Sir,
Opportunistic parasitic infections are the sole hallmark of HIV infection and is encountered in 90% of AIDS patients in the developing countries.[1–3] Cryptosporidium, Isospora, Cyclospora, and Microsporidia are increasingly being recognized as important enteric pathogens in the HIV positive patients.[1–3]
A study was conducted to find out the prevalence of various enteric parasites in stool samples of HIV positive patients with and without diarrhea (100 and 40 respectively) and 10 samples from normal healthy controls. All samples were collected in clean, dry, widemouth, leakproof container and transported within two hours to the laboratory. Macroscopic and microscopic examinations of the stool samples were done. Modified Z-N staining (Hot method)[4] was done using 10% H2SO4 and smears were screened under oil immersion to identify oocysts of Cryptosporidium, Isospora, and Cyclospora. Chromotrope 2R staining[5] was done for all the samples using fast green, and smears were examined under oil immersion lens for pink coloured spores of microsporidia against green background.
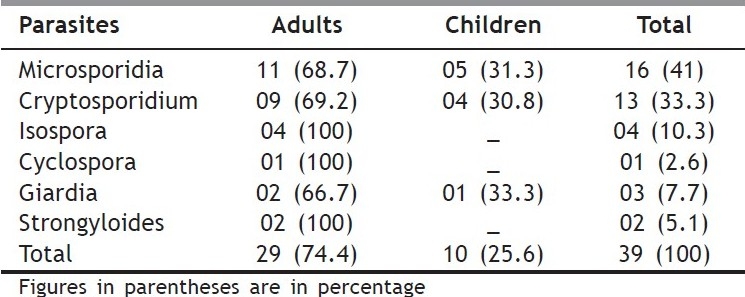
Among 100 HIV positive patients with diarrhea, there were 60% adults and 40% children. Majority of the patients (73.3%) were in the age group of 21-40 years. Out of 16 microsporidia reported [Table 1], liquid stool was seen in 37.5% cases, whereas abdominal pain was present in all 16 patients (100%). Out of 13 Cryptosporidium species reported, liquid stool was seen in 69.2% cases, 84.6% patients had 6-10 motions per day, and abdominal pain in 46.2% cases. Mixed parasitic infections were encountered in four patients, in two of which microsporidia and Cryptosporidium were detected together.
Table 1.
Parasites isolated from stool samples by wet mount, Z-N staining and Chromotrope 2R staining in HIV positive patients with diarrhea
Among the 40 HIV positive patients without diarrhea, in one oocysts of Cryptosporidium sp., in one cysts of Giardia lamblia, and in one ova of Ascaris lumbricoides were detected. No parasite was detected in any of the ten healthy controls.
Prevalence of enteric parasites in this study was 39%. This study was exactly similar to the study by Kumar et al.[1] Prevalence of microsporidia in HIV positive patients with diarrhea have been reported to be in the range of 1-29% by various authors.[2,3] Therefore, this study has a high prevalence of microsporidia (41%) and all these patients presented with abdominal pain. Other studies have reported mixed infections with enteric parasites,[2,3] as also reported by us.
One Cryptosporidium was detected in a HIV positive patient without diarrhea. Mohandas et al,[2] have reported cryptosporidium in 10.8% HIV infected patients, out of which 7.7% patients did not have diarrhea. No microsporidia was detected in this group which is statistically significant (P < 0.05) compared to HIV positive patients with diarrhea.
Therefore, opportunistic intestinal parasites are a common cause of diarrhea in HIV infected patients, and diarrhea due to microsporidia is on the rise, as evident in this study. Chromotrope 2R staining still remains the most commonly used method for detection of microsporidial spores. Therefore, apart from modified Z-N staining for detecting oocysts of Cryptosporidium, Isospora and Cyclospora, chromotrope 2R staining should also be done in routine laboratories for detection of microsporidial spores.
REFERENCES
- 1.Kumar SS, Anathan S, Lakshmi P. Intestinal parasitic infection in HIV infected patients with diarrhea in Chennai. Indian J Med Microbiol. 2002;20:88–91. [PubMed] [Google Scholar]
- 2.Mohandas K, Sehgal R, Sud A, Malla N. Prevalence of intestinal parasitic pathogens in HIV seropositive individuals in Northern India. Jpn J Infect Dis. 2002;55:83–4. [PubMed] [Google Scholar]
- 3.Cegielski JP, Ortega YR, Mekee S, Madden JF, Gaido L, Schwartz DA, et al. Cryptosporidium, Enterocytozoon and Cyclospora infections in pediatric and adult patients with diarrhea in Tanzania. Clin Infect Dis. 1999;28:314–21. doi: 10.1086/515131. [DOI] [PubMed] [Google Scholar]
- 4.Cruickshank R. 12th ed. Churchill Livingstone: 1975. The practice of Medical Microbiology; pp. 652–5. [Google Scholar]
- 5.Weber R, Bryan RT, Schwartz DA, Owen RL. Human microsporidial infections. Clin Microbiol Rev. 1994;7:426–61. doi: 10.1128/cmr.7.4.426. [DOI] [PMC free article] [PubMed] [Google Scholar]


