Abstract
Purpose
This systematic literature review analysed the change in range of knee flexion from pre-operative values, following conventional posterior stabilised (PS) and high-flexion (H-F) PS total knee arthroplasty (TKA).
Methods
We calculated the weighted mean differences of pre- and postoperative flexion using meta-analysis with random effect modelling. Eighteen studies met our inclusion criteria. These data included a total of 2,104 PS knees that received conventional implants and 518 knees that received H-F implants.
Results
The pooled gain in flexion was 4.70° in the conventional group (p <0.0001) and 4.81° in the H-F group (p = 0.0008). In the subgroup analysis, the Western patient group showed significant difference in the gain of flexion with both implants. In contrast, no significant gain in flexion was observed in the Asian patient group.
Conclusions
These results suggest that improvement of preoperative flexion after TKA using current H-F PS prostheses is similar to that of conventional PS prostheses.
Introduction
The range of flexion of the knee is an important indicator of the postoperative functional outcome of total knee arthroplasty (TKA) and restoration of normal range of flexion is one of the major goals of TKA [1]. The deep flexion capability of the knee is essential to many daily activities, such as getting in and out a bath tub, gardening, etc. [2]. This is particularly true in Asian countries where deep knee flexion involving kneeling or squatting is common [3, 4]. Although the clinical results of TKA are satisfactory with regard to pain relief and overall function, patients rarely achieve flexion beyond 120° after TKA [5].
Various factors may affect knee flexion after total knee arthroplasty, such as preoperative flexion, gender, body weight, intraoperative variables, postoperative rehabilitation and prosthesis design [6]. Recently, several high-flexion (H-F) TKA implants have been introduced to the market to accommodate high flexion of the knee if patients can achieve high flexion. Patients who wish to return to active lifestyles are usually selected to receive these H-F implants [7] . However, whether H-F TKA designs can help patients to achieve high flexion after TKA is still unclear [8–16]. Many studies have reported on knee flexion after TKA using either conventional or H-F implants. While there are studies showing that H-F posterior substituting (PS) TKA designs provide greater flexion and better kinematic patterns [8–10, 16–20] as compared to the conventional TKA components, there are also studies that found no significant differences in range of motion (ROM) between the H-F and the conventional PS TKAs [11–15]. Additionally, clinical outcomes are also reported to be similar between the two patient groups [11, 13–15, 19, 20]. There are two systematic review articles that compare the flexion capability of conventional and H-F TKA implants [21, 22]. While one meta-analysis concluded that H-F implant design improves overall range of motion as compared to conventional implant designs [22], the other systematic review pointed out that there was insufficient evidence of improved range of motion or functional performance after H-F TKAs [21].
Due to the possible difference in patient selection among different studies, a systematic review or meta-analysis that compares conventional and H-F TKAs with regard to the improvement of the patient’s pre-operative flexion range is needed. The objective of this study was to use a meta-analysis approach to examine published data to clarify whether conventional and H-F PS prostheses provide increased range of knee motion relative to patients’ pre-operative flexion in the Asian and Western populations. We postulated that H-F knee implants would have a significant advantage in terms of enhancing knee flexion when compared to conventional TKAs in both Asian and Western populations.
Materials and methods
Search methods
We performed a computerised search of the electronic databases MEDLINE through Pubmed (1966 to January 2010), EMBASE (1980 to January 2010) and the Cochrane Library (1992 to January 2010). The published literature was searched in all languages with English abstracts, and article retrieval ended on January 22, 2010. The following key words were used in the literature search: “knee arthroplasty, knee replacement” AND “flexion OR range of motion OR ROM” AND “treatment outcome”. We reviewed the titles of the studies and the retrieved abstracts to decide if there was a possibility for inclusion in the meta-analysis.
Selection criteria
All identified titles and abstracts were evaluated. All available randomised control trials, nonrandomised trials and observational studies were reviewed. Single case reports, comments, letters, editorials, protocols, guidelines, and review papers were excluded. The reference lists of review papers were appraised for relevant papers not identified by the initial search. Inclusion criteria were:
Reports dealing with patients undergoing primary condylar type TKAs, with a traditional PS knee implant and/or a H-F PS knee implant
Patients with osteoarthritis and other non-traumatic diseases. Studies which included a wider range of indications were excluded if the proportion of osteoarthritis and other non-traumatic diseases was lower than 85%
The minimal follow-up duration was at least one year
A single fixed-bearing PS prosthesis design was used
Studies reporting maximum preoperative and postoperative knee flexions along with standard deviation or standard error
After reviewing the titles and abstracts of the studies, we determined if the study was appropriate for retrieval. We then assessed the studies and identified those eligible for inclusion in the meta- analysis. The articles were divided into conventional PS and H-F PS prostheses groups. When two series involving the same prostheses from the same institution were available, the most recent article with the longest follow-up was used.
Methodological quality assessment
The methodological quality of each eligibility study was evaluated using a modified Coleman methodology score (modified CMS). The CMS was originally developed for grading clinical studies on patellar tendinopathy [23]. The subsections that make up the CMS are based on the subsections of the CONSORT statement (for randomised controlled trials) but are modified to allow for other trial designs [24]. Khanna et al. modified the CMS for a systematic review of minimally invasive surgery (MIS) TKAs. This is referred to as “modified CMS” [25]. This scoring system assesses methodology using ten criteria, giving a total score between 0 and 100. A score approaching 100 indicates that the study has a robust design and largely avoids chances, various biases, or confounding factors. A score greater than 85 is considered excellent; from 70 to 84 is good; from 69 to 50 is moderate; and less than 50 is considered poor [23].
Data extraction
For each eligible study, we extracted relevant data about the conventional PS group and/or the H-F PS group. These included the study design (i.e., randomised control trial, prospective case control study, retrospective case control study or observational study), the country where the study was primarily conducted, the number of implanted knees and patients, the duration of final follow-up, the loss to final follow-up, the patient characteristics (i.e., age, gender, diagnosis), the implants used, mean preoperative flexion and postoperative flexion data at final follow up with standard deviations.
Statistical analysis
All of the mean flexion angles were extracted as continuous variables from the included studies. The absolute mean difference, variance and the associated 95% confidence intervals were calculated for all the included studies. A random-effects model was used to calculate the overall mean difference between the two treatments and its corresponding 95% confidence interval. A random-effects model was used to account for the heterogeneity among the included studies. Statistical heterogeneity was assessed by calculating a Cochrane Q. All conventional PS and H-F PS data were analysed first to examine the efficiency of conventional and H-F PS prostheses in improving the pre-operative range of knee joint flexion. In the subgroup analysis, the patients were divided into a Western patient population and an Asian patient population. Meta analysis was performed using Review Manager software (version 5.0 for Windows, The Cochrane Collaboration, Oxford, England 2008).
Results
Literature description
A total of 1,229 articles were identified in the initial search, of which 926 articles were eliminated based on the title or abstract. In the remaining articles, 18 met our inclusion criteria for meta-analysis because they reported pre-operative and post-operative range of flexion with standard deviation or standard error in fixed bearing PS prostheses [12–14, 16, 26–39]. These articles were published in English between 1992 and 2010.
Eight studies were prospective RCT [13, 27, 30–33, 35, 36]. Among them, four dealt with the comparison of PS TKA and cruciate retaining (CR) TKA [30, 31, 33, 35]; two were the comparison of PS TKA with PS mobile-bearing TKA [27, 36]; one was the comparison of PS TKA to H-F PS mobile-bearing TKA [32]; and one was the comparison of PS TKA with H-F PS TKA [13]. Six of the 18 selected studies were case controlled studies that included the H-F PS TKAs [12, 14, 16, 28, 29, 37]. Among these, four dealt with comparison of standard PS TKA to H-F PS TKA [12, 14, 16, 29]; one study was on the comparison of flexion contracture patients to the no-flexion contracture patients [28] and one study was on the comparison of MIS PS TKA to conventional TKA [37].
Four of the 18 selected studies were observational studies [26, 34, 38]. Of these, two were the comparison of PS TKA and cruciate sacrificing TKA [26, 38]; one was the comparison PS TKA and CR TKA [39]; one study reported the outcome of H-F PS TKAs [34].
Seven prosthesis designs were used in the conventional PS group (Insall-Burstein I, NexGen LPS, Apollo PS, PFC sigma PS, Genesis II PS, Kinemax PS, Scorpio PS) and two prosthesis designs (LPS-Flex, Genesis II PS High-Flex) were used in the H-F PS group. Five of the 18 studies were on Asian patient populations [12, 16, 35–37] and 13 studies were on Western patient populations [13, 14, 26–34, 36, 38, 39]. Details of the studies are shown in Table 1.
Table 1.
Summary of included studies
| Author | Year | Country | Prosthesis design | Study design | Type of study |
|---|---|---|---|---|---|
| Western patient population | |||||
| Maloney and Schurman [38] | 1992 | USA | I-B I | Obs comp | Total-condylar vs I-B I |
| Parsley et al. [26] | 2006 | USA | Apollo PS | Obs comp | PS vs ultracongruent component (PCL resection) |
| Malik et al. [14] | 2009 | USA | Genesis II PS, Genesis II PS H-F | CCS (retrospective) | Conventional PS vs H-F PS |
| Nutton et al. [13] | 2008 | UK | Nexgen LPS, Nexgen LPS-Flex | RCT | Conventional PS vs H-F PS |
| Cheng et al. [28] | 2010 | UK | Kinemax PS | CCS (retrospective) | Pre-op flexion contracture vs no pre-op flexion contracture |
| McCalden et al. [29] | 2010 | Canada | Genesis II PS, Genesis II PS H-F | CCS (retrospective) | Compare PS, H-F PS and CR |
| Chaudhary et al. [30] | 2008 | Canada | Scorpio PS | RCT | PS vs CR |
| Tanzer et al. [31] | 2002 | Canada | Nexgen LPS | RCT | PS vs CR |
| Wohlrab et al. [32] | 2009 | Germany | Nexgen LPS | RCT (blinding not described) | Conventional fixed bearing PS vs H-F MB PS |
| Victor et al. [33] | 2005 | Belgium | Genesis II PS | RCT | PS vs CR |
| Gioe et al. [27] | 2009 | USA | PFC sigma PS | RCT | PS vs MB PS |
| Zeh et al. [34] | 2009 | USA | Genesis II PS H-F | Obs | |
| Bozic et al. [39] | 2005 | USA | Nexgen LPS | Obs comp | PS vs CR |
| Asian patient population | |||||
| Bin and Nam [16] | 2007 | South Korea | Nexgen LPS, Nexgen LPS-Flex | CCS (consecutive series) | Conventional PS vs H-F PS |
| Maruyama et al. [35] | 2008 | Japan | PFC sigma PS | RCT | PS vs CR (bilateral knee) |
| Hasegawa et al. [36] | 2009 | Japan | PFC sigma PS | RCT | PS vs MB PS (bilateral knee) |
| Ng et al. [12] | 2008 | China | Nexgen LPS (Zimmer),Nexgen LPS-Flex | CCS | Conventional PS vs H-F PS (bilateral knee) |
| Watanabe et al. [37] | 2009 | Japan | Nexgen LPS-Flex | CCS (retrospective) | MIS approach vs conventional approach |
RCT randomised controlled study, Obs Comp observational comparative study, CCS case controlled study, Obs observational study, I-B I Insall-Burstein I (Zimmer, Warsaw, IN, USA), Apollo PS Apollo Posterior Stabilized (Zimmer, Warsaw, IN, USA), Genesis II PS Genesis II Posterior Stabilized, Genesis II PS H-F Genesis II Posterior Stabilized High-Flex (Smith & Nephew, Memphis, TN, USA), Nexgen LPS Nexgen Legacy Posterior Stabilized, Nexgen LPS-Flex Nexgen Legacy Posterior Stabilized Flex (Zimmer, Warsaw, IN, USA), Kinemax PS Kinemax Posterior Stabilized (Stryker Orthopaedics, Mahwah, NJ, USA), Scorpio PS Scorpio Posterior Stabilized Total Knee System (Stryker Orthopaedics, Mahwah, NJ, USA), PFC sigma PS PFC sigma Posterior Stabilized (DePuy Orthopaedics, Warsaw, IN, USA), PCL posterior cruciate ligament, CR cruciate retaining, MB mobile bearing, MIS minimally invasive surgery
Patient characteristics
These 18 studies included a total of 2,622 knees, of which 2,104 knees were implanted using conventional PS and 518 knees using H-F PS implants. Eight knees were lost to final follow-up for conventional PS and 16 knees for H-F PS implants. The mean age of the patients across these 18 studies was 68.7 years; 67.6% were females and 93.9% were osteoarthritis patients. The mean postoperative follow-up duration was 29.5 months. The patient characteristics across the studies are shown in Table 2.
Table 2.
Patient characteristics of included studies
| Author | Number of knees (patients) | Mean follow-up(SD) | Mean age (SD)(years) | Diagnosis (%) | Gender (%) | BMI (SD) | MCMS | ||
|---|---|---|---|---|---|---|---|---|---|
| OA | RA | Female | Male | ||||||
| Conventional PS group (N= 2104 knees) | |||||||||
| Maloney and Schurman [38] | 53 (37) | 21 mo | 68 | 65 | 24 | 62 | 38 | N/S | 53 |
| Parsley et al. [26] | 121 (121) | Minimal 1 y | 68.2 (9.8) | 99.2 | 0.8 | 69 | 31 | 29.3 (5.6) | 49 |
| Malik et al. [14] | 50 (50) | 1 y | 67.1 (9.9) | 98 | 2 | 76 | 24 | 33.0 (6.6) | 41 |
| Nutton et al. [13] | 28 (28) | 1 y | 68 | 100 | 0 | 57 | 43 | N/S | 86 |
| Cheng et al. [28] | 144 (144) | 12 y | 70.1 | 100 | 0 | N/S | N/S | 67 | |
| McCalden et al. [29] | 1177 (1177) | 5.4 y (minimal 1 y) | 67.82 (9.66) | 91 | 0 | 58 | 42 | 32.12 (5.15) | 69 |
| Chaudhary et al. [30] | 38 (38) | 22.7 (5.2) mo | 70.2 (8.4) | Noninflammatory arthritis | 45 | 55 | 30.9 (4.3) | 86 | |
| Tanzer et al. [31] | 20 | 2 y | 66 | 90 | 10 | 80 | 20 | 29.9 | 63 |
| Wohlrab et al. [32] | 30 (30) | 5 y | 66.52 (9.05) | Degenerative arthritis | 70 | 30 | 24.4 (6.6) | 64 | |
| Victor et al. [33] | 7 | 21 (2) mo | 70 (3) | 100 | 0 | N/S | N/S | 32.7 | 69 |
| Gioe et al. [27] | 136 | 42 (14.2) mo | 72.62 (7.2) | 96 | 2 | 4 | 96 | 31.51 (6.7) | 92 |
| Bin and Nam [16] | 90 | 1 y | 66.3 (6.6) | Degenerative arthritis | 97 | 3 | 27.7 (4.4) | 64 | |
| Maruyama et al. [35] | 20 (20) | 30.6 mo | 74.3 | 100 | 0 | 60 | 40 | N/S | 58 |
| Hasegawa et al. [36] | 25 (25) | 40 mo | 73 | 100 | 0 | 88 | 12 | 25.21 | 70 |
| Ng et al. [12] | 35 (35) | 35 mo | 68 | 100 | 0 | 80 | 20 | N/S | 33 |
| Bozic et al. [39] | 130 (105) | 5.9 (0.7) mo | 65.8 (10.3) | 90.4 | 5.1 | 74.3 | 25.7 | 30.8 | 62 |
| High-flexion PS group (N= 518 knees) | |||||||||
| Malik et al. [14] | 50 (50) | 1 y | 65.1 (9.9) | 100 | 0 | 76 | 24 | 32.6 (5.6) | 41 |
| Nutton et al. [13] | 28 (28) | 1 y | 71 | 100 | 0 | 39 | 61 | N/S | 86 |
| McCalden et al. [29] | 197 (197) | 5.4 y (minimal 1 y) | 65.93 (10.54) | 90 | 0 | 57 | 43 | 32.71 (7.25) | 69 |
| Zeh et al. [34] | 63 (63) | 16.25 (7) mo | 68 (9.8) | 100 | 0 | N/S | N/S | 31.2 (4.9) | 61 |
| Bin and Nam [16] | 90 | 1 y | 66.6 (7.7) | Degenerative arthritis | 93 | 7 | 27.0 (4.2) | 64 | |
| Ng et al. [12] | 35 (35) | 35 mo | 68 | 100 | 0 | 80 | 20 | N/S | 33 |
| Watanabe et al. [37] | 28 (25)a | 2.6 y | 71 | 84 | 16 | 80 | 20 | 28.1 (4.3) | 56 |
| 27 (23)b | 2.8 y | 71 | 74 | 26 | 74 | 26 | 26.3 (4.2) | ||
| Overall mean(SD) | 29.5 (19.0) mo | 68.7 (2.5) y | 93.9 (9.7)% | 67.6 (20.7)% | 29.7 (2.8) | 63.5 (14.9) | |||
OA osteoarthritis, RA rheumatoid arthritis, N/S not stated, MCMS modified Coleman methodology score, SD standard deviation, BMI body mass index
a Minimally invasive surgery (MIS) approach
b Conventional approach
Methodological quality assessment
The mean CMS values calculated for the 18 studies were 63.5 (range, 33–86) (Table 2). Quality scores were excellent in three, good in one, moderate in 11, and poor in three studies.
Meta-analysis
All 18 studies reported preoperative and postoperative knee flexion with standard deviation or standard error (Table 3). For the studies that only reported standard errors, these values were converted to standard deviations by using the cohort size [38]. Ten studies indicated that the flexion was measured using a goniometer [12–14, 26–28, 30, 34, 35, 38] (Table 3), while others did not specifically indicate the methods for flexion angle measurements.
Table 3.
Summary of included studies
| Author | Prosthesis design | Number of knees (patients) | Flexion pre-op (SD) | Post-op at final follow-up (SD) | Measurement condition of flexion | Method of measurement of flexion |
|---|---|---|---|---|---|---|
| Conventional PS group | ||||||
| Maloney and Schurman [38] | I-B I | 53 (37) | 112 (13.1) | 112 (14.56) | N/S | Goniometer |
| Parsley et al. [26] | Apollo PS | 121 (121) | 116 (14.5) | 120.7 (9.3) | Passive | Goniometer |
| Malik et al. [14] | Genesis II PS | 50 (50) | 114.6 (13.4) | 118 (14.1) | Gravity-assisted | Goniometer |
| Nutton et al. [13] | Nexgen LPS | 28 (28) | 107 (15) | 106 (17) | Active | Goniometer |
| Cheng et al. [28] | Kinemax PS | 144 (144) | 101.66 (14.9) | 109.46 (12.34) | Supine | Goniometer |
| McCalden et al. [29] | Genesis II PS | 1177 (1177) | 109.40 (16.13) | 116.78 (11.51) | N/S | N/S |
| Chaudhary et al. [30] | Scorpio PS | 38 (38) | 111.5 (15.3) | 105.8 (13.5) | N/S | Goniometer |
| Tanzer et al. [31] | Nexgen LPS | 20 | 101 (23) | 111 (17) | N/S | N/S |
| Wohlrab et al. [32] | Nexgen LPS | 30 (30) | 105.67 (17.8) | 117.5 (9.94) | N/S | N/S |
| Victor et al. [33] | Genesis II PS | 7 | 103 (9) | 117 (7) | Passive | N/S |
| Gioe et al. [27] | PFC sigma PS | 136 | 111.9 (12.83) | 111.9 (10.5) | N/S | Goniometer |
| Bin and Nam [16] | Nexgen LPS | 90 | 122.9 (17.0) | 124.3 (9.2) | Supine | Goniometer |
| Maruyama et al. [35] | PFC sigma PS | 20 (20) | 120.3 (17.9) | 131.3 (13.4) | N/S | Goniometer |
| Hasegawa et al. [36] | PFC sigma PS | 25 (25) | 118.3 (11.8) | 130.0 (7.2) | N/S | N/S |
| Ng et al. [12] | Nexgen LPS | 35 (35) | 105 (15) | 105 (13) | N/S | Goniometer |
| Bozic et al. [39] | Nexgen LPS | 130 (105) | 102.9 (14.9) | 108.6 (7.8) | N/S | N/S |
| High-flexion PS group | ||||||
| Malik et al. [14] | Genesis II PS H-F | 50 (50) | 115 (21.3) | 120 (12.1) | Gravity-assisted | Goniometer |
| Nutton et al. [13] | Nexgen LPS-Flex | 28 (28) | 108 (15) | 110 (17) | Active | Goniometer |
| McCalden et al. [29] | Genesis II PS H-F | 197 (197) | 109.98 (17.54) | 119.65 (12.59) | N/S | N/S |
| Zeh et al. [34] | Genesis II PS H-F | 63 (63) | 114 (9.2) | 120.7 (11.8) | N/S | Goniometer |
| Bin and Nam [16] | Nexgen LPS-Flex | 90 | 123.3 (13.1) | 129.8 (5.2) | Supine | Goniometer |
| Ng et al. [12] | Nexgen LPS-Flex | 35 (35) | 104 (17) | 106 (14) | N/S | Goniometer |
| Watanabe et al. [37] | Nexgen LPS-Flexa | 28 (25) | 128.2 (15.4) | 125.2 (15.4) | N/S | N/S |
| Nexgen LPS-Flexb | 27 (23) | 121.3 (15.3) | 120.0 (14.5) | N/S | N/S | |
I-B I Insall-Burstein I, Apollo PS Apollo Posterior Stabilized (Zimmer, Warsaw, IN, USA), Genesis II PS Genesis II Posterior Stabilized, Genesis II PS H-F Genesis II Posterior Stabilized High-Flex (Zimmer, Warsaw, IN, USA), (Smith & Nephew, Memphis, TN, USA), Nexgen LPS Nexgen Legacy Posterior Stabilized, Nexgen LPS-Flex Nexgen Legacy Posterior Stabilized Flex (Zimmer, Warsaw, IN, USA); Kinemax PS Kinemax, Posterior Stabilized (Stryker Orthopaedics, Mahwah, NJ, USA), Scorpio PS Scorpio Posterior Stabilized Total Knee System (Stryker Orthopaedics, Mahwah, NJ, USA), PFC sigma PS PFC sigma posterior stabilized (DePuy Orthopaedics, Warsaw, IN, USA), N/S not stated, SD standard deviation
a Minimally invasive surgery (MIS) approach
b Conventional approach
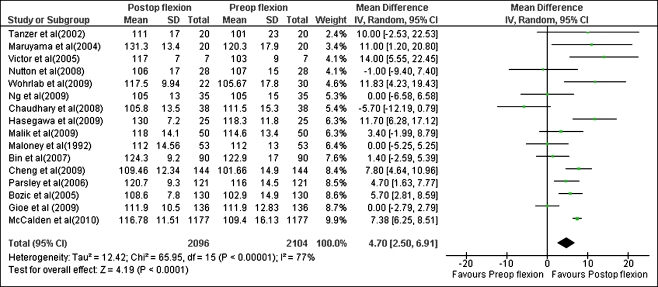
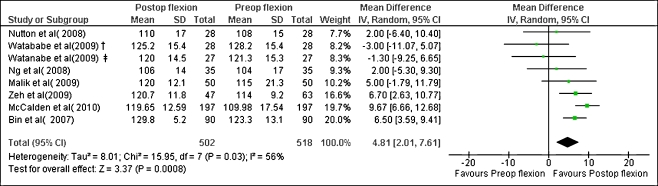
The overall mean differences of pre- and post-operative flexion were 4.70° in the conventional PS group (Fig. 1; p < 0.0001, 95% CI 2.50–6.91), and 4.81° in the H-F PS group (Fig. 2; p = 0.0008, 95% CI 2.01–7.61). A negative overall mean difference indicates a larger post-operative flexion angle than pre-operative flexion angle.
Fig. 1.
Forest plot of overall conventional posterior stabilised (PS) group. Weighted mean difference in flexion between preoperative and postoperative (°). A random effect model was used for analysis. SD standard deviation
Fig. 2.
Forest plot of overall high-flexion posterior stabilised (H-F PS) group. Weighted mean difference in flexion between preoperative and postoperative (°). A random effect model was used for analysis. † Minimally invasive surgery (MIS) approach, ‡ Conventional approach. SD standard deviation
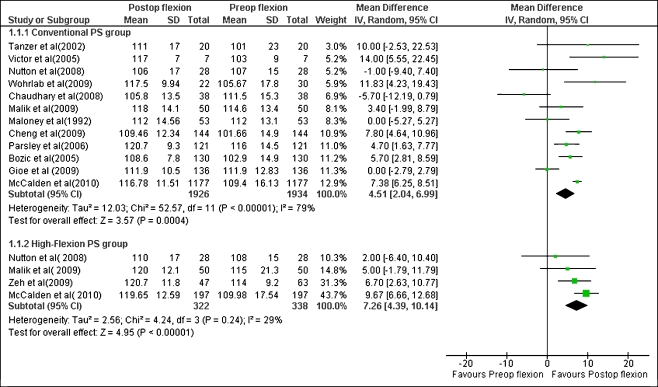
In the Western patient population, the overall mean differences between pre- and post-operative flexion were 4.51° and 7.26° in the conventional PS group (Fig. 3; P = 0.0004, 95% CI 2.04–6.99 ) and H-F PS group (Fig. 3; P < 0.00001, 95% CI 4.39–10.14), respectively.
Fig. 3.
Forest plot of conventional and high-flexion posterior stabilised (H-F PS) group in Western patient population. A random effect model was used for analysis. Weighted mean difference in flexion between preoperative and postoperative (°). SD standard deviation
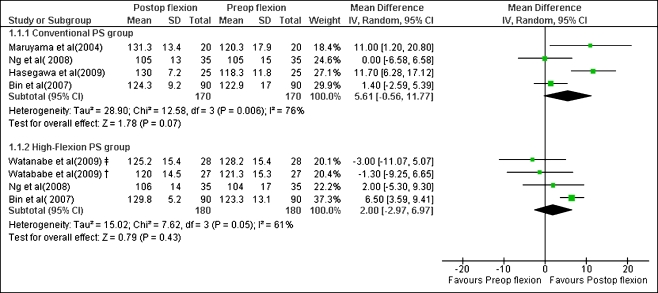
In the Asian patient population, the overall mean differences between pre- and post-operative flexion were 5.61° for the conventional PS patient group (Fig. 4; P = 0.07, 95% CI −0.56, 11.77) and 2.0° for the H-F PS patient group (Fig. 4; P = 0.43, 95% CI −2.97, 6.97).
Fig. 4.
Forest plot of conventional and high-flexion posterior stabilised (H-F PS) group in Asian patient population. A random effect model was used for analysis. Weighted mean difference in flexion between preoperative and postoperative (°). † Minimally invasive surgery (MIS) approach, ‡ Conventional approach. SD standard deviation
Discussion
The use of H-F TKA implants has become popular due to the expectation of achieving higher flexion after TKA surgery, especially for younger patients who are eager to return to demanding activities [6, 40]. However, it is unclear if current H-F TKA designs can improve postoperative knee flexion when compared to the pre-operative knee flexion. The findings of this review demonstrated that the improvement of flexion from preoperative values after surgery was significant in both the conventional (in seven implants) and H-F (two implants) PS groups (4.70˚, P < 0.0001 and 4.81˚, P = 0.0008, respectively). In subgroup analysis, the Western patient population group showed a significant difference between the improvement in flexion post-surgery with standard PS and with H-F PS implants (4.51˚, P = 0.0004 and 7.26˚,P < 0.00001, respectively). In the Asian patient population group, no significant difference was noted in the improvement of knee flexion post-surgery between the conventional and H-F PS groups (5.61˚, p = 0.07 and 2.0˚, p = 0.43, respectively). The data analysis did not fully support our hypothesis that H-F knee implants would have a significant advantage over the conventional TKAs in terms of enhancing knee flexion in both Asian and Western patient populations.
In literature, there are conflicting data on the effectiveness of various TKA implants in providing high knee flexion following surgery. Among the nine studies that reported on the flexion or ROM of H-F PS and conventional PS TKA designs (Table 4), four studies have shown a significantly improved flexion or ROM after use of a H-F PS TKA [16, 18–20]. Conversely, five studies found no significant differences in the range of motion or flexion between the H-F PS TKA and conventional PS TKAs [11–15].
Table 4.
Results of comparative studies between fixed-bearing conventional posterior stabilised (PS) and high-flexion posterior stabilized (H-F PS) total knee arthroplasty (TKA)
| Author | Year | Country | Study design | Prosthesis design | Number of knees (patients) |
Mean follow-up (years) |
Preop flexion (SD) |
Postop flexion (SD) |
Preop ROM (SD) |
Postop ROM (SD) |
P value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Huang et al. [19] | 2005 | Taiwan | CCS | Nexgen LPS | 25 (25) | 2 | N/S | N/S | 110 | 126 | P < 0.05 |
| Nexgen LPS-Flex | 25 (25) | N/S | N/S | 112 | 138 | ||||||
| Kim et al. [11] | 2005 | South Korea | RCT | Nexgen LPS | 50 (bilateral knee) | 2.1 | N/S | N/S | 126 | 136 | P > 0.41 |
| Nexgen LPS-Flex | 50 (bilateral knee) | N/S | N/S | 127 | 139 | ||||||
| Bin and Nam [16] | 2007 | South Korea | CCS | Nexgen LPS | 90 | 1 | 122.9 (17.0) | 124.3 (9.2) | 115.3 (22.5) | 123.6 (10.4) | P < 0.05 |
| Nexgen LPS-Flex | 90 | 123.3 (13.1) | 129.8 (5.2) | 117.9 (18.8) | 129.4 (5.4) | ||||||
| Weeden and Schmidt [20] | 2007 | USA | RCT | Nexgen LPS | 25 (25) | 1 | 121 | 120 | N/S | N/S | P < 0.05 |
| Nexgen LPS-Flex | 25 (25) | 122 | 133 | N/S | N/S | ||||||
| Ng et al. [12] | 2008 | China | CCS | Nexgen LPS | 35 (35) | 2.9 | 105 (15) | 105 (13) | N/S | N/S | P = 0.201 |
| Nexgen LPS-Flex | 35 (35) | 104 (17) | 106 (14) | N/S | N/S | ||||||
| Nutton et al. [13] | 2008 | Scotland | RCT | Nexgen LPS | 28 (28) | 1 | 107 (15) | 106 (17) | N/S | N/S | NS |
| Nexgen LPS-Flex | 28 (28) | 108 (15) | 110 (17) | N/S | N/S | ||||||
| Laskin [18] | 2007 | USA | CCS | Genesis II PS | 40 (40) | 2 | 116 | 118 | N/S | N/S | P < 0.01 |
| Genesis II PS H-F | 40 (40) | 117 | 133 | N/S | N/S | ||||||
| McCalden et al. [15] | 2009 | Canada | RCT | Genesis II PS | 50 (50) | 2.7 | 114 | 124 (7) | N/S | N/S | P = 0.811 |
| Genesis II PS H-F | 50 (50) | 111 | 123 (7) | N/S | N/S | ||||||
| Malik et al. [14] | 2009 | USA | CCS | Genesis II PS | 50 (50) | 1 | 114.6 (13.4) | 118 (14.1) | 114 (22) | 118 (14.1) | P = 0.43 |
| Genesis II PS H-F | 50 (50) | 115 (21.3) | 120 (12.1) | 115 (21.3) | 124.3 (9.2) |
Nexgen LPS Nexgen Legacy Posterior Stabilized, Nexgen LPS-Flex Nexgen Legacy Posterior Stabilized Flex (Zimmer, Warsaw, IN, USA), Genesis II PS Genesis II Posterior Stabilized, Genesis II PS H-F Genesis II Posterior Stabilized High-Flex (Smith & Nephew, Memphis, TN ,USA), RCT randomised controlled study, CCS case controlled study, N/S not stated, NS not statistically different, SD standard deviation
Schurman et al. evaluated 358 consecutive total knee replacements using five PS prosthetic designs (I-B I, I-B II, Apollo, Performance, Ascent) [41] with at least one-year follow-up. Absolute flexion was improved from preoperative (110° ) to postoperative (113°) (p = 0.02). No difference was found in improvement of range of motion among these five prostheses. Two studies evaluated change of flexion with comparison of high-flexion implants to standard implants [12, 42]. Ng et al. reported that the standard group lost 0.5˚ postoperative and the H-F group gained 2˚, but there were no significant differences between the two groups (p = 0.201) [12]. Similarly, Ahmed et al. did not show significant differences between the two groups (1˚ in standard group, 2˚ in H-F group, P = 0.416) [42].
There were two systematic reviews that reported on comparison of conventional PS and H-F PS TKA implants. A meta-analysis performed by Gandhi et al. [22] concluded that H-F implant designs improve the overall ROM compared with traditional implants but offer no advantage in Knee Society score in primary TKAs. Murphy et al. performed a systematic review [21] focussing on outcomes after HF TKAs. They found that there was insufficient evidence to support that H-F TKA implants improved ROM or functional performance and the claims of greater flexion, ROM, and function for H-F TKA reported in some of those studies were not supported due to poor study designs, short follow-up periods, inadequate blinding, and use of functional outcome measures that lacked sensitivity.
Direct comparison of conventional and H-F TKAs is difficult due to the variations in patient conditions, such as the pre-operative flexion angles [21]. Therefore, we compared the improvement of pre-operative flexion with the conventional and H-F PS TKAs. Our review showed significant improvement of knee flexion from pre-operative values with both the conventional PS TKA and H-F PS TKA, although the gain is less than 5˚ in both groups. In general, the H-F PS implants showed no advantage in improvement of knee flexion compared to the conventional PS implants. Among the Western patient group, however, the H-S implants showed a slightly higher improvement (2.5˚ on average) to pre-operative flexion compared to the conventional PS implants.
In Asia, daily activities are frequently carried out on the floor. Deep flexion of the knee joint is therefore very important in Asian countries, and is often necessary to perform routine activities such as kneeling, squatting and sitting with both legs crossed [3, 4]. One study on Asian patients showed an improvement in knee flexion using a high flexion design [19]. However, our review found no significant difference between the improvement of pre-operative knee flexion with standard PS and H-F PS implants in the Asian population.
Another issue relates to concerns that efforts to increase maximum flexion may negatively impact implant life [43–47]. The smaller radii of curvature of H-F TKA implants (LPS Flex) requires resection of an additional 2–4 mm of bone from the posterior condyles. This may weaken the bone supporting the load from the femoral component. Nagura et al. found that deep-flexion activities generate one to 13 times larger net quadriceps moments (average five) than walking [44]. Furthermore, in posterior-stabilised designs, additional bone is removed from the intercondylar area to accommodate the increased box height [48]. High flexion may also be associated with TKA cam-post instability. Moynihan et al. studied the in vivo knee kinematics of six patients who achieved high flexion after seven LPS H-F TKAs using dual-plane fluoroscopy. They found that cam-post dis-engagement occurred at high-flexion angles. At maximum flexion, five of the seven TKAs demonstrated cam-post disengagement and lateral femoral condylar liftoff [47]. Several studies have shown increasing contact stresses with increasing flexion and this could potentially lead to greater wear, increased patellar fracture or loosening and earlier failure of polyethylene inserts [44–46]. Ranawat et al. noted that shortening the posterior radius by removing more bone would result in instability and increased patellar and tibial stresses and revisions [43]. Han et al. reported a 38% prevalence of femoral component loosening in the LPS H-F TKA at a mean follow-up of 2.7 years in patients engaging in high-flexion activities [45]. Therefore, with the limited gains of current H-F PS implants, it is necessary to further investigate ways in which a new generation of TKA implants can improve patient outcome and knee flexion, while avoiding potential risk factors of deep flexion.
This study has several limitations. Radiographic measurement of the range of motion is considered to be the most accurate technique [49], but, in clinical practice, most surgeons measured the range of motion using a goniometer. In the selected papers, the method of measurement of ROM was generally unclear and lacked uniformity. Ten of the studies indicated their means of measurement using a universal goniometer [12–14, 16, 26–28, 30, 34, 35, 38] and only six reported basic technical details [13, 14, 16, 26, 28, 33]. There were only four studies that reported a randomised controlled trial (RCT) comparing H-F PS and conventional PS TKAs [11, 13, 15, 20]. These RCTs usually have small sample sizes and only one study reported the preoperative and postoperative flexion with standard deviation to perform meta-analysis comparing the conventional and H-F designs. Our eligible studies included different study designs (i.e., randomised control trials, nonrandomised trials, observational studies) that reported the preoperative and postoperative flexion with standard deviation or standard error. These studies included various patient’s characteristics, preoperative factors, surgical techniques, postoperative rehabilitation, and different fix-bearing PS designs. The conventional PS group included six designs and the H-F PS group included only two designs. We could not separate the meta-analysis for each manufacturer, because of small sample sizes for each implant design. In the future, if more studies are reported, a meta-analysis should be performed for individual implant designs. The minimal follow-up duration was over one year. It is possible that further changes might occur with longer follow-up. However, previous studies have reported that the ROM and flexion reach a plateau around one year after surgery, with few clinically significant changes with longer follow-up [3, 11, 50].
Conclusion
In conclusion, our meta-analysis was able to demonstrate that the improvement of preoperative flexion post-surgery was significantly different in the conventional PS and H-F PS groups (4.70˚, P < 0.0001 and 4.81˚, P = 0.0008). No advantage of H-F PS TKAs was found in the improvement of knee flexion compared to the conventional PS implants. In subgroup analysis, the Western patient population group showed a significant difference in the improvement of knee flexion with the conventional PS and H-F PS groups (4.51˚, P = 0.0004 and 7.26˚, P < 0.00001). The H-F PS implants, on average, showed 3˚ higher improvement in knee flexion compared to the conventional TKAs. Whereas in the Asian patient population group, no significant improvement to knee flexion was found between conventional and H-F PS implants (5.61˚, P = 0.07 and 2.0˚, P = 0.43). These results suggest that improvement of preoperative knee flexion after TKA using current H-F PS prostheses are similar to conventional PS prostheses.
Acknowledgments
Conflict of interest The authors have no conflicts of interests.
References
- 1.Ritter MA, Campbell ED. Effect of range of motion on the success of a total knee arthroplasty. J Arthroplasty. 1987;2:95–97. doi: 10.1016/S0883-5403(87)80015-3. [DOI] [PubMed] [Google Scholar]
- 2.Rowe AJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture. 2000;12:143–155. doi: 10.1016/S0966-6362(00)00060-6. [DOI] [PubMed] [Google Scholar]
- 3.Park KK, Chang CB, Kang YG, Seong SC, Kim TK. Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J Bone Joint Surg Br. 2007;89:604–608. doi: 10.2106/JBJS.F.00979. [DOI] [PubMed] [Google Scholar]
- 4.Nakamura S, Takagi H, Asano T, Nakagawa Y, Kobayashi M, Nakamura T. Fluoroscopic and computed tomographic analysis of knee kinematics during very deep flexion after total knee arthroplasty. J Arthroplasty. 2010;25:486–491. doi: 10.1016/j.arth.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Sultan PG, Most E, Schule S, Li G, Rubash HE (2003) Optimizing flexion after total knee arthroplasty: Advances in prosthetic design. Clin Orthop Relat Res 416:167–173 [DOI] [PubMed]
- 6.Dennis DA, Komistek RD, Scuderi GR, Zingde S. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007;464:53–60. doi: 10.1097/BLO.0b013e31812f785d. [DOI] [PubMed] [Google Scholar]
- 7.Li G, Schule S, Zayontz S, Maloney W, Rubash H (2003) Improving flexion in total knee arthroplasty. The adult knee, vol 2. Lippincott Williams & Wilkins, Philadelphia
- 8.Argenson JN, Komistek RD, Mahfouz M, Walker SA, Aubaniac JM, Dennis DA (2004) A high flexion total knee arthroplasty design replicates healthy knee motion. Clin Orthop Relat Res 428:174–179 [DOI] [PubMed]
- 9.Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, Rubash HE. Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: An in vitro robotic experimental investigation. J Bone Joint Surg Am. 2004;86-A:1721–1729. doi: 10.2106/00004623-200408000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Coughlin KM, Incavo SJ, Doohen RR, Gamada K, Banks S, Beynnon BD. Kneeling kinematics after total knee arthroplasty: Anterior-posterior contact position of a standard and a high-flex tibial insert design. J Arthroplasty. 2007;22:160–165. doi: 10.1016/j.arth.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475. doi: 10.2106/JBJS.D.02707. [DOI] [PubMed] [Google Scholar]
- 12.Ng FY, Wong HL, Yau WP, Chiu KY, Tang WM. Comparison of range of motion after standard and high-flexion posterior stabilised total knee replacement. Int Orthop. 2008;32:795–798. doi: 10.1007/s00264-007-0409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nutton RW, Linden ML, Rowe PJ, Gaston P, Wade FA. A prospective randomised double-blind study of functional outcome and range of flexion following total knee replacement with the nexgen standard and high flexion components. J Bone Joint Surg Br. 2008;90:37–42. doi: 10.1302/0301-620X.90B1.19702. [DOI] [PubMed] [Google Scholar]
- 14.Malik A, Salas A, Ben Ari J, Ma Y, Gonzalez Della Valle A (2010) Range of motion and function are similar in patients undergoing TKA with posterior stabilised and high-flexion inserts. Int Orthop 34(7):965–972 [DOI] [PMC free article] [PubMed]
- 15.McCalden RW, MacDonald SJ, Bourne RB, Marr JT. A randomized controlled trial comparing "high-flex" vs "standard" posterior cruciate substituting polyethylene tibial inserts in total knee arthroplasty. J Arthroplasty. 2009;24:33–38. doi: 10.1016/j.arth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Bin SI, Nam TS. Early results of high-flex total knee arthroplasty: Comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–355. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 17.Kanekasu K, Banks SA, Honjo S, Nakata O, Kato H. Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty. 2004;19:998–1003. doi: 10.1016/j.arth.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 18.Laskin RS. The effect of a high-flex implant on postoperative flexion after primary total knee arthroplasty. Orthopedics. 2007;30:86–88. [PubMed] [Google Scholar]
- 19.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: A minimum of 2 years of follow-up. J Arthroplasty. 2005;20:674–679. doi: 10.1016/j.arth.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 20.Weeden SH, Schmidt R. A randomized, prospective study of primary total knee components designed for increased flexion. J Arthroplasty. 2007;22:349–352. doi: 10.1016/j.arth.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Murphy M, Journeaux S, Russell T. High-flexion total knee arthroplasty: A systematic review. Int Orthop. 2009;33:887–893. doi: 10.1007/s00264-009-0774-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gandhi R, Tso P, Davey JR, Mahomed NN. High-flexion implants in primary total knee arthroplasty: A meta-analysis. Knee. 2009;16:14–17. doi: 10.1016/j.knee.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon study group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 24.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T. The revised consort statement for reporting randomized trials: Explanation and elaboration. Ann Intern Med. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 25.Khanna A, Gougoulias N, Longo UG, Maffulli N. Minimally invasive total knee arthroplasty: A systematic review. Orthop Clin North Am. 2009;40:479–489. doi: 10.1016/j.ocl.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Parsley BS, Conditt MA, Bertolusso R, Noble PC. Posterior cruciate ligament substitution is not essential for excellent postoperative outcomes in total knee arthroplasty. J Arthroplasty. 2006;21:127–131. doi: 10.1016/j.arth.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J. Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:2104–2112. doi: 10.2106/JBJS.H.01442. [DOI] [PubMed] [Google Scholar]
- 28.Cheng K, Ridley D, Bird J, McLeod G. Patients with fixed flexion deformity after total knee arthroplasty do just as well as those without: Ten-year prospective data. Int Orthop. 2010;34:663–667. doi: 10.1007/s00264-009-0801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCalden RW, MacDonald SJ, Charron KD, Bourne RB, Naudie DD. The role of polyethylene design on postoperative TKA flexion: An analysis of 1534 cases. Clin Orthop Relat Res. 2010;468:108–114. doi: 10.1007/s11999-009-1127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaudhary R, Beaupre LA, Johnston DW. Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am. 2008;90:2579–2586. doi: 10.2106/JBJS.G.00995. [DOI] [PubMed] [Google Scholar]
- 31.Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: Balancing the gap. J Arthroplasty. 2002;17:813–819. doi: 10.1054/arth.2002.34814. [DOI] [PubMed] [Google Scholar]
- 32.Wohlrab D, Hube R, Zeh A, Hein W. Clinical and radiological results of high flex total knee arthroplasty: A 5 year follow-up. Arch Orthop Trauma Surg. 2009;129:21–24. doi: 10.1007/s00402-008-0665-z. [DOI] [PubMed] [Google Scholar]
- 33.Victor J, Banks S, Bellemans J. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: A prospective randomised outcome study. J Bone Joint Surg Br. 2005;87:646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 34.Zeh A, Davis J, Laskin R, Klima S, Wohlrab D. Early results with the Genesis II Posterior Stabilized High Flexion knee prosthesis. A one year follow-up study. Acta Orthop Belg. 2009;75:792–800. [PubMed] [Google Scholar]
- 35.Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:349–353. doi: 10.1016/j.arth.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 36.Hasegawa M, Sudo A, Uchida A. Staged bilateral mobile-bearing and fixed-bearing total knee arthroplasty in the same patients: A prospective comparison of a posterior-stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc. 2009;17:237–243. doi: 10.1007/s00167-008-0662-3. [DOI] [PubMed] [Google Scholar]
- 37.Watanabe T, Muneta T, Ishizuki M. Is a minimally invasive approach superior to a conventional approach for total knee arthroplasty? Early outcome and 2- to 4-year follow-up. J Orthop Sci. 2009;14:589–595. doi: 10.1007/s00776-009-1383-2. [DOI] [PubMed] [Google Scholar]
- 38.Maloney WJ, Schurman DJ (1992) The effects of implant design on range of motion after total knee arthroplasty. Total condylar versus posterior stabilized total condylar designs. Clin Orthop Relat Res 278:147–152 [PubMed]
- 39.Bozic KJ, Kinder J, Meneghini RM, Zurakowski D, Rosenberg AG, Galante JO (2005) Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res 430:117–124 [DOI] [PubMed]
- 40.W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients. Acta Orthop. 2010;81:161–164. doi: 10.3109/17453670903413186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schurman DJ, Rojer DE (2005) Total knee arthroplasty: Range of motion across five systems. Clin Orthop Relat Res 430:132–137 [PubMed]
- 42.Ahmed I, Gray AC, Linden M, Nutton R. Range of flexion after primary tka: The effect of soft tissue release and implant design. Orthopedics. 2009;32:811. doi: 10.3928/01477447-20090922-13. [DOI] [PubMed] [Google Scholar]
- 43.Ranawat CS (2003) Design may be counterproductive for optimizing flexion after TKR. Clin Orthop Relat Res 416:174–176 [DOI] [PubMed]
- 44.Nagura T, Dyrby CO, Alexander EJ, Andriacchi TP. Mechanical loads at the knee joint during deep flexion. J Orthop Res. 2002;20:881–886. doi: 10.1016/S0736-0266(01)00178-4. [DOI] [PubMed] [Google Scholar]
- 45.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89:1457–1461. doi: 10.1302/0301-620X.89B11.19840. [DOI] [PubMed] [Google Scholar]
- 46.Sharma A, Komistek RD, Scuderi GR, Cates HE., Jr High-flexion TKA designs: What are their in vivo contact mechanics? Clin Orthop Relat Res. 2007;464:117–126. doi: 10.1097/BLO.0b013e318157e478. [DOI] [PubMed] [Google Scholar]
- 47.Moynihan AL, Varadarajan KM, Hanson GR, Park SE, Nha KW, Suggs JF, Johnson T, Li G. In vivo knee kinematics during high flexion after a posterior-substituting total knee arthroplasty. Int Orthop. 2010;34:497–503. doi: 10.1007/s00264-009-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakayama K, Matsuda S, Miura H, Iwamoto Y, Higaki H, Otsuka K. Contact stress at the post-cam mechanism in posterior-stabilised total knee arthroplasty. J Bone Joint Surg Br. 2005;87:483–488. doi: 10.1302/0301-620X.87B4.15684. [DOI] [PubMed] [Google Scholar]
- 49.Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ. Measuring flexion in knee arthroplasty patients. J Arthroplasty. 2004;19:369–372. doi: 10.1016/j.arth.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 50.Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am. 2003;85-A:127–1285. doi: 10.2106/00004623-200307000-00014. [DOI] [PubMed] [Google Scholar]