Abstract
Genital infection by human papillomavirus (HPV), a sexually transmitted disease (STD), has increased considerably due to the changes in sexual behaviour and an increase in the practice of oral sex. HPV, in a parallel manner, has been closely studied due to its oncogenic potential. We present the case of a 27-year-old patient, with a multi-partner sexual history and frequent practice of oral sex, who suffered from warts lesions on the genitalia and tongue. Squamous papilloma was diagnosed from a tongue biopsy. The treatment of the oral lesion was by way of surgery, without relapse in the first two years. Our discussion in this report is regarding the HPV infection in the oral cavity.
Keywords: Human papillomavirus, oral cavity, papilloma, sexually transmitted disease, sexual behaviour
INTRODUCTION
Human papillomavirus (HPV) is a DNA virus that belongs to the papilomaviridae family, frequently sexually transmitted, causing infections which have an incubation period varying from three weeks to an indeterminate length of time and are prevalent in women.[1,2]
The most common infected areas are: the vulva, perineum, urethral meatus, and cervix. However, with a rise in oral sexual practice, HPV is frequently found in the oral mucosa.[2] Currently, there are more than 100 types of HPV. Out of these, 24 are associated to oral lesions with different oncogenic potential. Among the lesions that may be found in the oral cavity, the oral squamous papilloma is the most frequent.
This study reports a case of concurrent HPV infection in the oral cavity and genital area of a monitored patient at the STD-Gynaecology department, Santa Casa de Misericórdia hospital, Vitória, discussing clinical manifestations and the treatment of oral infection.
CASE REPORT
A 27-year-old female was seen at the STD/gynaecology outpatient department of the Santa Casa de Misericórdia hospital in Vitória. She complained of a tumor on the anterior part of the tongue, associated to a similar growing lesion on the vulva, which was almost a year old and was not previously treated. There were no other symptoms. She related her first sexual relation at 21 years of age, multiplicity of partners with two in the past year, and frequent practice of oral sex. She had given birth twice (one transpelvic and one caesarean).
Upon examination, a pink coloured, rough surfaced exophytic lesion was revealed at the tip of the tongue, measuring approximately 1 cm [Figure 1]. There was a small, 2 cm condylomatic lesion on the vulva [Figure 2]. The colpocitology was collected and it appeared normal, and a cervical colposcopic examination did not reveal lesions.
Figure 1.

Papillomatosis lesion on the tip of the tongue
Figure 2.

Codylomatic lesion on the vulva
A biopsy of the oral lesion was carried out and examinations for other sexually transmitted diseases (STDs) were requested (HIV, syphilis, and hepatitis B and C).
The tests for other diseases were negative. Histopathology of the oral lesion evidenced an epithelium irregularly thickened by acanthosis and papillomatosis, with a concentration of parakeratosis [Figure 3]; with identification of koilocytes, with perinuclear cytoplasmatic halos and irregular hyperchromatic nuclei, some binuclear, compatible with viral tongue papilloma (HPV) [Figure 4].
Figure 3.
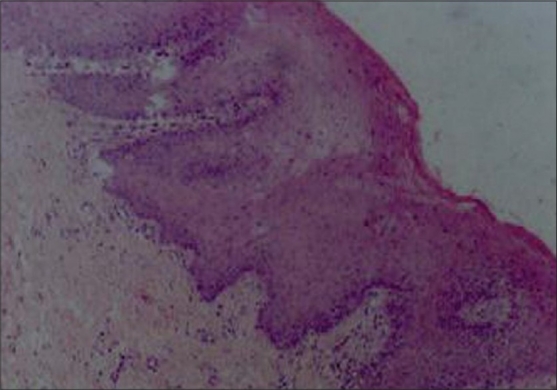
Biopsy of tongue lesion. Epithelium irregularly thickened by acanthosis and papillomatosis with area of parakeratosis (H&E, 100×)
Figure 4.
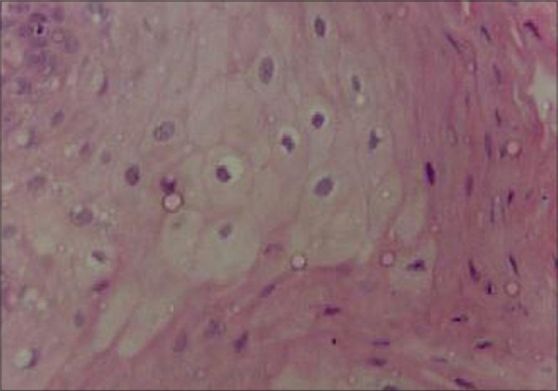
koilocytes, with perinuclear cytoplasmic halos and irregular and hyperchromatic nuclei (H&E, 400×)
Treatment of the tongue papilloma was conducted through surgical excision, and the one at the genitalia was treated through application of trichloroacetic acid at 90%. The patient was assessed by an otolaryngologist who found no evidence of lesions on the oropharynx. After excision, a tongue scraping was taken for study by polymerase chain reaction (PCR), the result of which was negative.
The patient was monitored for two years after treatment and no recurrence was observed, and thus released from treatment and appropriately guided regarding preventive methods for STDs.
DISCUSSION
Currently, with people beginning sexual activity earlier in life, and a higher number of sexual partners–factors which place individuals in a vulnerable position in relation to STDs, associated to other factors such as smoking, the immunological state, and other STDs–the incidence of HPV infection is increasing significantly.[1,3]
The possibility of oral exposure to HPV is through oral sex as well as throught intimate contact. The oral squamous papilloma represents tongue as the most prone area (which was observed in this report), responsible for approximately 55% of cases, and can also attack the palate, buccal mucous, gums, lips, tonsils, uvula, and roof of the mouth.[4]
Owing to the recognized oncogenic characteristic of HPV, most notably the causal factor of cervical cancer, many studies have been conducted. Nevertheless, the relation between these viruses and the pathogenic cancer in the oral mucous, is still controversial and; there appears to be more synergy of HPV with other chemical and physical carcinogenics such as tobacco and alcohol. A recent preliminary study evidenced 75% of suggestive findings of HPV in oral squamous cell carcinoma biopsies of the oral cavity.[3–5] However, the importance of multifactor aspects of mouth cancer and also the possibility of influence of the Epstein Barr virus should be highlighted.[3]
HPV has also been identified in other oral pathologies such as leukoplakias, vulgar pemphigus and lichen planus. On the other side, HPV infection in the oral cavity could be manifest in the other classic clinical ways such as: verruca vulgaris (HPV types 2, 4 and 20), and focal epithelial hyperplasia (HPV types 13 and 32). Oral squamous papilloma, as diagnosed in this report, is constituted of a benign tumor, which presented with an exophytic lesion of rough surface, pink or whitened colouration, sessile or pedicled.[4]
Clinically, HPV can manifest itself in three ways: transitory infection (sub clinical) in approximately 50% of cases; lesions which can spontaneously regress in 30% of cases; or persistent infections which even after treatment do not present viral elimination. HPV infection can be clinical or subclinical, that is to say, not detected by visual inspection but through magnification techniques such as colposcopy, reagents such as acetic acid, cytologies, biopsies, immunohistochemistry, and molecular biology techniques.[1,2]
Oral lesion diagnosis is basically clinical, followed by cytology, and confirmed by biopsy. A high sensitivity method of virus identification such as, polymerase chain reaction (PCR) was performed; however, nondetection of HPV DNA does not obviate the possibility of infection, since a small number of copies may be undetected, as occurred in this present study.[3,4]
Treatment should be individualized according to the number, size and location of lesions, patient wishes, cost and available resources. Surgical excision is the most recommended for few lesions, particularly when a biopsy is desired.[1–4] Clinical treatment is administered using keratolytic agents with cell destruction such as trichloroacetic acid 40–90%, frequently used, among others such as podophyline 25%, 5-flouracil and imiquimod. Surgical treatment is by surgical, electric, or laser excision. Cryotherapy and electrocauterisation are also good alternatives.
Accompaniment of the patient should be for 3–6 months after the lesions disappear, as the first three months is the higher-risk period of reoccurrence[1,2] The patient should be informed that the virus may remain in the body whether or not infection is cured.
Due to the oncogenic potential of the HPV, preventive methods must be reinforced to the patients. Vaccination against HPV is a currently available resource which has produced positive results in evaluated patients according to the recent studies.[6]
Oral cavity lesions have important meaning to health care providers dealing with STDs. A thorough examination of the mouth must be performed in all patients that present genital HPV infection.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Manual de Controle das Doenças Sexualmente Transmissíveis. 3 ed. Brasília: 1999. Ministério da Saúde. Secretaria de Projetos Especiais de Saúde. Coordenação de Doenças Sexualmente Transmissíveis e AIDS; pp. 95–100. [Google Scholar]
- 2.Passos MRL. Niterói: RQV; 2004. Deessetologia no bolso: o que deve saber um profissional que atende DST; pp. 70–5. [Google Scholar]
- 3.Castro TMPG, Neto CER, Scala KA, Scala WA. Manifestações orais associadas ao papilomavírus humano (hpv) conceitos atuais: revisão bibliográfica. Rev Bras Otorrinolaringol. 2004 Jul-Ago;:70–4. [Google Scholar]
- 4.Castro TMPP, Duarte ML. Condiloma lingual: relato de caso clínico. Rev Bras Otorrinolaringol. 2004;70:565–8. [Google Scholar]
- 5.Xavier SD, Filho IB, Lancellotti CLP. Prevalência de achados sugestivos de papilomavírus humano (HPV) em biópsias de carcinoma espinocelular de cavidade oral e orofaringe: estudo preliminar. Rev Bras Otorrinolaringol. 2005 Jul-Ago;:v.71–n.4. [Google Scholar]
- 6.Mao C, Koutsky LA, Ault KA, Wheeler CM, Brown DR, Wiley DJ, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia: a randomized controlled trial. Obstet Gynecol. 2006;107(3):18–27. doi: 10.1097/01.AOG.0000192397.41191.fb. [DOI] [PubMed] [Google Scholar]


