Abstract
Objective: To investigate the effect of workers' compensation policies related to expedited surgical fees and private clinic surgical setting on disability duration among injured workers.
Methods: The study included 1,380 injured workers with knee meniscectomy between 2001 and 2005 in British Columbia. Using linked workers' compensation claim and surgery/clinical records, wait time for surgery (time from last surgical consult to surgery) and time from surgery to return to work were computed and compared for workers who received care in public versus private facilities, and according to whether their surgeons received fees intended to expedite care.
Results: The public expedited group had the shortest disability duration from surgical consult to return to work; the expedited fee reduced the surgery wait time (~2 work weeks), and surgeries performed in public hospitals had a shorter return-to-work time (~1 work week).
Discussion: An overall difference of approximately three work weeks in disability duration may have meaningful clinical and quality-of-life implications for injured workers. However, minimal differences in expedited surgical wait times by private clinics versus public hospitals, and small differences in return-to-work outcomes favouring the public hospital group, suggest that a future economic evaluation of workers' compensation policies related to surgical setting is warranted.
Abstract
Objectif : Étudier l'effet des politiques d'indemnisation en matière de frais de chirurgie accélérée et de cliniques de chirurgie privées sur la durée du temps d'invalidité chez les travailleurs qui se sont blessés.
Méthode : L'étude portait sur 1380 travailleurs qui ont subi une méniscectomie du genou entre 2001 et 2005 en Colombie-Britannique. Les données au sujet des demandes d'indemnisation couplées aux dossiers cliniques/chirurgicaux, aux temps d'attente (entre la dernière consultation et le moment de la chirurgie) et aux temps entre la chirurgie et le retour au travail ont été analysées pour comparer les établissements publiques et privés, et pour connaître l'effet des frais visant un traitement accéléré.
Résultats : Le groupe public qui a défrayé pour un traitement accéléré montre le temps d'invalidité le plus court entre la consultation pour la chirurgie et le retour au travail; les frais de traitement accéléré ont réduit le temps d'attente pour la chirurgie (~2 semaines ouvrables), et les chirurgies pratiquées dans les hôpitaux publics donnaient lieu à des temps de retour au travail plus courts (~1 semaine ouvrable).
Discussion : Une différence générale d'environ trois semaines ouvrables dans le temps d'invalidité peut avoir des répercussions importantes en termes clinique et de qualité de vie pour les travailleurs blessés. Cependant, de minces différences dans le temps d'attente pour le traitement accéléré dans les cliniques privées comparé aux hôpitaux publics, et de petites différences dans les résultats en matière de retour au travail en faveur du groupe ayant subi la chirurgie dans les hôpitaux publics, laissent croire qu'il est justifié de procéder à une évaluation économique des politiques d'indemnité en fonction du type d'établissement chirurgical.
Some workers' compensation systems in Canada pay additional surgical fee supplements to expedite care (expedited fees) and pay (higher) fees for surgeries performed in private clinics, in the belief that these measures will reduce surgery wait times, decrease total disability time, improve return-to-work outcomes and reduce disability costs. In 2004, for example, WorkSafeBC (the workers' compensation system in British Columbia) paid almost 375% more ($3,222) for an expedited knee surgery performed in a private clinic than for a non-expedited knee procedure in a public hospital ($859) (both fees represent the aggregation of facility, surgical and anaesthetists' fees). In British Columbia (BC), “expedited” is defined as surgeries performed within 21 days of surgery approval.
Work-related musculoskeletal injuries are the most common injury seen by provincial compensation systems in Canada. In British Columbia from 2004 to 2008, musculoskeletal injuries (e.g., knee strains, back strains) accounted for more than 55% of all lost-time claims, work disability days and disability costs (WorkSafeBC 2009). Among the approximate 10% of all lost-time claims for work injuries that proceed to surgical intervention, knee procedures are the most common.
WorkSafeBC began paying for surgeries for work-related musculoskeletal injuries in private clinics in 1996 and started paying for expedited surgical care in 2001 in order to improve disability-related outcomes such as shortening return-to-work times. Canadian researchers recently examined evidence on wait times for musculoskeletal procedures (knee and hip) and concluded that individuals waiting more than 12 months may have worse surgical outcomes (Sanmartin et al. 2005). Evidence for work-related outcomes for orthopaedic surgeries comes from a Norwegian study, showing increased odds of not returning to work the longer injured workers wait for surgery (OR=4.9 for injured workers who waited six to nine months for surgery compared to those who underwent surgery within one month of placement on the surgery wait list) (Rossvoll et al. 1993).
Studies comparing health outcomes for private versus public healthcare settings indicate that setting matters, with higher mortality rates observed in for-profit hospitals (Devereaux et al. 2002) and higher hospitalization rates for complications observed in private long-term care facilities (McGregor et al. 2005). The authors of these studies hypothesize that for-profit facilities tend to lower staff complements compared to non-profit facilities, leading to poorer health outcomes for patients. Prior studies comparing surgical outcomes between private versus public settings are limited. One study of day surgeries reported shorter wait times for cataract procedures performed in private clinics compared to a public hospital, but no difference between the two patient groups in visual acuity or incidence of complications post-operatively (Wegener et al. 1998). One other study of musculoskeletal surgeries in the United Kingdom reported worse disability outcomes in the public patient group compared to the private patient group following hip replacement, but the public patients had worse pain and disability measures pre-operatively (Williams et al. 2002).
Despite the expectation of policy makers at WorkSafeBC that expedited fees and private clinics would improve wait times and disability-related outcomes, results have not been evaluated. The purpose of this study was to investigate the effect of expedited surgical fees (yes versus no) and surgical setting (private clinic versus public hospital) on the wait time and return-to-work time following surgery among a sample of workers with work-related knee injuries in British Columbia. This paper focuses on disability duration outcomes. An economic analysis of expedited fees and private clinics necessitates a different study design, and as such is the focus of future work.
Methods
Study sample
This study focused on a sample of injured workers with an accepted workers' compensation time-loss claim for a knee injury and who underwent surgery for knee meniscectomy or meniscal repair between January 2001 and December 2005. The cohort was identified using WorkSafeBC claims and surgery/clinical records. Included individuals were surgery- and claim-free for at least one year prior to the start of follow-up. The study sample was restricted to those whose surgeries were day procedures (less than 24-hour total stay), because this was the only type of surgical procedure performed in private clinics for comparison with public hospitals. Individuals whose surgery included anterior cruciate ligament (ACL) repair, as a complicating co-morbidity, were also excluded. The final study sample included all public non-expedited surgeries performed during the study period, and a random 40% sample of expedited surgeries, stratified by private and public setting. Expedited surgeries were sampled, because of the labour-intensive manual data abstraction procedures. Three study groups were created, defined according to whether the WorkSafeBC injured worker received private expedited, public expedited or public non-expedited care. There were no cases of private non-expedited care because private clinics (generally) perform only expedited surgeries.
Study variables
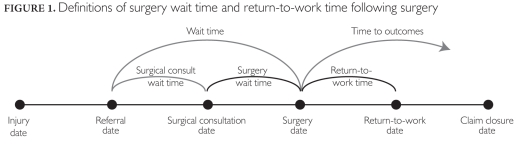
The two disability duration outcomes were wait time for surgery and return-to-work time post-surgery (Figure 1). Wait time for surgery was defined as calendar days from last pre-surgical consult to surgery date. Return-to-work time was defined as days between surgery date and first return-to-work date. Individuals who had yet to return to work (i.e., ongoing disability past a year (n=193 or 14.0%) were assigned 365 days, because return to work within one year was a clinically relevant outcome of interest. Two full-time data extraction technicians reviewed the clinical records (scanned electronic documents equivalent to a patient chart) to abstract dates and to construct the outcome and explanatory variables. Key return-to-work variables were dual-abstracted by the technicians, with disagreements resolved by consensus and reviewed by study investigators. Study investigators also reviewed a random 10% sample of the study database and found an average 98.2% agreement across all study variables.
FIGURE 1.
Definitions of surgery wait time and return-to-work time following surgery
While wait time definitions vary considerably across studies (Sanmartin 2000; Sanmartin et al. 2000), the period from last surgical consult to surgery was the critical time for this study, as the workers' compensation policy around expedited fees is designed to target and reduce this specific wait time. Furthermore, in the absence of definitive information on when a patient decides to undergo surgery or is placed on a waiting list, many other researchers in the field of musculoskeletal surgeries have used the last pre-surgical visit as an indicator of the decision to proceed with surgery (Coyte et al. 1994), with evidence of good agreement for musculoskeletal surgeries such as knee and hip replacement (Sanmartin 2000) and for elective orthopaedic procedures (Shortt et al. 2004). For both these reasons, we adopted the definition using last surgical consult to surgery data as surgery wait time.
The two primary explanatory variables were surgical setting and expedited status. Information on surgical setting (private clinic versus public hospital, based on a care facility code) and whether or not an expedited fee was paid (benefits payment code) were derived from the WorkSafeBC medical benefits payment records. Covariate data on the health authority of surgical setting (five provincial regions) and co-morbidities (osteoarthritis, other joint pathologies, prior claims/work-related surgeries) were abstracted from the WorkSafeBC clinical records. The WorkSafeBC injury claim records also provided data on age at time of surgery (four categories), gender, injury characteristics and wage and occupation of employment at time of injury.
Analysis
Baseline characteristics of the three study groups of interest were compared. Median days (with inter-quartile ranges) were calculated for both outcome measures for the three study groups, and were adjusted for the effects of age, gender, wage, health authority, co-morbidities and occupation (see Table A-1 in the Appendix).
Table A-1.
Distribution of demographic, socio-economic, occupational, geographic and clinical/co-morbid characteristics for workers with meniscal knee surgery (n=1,380), by surgical setting and expedited study groups
| Private Clinic, Expedited Group (n=574) | Public Hospital, Expedited Group (n=568) | Public Hospital, Non-Expedited Group (n=238) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % or mean | (95% CI) | n | % or mean | (95% CI) | n | % or mean | (95% CI) | ||
| Age | Mean 15−30 years 30−40 years 40−50 years 50−65 years |
42 112 201 219 |
46.1 7.3% 19.4% 35.0% 38.2% |
(45.3−46.9) (5.2−9.5) (16.3−22.8) (31.1−38.9) (34.2−42.1) |
43 120 206 199 |
45.5 7.6% 21.1% 36.3% 35.0% |
(44.7−46.3) (5.4−9.8) (17.8−24.5) (32.3−40.2) (31.1−39.0) |
18 54 85 81 |
44.7 7.6% 22.7% 35.7% 34.0% |
(43.5−46.0) (4.2−10.9) (17.3−28.0) (29.6−41.8) (28.0−40.1) |
| Wage1 | Mean ($1,000s) <$30,000 $30−$40,000 $40−$50,000 $50−$60,000 >$60,000 |
135 109 117 90 123 |
45.4 23.5% 19.0% 20.4% 15.7% 21.4% |
(43.7−47.1) (20.0−27.0) (15.8−22.2) (17.1−23.7) (12.7−18.7) (18.1−24.8) |
117 111 112 101 127 |
46.5 20.6% 19.5% 19.7% 17.8% 22.4% |
(44.7−48.3) (17.3−23.9) (16.3−22.8) (16.4−23.0) (14.6−20.9) (18.9−25.8) |
60 51 44 38 45 |
43.1 25.2% 21.4% 18.5% 16.0% 18.9% |
(40.5−45.7) (19.7−30.8) (16.2−26.7) (13.5−23.5) (11.3−20.7) (13.9−23.9) |
| Gender | Women | 97 | 16.9% | (13.8−20.0) | 79 | 13.9% | (11.1−16.8) | 50 | 21.0% | (15.8−26.2) |
| Health Authority (Location) |
Vancouver Vancouver Island Interior Fraser Valley Northern |
270 145 49 87 23 |
47.0% 25.3% 8.5% 15.2% 4.0% |
(42.9−51.1) (21.7−28.8) (6.2−10.8) (12.2−18.1) (2.4−5.6) |
84 130 140 172 42 |
14.8% 22.9% 24.6% 30.3% 7.4% |
(11.9−17.7) (19.4−26.4) (21.1−28.2) (26.5−34.1) (5.2−9.6) |
35 65 37 78 23 |
14.7% 27.3% 15.5% 32.8% 9.7% |
(10.2−19.2) (21.6−33.0) (10.9−20.2) (26.8−38.8) (5.9−13.4) |
| Occupation (Top 4)2 |
Service Construction Other trades Transportation |
67 87 90 104 |
11.7% 15.2% 15.7% 18.1% |
(9.0−14.3) (12.2−18.1) (12.7−18.7) (15.0−21.3) |
67 111 77 89 |
11.8% 19.5% 13.6% 15.7% |
(9.1−14.5) (16.3−22.8) (10.7−16.4) (12.7−18.7) |
28 40 35 40 |
11.8% 16.8% 14.7% 16.8% |
(7.6−15.9) (12.0−21.6) (10.2−19.2) (12.0−21.6) |
| Clinical/Co-morbid Conditons | Previous knee claim Previous knee surgery Osteoarthritis3 Other joint pathologies4 ACL diagnoses |
166 116 353 154 54 |
28.9% 20.2% 61.5% 26.8% 9.4% |
(25.2−32.6) (16.9−23.5) (57.5−65.5) (23.2−30.5) (7.0−11.8) |
147 108 311 172 67 |
25.9% 19.0% 54.8% 30.3% 11.8% |
(22.3−29.5) (15.8−22.3) (50.6−58.9) (26.5−34.1) (9.1−14.5) |
68 59 130 59 27 |
28.6% 24.8% 54.6% 30.3% 11.3% |
(22.8−34.4) (19.3−30.3) (48.3−61.0) (24.4−36.1) (7.3−15.4) |
| Returned to work within 365 days | 507 | 88.3% | (85.7−91.0) | 478 | 84.2% | (81.1−87.2) | 202 | 84.9% | (80.3−89.5) | |
1 Annualized wage used for lost-time compensation.
2 Standard Occupation Classification (SOC) at time of injury.
3 Includes diagnoses of articular cartilage changes and chondromalacia.
4 Includes diagnoses of osteophytes, plicas and knee-locking.
Differences in median days for both outcomes associated with expedited status and surgery setting were also investigated for individuals in the 25th, 50th and 75th percentiles of the distributions using quantile regression models (see Table A-2 in the Appendix). Quantile regression (Koenker and Hallock 2001) is appropriate for examining skewed distributions and censored outcomes because it permits a robust analysis of the entire observed distribution of outcomes and allows for the investigation of different effects for those who may have longest wait times and return-to-work times as unique subgroups within the study population (Hogg-Johnson and Cole 2003). The estimates of the effect of the key explanatory variables on the two outcomes in the regression models were adjusted for covariates and clustering at the level of surgeon using bootstrap re-sampling methods (see Table A-3 in the Appendix). Censoring individuals who had yet to return to work after one year did not affect the analysis because 365 days was past the 75th percentile — the longest duration we analytically investigated.
Table A-2.
Adjusted quantile regression results for differences in median days (and inter-quartile range) for surgical wait time among injured workers undergoing knee meniscectomy or meniscal repair surgery by surgical setting and expedited status. The regression coefficients represent the difference in days relative to the median number of days for the public, non-expedited group, by individuals in the 25th, 50th and 75th percentiles, respectively.
| 25th Percentile | 50th Percentile | 75th Percentile | ||
|---|---|---|---|---|
| Coefficient [95% CI]1 | Coefficient [95% CI]1 | Coefficient [95% CI]1 | ||
| Surgical Setting and Expedited Status | Public hospital; non-expedited Private clinic; expedited |
REF −5.67 [−12.18, 0.85] −5.67 [−12.11, 0.78] |
REF −12.50 [−18.77, −6.23]*** −14.00 [−20.00, −8.00]** |
REF −34.00 [−50.93, −7.07]*** −33.00 [−49.38, −16.62]*** |
| Public hospital; expedited | ||||
| Gender | Women vs. Men | −0.33 [−3.99, 3.32] | 2.75 [−1.26, 6.76] | −1.00 [−6.71, 4.71] |
| Age | <30 years 30−40 years 40−50 years 50−65 years |
REF −3.67 [−10.02, 2.68] 1.00 [−5.70, 7.70] 0.67 [−5.71, 7.05] |
REF −2.00 [−8.95, 4.95] −0.75 [−7.60, 6.10] −0.75 [−8.01, 6.51] |
REF 1.00 [−11.07, 13.07] −2.00 [−12.58, 8.58] 0.00 [−11.19, 11.19] |
| Wage | <$30,000 $30−$40,000 $40−$50,000 $50−$60,000 >$60,000 |
REF 1.00 [−3.16, 5.16] 1.33 [−3.97, 6.64] 0.00 [−4.21, 4.21] 0.33 [−4.29, 4.95] |
REF 2.25 [−1.87, 6.37] 0.00 [−4.49, 4.49] −0.75 [−5.38, 3.88] 0.25 [−3.82, 4.32] |
REF −1.00 [−8.44, 6.44] −2.00 [−9.82, 5.82] −5.00 [−12.45, 2.45] −4.00 [−11.46, 3.46] |
| Health Authority | Vancouver Coastal Vancouver Island Interior Fraser Northern |
REF 0.00 [−5.27, 5.27] −5.00 [−9.82, −0.18]* 3.33 [−1.42, 8.08] −5.67 [−12.93, 1.60] |
REF −3.50 [−9.30, 2.30] −4.75 [−10.11, 0.61] 4.50 [−1.18, 10.18] −4.75 [−14.07, 4.57] |
REF −10.00 [−19.19, −0.81]* −11.00 [−20.76, −1.24]* −1.00 [−10.58, 8.58] −11.00 [−22.26, 0.26] |
| Constant | 18.33 [9.84, 26.83]*** | 37.50 [28.91, 46.09]*** | 80.00 [62.03, 97.97]*** | |
* p<0.05, ** p<0.01, *** p<0.001
1 95% confidence intervals in brackets. Standard errors were obtained via bootstrap estimation based on re-sampling at the level of the surgeon (using scrambled surgeon identifier obtained from WorkSafeBC surgical/clinical data).
Table A-3.
Adjusted quantile regression results for differences in median days (and inter-quartile range) for return-to-work time among injured workers undergoing knee meniscectomy or meniscal repair surgery by surgical setting and expedited status. The regression coefficients represent the difference in days relative to the median number of days for the public, non-expedited group, by individuals in the 25th, 50th and 75th percentiles, respectively.
| 25th Percentile | 50th Percentile | 75th Percentile | ||
|---|---|---|---|---|
| Coefficient [95% CI]1 | Coefficient [95% CI]1 | Coefficient [95% CI]1 | ||
| Surgical setting and expedited status | Public hospital, non expedited Private clinic; expedited Public hospital; expedited |
REF 5.37 [−1.22, 11.95] 6.88 [0.15, 13.62]* |
REF 6.00 [−5.68, 17.68] 3.67 [−6.63, 13.97] |
REF −2.14 [−36.60, 32.32] 6.72 [−37.69, 51.14] |
| Gender | Women vs. men | 11.04 [2.13, 19.95]* | 19.00 [5.95, 32.05]** | 30.64 [−9.27, 70.55] |
| Age | <30 years 30−40 years 40−50 years 50−65 years |
REF −2.25 [−12.90, 8.40] −2.08 [−13.12, 8.97] 0.40 [−11.15, 11.96] |
REF −4.00 [−27.11, 19.11] −5.33 [−27.28, 16.61] 2.33 [−21.45, 26.12] |
REF −57.32 [−162.95, 48.31] −51.59 [−156.30, 53.13] −19.89 [−130.91, 91.12] |
| Wage | <$30,000 $30−$40,000 $40−$50,000 $50−$60,000 >$60,000 |
REF −2.90 [−11.08, 5.27] −6.98 [−14.80, 0.84] −8.88 [−16.60, −1.17]* −15.87 [−23.66, −8.07]*** |
REF −14.00 [−28.57, 0.57] −18.67 [−34.28, −3.05]* −28.33 [−43.40, −13.27]*** −30.33 [−45.20, −15.47]*** |
REF −150.74 [−248.07, −53.42]** −169.62 [−266.26, −72.97]*** −181.60 [−278.47, −84.72]*** −190.18 [−282.67, −97.69]*** |
| Health Authority | Vancouver Coastal Vancouver Island Interior Fraser Northern |
REF −9.69 [−17.53, −1.86]* −14.12 [−22.77, −5.46]** −7.15 [−15.30, 0.99] −13.46 [−26.26, −0.67]* |
REF −22.00 [−34.56, −9.44]*** −17.33 [−33.40, −1.26]* −13.00 [−26.73, 0.73] −14.67 [−46.10, 16.76] |
REF −28.44 [−69.85, 12.98] −35.11 [−82.08, 11.87] −23.82 [−66.47, 18.83] −26.01 [−111.82, 59.80] |
| Clinical | Previous same-knee surgery (yes vs. no) Osteoarthritis (yes vs. no) |
5.42 [−0.35, 11.19 3.98 [−0.24, 8.20] |
15.33 [3.93, 26.74]** 8.67 [1.35, 15.99]* |
55.80 [−2.33, 113.93] 5.45 [−17.26, 28.15] |
| Occupation | Managemt./admin./clerical Health Sales Service Construction trades Other trades Transportation Primary Processing, manufacturing |
REF 20.33 [8.45, 32.20]*** −1.37 [−11.13, 8.40] 15.04 [5.75, 24.33]** 15.46 [7.50, 23.42]*** 13.19 [4.75, 21.63]** 19.65 [11.75, 27.56]*** 25.42 [14.76, 36.09]*** 14.71 [3.58, 25.85]** |
REF 20.33 [2.07, 38.60]* −2.33 [−15.58, 10.92] 22.67 [5.92, 39.42]** 29.00 [14.61, 43.39]*** 21.67 [9.60, 33.73]*** 28.00 [15.61, 40.39]*** 63.00 [32.93, 93.07]*** 29.00 [13.68, 44.32]*** |
REF 30.28 [−4.23, 64.78] −19.36 [−55.98, 17.26] 34.49 [−11.55, 80.53] 77.72 [−3.37, 158.82] 38.53 [8.19, 68.87]* 49.13 [14.66, 83.60]** 165.27 [67.43, 263.11]*** 75.12 [8.98, 141.25]* |
| Constant | 25.29 [9.97, 40.60]** | 53.33 [22.62, 84.05]*** | 277.34 [154.66, 400.02]*** | |
* p<0.05, ** p<0.01, *** p<0.001
1 95% confidence intervals in brackets. Standard errors were obtained via bootstrap estimation based on re-sampling at the level of the surgeon (using scrambled surgeon identifier obtained from WorkSafeBC surgical/clinical data).
Data analysis was completed using SAS 9.1 (SAS Institute, Cary, NC) and Stata 10.0 (StataCorp, College Station, TX). Ethical approval for the research project was obtained from the Behavioural Research Ethics Board at the University of British Columbia (Certificate # H06-80221). The study procedures were also completed under a data access agreement between the University of British Columbia and WorkSafeBC governing the privacy and confidentiality conditions for use of the data for research purposes (Population Data BC 2009).
Results
Study sample
A total of 4,089 unique knee meniscectomies or knee meniscal repairs were identified in the BC workers' compensation data between 2001 and 2005. Of these, 3,395 (83%) were eligible for inclusion in the study, with no complicating ACL repair procedure and no claim/surgery in the year prior to entry into the study. All eligible 263 public hospital non-expedited procedures were data extracted, as were 1,347 expedited procedures (a 40% stratified random sample by surgical setting and year). A total of 230 (7%) surgeries were subsequently excluded either as ineligible (n=136) based on information obtained from the data abstraction (e.g., surgery performed out of province, lost to follow-up) or because of missing data (n=94) (e.g., no operative report). The final analytic sample included 1,380 unique workers' compensation claims for knee meniscectomy or knee meniscal repair, of which 238 were public hospital non-expedited procedures, 568 public hospital expedited procedures and 574 private clinic expedited procedures (Table 1).
TABLE 1.
Final study sample of included injured workers with knee surgery between 1999 and 2001, by surgical setting and expedited status (n=1,380)
| Surgical Setting | ||
|---|---|---|
| Public hospital | Private clinic | |
| Expedited surgery | 568 (41.2%) | 574 (41.6%) |
| Non-expedited surgery | 238 (17.2%) | NA1 |
1 There were no cases of private non-expedited care because private clinics (generally) perform only expedited surgeries.
Descriptive baseline characteristics
The three study groups defined by expedited status and surgical setting did not differ statistically on baseline characteristics of age at time of surgery, wage at time of injury, percentage of women or occupation (95% confidence intervals for all estimates overlapped across the three study groups). The mean age at time of surgery ranged from 44.7 years in the public non-expedited group to 46.1 years in the private expedited group. The mean wage at time of injury ranged from $43,100 per annum in the public non-expedited group to $46,500 per annum in the public expedited group. Women represented 21.0% of the public non-expedited surgical group, compared to 16.9% of the private expedited group and 13.9% of the public expedited group. In all three study groups, the most common occupations were transportation, construction trades and other trades.
The study groups did not differ statistically on clinical or co-morbidity characteristics at baseline. The majority of the knee meniscal surgeries involved a medial meniscus diagnosis, ranging from 71.0% in the public non-expedited group to 74.8% in the private expedited group. Surgeries involving both a medial and a lateral meniscus diagnosis ranged from 11.3% in the public, non-expedited group to 15.7% in the private expedited group. For co-morbidities, history of a previous same-knee claim (but not in the year prior to the study surgery) ranged from 25.9% in the public expedited group to 28.6% and 28.9% in the public non-expedited and private expedited groups, respectively. The most common co-morbidity was osteoarthritis, ranging from 54.6% in the public non-expedited group to 61.5% in the private expedited group. The number and percentage of private, expedited surgeries is related to the number of private clinics available in the provincial health regions, ranging from 69% and 43% of included surgeries in the larger urban health regions to 26% in the northern (rural and remote) region of the province.
Wait time for surgery and return-to-work time following surgery
The median surgery wait time was 22 and 24 calendar days for expedited surgeries (public hospital and private clinic, respectively), compared to 37 calendar days for non-expedited surgeries (public hospital only), or a difference of approximately two work weeks longer (Table 2). The majority of the study sample returned to work within one year post-surgery — 84.2% and 84.9%, respectively, among the public expedited and non-expedited groups, and 88.3% among the private expedited group. The median time to return to work following surgery was 58 and 60 calendar days for public hospital surgeries (non-expedited and expedited, respectively), compared to 66 days for private clinic surgeries (expedited only), or approximately one work week longer (Table 2). The total disability duration in this study defined as last surgical consult to first return to work was 91 and 101 days for expedited surgeries (public hospital and private clinic, respectively) compared to 117 days for non-expedited surgeries (public hospital only), an overall difference attributable largely to the expedited surgical wait time.
TABLE 2.
Median wait time for surgery and return-to-work time post-surgery by expedited status and surgical setting, adjusted for socio-demographic, clinical and work characteristics1
| Wait Time for Surgery (median days, IQR)3 | ||
|---|---|---|
| Public hospital | Private clinic | |
| Expedited surgery | 22 (12, 38) | 24 (13, 39) |
| Non-expedited surgery | 37 (18, 71) | NA2 |
| Return-to-Work Time Post-Surgery (median days, IQR) | ||
| Public hospital | Private clinic | |
| Expedited surgery | 60 (35, 162) | 66 (37, 161) |
| Non-expedited surgery | 58 (29, 164) | NA2 |
| Combined Disability Time (median days, IQR)3 | ||
| Public hospital | Private clinic | |
| Expedited surgery | 91 (58, 186) | 101 (62, 194) |
| Non-expedited surgery | 117 (65, 220) | NA2 |
1 Adjusted for age, gender, wage, occupation, health authority and co-morbidities (previous surgery/claim and osteoarthritis).
2 There were no cases of private non-expedited care because private clinics (generally) perform only expedited surgeries.
3 Note that median times are not additive.
Results for multivariable quantile regression
The effect of the expedited fee on the wait time to surgery varied for different groups. Looking first at the 50th percentile of the distribution of surgery wait time, we found the difference was 12.5 and 14.0 fewer days for expedited knee surgeries (private and public, respectively) compared to the median wait for non-expedited surgeries (Table 3). The 75th percentile of the distribution had a difference of 33 and 34 fewer days for expedited care for both surgical settings. Differences were not significant at the 95% confidence interval level for the 25th percentile of the distribution (i.e., ~6 days less for both expedited groups compared to the non-expedited group).
TABLE 3.
Adjusted quantile regression results for differences in median days for surgical wait time and return-to-work time among injured workers undergoing knee meniscectomy or meniscal repair surgery, by surgical setting and expedited status. The regression coefficients represent the difference in days relative to the median number of days for the public, non-expedited group, by individuals in the 25th, 50th and 75th percentiles of the distribution, respectively.
|
25% Percentile Coefficient (95% CI) |
50% Percentile Coefficient (95% CI) |
75% Percentile Coefficient (95% CI) |
|
|---|---|---|---|
| Surgical Wait Time Model1 | |||
| Public hospital, non-expedited Public hospital, expedited Private clinic, expedited |
REF −5.7 (−12.1, 0.8) −5.7 (−12.2, 0.9) |
REF −14.0 (−20.0, 8.0) −12.5 (−18.8, −6.2) |
REF −33.0 (−49.4, 16.6) -34.0 (−50.9, 17.1) |
| Return-to-Work Time Model2 | |||
| Public hospital, non-expedited Public hospital, expedited Private clinic, expedited |
REF 5.4 (−1.2, 11.9) 6.9 (0.2, 13.6) |
REF 6.0 (−5.7, 17.7) 3.7 (−6.6, 14.0) |
REF −2.1 (−36.6, 32.2) 6.7 (−37.7, 51.1) |
1 Model adjusted for age, gender, wage and health authority (geographic location).
2 Model adjusted for age, gender, wage, occupation, health authority (geographic location) and clinical/co-morbid characteristics.
The difference in time to return to work post-surgery was approximately one week longer (four to six days) for both the public and private expedited groups compared to the median time for the public non-expedited group (Table 3) across the distribution, with the exception of the public expedited group at the 75% percentile (two days less). None of the differences for return to work were statistically significant across the percentile groups. The overall net effect was that the public expedited group had the shortest disability duration from surgical consult to return to work, whereby the expedited fee significantly reduced the surgery wait time (regardless of surgical setting), and surgeries performed in public hospitals had the shortest return-to-work time.
Discussion
Workers' compensation systems in Canada have been social insurance providers, including the payer of health services, for injured workers since the early 1900s. Indeed, this system evolved separately and well before the introduction of the universal coverage of hospital and physician care in Canada (Bogyo 2008). These systems have evolved over the past decade to develop policies and practices such as expedited fees and/or the use of private clinics for delivery of health services to injured workers (Hurley et al. 2008; Bogyo 2008). The intent of these recent policies and programs is to return workers to work as soon as possible without unnecessary delays. This approach benefits both the workers' compensation system, by reducing disability duration (including claim costs borne by the compensation system and ultimately the employer), and the workers, who have a decreasing probability of returning to work the longer they are off work (Hogg-Johnson and Cole 2003).
The introduction of these recent policies and procedures has sparked a larger debate about perceived unequal access to healthcare for Canadians (see Hurley et al. 2008 and Bogyo 2008). Some commentators (Hurley et al. 2008) argue that expedited fees and the use of private clinics as a means of accelerating access to care undermine the core principles of the Canada Health Act by condoning cause-of-injury, illness- or insurance plan—related queue jumping, or by reallocating limited human resources (e.g., orthopaedic surgeons) from serving patients paid through the public system to patients paid through a parallel insurance fund. Others argue (Bogyo 2008), conversely, that workers' compensation benefits provide healthcare coverage to individuals who might not otherwise be covered by provincial health insurance (e.g., foreign workers), that decisions are based on medical need rather than preferred access, and that the additional source of funding can reduce the burden on the overall system by purchasing after-hour services such as surgery time. The results of our analysis inform this debate by providing evidence on the effects of certain policies enacted by this parallel funding system, on wait times for surgery, elapsed time until return to work and disability time for injured workers.
Our analysis focused on an internal comparison of injured workers by differences in expedited status and surgical setting under the workers' compensation insurance system, to investigate the effect of private delivery of care and fee incentives in the context of a publicly administered workers' compensation system. This study did not provide an opportunity to compare access and disability outcomes for individuals undergoing the same surgery through the two different insurance plans (i.e., workers' compensation and provincial health). However, the evaluation of these policies and procedures is warranted internally within the workers' compensation environment, and may also provide evidence to inform policies and procedures for the broader healthcare system.
As a policy under the workers' compensation insurance system, expedited fees were effective in reducing wait time to surgery. While a difference of only two weeks may not improve longer-term clinical outcomes post-surgery, it represents a reduction in the total disability duration (i.e., pain, suffering, quality of life) for the injured worker and increases the worker's likelihood of successfully returning to work; the reduced disability duration also represents a cost saving to the workers' compensation system for time-loss benefits and to employers who pay compensation premiums based on the frequency and duration of their claims experience. Since our study period, the majority of workers' compensation surgeries have become expedited, suggesting that unequal access is not a major issue within the workers' compensation population today. These results suggest that the expedited fee does no harm within the narrow context of the workers' compensation environment, though the cost—benefit question remains.
What is less clear is whether the expedited fee incentive creates inequity within our overall healthcare system. Planned surgeries covered by workers' compensation insurance in British Columbia, regardless of expedited status, are provided in public hospitals during blocks of surgical time purchased outside regular operating hours and should not, by definition, affect access to surgeries by the general public; it may, in fact, help to reduce wait times overall in the system by using compensation dollars to increase operating times. However, the provision of surgeries “after hours” or within private clinics may result in a redistribution of finite resources (e.g., surgeons, surgeon time, surgical staff) from one insurance provider to another, favouring those associated with higher fees, thus creating inequities. An evaluation of the effect of workers' compensation policies on inequity in the provincial healthcare system was not part of this study and warrants future investigation.
Despite surgery wait time differences, injured workers in the public hospital group tended to do slightly better in terms of time to return to work after surgery compared to workers in the private clinic group. This finding is consistent with previous evidence that suggested better outcomes from public than private clinical settings (Devereaux et al. 2002; McGregor et al. 2005; Wegener et al. 1998). In this case, the improved outcomes were a shorter disability duration and earlier return to work for injured workers. Some might argue that the approximate one-week difference was not statistically significant and, as such, the provision of surgeries with private clinics “does no harm” within the context of the workers' compensation environment. Yet, as with expedited fees, it remains unclear whether the reliance on for-profit clinics increases capacity for surgeries with costs borne appropriately by employers and industries for work-related injuries, or whether they redistribute finite resources away from the provision of surgeries within the public healthcare system. Further, minimal differences in disability duration for patients treated by private clinics relative to those treated in public hospitals, given the added cost associated with surgeries performed in for-profit clinics, suggest that a future economic evaluation of this workers' compensation policy is warranted.
In addition to the broader policy implications of the expedited fee and private clinic surgical settings, this study turned up a number of other interesting findings, despite some limitations. First, the median surgery wait times for expedited surgeries, at 22 and 24 days for public and private surgical settings, respectively, exceeded the 21-day definitional criterion. The criterion used to determine whether the expedited fee is paid is, by definition, from surgical approval date to surgery. However, the former date was not consistently recorded in the clinical data files at WorkSafeBC. We relied on last surgical consult date, a date that was consistently recorded in those files, as a proxy for surgery approval date, and this approach may explain some of the observed discrepancy. Yet, it cannot explain either the 50% of the distribution that had surgery wait times greater than 21 days despite an expedited fee having been paid, or, most notably, the upper inter-quartile value of 38 days. The findings on expedited fees for the observed surgical wait times beyond the 21-day criterion reported here have already prompted administrative changes by WorkSafeBC.
In the current study, it was thought that surgical cases complicated by pre-existing co-morbidities would be directed to a public hospital in the event that a longer stay seemed likely (i.e., surgeries performed in a private clinic would require that the individual be transferred to a public hospital if the stay was longer than a day). Indeed, the public non-expedited group had greater variability in their wait times, suggesting that the time leading up to surgery may be confounded by co-morbidities and that individuals with complications may be directed to the public system. Regardless, all wait times in the current study were within 12-month (Sanmartin et al. 2005) and six- to nine-month (Rossvoll et al. 1993) periods identified by others for improved outcomes, including return to work; and a median difference of two weeks between groups classified by expedited status was not likely to lead to major differences in return-to-work outcomes, as was seen in our final results.
Sample selection related to compensation and clinical characteristics is critical when evaluating program or treatment effects using non-experimental observational designs. The decision of where (private versus public) and when (within 21 days of surgical approval or not) work-related surgeries are performed is based on input from the injured worker's case manager and surgeon, injured worker preference (i.e., opting for a surgeon, date or location of choice) and availability of surgeon/surgical facilities. The possibility of differential sample selection into study groups was investigated. Average age, proportion female, pre-claim wage, type of occupation, presence of co-morbidity/co-pathology and having a previous knee claim were distributed similarly across the public non-expedited, public expedited and private expedited study groups, indicating that across multiple demographic, socio-economic and clinical characteristics there did not appear to be systematic differential sample selection. Finally, the incentive for surgeons is the same regardless of where they perform an expedited surgery — the fee is paid to them directly for both private and public settings in addition to their regular payment structures.
Conclusion
A difference of approximately two weeks in surgery wait time associated with the expedited fee policy may have meaningful clinical and quality-of-life implications for injured workers, in addition to being cost-effective policy for workers' compensation insurance systems, but did not affect the return-to-work time post-surgery as part of total disability duration. Minimal (and not statistically significant) differences in disability duration were observed for surgeries performed in private clinics versus public hospitals. The expedited and private clinic policies do not appear to introduce harmful consequences to injured workers within the workers' compensation insurance system, although an economic analysis of the policies may be informative to the workers' compensation system and may provide evidence to inform the broader societal consequences of these policies. Evaluating the effect of workers' compensation policies and practices on issues of access and resources for all Canadians within provincial healthcare systems, while a more challenging endeavour, also warrants future investigation.
Contributor Information
Mieke Koehoorn, Associate Professor, School of Population and Public Health, University of British Columbia, Vancouver, BC.
Christopher B. McLeod, Post-Doctoral Fellow, College for Interdisciplinary Studies, University of British Columbia, Vancouver, BC.
Jonathan Fan, Research Coordinator, College for Interdisciplinary Studies, University of British Columbia, Vancouver, BC.
Kimberlyn M. McGrail, Assistant Professor, Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, BC.
Morris L. Barer, Professor and Director, Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, BC.
Pierre Côté, Scientist and Associate Professor, Toronto Western Research Institute, Toronto Western Hospital, Dalla Lana School of Public Health, University of Toronto, Toronto, ON.
Sheilah Hogg-Johnson, Senior Scientist and Assistant Professor, Institute for Work & Health, Toronto, ON.
References
- Bogyo T.J. 2008. The Case for Excluding Workers' Compensation Insurance from Medicare. Healthcare Papers 8(3): 21–29 [DOI] [PubMed] [Google Scholar]
- Coyte P.C., Wright J.G., Hawker G.A., Bombardier C., Dittus R.S., Paul J.E., Freund D.A., Ho E. 1994. Waiting Times for Knee-Replacement Surgery in the United States and Ontario. New England Journal of Medicine 331(16): 1068–71 [DOI] [PubMed] [Google Scholar]
- Devereaux P.J., Choi P.T., Lacchetti C., Weaver B., Schunemann H.J., Haines T., Lavis J.N., Grant B.J., Haslam D.R., Bhandari M., Sullivan T., Cook D.J., Walter S.D., Meade M., Khan H., Bhatnagar N., Guyatt G.H. 2002. A Systematic Review and Meta-Analysis of Studies Comparing Mortality Rates of Private For-Profit and Private Not-for-Profit Hospitals. Review. Canadian Medical Association Journal 166(11): 1399–406 [PMC free article] [PubMed] [Google Scholar]
- Hogg-Johnson S., Cole D.C. 2003. Early Prognostic Factors for Duration on Temporary Total Benefits in the First Year among Workers with Compensated Occupational Soft Tissue Injuries. Occupational and Environmental Medicine 60(4): 244–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley J., Pasic D., Lavis J.N., Culyer A.J., Mustard C.A., Gnam W. 2008. Parallel Payers and Preferred Access: How Canada's Workers' Compensation Boards Expedite Care for Injured and Ill Workers. Healthcare Papers 8(3): 6–14 [DOI] [PubMed] [Google Scholar]
- Koenker R., Hallock K.F. 2001. Quantile Regression. Journal of Economic Perspectives 15: 143–56 [Google Scholar]
- McGregor M.J., Cohen M., McGrail K., Broemeling A.M., Adler R.N., Schulzer M., Ronald L., Cvitkovich Y., Beck M. 2005. Staffing Levels in Not-for-Profit and For-Profit Long-Term Care Facilities: Does Type of Ownership Matter? Canadian Medical Association Journal 172(5): 645–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Population Data BC, University of British Columbia 2009. Research Data Access Framework. Retrieved July 5, 2011. http://www.popdata.bc.ca/dataaccess/rdaf
- Rossvoll I., Benum P., Bredland T.R., Solstad K., Arntzen E., Jorgensen S. 1993. Incapacity for Work in Elective Orthopaedic Surgery: A Study of Occurrence and the Probability of Returning to Work After Treatment. Journal of Epidemiology and Community Health 47(5): 388–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanmartin C. 2000. A Study of Surgical Waiting Lists and Waiting Times for Selected Procedures in British Columbia. University of British Columbia, Department of Health Care and Epidemiology; PhD thesis. Koerner Library Call Number: AW5 .B7 2000-566153. [Google Scholar]
- Sanmartin C., Bohm E., Coner-Spady B., DeCoster C., Dunbar M., Lorenzetti D., McLaren L., McGurran J. 2005. Towards Establishing Evidence Based Benchmarks for Acceptable Waiting Times for Joint Replacement Surgery. Report 2. Retrieved July 5, 2011. http://www.wcwl.ca/media/pdf/library/cihr_synthesis_reports.2.pdf
- Sanmartin C., Shortt S.E., Barer M.L., Sheps S., Lewis S., McDonald P.W. 2000. Waiting for Medical Services in Canada: Lots of Heat, But Little Light. Canadian Medical Association Journal 162(9): 1305–10 [PMC free article] [PubMed] [Google Scholar]
- Shortt S.E., Shaw R.A., Elliott D., Mackillop W.J. 2004. Monitoring Trends in Waiting Periods in Canada for Elective Surgery: Validation of a Method Using Administrative Data. Canadian Journal of Surgery 47(3): 173–78 [PMC free article] [PubMed] [Google Scholar]
- Wegener M., Alsbirk P.H., Hojgaard-Olsen K. 1998. Outcome of 1000 Consecutive Clinic- and Hospital-Based Cataract Surgeries in a Danish County. Journal of Cataract and Refractive Surgery 24(8): 1152–60 [DOI] [PubMed] [Google Scholar]
- Williams O., Fitzpatrick P., Hajat S., Reeves B.C., Stimpson A., Morris R.W., Murray D.W., Rigge M., Gregg P.J. and National Total Hip Replacement Outcome Study Steering Committee 2002. Mortality, Morbidity, and 1-Year Outcomes of Primary Elective Total Hip Arthroplasty. Journal of Arthroplasty 17(2): 165–71 [DOI] [PubMed] [Google Scholar]
- WorkSafeBC — Workers' Compensation Board of British Columbia 2009. WorkSafeBC Statistics 2008. Richmond, BC, Workers' Compensation Board of British Columbia. Retrieved July 5, 2011. http://www.worksafebc.com/publications/reports/statistics_reports/assets/pdf/stats2008.pdf