Abstract
Background:
This study analyzes the social, economic and behavioral factors most frequently associated with adherence to Highly Active Antiretroviral Treatment (HAART) in urban India.
Materials and Methods:
Data was collected in a metropolitan teaching hospital in Mumbai using a cross-sectional survey design. Face-to-face interviews were conducted with 152 patients. The semistructured survey included both open and closed ended questions on socio-demographic, economic and behavioral factors. Factors affecting treatment adherence were analyzed.
Results:
The median age of patients was 40.5 years, 73% were males and all were heterosexual. Patients had been given ART from six months to five years (median is equal to 3.5). Ninety per cent lived at home and commuted to the clinic by bus or train. Behaviorally, 37% were sexually active, but only 55% used condoms. In assessing adherence, income, education, knowledge of their drugs, transportation, side effects, cost of treatment, distance from clinic and personal clinic satisfaction were analyzed. We found that 75% of patients reported cost of HAART to be the single greatest obstacle to adherence (p less than 0.01). Additionally, those claiming knowledge of their drugs were 2.3 times more likely to be adherent (p less than 0.03), while those who abused drugs or alcohol were 53% less likely to be adherent (p less than 0.03). There was no correlation with other factors.
Conclusions:
Our study population was representative of the lower middle class of India. It found that an educated, employed group considered the cost of treatment to be a significant obstacle for successful therapy. Additionally, it showed a significant increase in adherence when patients had knowledge of their HAART medications. Therefore, reducing the cost of medication as well as teaching about antiretroviral medications are both likely to improve adherence.
Keywords: Adherence, compliance, cost, HIV/AIDS, India, treatment
INTRODUCTION
The success of HAART is extremely dependent on patients’ adherence to the treatment regimen. A recent study found that in patients exhibiting 95% or greater adherence to their treatment regimen, there was both an increase in virocidal success (total reduction in viral load) and nondetectable HIV RNA levels. In addition, these patients did not manifest opportunistic infections such as pneumonia, skin cancers and tuberculosis.[1] In order to enhance the efficacy of antiretroviral therapy, we need to address those demonstrable barriers that negatively impact patients’ ability to adhere to the protocol. In passing, it is worth noting that when referring to adherence in this study, we are invoking both the patient's own ability as well as proper conceptualization of the medical strategy to conscientiously follow the regimen prescribed; whereas compliance addresses idiosyncratic and contrary willful factors at play vis-a-vis a clinician's orders or management plans.[2]
India is a nation of over a billion people and it has some of the poorest health outcomes in the world. According to the UNAIDS report, there are 2.47 million persons in India living with HIV, equivalent to approximately 0.36 per cent of the adult population; almost 50 per cent of the previous high estimate of 5.2 million.[3] While adult HIV prevalence among the general population is 0.36 per cent, in high-risk groups, like injecting drug users (IDUs), it may be as high as 8.71 per cent, while it is 5.69 per cent and 5.38 per cent respectively among men who have sex with men (MSM) and female sex workers (FSWs).[4]
Worldwide, there is a plethora of published literature focusing on primary prevention of HIV/AIDS. On the other hand, literature concerning secondary prevention measures is only just now emerging. Several studies have examined socio demographic and behavioral factors that contribute to an individual's non-adherence to a prescribed treatment regimen. Although previous research has clearly demonstrated that behavioral factors make an impact at all stages of the infection, there is mixed evidence as to whether or not a patient's socio demographic characteristics could have an effect on the actual continuation of treatment. Some studies have established an association between demographic factors and poor patient adherence.[1,5–9] In contrast, other studies[2,10] found no relation between specific patient demographics and poor adherence. Despite these inconsistencies, most researchers agree that behavioral factors do indeed play a significant role in patients’ non-adherence to their prescribed regimen.
Intervention efforts in India are mainly and by necessity directed towards primary prevention. Given the limited medical resources available to an ordinary citizen, such efforts are very much appropriate and understandable.[11–13] Likewise, intervention research in India has primarily concentrated on primary prevention with targeted high-risk groups, including commercial sex workers, truck drivers, injection drug users and urban youth.[14–16] However, there is limited data on the role of secondary prevention measures in improving health outcomes and reducing transmission. This has been partly due to the prohibitive costs of HAART in the past. However, recent governmental efforts have resulted in substantially reducing the costs of drugs making them more available to the general HIV-infected population.[11] Although there is not enough adherence data in India, previous research has clearly established that adhering to any chronic treatment poses a potential risk of failure. India is an ethnically diverse country, and therefore, it is essential to examine all the wide-ranging and variegated factors that enhance a patient's ability and those that prevent patients from continuing and successfully completing their medical treatment.
The present study was conducted to identify and describe those social, cultural, economic and behavioral factors that might be associated with both adherence and non-adherence to HAART.
MATERIALS AND METHODS
This was a cross-sectional survey design. The study was conducted at Seth G.S. Medical College and King Edward Memorial (KEM) Hospital in Mumbai, India. KEM Hospital is a leading teaching hospital located in Mumbai, a city of roughly 12 million people. Mumbai, a major city in India, has among the highest prevalence rates for HIV/AIDS in the nation.[4] The HIV/AIDS Clinic at KEM has an annual caseload of over 2,500 patients. Most of the patients are of a lower socio economic status; however, because of the lack of trained HIV treatment specialists, patients from the surrounding smaller cities and rural areas seek services from these urban clinics.
A random sample of 152 patients, both men and women, attending the HIV Clinics in KEM Hospital were recruited to participate in the study. Patients currently on HAART, consistent with the guidelines of the U.S. Public Health Service,[17] for a minimum of six months and between the ages of 18-64, were eligible to participate in this study. Eligible patients were administered a semistructured survey instrument in a face-to-face format, after obtaining written consent. The interviews were conducted in the local languages of Hindi, Marathi and English depending on the specific comfort level of each participant.
The semistructured survey instrument had 43 items and it was comprised five sections. The first section examined the socio demographic profile of each patient. The second section was designed to assess the patient's non-adherence to their regimen. The third and fourth section respectively focused on individual behaviors and practices and knowledge and attitudes related to treatment. The final portion evaluated the level of the individual patient's access to care. Some questions were open-ended to elicit additional information on the subject. The instrument was translated into the Hindi and Marathi languages and was translated back to English to ensure reliability. Furthermore, the instrument was pilot-tested to ensure clarity of the questions.
The data was entered into an MS Access database. Data was analyzed using SAS Statistical Software 9.2. Participants’ profiles were analyzed with respect to time, person and place. Participants’ knowledge, attitude and behaviors related to drug treatment were compared among different demographic groups. Factors affecting treatment adherence were subsequently analyzed using appropriate statistical procedures.
Ethical issues
Ethical approval for the study was obtained from the University of South Florida Institutional Review Board. During the process of developing the MS Access database, unique identifiers unrelated to the name of the participating patient volunteers were created. This ensured that individual patient confidentiality was preserved to the greatest possible extent. Written informed consents were also obtained from all study participants. If a participant was unable to read then the research assistant verbalized the content of the informed consent to the patient and a verbal assent was then properly recorded.
RESULTS
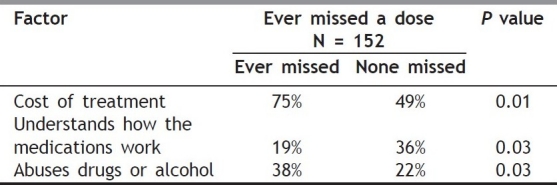
A total of 152 patients were studied; a majority of them were (131 or 90%) Hindus. The median age of patients was 40.5 years [Table 1], 111 (73%) were male and all were heterosexual. Patients had been given HAART from six months to five years (median is equal to 3.5). Ninety per cent lived at home and commuted to the clinic by bus or train. Seventy-three percent were employed, 53% had completed high school and 25% possessed some degree of college education. Behaviorally, 37% were sexually, active but only 55% used condoms. Figure 1 depicts that more than 25% of patients reported a one to six months lapse in time since their last clinic visit. Nearly 30% of respondents admitted to missing medication over a week while 18% had missed a dose in the last 24 hours, and 43% reported ever missing a dose, as noted in Table 2. In assessing adherence, the following were analyzed: income, education, knowledge of their drugs, mode of transportation, side-effects, distance from clinic, cost of treatment, concurrent drug/alcohol abuse, and clinic satisfaction. We found that 75% of patients reported cost of HAART to be the single greatest obstacle to adherence (P less than.01)[Table 3]. Additionally, those claiming knowledge about their drugs were 2.3 times more likely to be adherent (P less than.03), while those who abused drugs or alcohol, regardless of their level of knowledge, were 53% less likely to be adherent (P less than 0.03). There was no correlation with other factors analyzed in this study.
Table 1.
Demographic data of study population
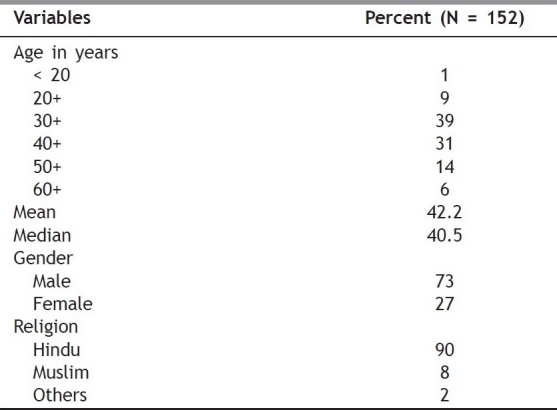
Figure 1.
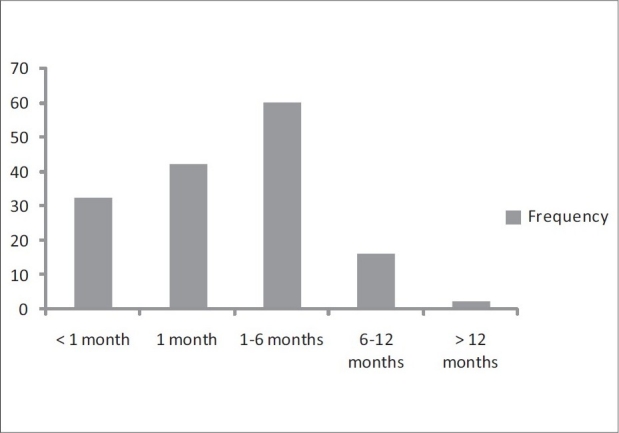
Time since last patient clinic visit
Table 2.
Adherence Markers (N=152)
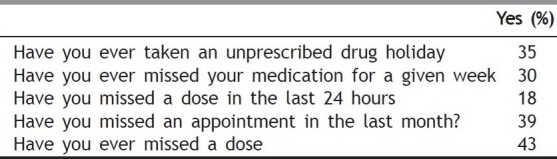
Table 3.
Factors associated with non-adherence
DISCUSSION
Nearly 75% of our study participants reported that the greatest barrier to adherence was the cost of therapy. Therefore, the findings of this study were clinically significant since they identified the major obstacle to treatment adherence in this population. However, it is worth mentioning that there may have been a few inherent confounding limitations in our study. Several sources of bias may have occurred in our analysis since only those patients who continued treatment were included and those who no longer presented for medical treatment were omitted. It is also possible that patients who had consented to actually participate in the study differed a priori in their level of adherence from those who did not consent i.e., their level of enthusiasm and respect for the study probably reflected a higher likelihood of adherence.
In addition, the logistics of data collection may have also led to bias since patients were asked to recollect and describe adherence markers from the past, which may have resulted in recall bias. Of relevance is also the fact that the small number of participants recruited may not allow generalization of the study findings to the entire HIV population in India. Nevertheless, this study will serve as a useful future replicable template and may be potentially implemented using a multisite large scale population.
A large number of research studies regarding patient nonadherence have been conducted both in the U.S. and abroad. Several variegated factors have been previously described in the literature comprising patient, provider and interpersonal factors. Unfortunately, these factors have been found to vary according to the populations sampled and the methodology employed. Previous investigators have recommended further examination of the relationship between socio behavioral and demographic factors vis-a-vis non-adherence;[4] each individual region seeming to have its own individual bioregional and social context specifically impacting the degree of non-adherence of the indigenous individual.
Identifying the barriers to maintaining individual treatment can positively enhance each patient's health outcome, thus simultaneously enhancing their relationship with the attending clinician. Our study highlights that within an educated, gainfully employed segment of the population, the cost of treatment was an insurmountable obstacle to adherence. Additionally, it showed a significant increase in adherence when education on HAART was diligently employed.
Based on the current findings, future cost effective interventions can be designed to enhance treatment efficacy. Additionally, it can be safely asserted that those patients from a lower socio-economic status could be promptly referred to governmental agencies or community based non-governmental service organizations, in order to enhance or promote an individual's fund of knowledge about the drugs’ actions and therefore lessening the potentially negative impact of a rigid sectarian belief system. Enhanced adherence and treatment efficacy will in turn lead to quantifiable improved health outcomes, decreased prevalence of drug resistance and an ameliorated risk of transmission of the virus by infected individuals to the uninfected community at large. Therefore, by buttressing the medical management of the already afflicted, the resultant outcome would ultimately also be instrumental in community-wide primary prevention efforts.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 2.Williams AG. Adherence, Compliance, and HAART. AIDS Clinical Care. 1997;9:51–5. [PubMed] [Google Scholar]
- 3.UNGASS Country Progress Report 2008 India. ational AIDS Control Organization, New Delhi, India. [retrieved on 2009 Jun 30]. Available from: http://data.unaids.org/pub/Report/2008/india_2008_country_progress_report_en.pdf .
- 4.NACO Surveillance Report. 2006. [retrieved on 2009 Jun 30]. Available from: http://www.nacoonline.org/Quick_Links/HIV_Data/
- 5.Lieb S, Brooks RG, Hopkins RS, Thompson D, Crockett LK, Liberti T, et al. Predicting death from HIV/AIDS: A case-control study from Florida public HIV/AIDS clinics. J Acquir Immune Defic Syndr. 2002;30:351–8. doi: 10.1097/00126334-200207010-00012. [DOI] [PubMed] [Google Scholar]
- 6.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28:47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Bartlett JA. Addressing the challenges of adherence. J Acquir Immune Defic Syndr. 2002;29:S2–10. doi: 10.1097/00126334-200202011-00002. [DOI] [PubMed] [Google Scholar]
- 8.Gordillo V, del Amo J, Soriano V, González-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13:1763–9. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- 9.Gray L, Edmondson E, Lemke AL. University of Washington, School of Social Work; HIV/AIDS Project Development and Evaluation Unit. HIV treatment adherence: A guide for program development. 1998 Oct 31; [Google Scholar]
- 10.Webster RD, Barr D JD. Forum for Collaborative HIV Research. Washington, D.C: Center for Health Policy Research, George Washington University Medical Center; 1999. Adherence to Highly Active Antiretroviral Therapy (HAART) among individuals with HIV/AIDS: A compendium of HAART adherence research, November 1997 - November 1999; pp. 1–24. [Google Scholar]
- 11.Southik B. Indian drugs boss hails Aids deal. 2003. Oct 29, [retrieved on 2004 Feb 11]. Available from: BBC News Online http://news.bbc.co.uk/2/hi/south_asia/3220619.stm .
- 12.WHO. The 3 by 5 initiative. 2003. [retrieved 2004 Feb 11]. Available from: http://www.who.int/3by5/en/
- 13.Deshmukh JS, Wadhva SK, Zodpey SP. AIDS: Knowledge and attitudes of university students in Nagpur. Indian J Med Sci. 1998;52:302–8. [PubMed] [Google Scholar]
- 14.Bentley ME, Spratt K, Shepherd ME, Gangakhedkar RR, Thilikavathi S, Bollinger RC, et al. HIV testing and counseling among men attending sexually transmitted disease clinics in Pune, India: Changes in condom use and sexual behavior over time. AIDS. 1998;12:1869–77. doi: 10.1097/00002030-199814000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Joshi S, Joglekar N, Ghate M, Unni J, Risbud A, Bentley M, et al. Phase I safety & preliminary acceptability of nonoxynol-9 vaginal pessary as a vaginal microbicide in low risk women in Pune, India. Indian J Med Res. 2003;117:152–7. [PubMed] [Google Scholar]
- 16.Sahasrabuddhe VV, Gholap TA, Jethava YS, Joglekar NS, Brahme RG, Gaikwad BA, et al. Patient-led partner referral in a district hospital based STD clinic. J Postgrad Med. 2002;48:105–8. [PubMed] [Google Scholar]
- 17.U.S. Public Health Service. [Accessed on 2009 Apr 4]; Available from: http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf . [Google Scholar]


