Abstract
Background:
Human immunodeficiency virus (HIV) infection primarily affects women during their reproductive years, and the coexistence of reproductive tract infections (RTIs) is not surprising given the fact that HIV is mainly acquired via heterosexual contact.
Aim:
The aim of the study was to compare the occurrence of RTIs among infected and noninfected women.
Materials and Methods:
A case control study of 83 HIV positive women, tested by two enzyme linked immunosorbent assay (ELISA) and a matched control of 87 HIV negative women were screened for RTIs. They were submitted to gynecological examination and cervical cytology.
Results:
The mean age for HIV positive women was 30 years and that for HIV negative women was 27 years. 18% HIV positive women had menstrual irregularities compared to 6% in seronegative group (P= 0.024). Vaginal infections including sexually transmitted infections (STIs) were found in 47 (57%) HIV positive women and 30 (34%) HIV negative women (P= 0.0037). Vaginal candidiasis was the most common infection (34%) in HIV positive women, followed by trichomoniasis (12%). Human papilloma virus (HPV) infection was seen in nine HIV positive women versus none in HIV negative women. Cervical cytology showed inflammation in 53 (64%) HIV positive women compared to 27 (31%) HIV negative women (P= 0.000023). Genital neoplasia, including carcinoma in situ was observed in 2 (2.5%) HIV positive women and in none of the HIV negative women.
Conclusion:
It is seen that reproductive tract morbidities are common in HIV positive women. So it is imperative that HIV positive women have a complete gynecological evaluation including a Papanicolaou (PAP) smear with aggressive screening of STIs.
Keywords: Cervical cytology, HIV positive women, reproductive tract infections
INTRODUCTION
After 26 years since the first case of HIV was detected, the rapid increase in the number of women infected with HIV worldwide forecasts an inevitable greater number of women who will develop and die of acqiured immunodeficiency syndrome (AIDS). Currently, almost half of all new HIV infections are being reported in women, of these less than 50% are aware of their infection and 84% are in reproductive age group, i.e., 15 to 45 years.[1] RTIs/STIs most commonly affect this age group. Both ulcerative (syphilis, chancroid+herpes) and nonulcerative infections (trichomoniasis, chlamydia and gonorrhea), and other nonsexually transmitted RTIs that involve inflammation of the reproductive tract especially in women have been implicated in the spread of HIV.[2] These infection display an epidemiological synergy with HIV.
There are very few studies done in India to compare the RTIs and gynecological morbidities in HIV seropositive and HIV seronegative women. We have carried out this study to mainly highlight the importance of a detailed gynecological examination and cervical cytology in HIV positive women.
MATERIALS AND METHODS
This study was conducted between May 2002 and April 2004 in the Department of Skin and VD, Baroda Medical College. A total of 83 HIV seropositive women in the age range of 15 to 35 years (tested by 2 ELISA) were enrolled in the study. A matched control (more or less matched for age and socioeconomic status) of 87 HIV seronegative women attending the outpatient department were also enrolled. A detailed history was taken and a thorough examination for RTIs was done. Smear examination (gram staining, KOH smear, and wet mount) was also carried out. All patients were subjected to PAP smear (cervical cytology) and if suspicious, colposcopy was done by the gynecologist. The data was analyzed by using uni-square test.
RESULTS
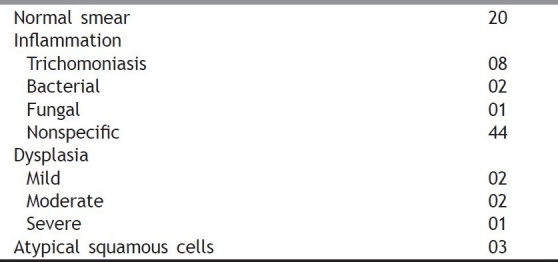
The mean age for HIV positive women was 30 years and that for HIV negative women was 27 years. The major mode of transmission in HIV positive females was sexual transmission (70%). Menstrual irregularities were higher in HIV positive women as shown in Table 1. These mainly included amenorrhoea (12%), oligomenorrhoea (6%), intermenstrual bleeding (4%), and menorrhagia (6%), in the seropositive group. STIs/RTIs as shown in Table 2 were seen in 57% of the HIV positive females compared to 35% HIV negative females. Table 3 shows in detail the STI/RTI profile in HIV positive and HIV negative females. An abnormal PAP smear was significantly higher in the seropositive group compared to the seronegative group [Table 4]. Table 5 shows the details of PAP smear in the HIV positive women. Here, abnormal PAP smear includes inflammation, atypical squamous cells, and dysplasia.
Table 1.
Menstrual irregularities
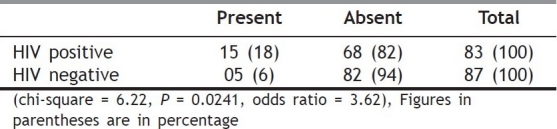
Table 2.
Sexually transmitted infections/reproductive tract infection
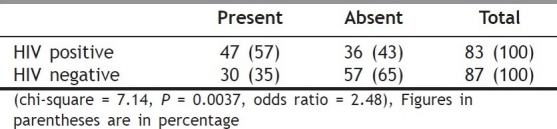
Table 3.
Reproductive tract infection/sexually transmitted infections profile
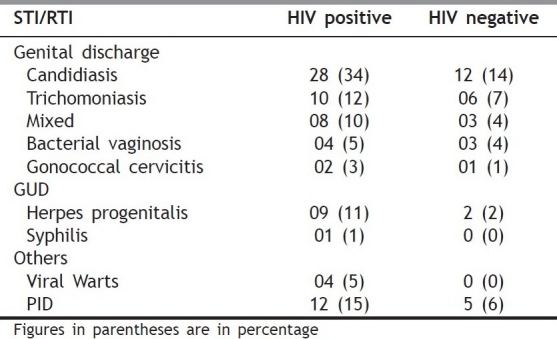
Table 4.
PAP smear
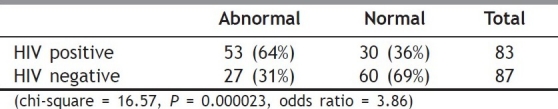
Table 5.
Detail of PAP smear
DISCUSSION
RTIs including STIs and HIV/AIDS are being increasingly recognized as a serious public health problem. RTIs are suffered by both men and women, but their consequences are far more devastating and wide spread among women. Among women, RTIs often go undiagnosed and untreated. It is the burden of asymptomatic disease that is responsible for the frequent and severe or long-term morbidity and in part for the persistence and spread of STIs in the community.
HIV infection and other STIs (both ulcerative and nonulcerative) increase the transmission of HIV by approximately three to five fold.[3,4] Vaginal candidiasis may occur earlier than other conditions and may serve as an early marker of HIV infection in women[5] in our series, as high as 34% HIV positive females had candidiasis. Herpes was seen in 11% of the HIV positive females compared to 2% in HIV negative females. HSV-2 shedding is also high in HIV infected women hence increasing the chances of transmission and acceleration of HIV disease. It may present asymptomatically in HIV positive females.[6] HSV-2 may be associated with the most extensive ulcerative disease in HIV infected women[7] as seen in our patient. Viral warts were seen in 5% of the HIV positive females compared to none in the HIV negative group. A study done by Palefsky et al., showed evidence of HPV infection in 58% of HIV positives vs. 26% of controls. They assessed HPV within cervical vaginal lavage fluids,employing polymerase chain reaction (PCR). This technique was not available in our hospital. Data from WIHS study demonstrated 40% prevalence of abnormal PAP smear in HIV infected women vs.17% in HIV negative control.[8] Inflammation was seen in 73% of the smears in our study. Studies have implicated microbes in inflammatory smears, especially Chlamydia, HSV, and trichomonas vaginalis.[9] All patients with dysplasia were subjected to colposcopy, out of which two were diagnosed with carcinoma in situ. In 1993, the United State Centers for Disease Control and Prevention (CDC) added cervical cancer to the list of AIDS defining conditions. Vulvo-vaginal candidiasis, cervical dysplasia, cervical cancer in situ, and PID were also added to the revised classification system of HIV infection under category B.[10]
Because of their inherent biological vulnerability for RTI/STI, all HIV positive females must be screened periodically for evidence of genital tract involvement, so that they can be promptly and effectively treated. Moreover, impact of silent STIs on pregnancy can also be prevented on screening. In a resource restricted set-up, HIV positive females can be helped by basic investigations including a PAP smear. There is a growing need for HIV clinicians to not only provide basic but also gender specific care to the HIV infected women as they are afflicted by the same HIV manifestation as in male in addition to female specific manifestations.
ACKNOWLEDGMENT
Department of Gynecology, Baroda Medical College, Gujarat provided their valuable help and guidance in carrying out this study.
Footnotes
Source of Support: Department of Gynecology, Baroda Medical College, Gujarat
Conflict of Interest: None declared.
REFERENCES
- 1.Women and HIV infection including mother to child transmissions-pecialists training and reference module. NACO. 2000:172–84. [Google Scholar]
- 2.Wasserheit JN, Sterling JC, Kurtz JB. 6th ed. Oxford: Blackwell Science; Viral infections. Rook/Wilkinson/Ebling Textbook of dermatology. [Google Scholar]
- 3.Tezlak EE, Chaisson MA, Bevier PJ, Stoneburner RL, Castro KG, Jaffe HW. HIV-1 seroconversion in patients with and without genital ulcer disease: A prospective study. Ann Intern Med. 1993;119:1181–6. doi: 10.7326/0003-4819-119-12-199312150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Rhoads J, Wright C, Redfield RR, Burke DS. Chronic vaginal candidiasis in women with human immunodeficiency virus infections. JAMA. 1987;257:3105–7. [PubMed] [Google Scholar]
- 5.Brown ZA, Vontver LA, Benedetti J, Critchlow CW, Hickok DE, Sells CJ, et al. Genital Herpes in pregnancy: Risk factors associated with recurrence and asymptomatic viral shedding. Am J Obstet Gynecol. 1985;153:24–30. doi: 10.1016/0002-9378(85)90584-8. [DOI] [PubMed] [Google Scholar]
- 6.Maier JA, Bergman A, Ross MG. Acquired immunodeficiency syndrome manifested by chronic primary genital herpes. Am J Obstet Gynecol. 1986;155:756–8. doi: 10.1016/s0002-9378(86)80014-x. [DOI] [PubMed] [Google Scholar]
- 7.Fruchter RG, Palefsky J, Riester KA. Abnormal cervical cytology in HIV infected women. J Acquired Immune Defic Syndr Hum Retroviral. 1997;14:A17. [Google Scholar]
- 8.Palefsky J, Minkoff H, Kailash LA. Cervico vaginal human papilloma virus infection in HIV positive and high risk HIV negative women. J Acquired Immune Defic Syndr Hum Retroviral. 1997;14 all(abstracts) [Google Scholar]
- 9.Madhivanan S, Cu-Uvin Prevalence of cervical dysplasia among women attending an HIV care centre in Chennai, South India. J Obstet Gynecol Indian. 2003;53:367–70. [Google Scholar]
- 10.Cotton DJ. AIDS in women. Textbook of AIDS medicine. In: Merigan, Barlett, Bolognesi, editors. 2nd ed. Williams and Wilkins; 1999. pp. 151–9. [Google Scholar]


