Abstract
Background:
Cryptococcus neoformans is the most common fungal pathogen to infect the central nervous system, and an effective diagnostic method is therefore necessary for the early diagnosis of cryptococcal meningitis.
Aim:
The efficacy of India ink preparation, cerebrospinal fluid (CSF) culture and CSF cryptococcal antigen detection by the latex agglutination test for diagnosis of cryptococcal meningitis are compared to determine the most efficient test.
Materials and Methods:
Two hundred CSF samples from human immunodeficiency virus - positive patients suspected to be suffering from meningitis were screened for Cryptococcus neoformans.
Results:
Latex agglutination for cryptococcal antigen detection was found to be more sensitive compared to India ink staining and CSF culture.
Conclusions:
Antigen detection by latex agglutination proved to be both sensitive and specific method for the diagnosis of cryptococcal meningitis. Rapid, early diagnosis of infection by detection of cryptococcal antigen by latex agglutination may alter the prognosis for these patients.
Keywords: Antigen detection, Cryptococcus, India ink
INTRODUCTION
Cryptococcal meningitis is caused by Cryptococcus neoformans which is the most common fungal pathogen of the central nervous system (CNS).[1] Unless diagnosed early and specific treatment instituted, cryptococcosis is often fatal and can cause severe neurological sequelae even after clinical cure. Though once known to be rare, cryptococcosis has occurred at a high frequency in India in the past two decades. [2–7] It is gaining importance due to the rising population of immunocompromised patients especially those with acquired immunodeficiency syndrome (AIDS).[8] Cryptococcal meningitis is the fourth most commonly recognized cause of life-threatening infection among AIDS patients.[9] In AIDS patients, it is characterized by lack of meningeal signs and diminished inflammatory response.[10]
Conventional methods such as culture and India ink are specific but cumbersome and time consuming.[11] Rapid diagnosis is essential for prompt therapy as mortality due to infection is high.[12] This study was therefore carried out to compare and evaluate the conventional methods with cryptococcal antigen detection by the latex agglutination (LA) test.
MATERIALS AND METHODS
Two hundred cerebrospinal fluid (CSF) samples from human immunodeficiency virus (HIV)-positive patients suffering from meningitis were screened for Cryptococcus neoformans using India ink preparation, culture on Sabouraud's dextrose agar (SDA) and cryptococcal antigen detection by the LA test (Murex). Cultures were incubated at 37°C and 25-27°C.
Suspected growth on SDA was confirmed as Cryptococcus neoformans by its ability to produce phenol oxidase on caffeic acid agar and urease production on Christensen's urea medium.
RESULTS
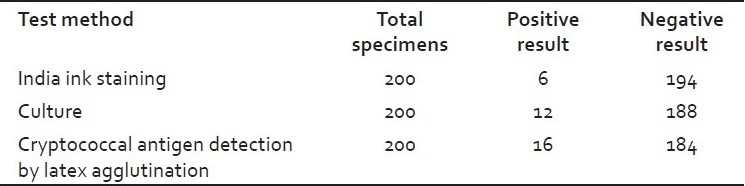
It was observed that only six patients were positive by India ink preparation. Most cultures were positive after 72 h incubation. It was also observed that in four patients, antigen detection was positive though the culture was negative [Table 1]. In all these patients, empirical antifungal treatment was started on suspicion of cryptococcal meningitis immediately on admission. Hence, this could probably be the reason for culture being negative.
Table 1.
Comparison of India ink, culture, and latex agglutination
DISCUSSION
Cryptococcosis is the most common systemic fungal infection in AIDS[13] and its incidence is increasing with the rapid spread of AIDS. The CSF may appear normal in these patients with cryptococcal meningitis and many of them have normal levels of protein and glucose in CSF. Classical meningeal symptoms occur in only about a quarter or one-third of the patients that cause delay in the diagnosis. Asymptomatic patients may have a positive culture of CSF with no other abnormality of the fluid.[9]
Culture is considered to be the “gold standard” method of diagnosis for Cryptococcus neoformans, but it takes at least 3 days to a maximum time of a month for growth. The other method is by the demonstration of encapsulated yeasts in India ink preparations from CSF which though specific shows poor sensitivity (50-80%).[14] Antigen detection represents the most immediate and rapid way to enhance methods for diagnosis of cryptococcosis.[15–17] It is a highly and rapid test, and the antigen can remain detectable for several months after infection.[18]
A comparison of the three methods in our study revealed that India ink staining though rapid and specific (specificity: 100%) was not so sensitive (sensitivity: 50%). Antigen detection has thus proved to be both a sensitive and specific method for diagnosis of cryptococcal meningitis (16 positive) compared to culture (12 positive) and India ink staining (6 positive). It is also a rapid diagnostic method. False positive latex agglutination reactions are seen in infections with Trichosporon beigelli and DF-2 bacillus (dysgonic fermenter-2 bacillus is a fastidious gram negative bacillus; this designation is given by the Center for Disease Control), both of which can be easily diagnosed clinically from cryptococcal infection.[19]
CONCLUSIONS
With the rising incidence of AIDS, cryptococcal infection in suspected cases of meningitis should be kept in mind while establishing a diagnosis. Rapid, early diagnosis of infection by detection of cryptococcal antigen by latex agglutination when compared to culture and India ink examination of CSF and subsequent treatment may alter the prognosis for these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dismukes WE. Cryptococcal meningitis in patients with AIDS. J Infect Dis. 1988;157:624–8. doi: 10.1093/infdis/157.4.624. [DOI] [PubMed] [Google Scholar]
- 2.Banerjee U. Cryptococcosis at AIIMS. Natl Med J India. 1994;7:51–2. [PubMed] [Google Scholar]
- 3.Banerjee U, Datta K, Majumdar T, Gupta K. Cryptococcosis in India: The awakening of a giant? Med Mycol. 2001;39:51–67. doi: 10.1080/mmy.39.1.51.67. [DOI] [PubMed] [Google Scholar]
- 4.Banerjee U, Datta K, Casadevall A. Serotype distribution of Cryptococcus neoformans in patients in a tertiary care centre in India. Med Mycol. 2004;42:181–6. doi: 10.1080/13693780310001615376. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee U. Progress in diagnosis of opportunistic infections in HIV/AIDS. Indian J Med Res. 2005;121:395–406. [PubMed] [Google Scholar]
- 6.Chakrabarti A, Gupta B. Isolated detection of cryptococcal polysaccharide antigen in patients with cryptococcosis. Clin Infect Dis. 1997;25:1494–5. doi: 10.1086/517012. [DOI] [PubMed] [Google Scholar]
- 7.Chakrabarti A, Sharma A, Sood A, Grover R, Sakhuja V, Prabhakar S, et al. Changing scenario of cryptococcosis in a tertiary care hospital in north India. Indian J Med Res. 2000;112:56–60. [PubMed] [Google Scholar]
- 8.Kozel TR. Virulence factors of Cryptococcus neoformans. Trends Microbiol. 1995;3:295–9. doi: 10.1016/s0966-842x(00)88957-x. [DOI] [PubMed] [Google Scholar]
- 9.Kwon-Drung KJ, Bennette JE, editors. Medical mycology. London: Lea and Febiger; 1992. pp. 396–439. [Google Scholar]
- 10.Chuck SL, Sande MA. Infections with Cryptococcus neoformans in acquired immunodeficiency syndrome. N Engl J Med. 1989;321:794–9. doi: 10.1056/NEJM198909213211205. [DOI] [PubMed] [Google Scholar]
- 11.Saha DC, Xess I, Jain N. Evaluation of conventional and serological methods for rapid diagnosis of cryptococcosis. Indian J Med Res. 2008;127:483–8. [PubMed] [Google Scholar]
- 12.Iyer RS, Banker DD. Cryptococcal meningitis in AIDS. Indian J Med Sci. 2002;56:593–7. [PubMed] [Google Scholar]
- 13.Powderly WG. Cryptococcal meningitis in HIV-infected patients. Current Infectious Disease Reports. 2000;2:352–7. doi: 10.1007/s11908-000-0015-y. [DOI] [PubMed] [Google Scholar]
- 14.Snow RM, Dismukes WE. Cryptococcal meningitis: Diagnostic value of cryptococcal antigen in cerebrospinal fluid. Arch Intern Med. 1975;135:1155–7. doi: 10.1001/archinte.135.9.1155. [DOI] [PubMed] [Google Scholar]
- 15.Diamond RD, Bennett JE. Prognostic factors in cryptococcal meningitis: A study in 11 cases. Ann Intern Med. 1974;80:176–81. doi: 10.7326/0003-4819-80-2-176. [DOI] [PubMed] [Google Scholar]
- 16.Gordon MA, Vedder DK. Serologic tests in diagnosis and prognosis of cryptococcosis. JAMA. 1966;197:961–7. [PubMed] [Google Scholar]
- 17.Gordon MA. Cryptococcal antigen test. JAMA. 1981;246:1403. [PubMed] [Google Scholar]
- 18.Lu H, Zhou Y, Yin Y, Pan X, Weng X. Cryptococcal antigen test revisited: Significance for cryptococcal meningitis therapy monitoring in a tertiary Chinese hospital. J Clin Microbiol. 2005;43:2989–90. doi: 10.1128/JCM.43.6.2989-2990.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feldmesser M, Harris C, Reichberg S, Kahn S, Casadevall A. Serum cryptococcal antigen in patients with AIDS. Clin Infect Dis. 1996;23:827–30. doi: 10.1093/clinids/23.4.827. [DOI] [PubMed] [Google Scholar]


