Abstract
Correct placement of iliosacral screws remains a surgical challenge. The aim of this retrospective study was to identify parameters which impact the accuracy of this technically demanding procedure. Eighty-two patients with vertically unstable pelvic injuries treated with a total of 147 iliosacral screws were included. Assessment of postoperative CT scans revealed screw misplacement in 13 cases (8%), of which six occurred following insertion of two unilateral screws into S1. Six screw misplacements occurred in patients with dislocation injuries of the posterior pelvis. Comparison of a navigated and the standard technique revealed a decreased screw misplacement rate in the navigated group (15% standard vs. 3% navigation, p < 0.05). In addition, the malposition rate was influenced by the surgeon’s individual experience (20% for low vs. 3.9% for high volume surgeons, p < 0.05). Overall, the accuracy of iliosacral screw placement depends on the number of screws inserted into S1 and the extent of dislocation. In experienced hands, the use of navigation represents a helpful tool to improve the placement accuracy.
Introduction
Over the last decade, advances in computer-assisted surgery for the treatment of skeletal injuries have paved the way for the establishment of navigation systems for pedicle screw instrumentation of vertebral fractures [1, 2]. Experimental and clinical data suggest that the use of navigated pedicle screw instrumentation can result in a more accurate screw placement and lower fluoroscopic exposure time compared to non-navigated standard instrumentation [3, 4].
More recently, a number of reports also proposed navigated procedures for fixation of unstable pelvic ring injuries, predominantly of the posterior pelvis [5–7]. The current standard for treatment of those injuries is the percutaneous iliosacral screw fixation using fluoroscopic techniques according to Matta and Saucedo [8]. This technique, which was pioneered in the prone position, was later modified, allowing its use in the supine position with or without a percutaneous approach. Due to the relatively high misplacement rates [9], navigated procedures were subsequently introduced to increase the safety of screw placement, especially when the percutaneous technique is used [10, 11].
Few reports exist regarding the use of navigation for pelvic injury. Furthermore, the influence of fracture patterns and surgeon experience has yet to be evaluated. The aim of this study was to identify parameters that affect the accuracy of iliosacral screw placement in trauma patients. Special focus was placed on the surgeon’s individual experience, the use of navigated techniques, and patterns of injury.
Materials and methods
Study design
Case records from a consecutive series of patients with unstable pelvic fractures, admitted between January 2002 and August 2007 and treated with iliosacral screws, were reviewed retrospectively. Initial anteroposterior radiographs and CT scans were obtained and fracture classification was performed according to the Orthopaedic Trauma Association (OTA).
Patient demographic data, additional osteosynthetic procedures (e.g. anterior pelvic fixation), duration of surgery (incision to closure time) and fluoroscopic exposure times were determined in all patients with vertically unstable pelvic fracture (OTA type 61-C). The accuracy of screw placement was assessed postoperatively by a procedure blinded radiologist using a standardised CT-protocol (140 kV, 40 mAs, Collimation 3 mm, Pitch 0.7; Somatom Volume Zoom, Siemens) with a 16-slice spiral CT (XM 8000, Philips). Cross-sectional, sagittal and coronal views were obtained from each patient. Malposition was defined as any screw penetration of the bony cortices, regardless of the direction of the penetration (spinal canal, neuroforamen, intervertebral L5/S1, ventral penetration); on the other hand, correct screw placement was defined as a complete intercortical screw position.
The influence of navigation on the screw positioning was assessed by comparison of screw misplacement rates in patients treated using navigation or by standard procedure. To evaluate the impact of individual experience, low (1–20 screws) and high (>100 screws) volume surgeons were defined retrospectively and screw misplacement rate was compared between these two groups. All procedures of the navigated group were performed by just one surgeon, who also represents the high volume surgeon in this study. After introduction of the navigated procedure to our institution in 2005, this surgeon used the navigated procedure in all his cases involved in this study.
Operative procedures
An open reduction in prone position was performed in all cases of sagittal and vertical dislocated fracture types. Undislocated or slightly vertically dislocated fracture types were treated percutaneously supine and cases of bilateral fracture percutaneously prone. Navigation was performed with the Stryker Navigation System (Stryker-Leibinger, Freiburg, Germany) and the two-dimensional C-arm fluoroscope „Exposcop 8000“ (Ziehm Imaging GmbH, Nürnberg, Germany).
Prior to the navigated procedure, the C-arm was calibrated, provided with a tracker, and connected to the navigation system. The dynamic reference was attached to the iliac spine and validated. Subsequently, the three standard views of the pelvis (inlet, outlet, lateral) were obtained. The calibration of the drill sleeve completed the preoperative setting. The navigation system was used to define the correct approach for skin incision and to pilot the guide wire placement.
To avoid a mismatch between virtual imaging and real guide wire placement, we performed three single C-arm shots corresponding to the standard views to verify the correct placement of the guide wire. The control imaging was repeated three times during guide wire placement: first, after penetration of the lateral cortical iliac wall, second, after reaching the sacral ala and third, after placement in the sacral vertebral body. In case of correct guide wire placement, the length of the screw was measured and, after overdrilling the guide wire, the cannulated screw was inserted. Cannulated titanium screws with a 7.3-mm-diameter were inserted (Synthes, Umkirch, Germany), usually short-threaded (16-mm length) via 2.8-mm guide wires.
Statistical analysis
All data are given as mean value ± standard deviation and range. Differences between the non-navigated and the navigated techniques were evaluated by a standard t-test. If the sample data were not normally distributed, the Mann–Whitney rank sum test was used instead. Fisher’s exact test was used to detect differences between the groups regarding the screw misplacement rate. All tests were calculated with a desired power of β = 0.8 and a significance level of α = 0.05. Statistical analysis was performed with SigmaStat (version 2.03) by SPSS (SPSS, Inc., Chicago, IL).
Results
The study group included 82 patients with unstable pelvic fractures of the posterior pelvic ring (OTA type 61-C) in which the posterior injury was treated with iliosacral screw fixation. The group consisted of 52 females and 30 males with an average age of 49.7 ± 20.6 years (range, 13–87). Overall, 147 iliosacral screws were implanted, procedural time per screw was 37.5 ± 23.3 minutes (range, 12.5–199) and fluoroscopic time per screw was 83.3 ± 46.5 seconds (range, 15–354). Additional stabilisation procedures were performed for anterior pelvic ring and acetabular instabilities (Table 1).
Table 1.
Overall procedures performed for acetabular and pelvic ring stabilization
| Additional procedures | Standard supine | Standard prone | Navigation supine | Navigation prone |
|---|---|---|---|---|
| Percutaneous (N = 19) | Open (N = 17) | Percutaneous (N = 38) | Open (N = 8) | |
| Symphysis plate (n) | 0 | 3 | 6 | 1 |
| External fixateur (n) | 7 | 2 | 9 | 0 |
| Posterior banding (n) | 0 | 3 | 3 | 4 |
| Acetabular osteosynthesis (n) | 0 | 1 | 0 | 0 |
Assessment of postoperative CT scans revealed a malposition of iliosacral screws in 8.8% (n = 13/147, Table 2). Five cases required revision of screw position. Altogether, in 38 patients two screws were inserted unilaterally into S1. Using this technique, six screw misplacements were observed. A relatively high incidence of screw malposition was observed in patients with dislocation injuries of the posterior pelvis requiring open reduction in the prone position (6 of 45 screws). In four of these cases a unilateral insertion of two screws into S1 was performed at the same time.
Table 2.
Occurrence of screw malpositions
| Malposition | Standard supine | Standard prone | Navigation supine | Navigation prone |
|---|---|---|---|---|
| Neuroforamen | 2(R) | 3* | 2** | - |
| Spinal canal | 1(R) | 2**(RR) | - | - |
| Intervertebral L5/S1 | - | 1* | - | - |
| Ventral penetration | 1(R) | - | 1 | - |
| Total (n) | 4 | 6 | 3 | - |
(R) revision was performed; * two screws unilateral into S1
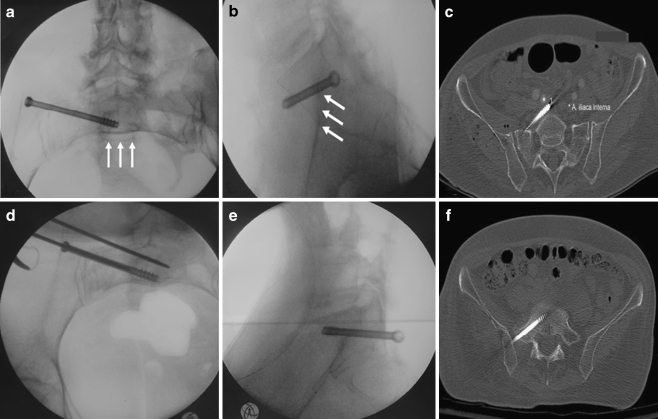
One further misplaced screw was related to misinterpretation of the lateral C-arm view intraoperatively. The patient, suffering from an OTA type 61-C1 fracture, was stabilised with one screw in the standard supine technique. Postoperative CT scan revealed an anterior cortical penetration of the screw tip close to the iliac vessels. The screw provided insufficient fixation and was subsequently replaced in the prone position (Fig. 1).
Fig. 1.
Case study of the standard procedure. a Intraoperative inlet projection, at first view suggesting correct placement of the screw; arrows indicate the lower ventral margin of the first sacral vertebra (S1), demonstrating insufficient adjustment of the inlet view. b Lateral view also obtained intraoperatively; screw tip outside S1; arrows showing the “iliac cortical density” (ICD). c Postoperative CT scan revealing ventral misplacement of the screw, closely located to the internal iliac artery (*). d Inlet view during revision surgery; guide pin parallel to the misplaced screw with dorsal correction. e Lateral view, indicating regular placement of the exchanged screw. f CT scan after screw correction
Six surgeons implanted 147 screws. One hundred and two were implanted by a single surgeon whereas the remaining five surgeons inserted 45 screws (maximum per surgeon 18 screws). We found a malposition rate of 20% for low volume surgeons in contrast to a malposition rate of only 3.9% for the most experienced surgeon (Table 3). Using the navigated technique, no severe misplacement requiring revision was found. In the entire study, population navigation revealed a significant decrease of screw malpositioning (15% standard vs. 3% navigated, p < 0.05, ß = 0.5), an increase of procedure time and a reduction of fluoroscopic exposure time (Table 4).
Table 3.
Malpositioning rate referenced to low and high volume surgeons
| Individual experience | Malposition rate (n) |
|---|---|
| High volume surgeons (N = 1) (> 100 screws) |
4/102 (3.9%)* |
| Low volume surgeons (N = 5) (< 20 screws each) |
9/45 (20%) |
| Malposition overall | 13/147 (8.8%) |
*p < 0.05 vs. low volume surgeons, ß = 0.7
Table 4.
Features of standard and navigated iliosacral screw placement (data given per screw). Image converter time involves every C-arm shot taken intraoperatively. Dose of radiation exposure: 42.5 mGy/min
| Features | Standard | Navigation | P values |
|---|---|---|---|
| Surgeons, N = 6 | Surgeons, N = 1 | ||
| Malposition rate | 15.4% (n = 10/65) | 3.6% (n = 3/82) | p < 0.05 (ß = 0.5) |
| Procedure time (min) | 29.4 ± 12.9 (12.5–75) | 39.2 ± 22.2 (15–199) | p < 0.01 (ß = 0.8) |
| Image converter time (s) | 103.1 ± 46.6 (18–354) | 62.8 ± 30 (15–156) | p < 0.001 (ß = 1.0) |
Discussion
Iliosacral screws are indispensable tools for the surgical stabilisation of posterior pelvic injuries [8]. Screws can be inserted via an open approach in the prone position, or percutaneously in the supine position. The percutaneous procedure is considered to be technically challenging and is associated with high screw misplacement rates of up to 24% [9].
Our study demonstrates a misplacement rate of 8%, which is in line with previous findings [12–14]. However, in comparison to other surgical procedures this misplacement rate is still unacceptably high. We therefore sought to determine which procedure-related parameters influence the screw misplacement rate during stabilisation of posterior pelvic injuries.
Our data suggest that the experience level of the surgeon significantly impacts the screw misplacement rate. We found a five-fold higher malposition rate for low volume surgeons as compared to the single high volume surgeon. Although the group of high volume surgeons consists of only one surgeon, perhaps limiting the overall interpretation, it implicates that training can help to reduce the complication rate. Further prospective studies would be useful to confirm this finding.
Misinterpretation of the C-arm images, particularly in displaced and insufficiently reduced lesions, is a risk factor for screw misplacement that may result in injuries to blood vessels and nerve tracts. Our data indicate that the accurate acquisition of the Matta-projections by correct positioning of the C-arm and a detailed knowledge of the sacral anatomy are prerequisites for identifying the landmarks and the safe zone for screw insertion, particularly with regard to the “iliac cortical density” (ICD).
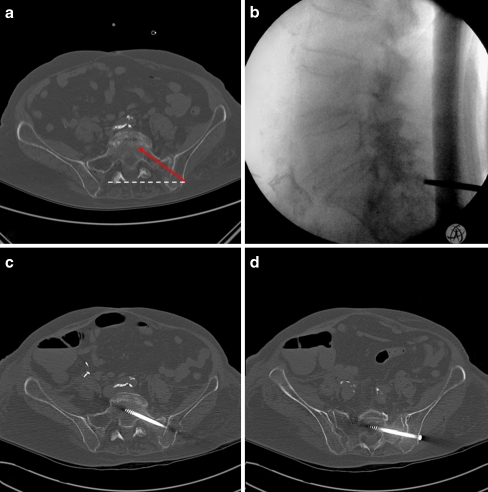
We postulate that a preoperative surgical plan, including an analysis of the preoperative pelvic CT scan showing the relationship between the iliac cortical density (ICD) and the sacral alar slope, is indispensable to reduce the rate of misplaced screws (Fig. 2). This view is further supported by a study of Routt et al. which demonstrated that an accurate lateral sacral view is necessary for safe iliosacral screw placement [13].
Fig. 2.
Preoperative planning for iliosacral screw placement. a Identification of the entry point to the safe iliosacral corridor (solid red line) with regard to the lateral aspect of the sacral spine (dashed white line). b Lateral C-arm view showing the corresponding starting point posterior to the spinal canal. c CT scan revealing a regular screw position to S1. d To enhance stability, a second screw was inserted to S2
Since bent guide wires are a possible cause of complication [15], we suggest placing the guide wire under image control at three different time points: after penetration of the lateral cortical iliac wall; after reaching the sacral ala; and after placement in the sacral vertebral body. These control images are also necessary when a navigation system is used, particularly to avoid a mismatch between virtual imaging and real guide wire position.
Our data support the notion that these procedures should only be performed under the supervision of highly experienced surgeons, particularly in dislocated fracture patterns where an insufficient reduction can endanger adjacent neural and vascular structures during screw placement [16].
The number of iliosacral screws required for stable fixation of the posterior pelvic ring is still a matter of controversy. Ebraheim et al. suggested that placement of one screw through the S1 pedicle is safer due to the relative low pedicle height and depth [17]. In our study we could confirm these findings, since the insertion of two unilateral screws into S1 was associated with a higher screw misplacement rate.
Alternative fixation methods should be considered in those cases where the insertion of two screws might be associated with a higher complication rate, such as low height of S1, fused vertebrae, etc. An additional ilioiliac tension band plate or, technically more demanding, a second screw into S2 are the treatment alternatives of choice in our centre to achieve sufficient fracture stabilisation and early mobilisation.
Recent studies propose computer-assisted procedures in pelvic surgery to reduce the risk of screw misplacement based on previous experiences in spinal surgery [5, 7]. Our study data suggest that the use of navigation is associated with a lower screw misplacement rate compared to the standard procedure. This has recently been confirmed by other studies [6, 18–21]. Placement precision may further be optimised by using 3D image converters. The findings of other study groups indicate that the misplacement rates of the 3D fluoroscopic navigated technique tend towards zero [22, 23].
However, although these data suggest a beneficial effect of navigation procedures, there is still the need for randomised controlled trials consisting of larger study subpopulations with similar fracture types and similarly experienced surgeons to prove the benefit of navigation with regard to the malposition rate.
Further, the use of navigation leads to a potential increase of costs and in the beginning a relevant learning curve has to be overcome [22]. We therefore recommend to restrict the use of navigation to a small team until the learning process has been completed [24]. We further recommend that an experimental trial of the navigated procedure prior to its clinical use be considered.
Conclusion
In summary, our experience from more than 140 iliosacral screws implanted over a five-year period suggests that:
The accuracy of iliosacral screw placement depends on the surgeon’s experience.
The use of navigation seems to provide a helpful tool to reduce the misplacement rate of iliosacral screws.
Unilateral insertion of two iliosacral screws into S1 increases the risk of screw malposition. Alternatively, placement of a second screw to S2 can be considered.
Inadequate identification of anatomical landmarks, especially those obtained from lateral C-arm imaging, is a further risk factor for screw malpositioning.
Screw malpositions occur more frequently in dislocation injuries requiring open reduction.
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- 1.Gebhard F, Weidner A, Liener UC, Stockle U, Arand M. Navigation at the spine. Injury. 2004;35(Suppl 1):35–45. doi: 10.1016/j.injury.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Troccaz J, et al. Computer-assisted spine surgery. Comput Aided Surg. 1998;3(6):297–305. doi: 10.3109/10929089809148150. [DOI] [PubMed] [Google Scholar]
- 3.Laine T, Schlenzka D, Makitalo K, Tallroth K, Nolte LP, Visarius H. Improved accuracy of pedicle screw insertion with computer-assisted surgery. A prospective clinical trial of 30 patients. Spine. 1997;22(11):1254–1258. doi: 10.1097/00007632-199706010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9(3):235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briem D, Linhart W, Lehmann W, Begemann PG, Adam G, Schumacher U, et al. Computer-assisted screw insertion into the first sacral vertebra using a three-dimensional image intensifier: results of a controlled experimental investigation. Eur Spine J. 2006;15(6):757–763. doi: 10.1007/s00586-005-0992-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grützner PA, Rose E, Vock B, Holz F, Nolte LP, Wentzensen A. Computer-assisted screw osteosynthesis of the posterior pelvic ring. Initial experiences with an image reconstruction based optoelectronic navigation system. Unfallchirurg. 2002;105(3):254–260. doi: 10.1007/s001130100339. [DOI] [PubMed] [Google Scholar]
- 7.Stockle U, Krettek C, Pohlemann T, Messmer P. Clinical applications—pelvis. Injury. 2004;35(Suppl 1):46–56. doi: 10.1016/j.injury.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Ortop. 1989;242:83–97. [PubMed] [Google Scholar]
- 9.Tonetti J, Carrat L, Blendea S, Merloz P, Troccaz J, Lavallee S, et al. Clinical results of percutaneous pelvic surgery. Computer assisted surgery using ultrasound compared to standard fluoroscopy. Comput Aided Surg. 2001;6(4):204–211. doi: 10.3109/10929080109146084. [DOI] [PubMed] [Google Scholar]
- 10.Gautier E, Bachler R, Heini PF, Nolte LP. Accuracy of computer-guided screw fixation of the sacroiliac joint. Clin Ortop. 2001;393:310–317. doi: 10.1097/00003086-200112000-00036. [DOI] [PubMed] [Google Scholar]
- 11.Stockle U, Konig B, Hofstetter R, Nolte LP, Haas NP. Navigation assisted by image conversion. An experimental study on pelvic screw fixation. Unfallchirurg. 2001;104(3):215–220. doi: 10.1007/s001130050717. [DOI] [PubMed] [Google Scholar]
- 12.Hinsche AF, Giannoudis PV, Smith RM. Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Ortop. 2002;395:135–144. doi: 10.1097/00003086-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Routt ML, Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997;11(8):584–589. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Templeman D, Goulet J, Duwelius PJ, Olson S, Davidson M. Internal fixation of displaced fractures of the sacrum. Clin Ortop. 1996;329:180–185. doi: 10.1097/00003086-199608000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Arand M, Kinzl L, Gebhard F. Sources of error and risks in CT based navigation. Orthopade. 2002;31(4):378–384. doi: 10.1007/s00132-001-0279-4. [DOI] [PubMed] [Google Scholar]
- 16.Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2003;17(2):88–94. doi: 10.1097/00005131-200302000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Ebraheim NA, Xu R, Biyani A, Nadaud MC. Morphologic considerations of the first sacral pedicle for iliosacral screw placement. Spine. 1997;22(8):841–846. doi: 10.1097/00007632-199704150-00002. [DOI] [PubMed] [Google Scholar]
- 18.Arand M, Kinzl L, Gebhard F. Computer-guidance in percutaneous screw stabilization of the iliosacral joint. Clin Ortop. 2004;422:201–207. doi: 10.1097/01.blo.0000128644.46013.08. [DOI] [PubMed] [Google Scholar]
- 19.Schep NW, Haverlag R, Vugt AB. Computer-assisted versus conventional surgery for insertion of 96 cannulated iliosacral screws in patients with postpartum pelvic pain. J Trauma. 2004;57(6):1299–1302. doi: 10.1097/01.TA.0000133573.53587.2E. [DOI] [PubMed] [Google Scholar]
- 20.Stockle U, Konig B, Dahne M, Raschke M, Haas NP. Computer assisted pelvic and acetabular surgery. Clinical experiences and indications. Unfallchirurg. 2002;105(10):886–892. doi: 10.1007/s00113-002-0438-z. [DOI] [PubMed] [Google Scholar]
- 21.Tonetti J, Carrat L, Blendea S, Troccaz J, Merloz LS, et al. Clinical validation of computer assisted pelvic surgery using ultrasound. A percutaneous safe technique with low radiation exposure. Stud Health Technol Inform. 2001;81:515–520. [PubMed] [Google Scholar]
- 22.Briem D, Linhart W, Bock T, Begemann PGC, Halata Z, Rueger JM, Windolf J. Computer-assisted screw placement into the posterior pelvic ring: assessment of different navigated procedures in a cadaver trial. Unfallchirurg. 2006;109(8):640–646. doi: 10.1007/s00113-006-1100-y. [DOI] [PubMed] [Google Scholar]
- 23.Hufner T, Geerling J, Gansslen A, Kendoff D, Citak C, Grutzner P, Krettek C. Computer-assisted surgery for pelvic injuries. Chirurg. 2004;75(10):961–966. doi: 10.1007/s00104-004-0945-2. [DOI] [PubMed] [Google Scholar]
- 24.Konrad G, Zwingmann J, Kotter E, Südkamp N, Oberst M. Variability of the screw position after 3D-navigated sacroiliac screw fixation. Influence of the surgeon's experience with the navigation technique. Unfallchirurg. 2010;113(1):29–35. doi: 10.1007/s00113-008-1546-1. [DOI] [PubMed] [Google Scholar]