Abstract
Bone transport can be performed with an external fixator alone or with the monorail technique which entails the combination of a fixator and an intramedullary nail. The purpose of this study was to compare the complication rates and long-term outcomes of these methods. Two groups of patients, the external fixator (n = 21) and the monorail group (n = 18), were compared. The average follow-up period was 7.9 ± 5.6 years and the mean defect length 8.3 ± 3.1 cm. Healing was achieved in 19 (90%) and 13 (72%) of the fixator and monorail patients, respectively. Six patients underwent amputations because of persistent infections (two in the fixator and four in the monorail group). The rate of deformities was significantly higher in the fixator group (p = 0.049). No statistically significant difference was found when comparing categories of the SF-36 test or the ability to work or do sports. The main advantages of the monorail method are reduction of the external fixation time and the lower rate of deformities. However, the authors recommend segmental transport with external fixator in patients with chronic infections.
Introduction
Management of long bone defects in the lower extremity has always been challenging for the orthopaedic surgeon. Most often segmental bone defects are reconstructed by transplantation of vascularised or non vascularised autogeneous bone, allograft bone transplantation, or segment transport [1–3].
Advantages of free vascularised bone grafts include the ability to treat concomitant soft tissue defects by osteocutaneous flaps and provide better resistance to infections [4–6]. However, problems with vascularised bone grafts include donor site morbidity, possibility of necrosis due to anastomotic complications, long remodelling time and high fracture rate [7–10]. The advantages of bone transport include minimal soft tissue trauma, treatment of large bone defects with regenerate of the same diameter and elimination of donor site morbidity [1, 11, 12]. On the other hand, bone transport using external fixators alone, as first introduced by Ilizarov, requires long-term treatment with external fixators [13]. Complications are very common, including pin tract infections, joint stiffness, malalignment and refractures [14, 15]. The treatment of choice depends on many factors such as vascularity, location, size and aetiology of the defect. Further factors that should be taken into consideration include the patient’s age, comorbidities, immunosupression, smoking and general health.
In 1992, Raschke et al. [16] described a technique of segmental transport over an intramedullary nail to provide a more comfortable bone transport process, to shorten the external fixation period, and to provide internal support for the regenerated bone. This technique is gaining wider acceptance because of the improvement in patient comfort. Two important drawbacks of this procedure are the inability to correct associated complex deformities and the risk of introducing infections especially from pin tracts into the medullary cavity.
The purpose of this study was to answer the following questions: (1) What are the advantages/disadvantages of the one method compared to the other? (2) Is the future quality of life and the ability to work or do sports influenced by the method by which the tibial bone defects are treated? (3) How could the amputation rates be reduced? To the best of our knowledge, there are no large studies comparing the two methods.
Patients and methods
We retrospectively analysed the charts and radiographs of 39 adult patients who underwent segmental tibial bone transport between 1992 and 2007 in our institution. The patients were divided into two groups. The first group (n = 21) had segmental bone transport using only an external ring fixator and the second (n = 18) was treated with the monorail technique. Criteria for inclusion included all adult patients with a greater than 3-cm post-traumatic segmental bone defect of the tibia and a minimum follow-up of two years. The medical records were reviewed to determine the patient’s gender, age, location and size of the defect, the presence of chronic infection defined by positive cultures for more than two months preoperatively, the number of previous operations, smoking habits and complications such as deformities, persistent infections, amputations and bone regeneration insufficiency. Deformities were defined as pathological angulation of 5° or more according to the classification of Paley et al. [17].
All patients received a questionnaire including the SF-36 Health Survey questionnaire with the following additional questions: (1) Are you satisfied with the procedure or would you prefer a primary amputation? (2) Have you returned to your original profession or have you changed profession? (3) Have you resumed sport activities?
Two patients were lost from follow-up. The mean age of the patients in the fixator group was 46.6 ± 14.7 years and 46.7 ± 14.0 years (p = 0.982) in the monorail group (Table 1). Twenty-eight percent of the monorail and 22% of the fixator patients were females ( p = 0.777). The defect length measured 8.1 ± 2.8 cm in the fixator group and 8.5 ± 3.4 cm ( p = 0.653) in the monorail group. Twenty-two percent of the monorail and 29% of the external fixator patients were smokers. The average clinical and radiological follow-up was 7.9 ± 5.6 years.
Table 1.
Preoperative data show that both groups are comparable
| Demographics | Fixator group (n = 21) | Monorail group (n = 18) | P value |
|---|---|---|---|
| Age in years | 46.6 ± 14.7 | 46.7 ± 14.0 | 0.982 |
| Defect length in cm | 8.1 ± 2.8 | 8.5 ± 3.4 | 0.653 |
| Chronic osteitis | 12 | 10 | 0.921 |
| Female gender | 5 | 5 | 0.777 |
| Right side | 11 | 7 | 0.523 |
| Open fractures | 16 | 13 | 0.959 |
| Nicotine abuse | 6 | 4 | 0.726 |
| Operations prior to bone transport | 5.7 ± 2.2 | 4.3 ± 2.9 | 0.112 |
Fourteen patients (67%) in the external fixator group and ten (56%) in the monorail group had chronic osteitis prior to segment transport (p = 0.921). History of open fractures was present in 76% and 72% of the external fixator and monorail patients, respectively. In the fixator group, more operative procedures had been performed prior to the segment transport compared to the monorail group (external fixator group 5.7 ± 2.2, monorail group 4.3 ± 2.9, p = 0.112).
Using the monorail technique an osteotomy was performed with an osteotome and an antegrade intramedullary nail was inserted and statically locked. Two Schanz screws were inserted proximal to the level of the osteotomy site and two distal to it on the segment to be transported. A contact of the nail with the Schanz screws was avoided in order to prevent spreading of pin tract infections along the intramedullary nail. In the fixator group a three ring circular external fixator was applied before the corticotomy. Distraction was started in both groups on the fifth postoperative day at a rate of 1 mm/day [18, 19].
Statistical analysis
Statistical significance was evaluated between the different groups using Mann–Whitney U test and Student’s two tailed t-test for continuous data, and Fisher's exact test and Pearson chi-square were used for categorical values. A p value ≤0.05 (two tailed) was considered to be statistically significant. All statistical analyses were performed using SPSS (SPSS 15.0, SPSS Inc., Chicago, IL, USA). All values are presented in the form of mean ± SD (standard deviation).
Results
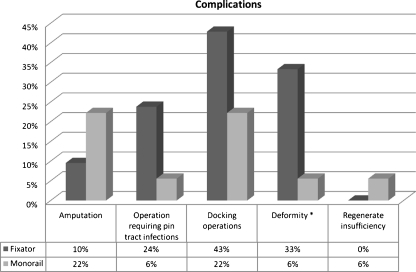
The external fixator was applied for 15.9 ± 6.1 months in the external fixator group and for 5.9 ± 1.5 months in the monorail group (p < 0.0001). The treatment was successful in 19 patients (90%) in the fixator group and 13 patients (72%) in the monorail group (p = 0.215). Failure of the treatment culminated in amputation in six cases (two in the fixator and four in the monorail group) and insufficient bone regenerate in one case (monorail group). The rate of deformities (>5°) was significantly higher in the fixator group (33% vs. 6%, p = 0.049, Table 2, Fig. 1).
Table 2.
Results
| Parameter | Fixator group (n = 21) | Monorail group (n = 18) | P value |
|---|---|---|---|
| Healing | 19 | 13 | 0.215 |
| Amputation | 2 | 4 | 0.387 |
| Regenerate Insufficiency | 0 | 1 | 0.462 |
| Deformity | 7 | 1 | 0.049* |
| Number of additional surgical procedures | 3.4 ± 3.2 | 3.3 ± 3.9 | 0.967 |
| Pin tract infections that require operation | 5 | 1 | 0.190 |
| Docking operations | 9 | 4 | 0.307 |
| External fixation time in months | 15.9 ± 6.1 | 5.9 ± 1.5 | <0.0001* |
| SF-36 | |||
| Physical functioning | 66.6 | 55.6 | 0.084 |
| Physical pole functioning | 41.7 | 48.9 | 0.496 |
| Bodily pain | 64.2 | 60.4 | 0.687 |
| General health | 66.4 | 58.8 | 0.588 |
| Vitality | 59.4 | 53.3 | 0.857 |
| Social functioning | 73.5 | 67.7 | 0.879 |
| Role emotional | 77.6 | 78.5 | 0.361 |
| Mental health | 74.4 | 69.2 | 0.916 |
| Employment status | |||
| Patients that returned to work | 13 | 11 | 0.959 |
| Returned to their original employment | 6 | 6 | 0.748 |
| Ability to do sports | |||
| Major | 0 | 2 | 0.206 |
| Minor | 9 | 9 | 0.752 |
| None | 12 | 7 | 0.341 |
* Statistically significant (p < 0.05)
Fig. 1.
Rates of complications in both groups (*statistical significance)
The mean number of additional surgical procedures was 3.4 per patient (range, 0–11) in the external fixator group and 3.3 (range, 0–14) in the monorail group (p = 0.967). Surgical procedures after bone transport included the following: plating of the docking site (n = 13), corrective osteotomies (n = 5), transtibial amputations (n = 4), transfemoral amputations (n = 2), talotibial fusion (n = 6), debridements (n = 39), arthrolysis of knee joint (n = 5), knee endoprosthesis (n = 2), skin grafting or myocutaneous flap (n = 2), ORIF of refractures (n = 2), placement of new pins (n = 6) and partial diaphyseal tibial replacement (n = 1). A docking operation was performed in nine patients in the external fixator group and in four patients in the monorail group (p = 0.307). Five patients had debridement for pin tract infections in the fixator group and one in the monorail group (p = 0.190).
Four patients of the monorail group and two of the fixator group had amputations due to persistent bone infections. Two of the amputated monorail patients and one of the external fixator patients were smokers. Insufficient callus regenerate was observed in one 49-year-old patient in the monorail group. This patient was a heavy smoker, which presents one of the most serious risk factors for this complication [20]. The transport index was 0.5 mm/day. Taking into account the age, the noncompliance and the absolute absence of bone vitality in the SPECT/CT we treated the patient with a partial diaphyseal tibial replacement (Fig. 2).
Fig. 2.
Anteroposterior and lateral radiographs after partial diaphyseal replacement because of insufficient callus regenerate
The results of the SF-36 Health Survey showed the following mean scores for the external fixator group / monorail group, respectively: 66.6/ 55.6 (p = 0.084) for physical functioning, 41.7/ 48.9 (p = 0.496) for physical role functioning, 64.2/ 60.4 (p = 0.687) for bodily pain, 66.4/ 58.8 (p = 0.588) for general health, 59.4/ 53.3 (p = 0.857) for vitality, 73.5/ 67.7 (p = 0.879) for social functioning, 77.6/ 78.5 (p = 0.361) for role emotional, and 74.4/ 69.2 ( p = 0.916) for mental health. There was no statistically significant difference between the study groups in all categories of the SF-36.
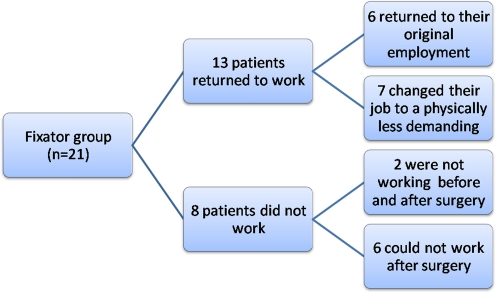
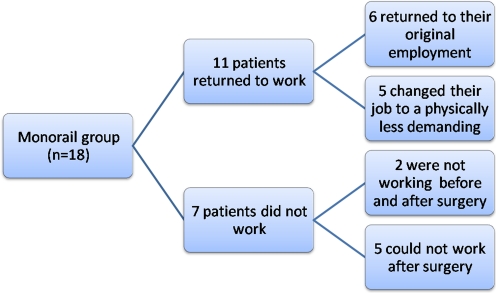
Thirteen patients of the external fixator group (62%) returned to work. Six of them returned to their original employment and seven returned to a physically less demanding profession. Two patients were not working before or after the surgery and six could not work after surgery (Fig. 3). Seven patients had a physically very demanding profession, e.g. fireman or farmer. One of them returned to his original employment, four returned to a less demanding job, whereas two could not work after surgery. Eleven patients in the monorail group (61%) returned to work including six patients returning to their original employment and five returning to a physically less demanding job. Two patients were not working pre- and postoperatively (Fig. 4). Seven patients had a physically demanding profession and three of them could not work postoperatively. Two returned to their original profession and two changed their jobs to a less demanding one.
Fig. 3.
Employment status after surgery in the external fixator group
Fig. 4.
Employment status after surgery in the monorail group
We classified the sporting activities of our patients into three categories: major (e.g. football, basketball, tennis), minor (cycling, jogging, swimming) and none. Nine patients (43%) in the external fixator group and nine patients (50%) in the monorail group resumed minor sporting activities (p = 0.752). Only two monorail patients were practising major sport activities.
All patients found the appearance of their limb acceptable. In the external fixator group 92.3% would undergo this reconstructive procedure again compared to 91.7% of the monorail patients.
Discussion
The main advantages of the monorail method for the treatment of segmental bone defects in this study were the significant reduction of time for external fixation and the significantly lower rate of deformities. Patients with external fixators only had the same healing rate and the same quality of life scores compared to patients treated with the monorail technique.
The significant reduction of deformities in the monorail group can be explained by the statically locked intramedullary nail, which maintains anatomical length and alignment during segment transport and consolidation [13].
The number of operations on the docking site was nine in the external fixator group and four in the monorail group (Fig. 1, Table 2). In case of delayed union at the docking site, removal of locking bolts or dynamisation of the external fixator was done. If insufficient healing was observed, debridement and plate osteosynthesis was indicated [21].
Two amputations were performed in 12 patients with chronic osteomyelitis (17%) in the external fixator group and four amputations out of ten patients with osteomyelitis (40%) in the monorail group. The authors believe that the risk of expanding an infection into the medullary cavity increases with the insertion of the intramedullary nail. Furthermore, pin tract infections may spread more easily along intramedullary implants [17]. The authors conclude that patients with preoperative chronic infections should be treated with external fixators only.
The rate of insufficient bone regeneration was not significantly different after segment transport by either method. This contradicts the hypothesis that consolidation of the newly regenerated bone is reduced by damage to the endosteal blood supply by nailing. Paley et al. found similar results when comparing patients who underwent lengthening using either external fixators alone or with an intramedullary nail. They suggested that the effect of revascularisation after reaming and better stability provided by the intramedullary nail with earlier functional loading compensated for any damage to the medullary vascularisation [22].
The high rate of unemployment after bone transport by both methods is thought to be due to the severe trauma and not the procedure itself. Gopal et al. studied the outcome of patients with open tibial fractures (Gustilo grade IIIb or IIIc) and found that only 40% of them returned to work [23].
One limitation of our study is that associated injuries affect the final functional outcome and can alter the results of the SF-36 Health Survey. For example, a patient with transtibial amputation had a physical functioning score of 67, whereas another with a contralateral pilon fracture had a physical functioning score of 59 despite good healing of the extremity treated with bone transport. Most of the physical disability of the first patient was caused by the post-traumatic ankle osteoarthritis and not the extremity with the bone transport, which has been without significant symptoms.
Considering the lower rate of postoperative infections and amputations in the external fixator group, the authors recommend segment transport by external fixator in patients with chronic infections.
To our knowledge, this is the first large study comparing the monorail method with external fixators for the treatment of bone defects in the lower extremity. This entity cannot be compared with studies about simple lengthening of the lower limb [22, 24] because of the posttraumatic aetiology, high chronic infection rate and more difficult surgical technique.
Conclusion
The use of the monorail technique for segmental bone transport reduces the rate of deformities of the lower limb and the external fixation time. On the other hand, healing rates, return to profession, sports activities and quality of life are comparable after segment transport with the monorail or external fixator technique. Finally, chronic infections should be treated with external fixators only because of a lower rate of reinfection and amputations.
Acknowledgments
Conflict of interest statement There was no financial support for this study. None of the authors have received or will receive benefits for professional or personal use from a commercial party related directly or indirectly to the subject of this article.
Footnotes
Each author certifies that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical Board Review approval was obtained for this study (#644 – 05/01/2010).
References
- 1.Cierny G, 3rd, Zorn KE. Segmental tibial defects. Comparing conventional and Ilizarov methodologies. Clin Orthop Relat Res. 1994;301:118–123. [PubMed] [Google Scholar]
- 2.Mankin HJ, Doppelt S, Tomford W. Clinical experience with allograft implantation. The first ten years. Clin Orthop Relat Res. 1983;174:69–86. [PubMed] [Google Scholar]
- 3.Mekhail AO, Abraham E, Gruber B, Gonzalez M. Bone transport in the management of posttraumatic bone defects in the lower extremity. J Trauma. 2004;56(2):368–378. doi: 10.1097/01.TA.0000057234.48501.30. [DOI] [PubMed] [Google Scholar]
- 4.Doi K, Kawakami F, Hiura Y, Oda T, Sakai K, Kawai S. One-stage treatment of infected bone defects of the tibia with skin loss by free vascularized osteocutaneous grafts. Microsurgery. 1995;16(10):704–712. doi: 10.1002/micr.1920161009. [DOI] [PubMed] [Google Scholar]
- 5.El-Gammal TA, El-Sayed A, Kotb MM. Microsurgical reconstruction of lower limb bone defects following tumor resection using vascularized fibula osteoseptocutaneous flap. Microsurgery. 2002;22(5):193–198. doi: 10.1002/micr.22501. [DOI] [PubMed] [Google Scholar]
- 6.El-Alfy B, El-Mowafi H, El-Moghazy N. Distraction osteogenesis in management of composite bone and soft tissue defects. Int Orthop. 2010;34(1):115–118. doi: 10.1007/s00264-008-0574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benacquista T, Kasabian AK, Karp NS. The fate of lower extremities with failed free flaps. Plast Reconstr Surg. 1996;98(5):834–840. doi: 10.1097/00006534-199610000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Chew WY, Low CK, Tan SK. Long-term results of free vascularized fibular graft. A clinical and radiographic evaluation. Clin Orthop Relat Res. 1995;311:258–261. [PubMed] [Google Scholar]
- 9.El-Gammal TA, Shiha AE, El-Deen MA, El-Sayed A, Kotb MM, Addosooki AI, Ragheb YF, Saleh WR. Management of traumatic tibial defects using free vascularized fibula or ilizarov bone transport: A comparative study. Microsurgery. 2008;28(5):339–346. doi: 10.1002/micr.20501. [DOI] [PubMed] [Google Scholar]
- 10.Minami A, Kimura T, Matsumoto O, Kutsumi K. Fracture through united vascularized bone grafts. J Reconstr Microsurg. 1993;9(3):227–232. doi: 10.1055/s-2007-1006649. [DOI] [PubMed] [Google Scholar]
- 11.Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res. 1994;301:111–117. [PubMed] [Google Scholar]
- 12.Marsh JL, Prokuski L, Biermann JS. Chronic infected tibial nonunions with bone loss. Conventional techniques versus bone transport. Clin Orthop Relat Res. 1994;301:139–146. [PubMed] [Google Scholar]
- 13.Song HR, Cho SH, Koo KH, Jeong ST, Park YJ, Ko JH. Tibial bone defects treated by internal bone transport using the Ilizarov method. Int Orthop. 1998;22(5):293–297. doi: 10.1007/s002640050263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wani N, Baba A, Kangoo K, Mir M (2010) Role of early Ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. Int Orthop. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 15.Lovisetti G, Sala F, Thabet AM, Catagni MA, Singh S (2010) Osteocutaneous thermal necrosis of the leg salvaged by TSF/Ilizarov reconstruction. Report of 7 patients. Int Orthop. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 16.Raschke MJ, Mann JW, Oedekoven G, Claudi BF. Segmental transport after unreamed intramedullary nailing. Preliminary report of a "Monorail" system. Clin Orthop Relat Res. 1992;282:233–240. [PubMed] [Google Scholar]
- 17.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 18.Liodakis E, Kenawey M, Krettek C, Ettinger M, Jagodzinski M, Hankemeier S (2010) Segmental transports for posttraumatic lower extremity bone defects: are femoral bone transports safer than tibial? Arch Orthop Trauma. [Epub ahead of print] [DOI] [PubMed]
- 19.Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am. 2006;88(10):2137–2145. doi: 10.2106/JBJS.E.01152. [DOI] [PubMed] [Google Scholar]
- 20.Kenawey M, Krettek C, Liodakis E, Meller R, Hankemeier S (2010) Insufficient bone regenerate after intramedullary femoral lengthening: risk factors and classification system. Clin Orthop Relat Res. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 21.Oh CW, Song HR, Roh JY, Oh JK, Min WK, Kyung HS, Kim JW, Kim PT, Ihn JC. Bone transport over an intramedullary nail for reconstruction of long bone defects in tibia. Arch Orthop Trauma Surg. 2008;128(8):801–808. doi: 10.1007/s00402-007-0491-8. [DOI] [PubMed] [Google Scholar]
- 22.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Jt Surg Am. 1997;79(10):1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Gopal S, Giannoudis PV, Murray A, Matthews SJ, Smith RM. The functional outcome of severe, open tibial fractures managed with early fixation and flap coverage. J Bone Joint Surg Br. 2004;86(6):861–867. doi: 10.1302/0301-620X.86B6.13400. [DOI] [PubMed] [Google Scholar]
- 24.Watanabe K, Tsuchiya H, Sakurakichi K, Yamamoto N, Kabata T, Tomita K. Tibial lengthening over an intramedullary nail. J Orthop Sci. 2005;10(5):480–485. doi: 10.1007/s00776-005-0939-z. [DOI] [PubMed] [Google Scholar]