoperative period. The experience of using iliac crest strut graft in post-traumatic acetabular wall defect is not mentioned in literature. As a precautionary measure we also advised six weeks bed rest to our patients. However, bedside mobilisation was initiated early in the postoperative period and the graft sustained the load well as no evidence of nonunion or graft failure was noticed in this series.
Tricortical iliac strut graft offers the advantages of easy harvesting and better structural support. It can be shaped to fit the defect created after debridement of the fragments. It also matches the thickness of posterior acetabular wall. It can be better compared to a single fragment of posterior acetabulum wall which has lost its soft tissue attachment. This graft can be easily fixed to the parent bone with screws. Further buttressing of the graft with a reconstruction plate gives extra stability. Despite this, we advised our patients to avoid weight bearing for six weeks in the postoperative period to allow enough time for the graft to incorporate without any axial load on it.
The first use of iliac crest strut graft in severely comminuted posterior acetabular wall fractures was reported by Daum in 1993 [3]. In his report of two cases, the late functional result was good in one case whereas the other needed total hip arthroplasty after two years. However he could not achieve anatomical reduction in both of his cases. The cause of the arthritis in one of his patients could be attributed to this incongruent reduction. The iliac crest autograft was reduced anatomically (0–1 mm displacement) to the posterior wall in all of our cases and hence a better outcome was achieved comparable to most other studies [4–6, 8, 14]. We believe this reduction is of utmost importance in preventing the development of hip arthrosis. Accordingly, the medium term clinical and radiological outcomes of our series are good. Seven out of eight patients had excellent to good clinical outcome. The graft incorporated into the parent bone in all cases and a well contained acetabulum was formed. Osteonecrosis was noticed after one year in a patient and he was treated with core decompression. No further progression of the lesion was noticed and even after 3.5 years the patient is doing well. Again this procedure does not place additional risk of infection, neurovascular injury or heterotopic infection. The major drawback of the study is the small number of patients. However, this is the largest series of iliac-crest-graft fixation in comminuted posterior wall fracture with an excellent to good outcome. It demands special attention as this technique may be indicated in special types of severely comminuted posterior acetabular fractures, where osteosynthesis in primum is difficult to achieve.
In conclusion, excision of the small comminuted fragments and reconstruction of the posterior–acetabular wall with an iliac crest strut graft is a novel technique in comminuted fracture management. The medium term clinical and radiological results of this method of fixation are encouraging. Further study of this technique should be conducted so that the treatment can be established as a definative procedure in the management of severely comminuted posterior acetabular wall fractures.
References
- 1.Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7:54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Brumback RJ, Holt ES, McBride MS. Acetabular depression fracture accompanying posterior fracture dislocation of the hip. J Orthop Trauma. 1990;4:42–46. doi: 10.1097/00005131-199003000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Daum WJ. Traumatic posterior acetabular defects reconstructed with iliac crest autograft: a report of two cases. Clini Orthop Rel Res. 1993;291:188–192. [PubMed] [Google Scholar]
- 4.Ebraheim NA, Patil V, Liu J, Sanford CG, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. Int Orthop. 2007;31(5):671–675. doi: 10.1007/s00264-006-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Tzioupis C, Moed BR. Two-level reconstruction of comminuted posterior-wall fractures of the acetabulum. J Bone Joint Surg Br. 2007;89:503–509. doi: 10.1302/0301-620X.89B4.18380. [DOI] [PubMed] [Google Scholar]
- 6.Goulet J, Rouleau J, Mason D, Goldstein S. Comminuted fractures of the posterior wall of the acetabulum: a biomechanical evaluation of fixate on methods. J Bone Joint Surg Am. 1994;76(10):1457–1463. doi: 10.2106/00004623-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Gupta RK, Singh H, Dev B, Kansay R, Gupta P, Garg S. Results of operative treatment of acetabular fractures from the Third World—how local factors affect the outcome. Int Orthop. 2009;33:347–352. doi: 10.1007/s00264-007-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Im GI, Shin YW, Song YJ. Fractures to the posterior wall of the acetabulum managed with screws alone. J Trauma. 2005;58(2):300–303. doi: 10.1097/01.TA.0000149329.86361.CE. [DOI] [PubMed] [Google Scholar]
- 9.Letournel E, Judet R (1993) Fractures of the acetabulum. Springer, Berlin Heidelberg New York
- 10.Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin Heidelberg: Springer; 1989. [Google Scholar]
- 11.Matta JM. Fractures of the acetabulum: accuracy of reduction and results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 12.Merle d’Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 13.Rommens PM, Giménez MV, Hessmann MH. Is the posterior wall avulsion the simplest acetabular fracture? Eur J Trauma. 2000;26:144–154. doi: 10.1007/PL00002438. [DOI] [Google Scholar]
- 14.Stockle U, Hoffmann R, Nittinger M, Sudkamp NP, Haas NP. Screw fixation of acetabular fractures. Int Orthop. 2000;24(3):143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]