Abstract
Human immunodeficiency virus (HIV) testing with pre and postcounseling aiming behavior change communication (BCC) for core/bridge population is the main element of holistic model of health care. Voluntary counseling and testing center (VCTC) remodeled as integrated counseling and testing center (ICTC)—general is the ‘gateways to care’. It was hospital-based cross sectional study of 811 clients registered at VCTC of Kesar SAL Hospital from January to December 2007. These patients either came voluntarily or by referral. Anonymous and unlinked information was collected on predesigned schedule and data was analyzed to find out the seropositivity, demographic characteristics (among attendees and HIV positives), and epidemiological vulnerability of different segments of population. Among the attendees, 64% were males, 75% in the age group of 20–49 years, 80% were currently married, and 70% were literate (< 10th standard). Also, 66% clients were gainfully employed, while one-fourth were housewives; 98% lived with families, 75% were referred by doctors, and only 19% walked in directly. Dominant reason for visiting ICTC was the history/presence of high risk behavior (HRB) (34%). 35% indulged in heterosexual route; other HRB (men having sex with men or MSM and injecting drug users or IDU) were rare. There were more positive among males, 20–49 years of age group, those living singly, unmarried, divorcee, widow(er) and separated. Similarly positives were more amongst illiterates, less educated and those engaged in unskilled and semi skilled jobs. Adolescent students (>14 years) accounted for one-fifth of the total positives. Direct walk in clients were more positive compared to those referred by doctors. Those who confessed of history/presence of HRB accounted for all except 3 (85%) positives. 51% indulged in heterosexual sex followed by MSM (8%). Overall sero positivity was 4.8%; high in males, 30–49 years age, unmarried and divorcee etc. Sero prevalence decreased with improvement in education and also with improvement in job nature. It was also high in those living alone compared to those staying with their family.
Such study shall in evaluating the performance of ICTC and designing the information, education, and communication (IEC) to increase the client uptake in terms of quality and quantity.
Keywords: Integrated counseling testing center, voluntary counseling and testing attendees, HIV sero positivity, socio-demographic variables
INTRODUCTION
All countries in the South East Asia are deeply concerned regarding the HIV epidemic and responding their best.[1] Some organizations such as, UNAIDS, WHO, and NACO estimate national adult prevalence in India as 0.36% amounting to 2.7 million (2.0–3.1 million) HIV positive people;[2] which accounts for 10% and 65% of the HIV burden of the world and South East Asia, respectively.[3] As per the current estimates for Gujarat, approximately 144,000 people are living with HIV/AIDS (PLHA) putting the state in moderate prevalence category. As per the Sentinel Surveillance of 2006,[4] A category has six districts, whereas B has four districts (including Ahmedabad in B category).
Voluntary counseling and testing (VCT) for HIV is a cost-effective intervention in preventing the spread of HIV transmission and is an integral part of HIV prevention program, which provides an opportunity to learn and accept the HIV status in a comfortable, convenient, and confidential manner.[5] Integrated counseling testing center (ICTC) network is the first interface between a person willing to get tested and the public health system.[6] Further, it is an entry point to care. In the NACP phase III, HIV testing facilities have been segregated in A and B categories by district and are now available at all medical colleges, district hospitals, and subdistrict hospitals (Community Health Centers). At subdistrict level, earlier VCTCs and facilities providing prevention of Parent to Child Transmission of HIV and AIDS (PPTCT) services are now remodeled as a hub to deliver integrated services to all clients.[7] Presence of infection everywhere highlights spread from urban to rural areas; from high risk to general population via bridge population, and from permissive to conservative societies.[8] Migration of labor, low literacy levels, gender disparities, and prevalent RTI/STI have contributed to this spread.[9] The data generated in VCTC provides an important clue to understand the epidemiology of the disease in a particular region.[10]
Ahmedabad is the seventh largest city of India with its population crossing five million is kept in category B, but still it is at a high risk due to presence of 1 million migrants, 2 lakhs commuting population, 4,000 commercial sex workers (CSWs), 3,000 men having sex with men (MSM), and more than 40 industrial estates.[6] Present study has been undertaken to find out the profile of those who come to avail the VCT services and also to know the profile of those found positives. An additional objective is to find out sero positivity in subsamples of the attendee in terms of various socio-demographic and epidemiological characteristics. This information will be useful in planning the local interventions for preparing the local action plan and implementing the information, education, and communication (IEC) and behavior change communication (BCC).
MATERIALS AND METHODS
The present study was conducted among the VCT attendees at the ICTC of Kesar SAL Hospital, Ahmedabad. This center was established in December 2006. Although, being in a medical college, it runs two centers independently, for VCT and PPTCT referred as ICTC (general) and ICTC (PPTCT) respectively. The study included 811 VCT attendees for a period of one year (Jan–Dec 2007), who came either voluntarily or referred by various department of this institute. Anonymous and unlinked information was collected (as per NACO guidelines) on predesigned schedule by the counselor who interviewed the attendees under strict confidentiality. After the pretest counseling and obtaining the consent from the attendees, blood samples were collected. As per the policy prescribed by NACO, HIV was confirmed by performing enzyme-linked immunosorbent assay (ELISA), by using two different antigens and a rapid test. The prior approval was taken from the appropriate authorities from the institute. Data was complied and analyzed in EPI INFO package.
RESULTS
Attendees’ profile: Out of 811 attendees, 519 (64%) were males and rest (36%) were females. Age group of 20–49 years accounted for 74.6% of the total attendees. One-fifth (20%) of the clients were illiterate; 80.4% were married; and 97.7% were living with families [Table 1]. Also, 74.6% were referred by doctors, and only 19.4% walked in directly; referrals from TIs were even poorer (only 6%). The most common reason for visiting ICTC was history or presence of HRB (34%), while in more than half of them (59%), no reason could be ascertained [Table 2]. Type of risk behavior accepted in 35.3% of attendees was heterosexual route (47% in males and 9.5% in females), followed by history of blood transfusion (6.5%). Other modes such as MSM and IDU needle sharing were very rare.
Table 1.
Percent profile of voluntary counseling and testing attendee and those found positive based on some demographic characteristics (n=811)
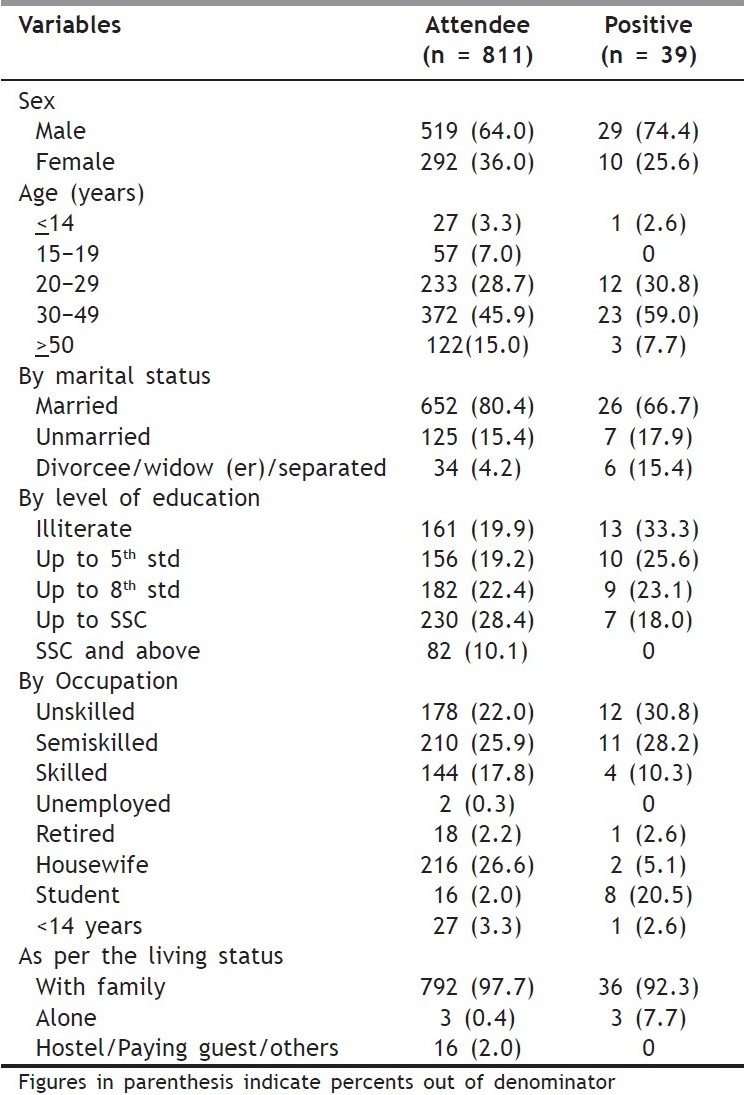
Table 2.
Percent profile of voluntary counseling and testing attendee and those found positive based on epidemiological characteristics (n = 811)
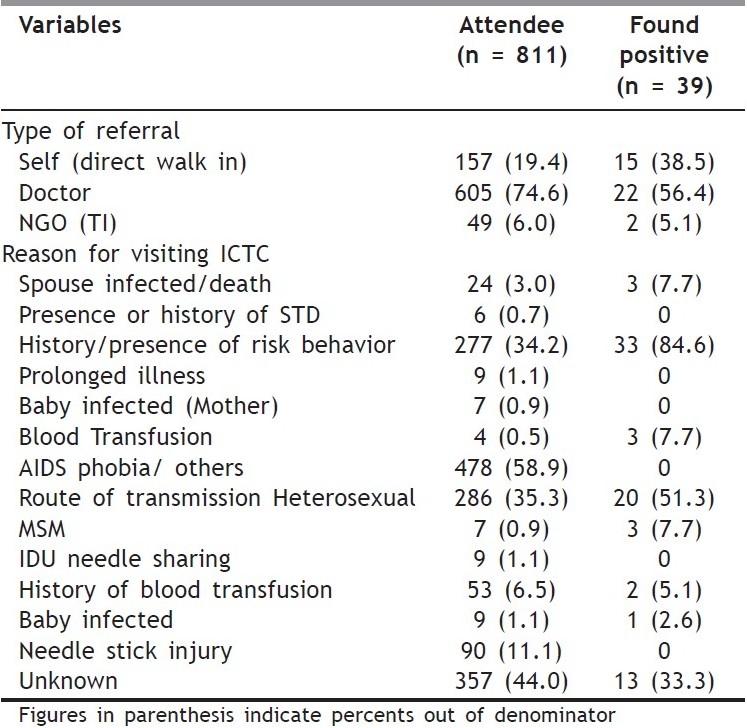
Profile of positives: Out of 39 cases found HIV positives, 74% were males, 90% were adults (20-49 years), all of them (100%) were illiterate or less educated (< 10th standard), 92.3% were living with family, and 66% were currently married. Also, 59% were engaged in unskilled or semiskilled jobs. Adolescents and students accounted for another 20.5% of positives. Therefore, profile of one found positive in present study is of married, male, aged 30–49 years, staying with his family who is either illiterate or educated only up to primary and engaged in unskilled or semiskilled job. Only 38.5% of positives walked in directly, while rests were either referred by doctors (56.4%) or by NGOs (5.1%). The most common reason for visiting ICTC was the history/presence of high risk behavior (84.6%), followed by blood transfusion (7.7%). The most common route of transmission which could be identified among positives was heterosexual route (51.3%), followed by MSM activities and blood transfusion.
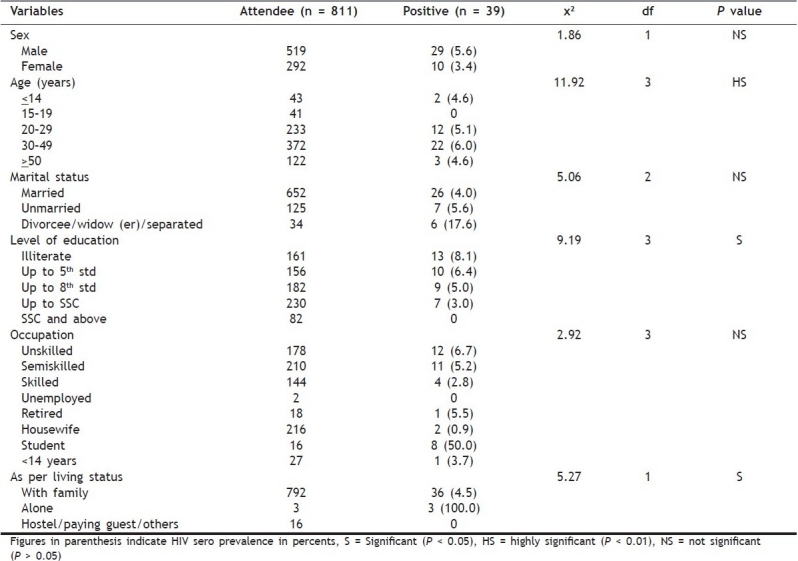
Sero prevalence: Out of 811 tested attendees, all (100%) underwent pretest counseling and 93% of them underwent posttest counseling and 39 of them were found HIV positive, with an overall sero positivity of 4.8%. Separately, it was high among males (5.6%) than females (3.4%), but the difference was not significant [Table 3]. The prevalence was significantly high in 30–49 years age group. The group of divorcee, widow, separated, etc. was very small (34) but reported a high prevalence (17.6%); however, the difference was not significant. Education and occupation showed an inverse relationship, whereby the HIV prevalence decreased with improvement in education and job nature. Here the differences were significant in case of education but were not significant in occupation. A small group of students aged >14 years[16] showed a very high prevalence of 50%. Significantly low prevalence was seen in the people who stay with their families compared to those who live single or stay at hostel or as paying guest. Here, three people staying all alone were tested and all of them (100%) were found positive [Table 3].
Table 3.
HIV sero positivity (%) of VCTC attendees based on demographic variables (n = 811)
DISCUSSION
VCT services cater to those who come to the center either from referral (care providers) or direct walk in clients; some times it can be referral from the targeted interventions by NGOs running in the area. So the profile of attendees depends upon the characteristics of the catchment areas and the population residing therein. Many people do not know that they are/may be HIV positive and the challenge is to make these people aware to come forward for the testing and adopt a healthy lifestyle, thereafter for the access to care and treatment and help in preventing further transmission. Counselling and testing are important for prevention and control of HIV/AIDS; however, it is neither desirable nor feasible to counsel and test everyone in the general population. The subpopulations which are vulnerable or practice high risk behavior (HRB) or have high HIV prevalence shall be the target group for these services. While in 2006, more than 2.1 million clients were counselled and tested throughout the country, the target is to counsel and test 22 million clients annually by the year 2012.[5]
The ICTC general or VCTC is an ideal point for prevention, where HIV negative individuals learn to use full array of existing services and interventions to adopt and maintain risk reduction behaviors, and HIV positive individuals use quality prevention services to adopt and sustain lifelong protective behaviors and avoid the virus transmission.[11]
Males (64%) accessed the services more than females in this study which is in accordance to the national figures and indicates the existence of some barriers preventing the access of females even now. Everyone, whether male or female, who was counseled underwent the testing; which indicates the effectiveness of counseling. While the ratio of those who came and collected test reports and received posttest counseling was better for males (93%) than females (83%). The HIV prevalence in the present study (4.8%) was less than the overall prevalence for Gujarat (7.3%),[12] and than in the studies from South Kannada (9.6%),[13] and West Bengal (17.1%).[10] Lower prevalence reported here may be due to the fact that this center mainly caters to the rural population where even now the prevalence is supposedly less. Sero positivity among VCT clients in Gujarat in 2006–07 was, as low as, 2.7% in Dang, a dominating tribal and rural district.[12] Sero prevalence was significantly high in males in this study, but HIV/AIDS in India is undergoing a feminization because females are increasingly getting infected, which is indicated by the increasing HIV prevalence in females. HIV prevalence among women, both for HRB group or married monogamous relationship, is on the rise.[14] An alarming fact was observed in this study that the prevalence is catching up in 20–]29 years of age group, though it is still highest in 30–49 years age indicating that AIDS still threatens the most productive segment of society in the prime of their working life. It emphasizes the need of some youth specific interventions or some school or college-based interventions whereby these people can be prepared beforehand. Education and job status showed the inverse relationship with the prevalence. In fact none of the positive was educated beyond 12th standard. It seems that overall development (reflected by better education and job opportunities) will provide some protection. As such the people who are educated or placed in better jobs (mostly go together) are more receptive to IEC and amenable to interventions. India's vulnerability to the AIDS epidemic can be attributed to pervasive poverty, huge illiteracy, less awareness, promiscuous behavior, and adverse attitude towards condom use.[15]
Since sex education is not included in school curriculum, so anyone who is illiterate or educated up to secondary level will not have adequate knowledge for protecting himself/herself from HIV/AIDS. A substantial number of HIV positives were contributed by males, married, and living with their families. These people, if not informed, will soon be infecting their spouses and enhancing the risk of parents to child transmission resulting in more and more “AIDS orphans”.
Almost 60% positives accepted route of transmission as sexual with another 33% unwilling to identify. At national level, 89% cases occurred among sexually active persons (20–49 years age group). The present study had 65.5% sero positives in 15–40 years of age group (27.5% in 15–19 and 37.9% in 30–39 years age group), which is higher than Lekhaet al.[16] One fifth of male sero positive in present study were illiterate so not being educated and promiscuous by habit they pick up HIV infection. In the male-dominated culture of India, women are vulnerable to HIV infection. Infection rates among women /newborns are rising mainly due to women's inability to negotiate for safe sex and their pushing into the early marriage.
Referral from TI was poor in this study because of the fact that no TI is operating in the nearby areas. Yield of positives amongst those who walked in directly was high than those who were referred by doctors. Arrival of such clients at ICTC depends upon the IEC activities in the catchment areas done by general system or by the staff at ICTC itself. In order to increase this number, the ICTC and especially its counselor should increase the IEC in a planned manner.
Present study found 69.0% male sero positives with risk behavior associated with heterosexual route followed by man having sex with man (10%) lower than the figures reported for entire state.[12,17] Best antidote to the HIV/AIDS challenge remains increased awareness and adaptation of safe behavioral practices and the solution lies in planning and designing the IEC activities keeping in mind the specific situations of the area.
Limitations: Current study is subjected to certain limitations since it was conducted in an institute with a predesigned schedule, therefore, results are based on the reporting and data collection by the personnel employed in the VCTC. Information regarding socioeconomic status, substance abuse, counseling performed and condom use are not available. All these variables could have unmasked certain behavior pattern and given new dimension to this study. This study setting being a hospital decreased its external validity. Results observed are subjected to bias arising from rate of reporting in the counseling and testing centre. A community based study though resource intensive would have been better to avoid such bias.
RECOMMENDATIONS
Prevention of HIV infection should theoretically be easier than prevention of water and air borne pathogens. HIV/AIDS is spread as much by human behavior and ignorance as by the virus. The wider clinical setting itself can provide enabling environment and reduce the stigma and discrimination. The empowerment of attendees and empathic attitude of staff at center is crucial, as clinical staff can set an example by exhibiting stigma free attitudes.
Timely and relevant use of data to guide decision making (though challenging) is critical. Program needs to invest resources not just to gather data, but also to create and stimulate a culture that emphasizes appropriate data analysis and use at all levels.
Improvement of IEC and HIV/AIDS awareness is one of the most effective strategies to control HIV/AIDS. A successful communication program helps to promote behavioral change, in addition to increasing knowledge regarding the disease. Such programs will be more effective if conducted in local languages and using the locally derived data. At the same time, they must keep in mind the following: social norms, cultural beliefs, and sensitivities of the community. Such intensive IEC will improve the uptake of VCT services by the target population.
ACKNOWLEDGEMENT
Author is grateful to the Project Director AMC ACS for granting the permission to facilitate this study.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.AIDS Watch. News from South –East Asia Region on STD. AIDS and Tuberculosis. 2000;5:6. [Google Scholar]
- 2.NACO News, behind the numbers. Newsletter of National AIDS Control Organization, Ministry of Health and Family Welfare (GOI) 2007;3:4. [Google Scholar]
- 3.HHS/CDC Global AIDS program (GAP) in India. The GAP India Fact sheet. Available from: http://www.Cdc.gov/nchstp/od/gap/counties/India.htm .
- 4.Integrated Rural HIV/AIDS programme (IRHAP) Building Capacity of Villages against HIV/AIDS, GUJARAT AIDS CONTROL SOCIETY. Health and family Welfare Department, Gujarat. 0-1, New Mental Hospital Compound, Meghaninagar, Ahmedabad. 16:2. [Google Scholar]
- 5.Ministry of Health and Family Welfare, (GOI) New Delhi: Voluntary Counseling and Testing; National AIDS Control Organization; pp. 01–08. [Google Scholar]
- 6.Pratisad, Come forwards and take leads stop AIDS. 2008;2 [Google Scholar]
- 7. Available from: http://www.naco.org .
- 8.Joshi PL. Vol. 27. New Delhi: Ranbaxy Science Foundation; HIV/AIDS in India.Round Table Conference Series: 6 April 2000. [Google Scholar]
- 9.Ahmed Muzaffar, Basir Gaash. Awareness Of HIV/AIDS in a remotely located conservative district of Jand K (KARGIL): Results of a community based study. Indian Journal of Community Medicine. 2002;28:12. [Google Scholar]
- 10.Joardar GK, Sarkar A, Chatterjee C, Bhattacharya RN, Banerjee P. Profile of attendees in the voluntary counseling and testing centre of North Bengal Medical College in Darjeeling District of West Bengal. Indian Journal of Community Medicine. 2006;31:241. [Google Scholar]
- 11.Report of National Round Table Discussion And Seminar New Delhi, 2004. Organized by Oxfam GB in Collaboration with Sexual Health Resource Centre. Vol. 20. Qutab Institutional Area, New Delhi 110 016, India: Oxfam(India) Trust, C 28-29; Maximizing Access, Care Propelling Prevention in HIV/AIDS. [Google Scholar]
- 12.Strategic Information and management Unit, Gujarat State AIDS Control Society. Meghaninagar, Ahmedabad 16: 2008. Jan-Mar. Quarterly CMIS Bulletin Gujarat. [Google Scholar]
- 13.Kumar A, Kumar P, Gupta M, Kamath A, Maheswari A, Singh S. Profile of Client Tested HIV Positive in a Voluntary Counseling and Testing Center of District Hospital, Udupi, South Kannada. Indian Journal of Community Medicine. 2008;33:156. doi: 10.4103/0970-0218.42051. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Mehendale Sanjay. HIV infection amongst persons with high risk behavior in Pune City: Update on findings from prospective Cohort study. AIDS Research and Review. 1998;1:2. [Google Scholar]
- 15.Kadri SM. Determinants of HIV/AIDS in India. Indian Journal for Practicing Doctors. 2008;5:73. [Google Scholar]
- 16.Tuli Lekha, Mohapatra TM, Gulati AK. Socio -economic relevance of opportunistic infections in HIV patients in and around Varanasi. Indian Journal of Preventive and Social Medicine. 2008;39:33. [Google Scholar]
- 17.Annual report 2006-2007. Strategic Information and Management unit. Gujarat State AIDS Control Society. 2007;15 [Google Scholar]


