Abstract
Objective
The development of locking plate systems has led to polyaxial screws and new plate designs. This study compares monoaxial head locking screws (PHILOS© by Synthes) and a new generation of polyaxial locking screws (NCB-LE© by Zimmer) with respect to biomechanical stability.
Methods
On nine pairs of randomised formalin fixed humerus specimens, standardised osteotomies and osteosyntheses with nine monoaxial (group A) und nine polyaxial (group B) plate/screw systems were performed. A material testing machine by Instron (M-10 14961-DE) was used for cyclic stress tests and crash tests until defined breakup criteria as endpoints were reached.
Results
After axial cyclic stress 200 times at 90 N, plastic deformation was 1.02 mm in group A and 1.25 mm in group B. After the next cycle using 180 N the additional deformation averaged 0.23 mm in group A and 0.39 mm in group B. The deformation using 450 N was 0.72 mm in group A compared to 0.92 mm in group B. The final full power test resulted in a deformation average of 0.49 mm in group A and 0.63 mm in group B after 2,000 cycles using 450 N. When reaching the breakup criteria the plastic deformation of the NCB plate was 9.04 mm on average. The PHILOS plate was similarly deformed by 9.00 mm.
As a result of the crash test, in group A the screws pulled out of the humeral head four times whereas the shaft broke one time and another time the implant was ripped out. The gap was closed four times. In group B, there were three cases of screw cut-through, four shaft fractures/screw avulsions from the shaft and two cases of gap closure.
Conclusion
The two systems resist the cyclic duration tests and the increasing force tests in a similar manner. The considerable clinical benefits of the polyaxial system are enhanced by equal biomechanical performance.
Introduction
Fractures of the proximal humerus make up 4–5% of all fractures with an increasing incidence. To date the therapeutic gold standard is adequate anatomical reduction with early passive and active rehabilitation focussing on the maintenance of the glenohumeral joint function. Despite optimised operative concepts the published complication rate remains high at 20–76% [9, 14, 16].
The most frequent complications such as osteosynthesis failure, secondary dislocation and head necrosis are correlated to fracture morphology and implant failure [4]. During the last decade a series of new implants have been developed; in particular, locking plates and nail systems with different designs have been introduced. The first generation of fixed angle systems comprised monoaxial head locking systems that have been studied clinically for about ten years [7]. The systems allow fixed angle locking of screws through fine threads in head and plate in a unidirectional sense. The first clinical studies have shown encouraging results, but at the same time, not all problems in the treatment of the humeral fracture have been solved [3, 11].
In response to the different fracture morphology, frequent bone defects and differing bone structures, the systems have been further developed to allow polyaxial locking by new locking systems.
An important innovation will allow control of grip and direction of the screw for the surgeon. Furthermore, the classical compression technique can be combined with the fixed angle locking system. The resulting hybrid technique allows conventional screw implantation as a lag-screw while the surgeon can sense the bone quality and may change the screw direction, finally locking the screw by a cap. This new generation of fixed angle plate systems has been clinically applied in recent years. Concomitant study work has proved both efficacy and low complication rates of these systems [12].
Morbidity is another important issue under discussion. Particularly nail systems for the proximal humerus, with convincing biomechanical characteristics, may be well inserted minimally invasively, but can lead to considerable damage of the rotator cuff at the point of insertion [1]. As a modification of the minimally invasive approach, the deltasplit has been increasingly used for humeral head reduction. The disadvantage nail the nail and the head locking systems is the impossibility of reducing the fragments. The latter represents the main advantage of the polyaxial hybrid systems that allow indirect fragment reduction at the plate by conventional compression technique with lag-screws that are locked at a fixed angle.
Our study analyses the biomechanical characteristics of these new systems in comparison to the head locking systems. Varying design and width of plates and screws and differing locking mechanisms complicate the analysis. Therefore the resulting plate/screw system had to be similar in order to allow testing both primary stability and elasticity of the bone implant interface with respect to biomechanical strength.
After proving the biomechanical comparability, the postulated clinical benefits of the new systems may be verified.
Methods
For this study nine pairs of formalin fixed cadaver humera were used. The specimens were all examined for integrity in order to exclude damage by pre-existing fractures or operations. All were cleaned, X-rayed and randomised. After truncating to a length of 25 cm from the head they were embedded at 90 degrees to horizontal level. As a fracture model an unstable subcapital humeral fracture was simulated (A3 in the AO classification). A standardised medial wedge osteotomy was performed with 10-mm defect zone and intact lateral contact.
Subsequently, the osteosynthesis on the randomised specimen was performed according to the protocol. The study surgeon implanted nine PHILOS plates (Synthes) as head locking systems in group A. The same number of NCB (non contact bridging) plates (Zimmer) were implanted with polyaxial fixed angle screws. In both groups three bicortical screws were locked with torsional moment to fix the shaft fragment. The head fragment received nine fixed angle screws in the PHILOS and five in the NCB group. The results were documented by X-ray and photography (Fig. 1).
Fig. 1.
X-ray of a PHILOS-plate prior to testing
The tests were performed using a series 5566 material testing machine by Instron (Instron Corporation, 825 University Avenue, Norwood, MA 02062-2643 USA). Cyclic stress tests with a frequency of 1 Hz were conducted. The test sequence started with 90 N, 180 N and 450 N in 200 cycles each. Subsequently a continuous stress of 450 N in 2,000 cycles was applied.
The fracture tests were performed on the intact specimen with a pressure increase of 1 N/s until breakup. Breakup criteria were sudden pressure drop of more than 30% or pressure deformation of more than 30 mm. For data acquisition the company-owned software Bluehill II of the series 5500 was used. One hundred data per second were recorded. Synchronously, all tests were photographed by a Direct X Webcam. Data recorded were traverse path (in mm), force (in Newton), time (in seconds), and pressure deformation as well as plastic deformation as a measure for the irreversible deformation under the influence of forces.
Data were analysed using standardised statistical software (Statistical Package for Social Science [SPSS]; SPSS Inc., Chicago, IL, version 17.0). As tests for significance, the t-test for paired samples as well as the variance analysis ANOVA were applied. The level of significance was set at p < 0.05.
Results of cyclic tests
The first tests applying a relatively low pressure (90 N) were performed in order to compress the specimen and avoid further deformation by minimal force in later test sequences. In all tests for each specimen the pressure deformation over time was graphically demonstrated and analysed. The relevant biomechanical index value, i.e. the plastic deformation as a measure of the irreversible deformation, was recorded by the software using the maximum value in the last cycle. The average plastic deformation as a measure under 90 N was 1.02 mm in group A and amounted to 1.25 mm in group B (Fig. 2). The difference was not statistically significant (p = 0.31). Both the slightest (0.33 mm) and the greatest (2.42 mm) deformation occurred in group B.
Fig. 2.
Box-plot analysis of 90 N test. The box shows the area of the middle 50% of the data. The horizontal line in the box represents the median while the whiskers reach out to the minimum and maximum values
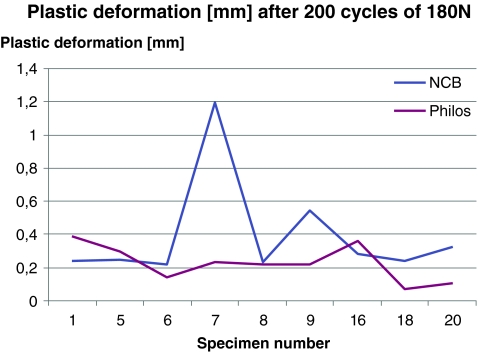
With doubled force of 180 N the resulting average plastic deformation was 0.23 mm in group A and 0.39 mm in group B (Fig. 3). Once again the difference was not statistically significant (p = 0.179), while the quantitative additional deformation was less than in the first 90 N test. A greater number of outliers mostly tending upwards were detected in group B.
Fig. 3.
Plastic deformation of all probe pairs at 180 N. Absolute values of plastic deformation in mm per specimen pair
By increasing the force to 450 N the irreversible deformation amounted to 0.72 mm in group A and 0.92 mm in group B (Table 1). The slightest deformation (0.09 mm) as well as the greatest (3.27 mm) this time resulted in group A. Significance level was p = 0.53.
Table 1.
Plastic deformation in mm of all specimens at 450 N
| Specimen number | Plastic deformation in mm (NCB) | Plastic deformation in mm (PHILOS) |
|---|---|---|
| 1 | 0.32625 | 0.53735 |
| 5 | 0.98484 | 1.60766 |
| 6 | 0.93844 | 0.36078 |
| 7 | 0.86562 | 1.25031 |
| 8 | 0.16188 | 0.39578 |
| 9 | 0.85031 | 0.35531 |
| 16 | 0.59281 | 1.03328 |
| 18 | 0.31625 | 0.09000 |
| 20 | 3.27281 | 0.86000 |
NCB non contact bridging
No probe failure according to the breakup criteria was observed in any of the tests. No cut-out of the screws or loosening of the plates was noticed.
Results of continuous stress test
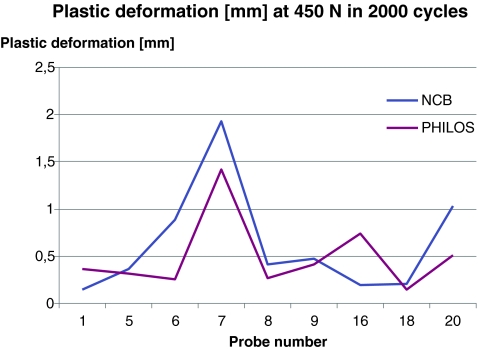
The test sequence was complemented by a continuous stress test that comprised 2,000 cycles with axial pressure of 450 N simulating complications such as implant failure, cut-out or loosening. The testing procedure was maintained as well as the frequency, only increasing the number of cycles. Despite a maximum pressure deformation of 5.37 mm the degree of plastic deformation in group A was only 0.49 mm on average. In group B maximum deformation was 3.65 mm with an average plastic deformation of 0.63 mm. The differences did not reach statistical significance (p = 0.32). The differences between the pairs were measurable while outliers were not found (Fig. 4). Again, in the 2,000 cycles test there was no probe failure.
Fig. 4.
Plastic deformation in mm at 450 N in 2,000 cycles. Absolute values of plastic deformation in mm per specimen pair
Results of crash test
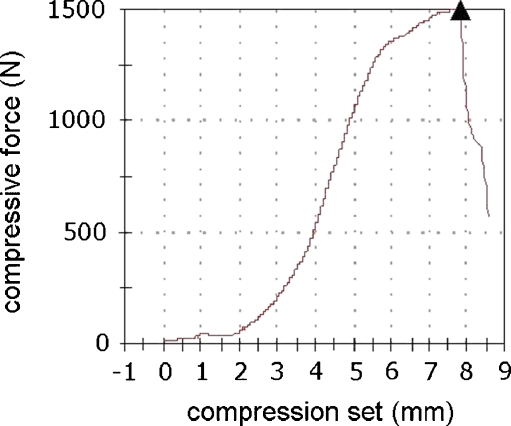
The crash test was performed increasing the force by 1 N per second until breakup criteria were reached. Breakup criteria were defined as sudden pressure drop of more than 30% or the preceding value of a total deformation of more than 30 mm. Also included were implant failure and screw cut-out. Pressure force per time and pressure force per pressure deformation were graphically demonstrated for each specimen (Fig. 5). In both groups in three of the specimens a cut-out of the screws through the head occurred. The medial support was reached three times in group A and twice in group B. This phenomenon simulates the combination of slow screw tearing from and cutting-out through the head.
Fig. 5.
Graph of probe 5 until breakup. The graph represents pressure deformation in mm per pressure force in Newton. At 1500 N (see triangular sign) sudden pressure drop of more than 20% led to breakup of test
Angular stability was retained in all 18 specimens. No screw fracture was observed. The shaft fractured four times in group B and once in group A. This difference may be caused by the different width of the screws being 3.5 mm in group B and 4.5 mm in group A.
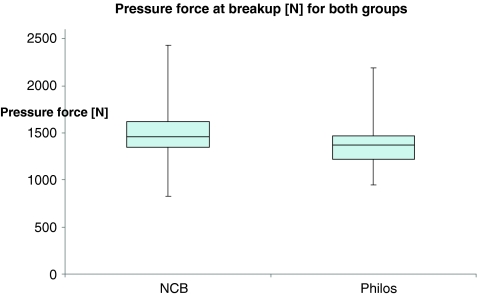
The average pressure deformation on reaching the breakup criteria was 9.78 mm in group A and 9.04 mm in group B. Individual specimens showed extreme values up to 14 mm in group B, eventually indicating the elastic component of the locking mechanism of the polyaxial screw system. The pressure forces when reaching the breakup criteria were 1,430 N in group A and 1,467 N in group B. None of the data showed statistical differences between the groups. The boxplot analysis showed similar results for failure (Fig. 6) with two specimens tolerating greater pressures of 2,000 and 2,500 N, while the samples were comparable.
Fig. 6.
Boxplot analysis of maximum pressure force at breakup for both groups. The box shows the area of the middle 50% of the data. The horizontal line in the box represents the median while the whiskers reach out to the minimum and maximum values
Discussion
The goal of any surgical reduction of proximal humeral fractures is the anatomical reduction and functional restoration of the shoulder joint. This chore is particularly demanding when operating on geriatric patients with poor bone quality due to osteoporosis [10, 15]. A possible modern solution is offered by the newest generation of systems with angular stability. The design, together with the locking mechanism, allows implantation of this plate fixator as a hybrid system [2]. Screws may be inserted as lag screws, may be used for compression and indirect reduction and may anytime during the operation be locked at a fixed angle [13]. These advantages, in comparison to the head locking screws, are at the expense of thicker plates and fewer screws in the head fragment. Despite bigger screw holes the plates proved to be better in biomechanical fatigue testing as shown by Kuster et al., whilst developing the system.
Fixed angle systems have been in clinical use for about ten years now. The benefits, as well as remaining problems, have been identified in clinical studies [18, 19]. Comparative clinical and biomechanical studies to differentiate between the different systems have not been performed. Our biomechanical test sequence found the polyaxial locking technique using fewer and thicker screws equally effective as the classical head locking screw systems. The cyclic tests, the fatigue tests, and the crash tests all came to the same result. Both the elastic and the rigid qualities are comparable, even if the design of plates and screws is completely different.
In the cyclic stress tests the rigidity was similar in both groups. The plastic deformation amounted to a maximum of 13% of the pressure deformation, confirming the comparability of elastic moments in both groups. Because the plates were of different thicknesses the rigidity was not equal, and this moment must be linked to the fixed angle blockade of polyaxial screws. Particularly, the individual analysis validates the assumption that locking by compression force of the caps (based on friction), must allow a certain degree of elasticity. The experimental work of Wilkens et al., comparing conventional with locking screws under a load to failure of 1650 N, indicates that locking systems by friction are sufficient [20].
The fracture model, lacking a medial hinge, is similar to the models used in published biomechanical studies [5, 6, 8]. The realistic breakup criteria of screw cut-out of the head and medial gap closure by pitching in the varus direction reinforce this model.
That the impact of weakening of the head by osteoporosis may not be simulated, remains a problem of the fracture model. When using polyaxial screws, the surgeon may avoid incorrect screw placement into the damaged substance by free direction of the screws and manual control prior to final blockade. This phenomenon cannot be subject to biomechanical testing, but is a major advantage in clinical use.
Yet unsolved is the question as to which bone to use for biomechanical testing. Our study was performed on formalin fixed bone, due to better availability. Some authors found it equal to the quality of fresh frozen bone [22]. On the other hand animal studies have revealed disadvantages [17, 21]. There is no obvious solution for the human model yet. The unrealistically high pressure forces (considering the advanced age of the donors) in the crash tests seem to be due to a sclerosis of the formalin fixed bone. The bone obviously appears to stiffen slightly during formalin fixation.
Conclusion
Polyaxial fixed angle locking systems represent a significant innovation for modern trauma surgery. Their use as a hybrid system combines advantages of the conventional techniques with angular stability. Free screw positioning with subchondral placement, three dimensional support and manual control allow metaphyseal and intraarticular fracture care, as well as periprosthetic fracture reduction. In detailed biomechanical testing the necessary rigidity and elastic characteristics of these plate systems have been proven.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Blum J, Hansen M, Rommens P. Die winkelstabile Marknagelung bei Frakturen am proximalen Humerus mit dem PHN (Proximaler Humerusnagel) Oper Orthop Traumatol. 2009;21:296–311. doi: 10.1007/s00064-009-1806-4. [DOI] [PubMed] [Google Scholar]
- 2.Erhardt J, Roderer G, Grob K, Forster T, Stoffel K, Kuster M. Early results in the treatment of proximal humeral fractures with a polyaxial locking plate. Arch Orthop Trauma Surg. 2009;129:1367–1374. doi: 10.1007/s00402-009-0924-7. [DOI] [PubMed] [Google Scholar]
- 3.Hessler C, Schmucker U, Matthes G, Ekkernkamp A, Gütschow R, Eggers C. Ergebnisse nach Versorgung instabiler proximalerHumerusfrakturen mittels winkelstabiler Platte. Unfallchirurg. 2006;109:867–874. doi: 10.1007/s00113-006-1138-x. [DOI] [PubMed] [Google Scholar]
- 4.Hessmann M, Rommens P. Osteosynthesetechniken bei proximalen Humerusfrakturen. Chirurg. 2001;72:1235–1245. doi: 10.1007/s001040170026. [DOI] [PubMed] [Google Scholar]
- 5.Hessmann M, Sternstein W, Mehler D, Korner J, Hofmann A, Rommens P. Sind winkelstabile Plattensysteme mit elastischen Eigenschaften fürdie Stabilisierung der Oberarmkopffraktur vorteilhaft? Biomed Technik. 2004;49:345–350. doi: 10.1515/BMT.2004.064. [DOI] [PubMed] [Google Scholar]
- 6.Hessmann M, Sternstein W, Krummenauer F, Hofmann A, Rommens P. Osteosynthese von Oberarmkopffrakturen—Einfluss desImplantatdesigns auf die biomechanische Stabilität. Chirurg. 2004;75:167–174. doi: 10.1007/s00104-004-0927-4. [DOI] [PubMed] [Google Scholar]
- 7.Kettler M, Braunstein V, Biberthaler P, Krammer M, Mutschler W. Komplikationen winkelstabiler Plattenosteosynthesen am Humeruskopf—Darstellung und Management. Trauma Berufskrankh. 2007;9:48–53. doi: 10.1007/s10039-005-1079-6. [DOI] [Google Scholar]
- 8.Lever J, Aksenov S, Zdero R, Ahn H, McKee M, Schemtisch E. Biomechanical analysis of plate osteosynthesis systems for proxima humerus fractures. J Orthop Trauma. 2008;22:23–29. doi: 10.1097/BOT.0b013e31815c89ce. [DOI] [PubMed] [Google Scholar]
- 9.Lill H, Josten C. Konservative oder operative Versorgung derHumeruskopffraktur beim alten Menschen? Chirurg. 2001;72:1224–1234. doi: 10.1007/s001040170025. [DOI] [PubMed] [Google Scholar]
- 10.Lohmann R, Haid K, Stöckle U, Raschke M. Epidemiologie und Perspektiven der Alterstraumatologie. Unfallchirurg. 2007;110:553–562. doi: 10.1007/s00113-007-1286-7. [DOI] [PubMed] [Google Scholar]
- 11.Maurer J, Rüter A. Winkelstabile Plattenosteosynthese amproximalen Humerus—Ein klinischer Vergleich von etablierten und neuenVerfahren. Trauma Berufskrankh. 2004;6:247–250. doi: 10.1007/s10039-003-0763-7. [DOI] [Google Scholar]
- 12.Röderer G, Gebhartd F, Erhardt J, Al-Agha S, AbouElsoud M, Kinzl L. Die non-contact-bridging(NCB)-Platte. Unfallchirurg. 2007;110:505–512. doi: 10.1007/s00113-006-1227-x. [DOI] [PubMed] [Google Scholar]
- 13.Röderer G, AbouElsoud M, Gebhard F, Claes L, Aschoff A, Kinzl L. Biomechanische Untersuchungen der winkelstabilen Plattenosteosyntheseam proximalen Humerus. Unfallchirurg. 2010;113:133–138. doi: 10.1007/s00113-009-1672-4. [DOI] [PubMed] [Google Scholar]
- 14.Strohm P, Köstler W, Südkamp N. Proximale Humerusfrakturen—was sollen wir tun? Z Orthop Unfall. 2008;146:312–317. doi: 10.1055/s-2008-1038541. [DOI] [PubMed] [Google Scholar]
- 15.Südkamp N. Erste Erfahrungen mit winkelstabilen Implantaten –obere Extremität: subcapitale Humerusfrakturen. Trauma Berufskrankh. 2004;6:13–18. doi: 10.1007/s10039-004-0857-x. [DOI] [Google Scholar]
- 16.Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 17.Virkus W, Goldberg S, Lorenz E. A comparison of compressive force generation by plating and intramedullary nailing techniques in a transverse diaphysial humerus fracture model. J Trauma. 2008;65:103–108. doi: 10.1097/TA.0b013e3181568ce7. [DOI] [PubMed] [Google Scholar]
- 18.Voigt C, Woltmann A, Lill H. Komplikationsmanagement nach winkelstabiler Plattenosteosynthese am proximalen Humerus. Chirurg. 2007;78:40–46. doi: 10.1007/s00104-006-1241-0. [DOI] [PubMed] [Google Scholar]
- 19.Voigt C, Lill H. Versorgung proximaler Humerusfrakturen—Fortschritte in der Plattenosteosynthese. Trauma Berufskrankh. 2007;9:43–47. doi: 10.1007/s10039-006-1118-y. [DOI] [Google Scholar]
- 20.Wilkens K, Curtiss S, Lee M. Polyaxial locking plate fixation in distal femur fractures: a biomechanical comparison. J Orthop Trauma. 2008;22:624–628. doi: 10.1097/BOT.0b013e31818896b3. [DOI] [PubMed] [Google Scholar]
- 21.Wingerter S, Calvert G, Tucci M, Benghuzzi H, Russel G, Puckett A. Mechanical strength repercussions of various fixative storage methods on bone. Biomed Sci Instrum. 2006;42:290–295. [PubMed] [Google Scholar]
- 22.Zech S, Goesling T, Hankemeier S, Knobloch K, Geerling J, Schultz-Brunn K, Krettek C, Richter M. Differences in the mechanical properties of calcaneal artificial specimens, fresh frozen specimens and embalmed specimens differ in experimental testing. Foot Ankle Int. 2006;27(12):1126–1136. doi: 10.1177/107110070602701220. [DOI] [PubMed] [Google Scholar]