Abstract
Rationale and Objectives
Emphysema is characterized by lung tissue destruction and trapped gas. On CT images this may be expressed by widespread areas with high specific gas volume (SVg). SVg is highly sensitive to very low attenuation values which frequently occur in CT images of patients with severe emphysema. The purpose of the present work is to study if and how different reconstruction settings and different scanners significantly influence SVg distribution particularly in the very low attenuation range.
Materials and Methods
Two sets of CT images taken from two different CT scanners at two different lung volumes on ten healthy volunteers and on eighteen subjects with severe emphysema were analyzed. Images were reconstructed using two different settings of reconstruction parameters: thin slice thickness/sharp filter and thick slice thickness /smooth filter. For each set of images average values of SVg, their variations (ΔSVg) from TLC to RV were calculated in the whole lung.
Results
Very low attenuation values are always present in CT images when the reconstruction setting thin slice/sharp reconstruction filter is used and in very large numbers in subjects with severe emphysema. SVg values were in general significantly higher in emphysematous subjects than in healthy subjects, both at TLC and RV (P<0.001), and were significantly influenced by the reconstruction filter (P<0.001) and CT scanner (P<0.001). ΔSVg was lower in emphysematous than in healthy (P<0.001) subjects and was significantly affected by the reconstruction setting but not by the CT scanner.
Conclusion
The disproportionate effect of low-attenuation pixels on SVg likely causes overestimation of the severity of emphysema and trapped gas. This can be significantly reduced, however, by using thick slices and a smooth filter for image reconstruction. ΔSVg is generally robust for quantifying the functional impairment of the lung in severe emphysema.
Index Terms: Biomedical image processing, computed tomography, density measurement
INTRODUCTION
Emphysema is characterized by the destruction of lung tissue in the distal airspaces. This is visualized by areas of abnormally low attenuation on CT images [1] whose pattern and distribution vary widely from one patient to another.
Coxson et al [2] proposed a simple method to convert lung density into specific gas volume (SVg), which is the volume of gas per gram of lung tissue. SVg can be suitably used to study emphysematous lungs on a regional basis and has a significant advantage in identifying trapped gas. Recently, we showed in a pig model of regional airway obstruction that SVg determined at different lung volumes provides a useful method for clearly identifying and quantifying the extent and severity of trapped gas [3]. These methods and findings have important potential clinical implications for the assessment of human subjects undergoing lung volume reduction surgery or minimally invasive interventions such as transbronchial stents or endobronchial lung volume reduction [4]–[6].
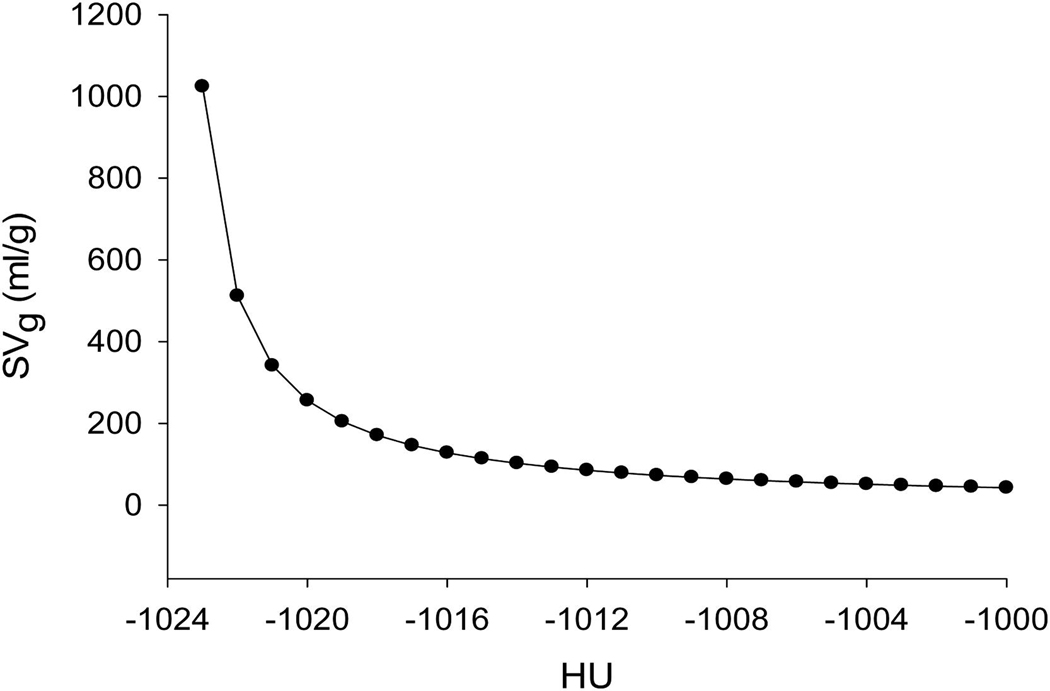
Since SVg is defined as the inverse of the lung density (minus the specific volume of lung tissue), it is highly sensitive to very low attenuation values, and these low-attenuation values are particularly relevant to those subjects with emphysema [7]. Figure 1 shows the relationship existing between density and specific gas volume when Hounsfield Unit (HU) values are extremely low (from −1024 HU to −1000 HU). The strong non-linear behavior of this relationship suggests that these very low attenuation values provide a disproportionate weighting when SVg is calculated in a given region (and result in values of gas per gram of tissue which are not physical). Very low attenuation values frequently occur in severe emphysema, where the density of the lungs is much lower than normal parenchyma and falls in a range where few, if any, manufacturers have optimized their scanners. Some systems, for instance, have significant and varying offsets at air density. Therefore, detailed quantitative CT for emphysema is dependent on the accuracy of air calibration. The presence of these very low attenuation values can also be due to artifacts of the reconstruction algorithms or to airways lying perpendicular to the slice and traversing its full thickness [8]. The choice of reconstruction parameters (i.e. filter reconstruction and slice thickness) significantly influences the presence and the amount of extremely low attenuation values and thus cannot be ignored. In fact, higher resolution filters as “bone”, “sharp,” and “very sharp” preserve the higher spatial frequencies, which results in better spatial resolution and edge detection in an image, at the expense of greater noise. On the other hand, softer filters as “smooth” and “soft” reduce the higher-frequency contribution, which decreases noise but also degrades spatial resolution [9]. The purpose of the present work is to study if and how different filters and scanner manufacturers significantly influence the distribution of attenuation (and consequently SVg) in the reconstructed image, particularly in lungs with significant fractions of very low-attenuation pixels. To do this, we analyzed CT data acquired both in healthy subjects and in patients with severe emphysema at two different lung volumes and obtained with different reconstruction parameters (namely, thick slice thickness with smooth filter and thin slice thickness with sharp filter), to study their effects on SVg distribution and SVg variation relative to lung volume variation.
Figure 1.
Relationship between Hounsfield Units (HU) and corresponding value of Specific Gas volume (SVg, ml/g) for very low attenuation values, where −1024 HU represents zero x-ray attenuation. Clearly, low-attenuation voxels have disproportionately high SVg.
MATERIALS AND METHODS
Subjects and Specimens
Two different sets of CT images were analyzed and obtained from: 1) ten healthy volunteers (3 males/7 females, age 44 ±6 years, weight 67±5 Kg, height 178±32 cm) with no history of smoking or lung disease and normal spirometric values; 2) eighteen subjects with severe emphysema, whose data originated from different locations and were part of the pre-treatment assessment database of a clinical trial evaluating the safety and effectiveness of a new procedure called airway bypass (ClinicalTrials.gov Identifier: NCT00391612). Inclusion criteria for the new treatment were smoking history, high resolution CT scan with evidence of homogeneous emphysema, post-bronchodilator pulmonary function tests showing: a ratio of FEV1/FVC < 70%, FEV1 ≤ 50% of predicted or FEV1 < 1 liter, RV/TLC ≥ 0.65 at screening. Local ethical committee reviews and approvals were obtained, and written informed consent was obtained from all the patients. The Institutional Review Board of Washington University in St. Louis approved the protocol for healthy humans; informed written consent was obtained from each healthy subject.
CT imaging
In healthy subjects CT was performed using a Siemens scanner (Somatom Definition Dual Source CT, DSCT; Siemens, Forchheim, Germany). In patients with emphysema, CT was performed by the same type of Siemens scanner in ten subjects, and by a GE scanner (Light Speed VCT; GE Healthcare, Milwaukee, WI, USA) in eight patients.
Transverse-plane CT images of healthy subjects were reconstructed with the following two different settings: a) thin slice thickness (1 mm) and sharp reconstruction filter (B50f); b) thick slice thickness (5 mm) and smooth reconstruction filter (B30f).
Transverse-plane CT images of subjects with emphysema acquired with GE scanners were reconstructed with a) thin slice thickness (1 mm) and sharp reconstruction filter (B50f) and b) thick slice thickness (5 mm) and smooth reconstruction filter (B30f).
Transverse-plane CT images of subjects with emphysema acquired with Siemens scanners were reconstructed with a) thin slice thickness (1 mm) and sharp reconstruction filter (B50f) and b) thick slice thickness (10 mm) and smooth reconstruction filter (B30f).
Scanner settings were: tube voltage, 120 kV; tube current, 110 mA; matrix 512×512. The CT raw data were reconstructed as contiguous transverse images in all cases. Healthy and emphysematous subjects were scanned during suspended end-inspiration at total lung capacity (TLC) and during suspended end-expiration at or near residual volume (RV). The radiologist instructed the subjects on the importance of breath-holding and immobility during scanning and on attaining reproducible maximum inspiratory and expiratory breath-hold identical to their pulmonary function tests.
CT image analysis
All CT images were first automatically segmented to accurately extract the lungs from CT images at the two different lung volumes using custom software developed in Matlab (Mathworks). First, the lungs were extracted from the CT images by using an optimal thresholding method [10] to automatically choose a threshold value to separate lung tissue from the chest wall, mediastinum, and large blood vessels. The surrounding air, identified as low-density tissue, was removed and morphological opening was used to eliminate the residual noise in the background. The left and right lungs were then separated by detecting the anterior and posterior junctions. Finally, the lung boundary along the mediastinum was optionally smoothed. For the following quantitative analysis, lung was defined as all material in each segmented CT slice with a Hounsfield Unit value ≤ −600.
In order to characterize the patient group in terms of disease severity, an emphysema index was calculated from CT images taken at both TLC and RV as the percentage of lung pixels with an attenuation value lower than a specific threshold. Attenuation thresholds of −950 HU form images of 1 mm section thickness and −910 HU for images 5–10 mm thick were chosen. For each segmented set of images obtained at different lung volumes the histograms of all pixels attenuation values were determined for both healthy subjects and emphysema patients. For each setting, in both healthy subjects and emphysema patients, specific gas volume (SVg) for each voxel of the segmented lungs was automatically calculated as (1):
| (1) |
where specific volume (ml/g) is the inverse of density (g/ml). The specific volume of the lung (tissue and gas) was measured from the CT as (2):
| (2) |
On the basis of existing literature [11], the specific volume of tissue was assumed to be
| (3) |
In equation (2), HU is the CT raw data rescaled into Hounsfield Units according to the linear transformation:
| (4) |
In the CT scanners used in the present study (Siemens, GE) RescaleIntercept is equal to −1024 and therefore this value represents zero density.
The volume of the lungs was calculated by summing the volumes of each voxel of the segmented lungs.
Statistical analysis
Statistical analysis was performed by SigmaStat software v11.0 (San Jose, California, USA). The influence of presence of disease, lung volume and reconstruction filter and their interactions on SVg and ΔSVg values was studied by analyzing the data obtained only by Siemens scanners through a three-way analysis of variance (ANOVA). The influence of scanner, lung volume and reconstruction filter and their interactions on SVg and ΔSVg values was studied by analyzing the data obtained only on COPD patients by a three-way analysis of variance (ANOVA). In the cases where the data were not normally distributed, nonparametric Kruskal-Wallis ANOVA on ranks was applied. Posthoc tests were based on Holm-Sidak and Dunn methods, for parametric and nonparametric ANOVA tests, respectively. All data are reported as mean values±standard error. P values lower than 0.05 were considered to indicate significant differences.
RESULTS
Lung volume assessed by CT and emphysema index values (calculated from the two considered reconstruction settings, i.e. thin slice thickness/sharp reconstruction filter and thick slice thickness/smooth reconstruction filter) are reported in Tables 1 and 2, respectively for healthy subjects and patients with emphysema. Compared to healthy subjects, patients were characterized by very high lung volumes at both TLC and RV, emphysema index values and the high values of RV/TLC (>63% in all patients) indicating a high degree of lung hyperinflation as requested by the clinical trial inclusion criteria (>65%).
Table 1.
CT volumes and emphysema index values in healthy subjects.
| CT Volume (L) | Emphysema Index (%) | ||||||
|---|---|---|---|---|---|---|---|
| Subject# | TLC(1) | RV(1) | RV/TLC(%) | TLC(2) | RV(2) | TLC(3) | RV(3) |
| S1 | 6.13 | 1.76 | 28.74 | 25 | 2 | 45 | 1 |
| S2 | 5.83 | 1.11 | 19.02 | 23 | 1 | 43 | 1 |
| S3 | 4.33 | 1.63 | 37.68 | 13 | 1 | 8 | 1 |
| S4 | 5.48 | 2.90 | 53.01 | 23 | 5 | 38 | 3 |
| S5 | 9.20 | 2.51 | 27.33 | 27 | 3 | 41 | 1 |
| S6 | 5.44 | 1.27 | 23.27 | 20 | 1 | 34 | 1 |
| S7 | 3.70 | 0.86 | 23.16 | 14 | 0 | 6 | 1 |
| S8 | 4.65 | 1.65 | 35.54 | 17 | 0 | 12 | 1 |
| S9 | 5.46 | 1.23 | 22.52 | 24 | 0 | 33 | 1 |
| S10 | 4.41 | 1.14 | 25.88 | 25 | 0 | 42 | 0 |
| Mean | 5.46 | 1.61 | 29.62 | 21 | 1 | 30 | 1 |
| SD | 1.52 | 0.65 | 10.06 | 5 | 2 | 15 | 1 |
| SE | 0.48 | 0.21 | 3.18 | 2 | 0 | 5 | 0 |
Calculated with from images reconstructed with B50f (thickness=1 mm);
Calculated with threshold at −950 HU (images reconstructed with B50f and thickness=1 mm);
Calculated with threshold at −910 HU (images reconstructed with B30f and thickness=5 mm).
Table 2.
CT volumes and emphysema index values in patients with emphysema.
| CT Volume (L) | Emphysema Index (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Patient# | Scanner | TLC(1) | RV(1) | RV/TLC(%) | TLC(2) | RV(2) | TLC(3) | RV(3) |
| P1 | 1 | 7.81 | 6.67 | 85.38 | 57 | 53 | 76 | 70 |
| P2 | 1 | 5.69 | 4.58 | 80.51 | 53 | 49 | 70 | 63 |
| P3 | 1 | 8.00 | 7.12 | 88.93 | 55 | 54 | 71 | 69 |
| P4 | 2 | 5.46 | 4.74 | 86.87 | 38 | 32 | 61 | 52 |
| P5 | 2 | 4.88 | 3.88 | 79.56 | 33 | 24 | 53 | 42 |
| P6 | 1 | 7.39 | 6.39 | 86.42 | 44 | 40 | 54 | 43 |
| P7 | 2 | 4.73 | 3.51 | 74.07 | 19 | 12 | 37 | 18 |
| P8 | 1 | 7.56 | 5.73 | 75.76 | 47 | 42 | 60 | 46 |
| P9 | 1 | 7.33 | 5.29 | 72.15 | 47 | 40 | 63 | 44 |
| P10 | 2 | 5.73 | 4.50 | 78.46 | 39 | 30 | 55 | 43 |
| P11 | 2 | 5.87 | 3.73 | 63.64 | 40 | 27 | 60 | 39 |
| P12 | 2 | 4.75 | 3.72 | 78.39 | 37 | 30 | 58 | 47 |
| P13 | 1 | 8.85 | 7.34 | 82.94 | 49 | 44 | 64 | 55 |
| P14 | 1 | 5.26 | 5.14 | 97.66 | 42 | 41 | 45 | 50 |
| P15 | 1 | 7.13 | 4.77 | 66.88 | 44 | 37 | 57 | 34 |
| P16 | 1 | 7.89 | 6.47 | 82.01 | 46 | 42 | 59 | 48 |
| P17 | 2 | 8.94 | 6.95 | 77.79 | 37 | 27 | 61 | 45 |
| P18 | 2 | 5.44 | 3.56 | 65.48 | 34 | 19 | 59 | 31 |
| Mean | 6.60 | 5.23 | 79.05 | 42 | 36 | 59 | 47 | |
| SD | 1.42 | 1.32 | 8.68 | 9 | 11 | 9 | 13 | |
| SE | 0.33 | 0.30 | 1.99 | 2 | 3 | 2 | 3 | |
Calculated with from images reconstructed with B50f (thickness=1 mm);
Calculated with threshold at −950 HU (images reconstructed with B50f and thickness=1 mm);
Calculated with threshold at −910 HU (images reconstructed with B30f and thickness=5 or 10 mm).
CT scanner: 1=Siemens; 2=GE
Emphysema index values were significantly affected by reconstruction settings (P<0.001); namely, they resulted generally higher when using the reconstruction setting thin slice/sharp filter.
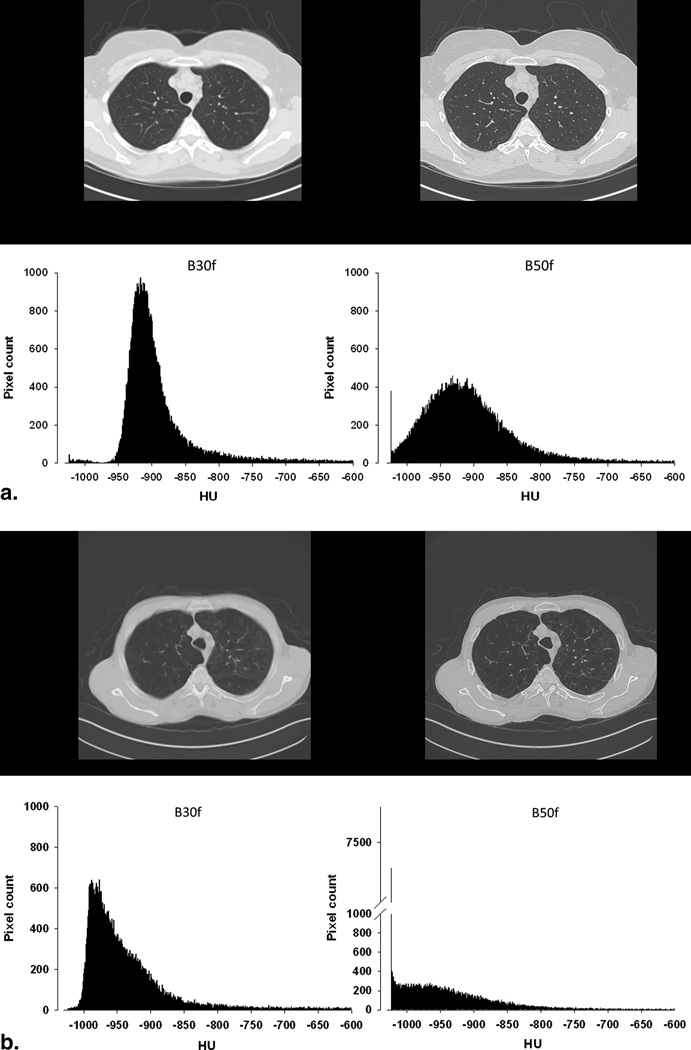
Two representative illustrations of the effects of the reconstruction settings on the histograms of attenuation values are presented in Figures 2a (healthy subject) and 2b (emphysematous subject). In each figure, the same slices taken at TLC with the corresponding attenuation histograms are shown as reconstructed by using the two different reconstruction filters.
Figure 2.
a. Histograms of HU values occurrence at Total Lung Capacity (TLC) from one selected slice of a healthy subject reconstructed with a smooth filter (B30f) and thick slice thickness (left panel) and with a sharp filter (B50f) and thin slice thickness (right panel).
b. Histograms of HU values occurrence at Total Lung Capacity (TLC) from one selected slice of a patient with emphysema reconstructed with a smooth filter (B30f) and thick slice thickness (left panel) and with a sharp filter (B50f) and thin slice thickness (right panel). In the emphysema patient histogram of the image reconstructed with the sharp filter, a spike at HU=−1024 is present.
With the reconstruction setting thin slice/sharp filter (B50f, left panels), in both healthy subjects and patients with emphysema, a significant number of pixels with HU = −1024 HU is present, particularly in emphysema. These spikes disappear when the image was reconstructed with the reconstruction setting thick slice/smooth filter (B30f, right panels).
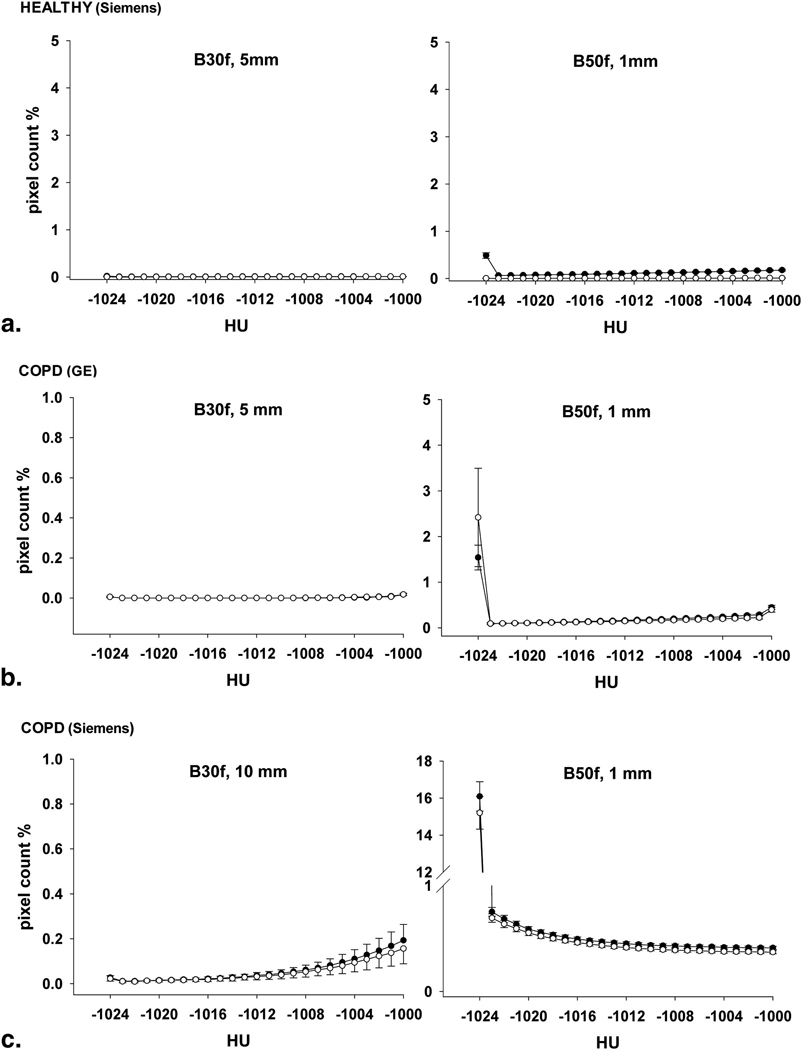
Figure 3 reports the average values of pixel counts in the very low attenuation range for all subjects (from HU=−1024 to HU=−1000) and show how the representative results illustrated in Figures 2a and 2b are generally valid.
Figure 3.
Pixel count in percentage of the all pixels inside the lungs at TLC and RV of the CT data reconstructed with the thick slice thickness and the smooth filter (B30f) (left panel) and with the thin slice thickness and sharp filter (B50f) (right panel)..A) Healthy subjects (n=10); B) patients analyzed with GE scanners (n=8); C) patients analyzed with Siemens scanners (n=10).
Each value represents the average ± S.E. Closed circles: TLC; open circles: RV.
In healthy subjects, with the setting thin slice/sharp filter at TLC the pixels with HU=−1024 were on average equal to ~0.5% of the total number of pixels in the segmented lung; that percentage became negligible at RV. In total, the percentage of pixels with attenuation value < −1000 was on average equal to 3.3 ± 1.1 % and 0.1 ±0.2%, respectively at TLC and RV. With the reconstruction setting thick slice/smooth filter, a negligible number of pixels were found in the same attenuation range both at TLC and RV (percentage of pixels < −1000 HU was equal to only 0.2 ± 0.06% and 0.1 ± 0.09 %, respectively at TLC and RV).
Subjects with emphysema were drastically different. With the setting thin slice/sharp filter (B50f), the pixels with HU=−1024 were on average equal to ~15–16% and ~1.7–2.4% of the total number of pixels in the segmented lung, respectively with Siemens and GE scanners. In total, the percentage of pixels with attenuation value <−1000 was on average equal to 27.8±3.8% and 26.0 ± 4.0 %, respectively at TLC and RV, in the Siemens scanners and to 0.24±0.09% and 0.25±0.2% in GE scanners. These high lung fractions will clearly distort measures of trapped gas using SVg.
With the reconstruction setting thick slice/smooth filter (B30f), the peak at −1024 HU disappeared both in Siemens and in GE scanners and changed the histogram in the very low attenuation range. In total, the percentage of pixels with attenuation value < −1000 was on average equal to 1.5±1.6% and 1.2±1.7%, respectively at TLC and RV, in the Siemens scanners and to 0.002±0.000% and 0.002±0.000% in GE scanners. In general, lung volume did not affect the shape of the pixel attenuation value histograms or the affect of the reconstruction filters in the very low attenuation range.
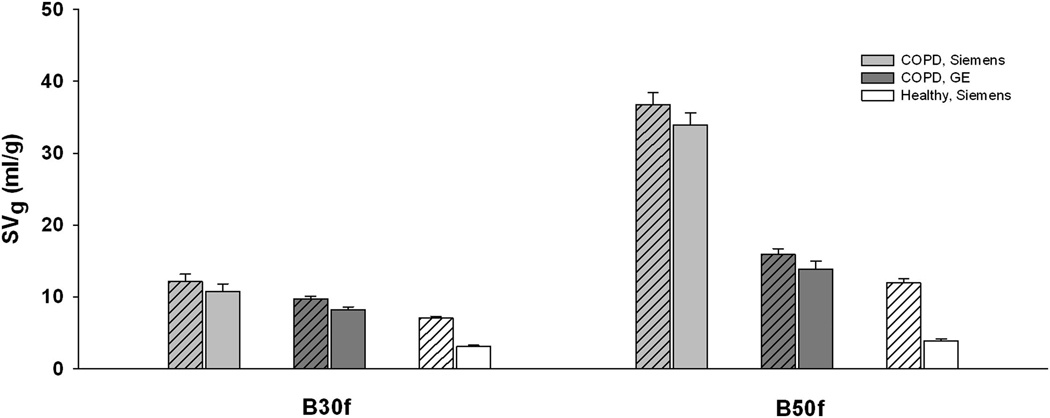
Figure 4 shows how average absolute values of SVg in the overall lung are influenced by reconstruction filter, lung volume and scanner type in patients with emphysema and healthy subjects. As expected, due to the presence of emphysema and gas trapping, SVg values were in general significantly higher in patients than in healthy subjects, both at TLC and RV (P<0.001). As also expected, SVg values were generally higher at TLC than at RV, both in healthy and emphysema subjects, but the effect of the volume, however, was more marked in the healthy subjects (P<0.001 and P=0.039, respectively). ANOVA analysis revealed that in both emphysema patients and healthy volunteers, absolute SVg was significantly influenced by the reconstruction filter (P<0.001), namely that SVg values were lower when using the reconstruction setting thick slice/smooth filter. The effect of the filter, providing lower values of SVg with B30f compared to B50f, was present both in Siemens and in GE scanners (P<0.001 and P=0.032, respectively), but was more marked in the former. Considering the same filter, SVg values obtained in emphysema patients from Siemens scanners were significantly higher than those obtained from GE scanners (P<0.001). Considering the same lung volume, ANOVA analysis revealed that SVg values by Siemens and GE scanners were not significantly different, both at TLC (P=0.060) and at RV (P=0.150).
Figure 4.
Specific gas volume values (SVg, ml/g) calculated in the whole lung in 10 healthy subjects acquired with a Siemens scanner (white bars); in 10 patients with emphysema acquired with Siemens scanners (gray bar) and in 8 patients with emphysema acquired with GE scanners (dark gray bar), at TLC and RV. Each bar represents the average ± S.E.
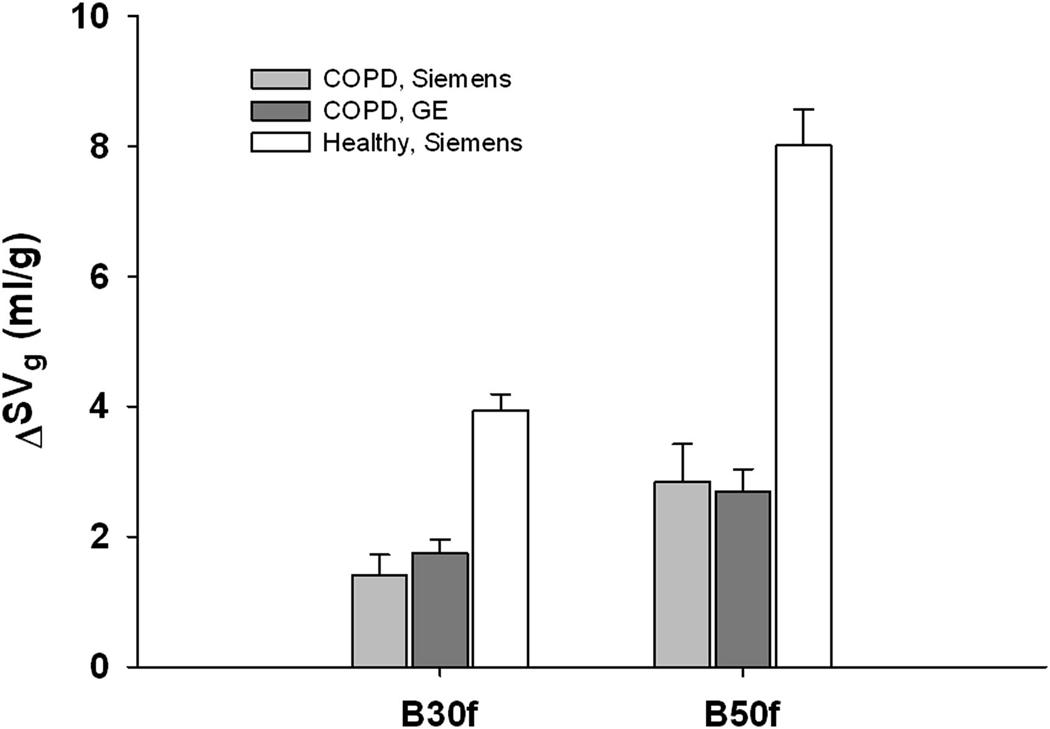
As expected, differences of specific gas volume between TLC and RV (ΔSVg) were generally lower in patients than in healthy subjects (P<0.001), representing higher amounts of trapped gas (Figure 5). The reconstruction setting significantly influenced this difference, with the thin slice/sharp reconstruction filter providing higher values ΔSVg. In particular, B50f doubled ΔSVg both in patients with emphysema and in healthy subjects: from 1.41±0.75 ml/g with B30f to 2.85±0.57 ml/g with B50f in patients analyzed by Siemens scanners (P=0.041); from 1.75±0.21 ml/g with B30f to 2.69±0.35 ml/g with B50f in patients analyzed by GE scanners (P=0.038); from 3.93±0.26 ml/g with B30f to 8.02±0.56 ml/g with B50f (P<0.001) in healthy subjects. Finally, ANOVA analysis revealed that ΔSVg values obtained in emphysema patients by Siemens and GE scanners were not significantly different (P=0.829). No interactions were found between scanner type and reconstruction filter on ΔSVg values.
Figure 5.
Differences of specific gas volume values from TLC to RV (ΔSVg = SVg,TLC-SVg,RV) calculated in the whole lung in 10 healthy subjects (white bar), in 10 patients with emphysema acquired with Siemens scanners (gray bar) and in 8 patients with emphysema acquired with GE scanners (dark gray bar). Each bar represents the average ± S.E.
DISCUSSION
For the quantification of the amount of trapped gas inside the lung via specific gas volume (SVg), it is necessary to account for the number of very low attenuation lung pixels, which have a strong impact on the calculation of SVg because of their disproportionate weighting. Our initial hypothesis was that the distribution of these very low attenuation values is dependent on the reconstruction algorithm used, and particularly by slice thickness and reconstruction filter. Therefore, in the present study we investigated how two different reconstruction settings (thick slice associated with a smooth filter (B30f) and thin slice associated with a sharp filter (B50f)) and two different brands of scanner (Siemens and GE) affect the presence and amount of extremely low attenuation pixel values and lung densitometry, namely specific gas volume calculations in both emphysematous and healthy lungs. Our main finding is that these effects are dramatic and statistically significant. Very low attenuation values are present in CT images when a thin slice/sharp reconstruction filter is used, particularly in patients with severe emphysema acquired with Siemens scanners (26–28% of the total number of pixels). The presence of these very low attenuation pixel values disappears when the reconstruction setting thick slice/smooth reconstruction filter is instead used.
In general, low spatial frequency algorithms provide optimal image contrast at the expense of spatial resolution. High spatial-frequency algorithms provide high spatial resolution at the expense of contrast resolution. Standard algorithms usually consider either medium spatial frequency filters (e.g. B30f) associated with thick collimation slices (e.g. 5 or 10 mm) or the high spatial resolution algorithms (e.g. B50f) associated with thin slices (e.g. 1 mm). Nowadays there is also a tendency in the clinical practice for lung CT analysis to obtain thin slice CT scans so that airways can be assessed.
Kemerink et al. [12] reported that zoom factor and reconstruction filter had a negligible influence on quantitative lung densitometry, with the exception of the ultra- high resolution filter in the case of extremely low lung density. This suggests that a relationship between CT reconstruction parameters and quantification of gas in the lungs (separate from tissue) exists, and it likely has important implications for the application of quantitative emphysema analysis to CT scans obtained in clinical research studies. This is particularly true when specific gas volume is used to evaluate regional emphysema or trapped gas, as highlighted by the relationship between HU and SVg shown in Figure 1. Our results indicate that the most reliable means of ensuring valid quantification of specific gas volume and trapped gas inside the lung is to use a reconstruction setting combining thick slice with a smooth reconstruction filter, to avoid the larger fraction of pixels with very low attenuation. This choice could require separately-reconstructed data when detailed studies on airways are needed.
This is in agreement with the workshop report [13], in which stated that a smooth reconstruction algorithm (B30f) should be used to avoid the errors described by Kemerink et al. [12] with the ultra- high resolution filter. The workshop agreed that all CT scans should be acquired in such a fashion as to enable the reconstruction of image data with larger slice thicknesses, i.e.7 mm, and with a standard reconstruction filter (B30f) or a better customized filter that might further optimize the determination of lung density or other important image measurements. More recently, Gierada et al. [14] found that the effects of section thickness and reconstruction kernel on CT measurements of emphysema varied in a systematic manner related to the emphysema index magnitude as assessed by density mask technique. Boedeker et al. and Gierada et al. [15,14] demonstrated that the choice of reconstruction algorithm can have a substantial effect on quantitative measures extracted from CT lung images in patients with emphysema. Yuan et al [16] found that image acquisition parameter including radiation dose, scanner type, and subject’s breath size should be standardized to estimate emphysema severity in longitudinal studies. None of these studies, however, have evaluated the effects of the reconstruction algorithms on SVg or the effects of large areas with very low x-ray attenuation.
There is a recent body of evidence that changes in SVg can be suitably used to study regional ventilation [17] and to define severity thresholds in severe emphysema [18]. We have recently shown that SVg determined at different lung volumes provides a useful method for identifying and quantifying the extent and severity of trapped gas [3]. In the present study we originally demonstrate that the presence of very low attenuation values, which occurs in an important manner in patients with severe emphysema when thin slice and sharp reconstruction filter are used, strongly influences the assessment of SVg. Therefore, particular attention must be paid in order to avoid the use of thin slices and sharp filters when calculating specific gas volume.
The main limitation of this study, due to the data available from the database of the clinical trial and healthy subjects, was not to consider all the possible combinations of slice thicknesses, reconstruction filters and brands of CT scanner. As a consequence, we were not able to provide conclusive data on the distinct effects of these parameters on the SVg calculation. However, the chosen combinations of slice thickness and reconstruction filters allowed consistency of data and congruence with common clinical settings.
Another slight limitation is represented by the relative small patient population, however, our results demonstrate consistency within each group of subjects and high statistical significance.
Our study included comparison between only two different CT scanner type (Siemens and GE) again due to the availability of these data in the database of the clinical trial. With only two brands of CT scanners, however, we were able to obtain results demonstrating how different CT scanners provide different absolute values of SVg. It must be noted, however, that when considering differences of SVg between high and low lung volumes (ΔSVg), this effect disappears. Moreover, the relative proportion between ΔSVg values of patients and healthy controls is very reproducible with different reconstruction settings (Fig. 5) and therefore this parameter provides in general more robust results.
In conclusion, quantitative CT analysis of the lung parenchyma in patients with emphysema based on images reconstructed with thin-slice and sharp filter algorithms is highly imprecise. The disproportionate effect of low-attenuation pixels on SVg, which likely causes overestimation of the severity of emphysema, can be significantly reduced by using thicker slices (5–10 mm) combined with a smooth filter (B30f) for image reconstruction. Variations of SVg between high and low lung volume, are in general more robust than SVg alone and allow quantification of the functional impairment of the lung in severe emphysema.
Acknowledgments
This work was supported by a NIH grant R01- HL090806.
References
- 1.Goldin JG. Imaging the lungs in patients with pulmonary emphysema. J Thorac Imaging. 2009 Aug;24(3):163–170. doi: 10.1097/RTI.0b013e3181b41b53. [DOI] [PubMed] [Google Scholar]
- 2.Coxson HO, Rogers RM, Whittall KP, D'yachkova Y, Paré PD, Sciurba FC, Hogg JC. A quantification of the lung surface area in emphysema using computed tomography. Am J Respir Crit Care Med. 1999 Mar;159(3):851–856. doi: 10.1164/ajrccm.159.3.9805067. [DOI] [PubMed] [Google Scholar]
- 3.Salito C, Aliverti A, Gierada DS, Deslée G, Pierce RA, Macklem PT, Woods JC. Quantification of trapped gas with CT and 3 He MR imaging in a porcine model of isolated airway obstruction. Radiology. 2009 Nov;253(2):380–389. doi: 10.1148/radiol.2532081941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choong CK, Macklem PT, Pierce JA, Das N, Lutey BA, Martinez CO, Cooper JD. Airway bypass improves the mechanical properties of explanted emphysematous lungs. Am J Respir Crit Care Med. 2008 Nov 1;178(9):902–905. doi: 10.1164/rccm.200712-1832OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venuta F, Rendina EA, Coloni GF. Endobronchial treatment of emphysema with one-way valves. Thorac Surg Clin. 2009 May;19(2):255–260. doi: 10.1016/j.thorsurg.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Berger RL, Decamp MM, Criner GJ, Celli BR. Lung volume reduction therapies for advanced emphysema: an update. Chest. 2010 Aug;138(2):407–417. doi: 10.1378/chest.09-1822. [DOI] [PubMed] [Google Scholar]
- 7.Kemerink GJ, Kruize HH, Lamers RJ, van Engelshoven JM. Density resolution in quantitative computed tomography of foam and lung. Med Phys. 1996 Oct;23(10):1697–1708. doi: 10.1118/1.597757. [DOI] [PubMed] [Google Scholar]
- 8.Fromson BH, Denison DM. Quantitative features in the computed tomography of healthy lungs. Thorax. 1988 Feb;43(2):120–126. doi: 10.1136/thx.43.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boedeker KL, McNitt-Gray MF, Rogers SR, Truong DA, Brown MS, Gjertson DW, Goldin JG. Emphysema: effect of reconstruction algorithm on CT imaging measures. Radiology. 2004 Jul;232(1):295–301. doi: 10.1148/radiol.2321030383. [DOI] [PubMed] [Google Scholar]
- 10.Hu S, Hoffman EA, Reinhardt JM. Automatic lung segmentation for accurate quantitation of volumetric X-ray CT images. IEEE Trans Med Imaging. 2001 Jun;20(6):490–498. doi: 10.1109/42.929615. [DOI] [PubMed] [Google Scholar]
- 11.Hedlund LW, Vock P, Effmann EL. Evaluating lung density by computed tomography. Semin Respir Med. 1983;5:76–87. [Google Scholar]
- 12.Kemerink GJ, Lamers RJ, Thelissen GR, van Engelshoven JM. CT densitometry of the lungs: scanner performance. J Comput Assist Tomogr. 1996;20:24–33. doi: 10.1097/00004728-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Newell JD, Jr, Hogg JC, Snider GL. Report of a workshop: quantitative computed tomography scanning in longitudinal studies of emphysema. Eur Respir J. 2004 May;23(5):769–775. doi: 10.1183/09031936.04.00026504. [DOI] [PubMed] [Google Scholar]
- 14.Gierada DS, Bierhals AJ, Choong CK, Bartel ST, Ritter JH, Das NA, Hong C, Pilgram TK, Bae KT, Whiting BR, Woods JC, Hogg JC, Lutey BA, Battafarano RJ, Cooper JD, Meyers BF, Patterson GA. Effects of CT section thickness and reconstruction kernel on emphysema quantification relationship to the magnitude of the CT emphysema index. Acad Radiol. 2010 Feb;17(2):146–156. doi: 10.1016/j.acra.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boedeker KL, McNitt-Gray MF, Rogers SR, Truong DA, Brown MS, Gjertson DW, Goldin JG. Emphysema: effect of reconstruction algorithm on CT imaging measures. Radiology. 2004 Jul;232(1):295–301. doi: 10.1148/radiol.2321030383. [DOI] [PubMed] [Google Scholar]
- 16.Yuan R, Mayo JR, Hogg JC, Paré PD, McWilliams AM, Lam S, Coxson HO. The effects of radiation dose and CT manufacturer on measurements of lung densitometry. Chest. 2007 Aug;132(2):617–623. doi: 10.1378/chest.06-2325. [DOI] [PubMed] [Google Scholar]
- 17.Fuld MK, Easley RB, Saba OI, Chon D, Reinhardt JM, Hoffman EA, Simon BA. CT-measured regional specific volume change reflects regional ventilation in supine sheep. J Appl Physiol. 2008;104(4):1177–1184. doi: 10.1152/japplphysiol.00212.2007. [DOI] [PubMed] [Google Scholar]
- 18.Mathews JJ, Maurer AH, Steiner RM, Marchetti N, Criner G, Gaughan JP, Coxson HO. New 133Xe gas trapping index for quantifying severe emphysema before partial lung volume reduction. J Nucl Med. 2008;49(5):771. doi: 10.2967/jnumed.107.048637. [DOI] [PubMed] [Google Scholar]