Abstract
Background:
Lack of insight or awareness of illness is most frequently observed in patients with schizophrenia, and it influences treatment compliance. It has been hypothesized that the frontal dysfunction may explain poor insight in schizophrenia.
Aim:
The purposes of the study were to assess the degree of insight in schizophrenia and to examine the association, if any, between the degree of insight and executive functions in patients with schizophrenia.
Materials and Methods:
In this pre-post study, 30 patients of both sexes diagnosed to have schizophrenia were assessed with the Scale to Assess Unawareness of Mental Disorder and Wisconsin Card Sorting Test (WCST). They were assessed once at the time of admission and then at the time of their discharge.
Results:
The study revealed that 70% of the subjects possessed poor awareness of mental disorder. There was significant improvement of insight over time. The degree of insight was significantly associated with the performance on WCST 2nd assessment. WCST scores were able to explain 42% of the variance in insight.
Conclusion:
Majority of schizophrenic patients possess poor insight. This poor insight is significantly associated with poor executive function. Hence poor insight may have a cognitive etiology.
Keywords: Executive functions, insight, psychopathology, schizophrenia
INTRODUCTION
Schizophrenia is a major mental illness that causes changes in perception, thoughts and behavior. The disorder is characterized by positive symptoms, negative symptoms and neuropsychological deficit. Researchers found poor insight to be a prevalent feature of schizophrenia, as well as an important discriminating factor.[1] International Pilot Study for Schizophrenia (IPSS) (WHO, 1973) revealed that 85% of the subjects vigorously denied that they were ill.[2] Similarly one study found 69% of patients diagnosed as schizophrenia had no insight.[3] Another study demonstrated that 76% of “drug refusers” versus 40% of “drug compliers” had no insight into illness.[4] Poor insight influences treatment compliance, the degree of supervision required and the decision as to whether a patient can safely be discharged from inpatient settings.
David (1990) suggested that insight is composed of 3 distinct overlapping dimensions: (1) recognition that one has mental illness, (2) compliance with the treatments and (3) ability to recognize psychotic events (delusions and hallucinations) as pathological.[5] In issues of etiology of poor insight, there is a hypothesis that poor insight in schizophrenia stems from enduring cognitive impairments, and studies have indicated that these impairments are similar to those experienced by anosognostic patients.[6,7] Broadly speaking, researches had emphasized that poor insight is significantly related with executive functioning, especially as measured by Wisconsin Card Sorting Test (WCST).[8,9]
The term executive function is employed with increasing frequency in neuropsychology, largely in connection with attempts to describe the behavioral deficits exhibited by the patients with frontal lobe disease.[10] Specifically, executive skills permit an adaptive balance of maintenance and shifting of cognitive or behavioral responses to the environmental demands, permitting longer-term goal-directed behavior. Many tasks are used to measure executive function, such as WCST, Category Test, Stroop Test, Controlled Oral Word Association Test, etc. These tests measure different executive skills. Patients with schizophrenia show deficit on all of the measures compared with normal controls.[11,12]
In a study of 31 chronic schizophrenic patients, 2 variables on the WCST (viz., the number of categories completed and percent perseverative response) were found to significantly discriminate between subjects of high versus low awareness.[8] In another study, the researchers administered the WCST and repeated the test over a period of 1 year on the patients of schizophrenia with unimpaired insight.[9] Results indicated that subjects with impaired insight demonstrated consistently poorer performance than subjects with unimpaired insight. Subjects with impaired insight made significantly more perseverative errors and achieved fewer categories correct, a pattern of performance deficits identified with neuropsychological dysfunction in schizophrenia.
On the contrary, Cuesta and Peralta (1994) examined the relationship of the frontal neurological signs, abnormal involuntary movements, soft neurological signs and a neuropsychological battery of results with lack of insight. No correlation between poor performance and lack of insight was found on any test.[13]
Hence the confusion regarding the impact of executive function on insight still exists. In India, there is a prominent lack of literature addressing this issue. The present scenario of an Indian tertiary psychiatric institute shows majority of patients with poor insight come from the lower socioeconomic stratum of the society. This leads to poor compliance and then higher relapse rates. To break this vicious circle, lack of awareness needs much more attention from its theoretical as well as practical point of view. The aims of the present study were (1) to assess the degree of insight in subjects with schizophrenia and (2) to examine the association, if any, between degree of insight and executive function in subjects with schizophrenia.
MATERIALS AND METHODS
The present study was a pre-post hospital-based study that used purposive sampling technique. It was conducted in the inpatient department of an apex institute in eastern India during the time span of March 2004 to January 2005. For this study, 30 patients of both sexes (male, 24; female, 6) with the diagnosis of schizophrenia according to ICD-10 DCR (WHO, 1993) criteria were enrolled.[14] Patients who were cooperative, were within the age group of 18-50 years and had a minimum educational level of up to class VIII were included. Patients with any psychiatric comorbidity, including mental retardation; with any past history of significant head injury, substance abuse or dependence and epilepsy; and those who had undergone treatment with electroconvulsive therapy in the last 6 months were excluded. Data was collected in 2 phases: Once at the time of their admission and then at the time of their discharge.
Tools used
Socio-demographic and Clinical Data Sheet: It is a specially designed, semi-structured pro forma sheet, which includes various socio-demographic and clinical variables.
Brief Psychiatric Rating Scale: It is a general psychopathology scale having 24 items.[15]
Scale to Assess Unawareness of Mental Disorder: It is a standardized scale on which ratings are made on the basis of direct patient interview. It has 3 general items which are most widely used to define insight (global awareness of mental disorder, awareness of the achieved effects of medication and awareness of the social consequences of having a mental disorder), and these include assessment of both current and past time periods.[16]
Wisconsin Card Sorting Test: It is a clinical neuropsychological instrument that assesses abstract reasoning ability and the ability to shift cognitive strategy in response to changing environmental contingencies. It requires strategic planning, organized searching utilizing environmental feedback to shift cognitive sets, directing behavior towards achieving a goal and modulating impulsive responding. Hence it is referred to as a measure of frontal or prefrontal functioning.[17]
This study was conducted to investigate the insight in schizophrenia and its association with executive functions. It differed from the previous studies only on the point that they had used only onetime assessment procedure.[5,9,18] In the present study, pre-post design was incorporated to explain specifically the change of insight during treatment period and its relationship with executive functions. The studies on schizophrenia showed that there is prominent deficit in executive functions.[19–21] Hence at the beginning of this study, it was an obvious question whether executive functions change during the treatment period and whether there is any significant association between the changes in insight and the change of executive function. Onetime assessment would be unable to answer these questions. Hence two-time assessment was necessary for this study.
Procedure
First, the admission registers of different wards were scanned to find out whether there were any new admissions with diagnosis of schizophrenia. If there was any such patient, the patient was interviewed and his/her case record file examined. The inclusion and exclusion criteria were used to select patients. The patients were informed about the study and consent was taken. The socio-demographic and clinical data sheet was filled up on the basis of interview and case record file. After that, the tools mentioned above assessed the patient. This phase was termed as “1st assessment” and it was completed within 3 days of admission. Those patients who were not cooperative within the first 3 days were observed for the next 7 days. If they became cooperative, they were taken up for the study and the “1st assessment” phase was then done; but if not, they were dropped. The 30 patients who were assessed in the 1 st assessment phase were again assessed during the time of their discharge. This phase was termed as “2nd assessment.” The same procedure that was used for the 1stassessment was repeated.
Data analysis: Data was analyzed using statistical packages for social sciences (SPSS version 10.00). The following statistics were used: descriptive statistics, Pearson's product moment correlation, regression analysis and t test.
RESULTS
1st assessment phase
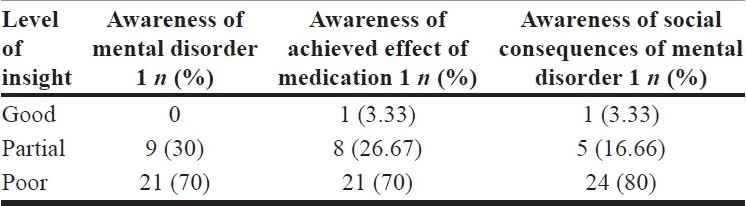
Results show that none of the subjects had good awareness of mental disorder — 30% of the subjects had partial awareness of mental disorder and 70% of the subjects had poor awareness of mental disorder [Table 1]. They also show that 70% of the subjects had poor awareness of achieved effect of medication, and 80% of the subjects had poor awareness of social consequences of mental disorder [Table 1].
Table 1.
Level of insight in 1st assessment phase (n = 30)
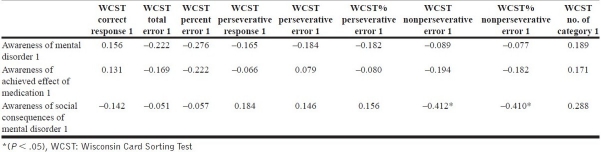
The study also indicates that awareness of social consequences of mental disorder was negatively related with WCST nonperseverative and percent nonperseverative errors [Table 2].
Table 2.
Correlation: Insight and Wisconsin Card Sorting Test in 1st assessment phase
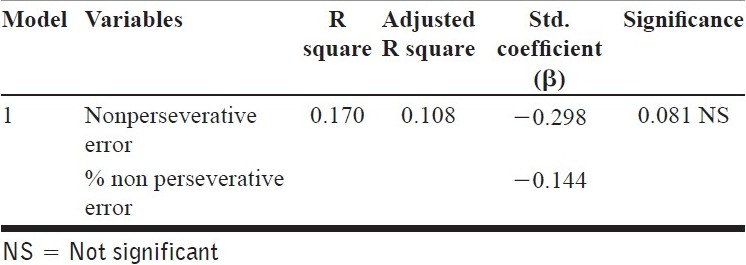
As there was significant association between awareness of social consequences of mental disorder and WCST nonperseverative and percent nonperseverative errors, the regression analysis was done with these variables.
Table 3 shows the model of regression analysis, which indicates that the independent variables were unable to explain the variance in the awareness of social consequences of mental disorder.
Table 3.
Regression: Dependent variable: Awareness of social consequences of mental disorder 1
2nd assessment phase
Results show that there was significant association between awareness of mental disorder and WCST variables in the 2nd assessment phase [Table 4]. Moreover, the WCST variables that had significant association with insight were analyzed in a linear regression model. This regression model indicates that independent variables could explain about 42% of the variance in the awareness of mental disorder [Table 5].
Table 4.
Correlation: Insight and WCST in 2nd assessment phase
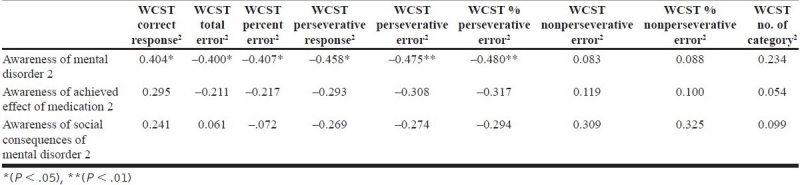
Table 5.
Regression: Dependent variable: Awareness of mental disorder 2
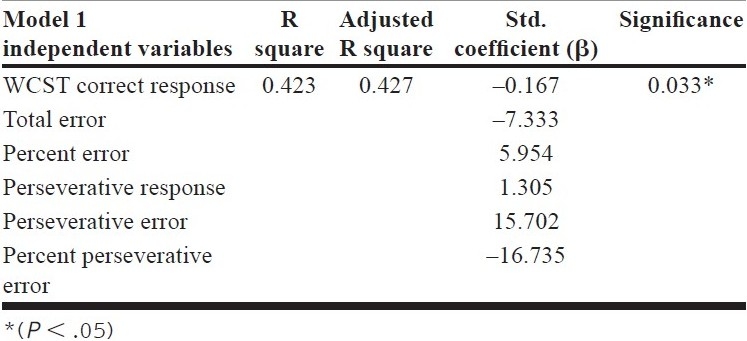
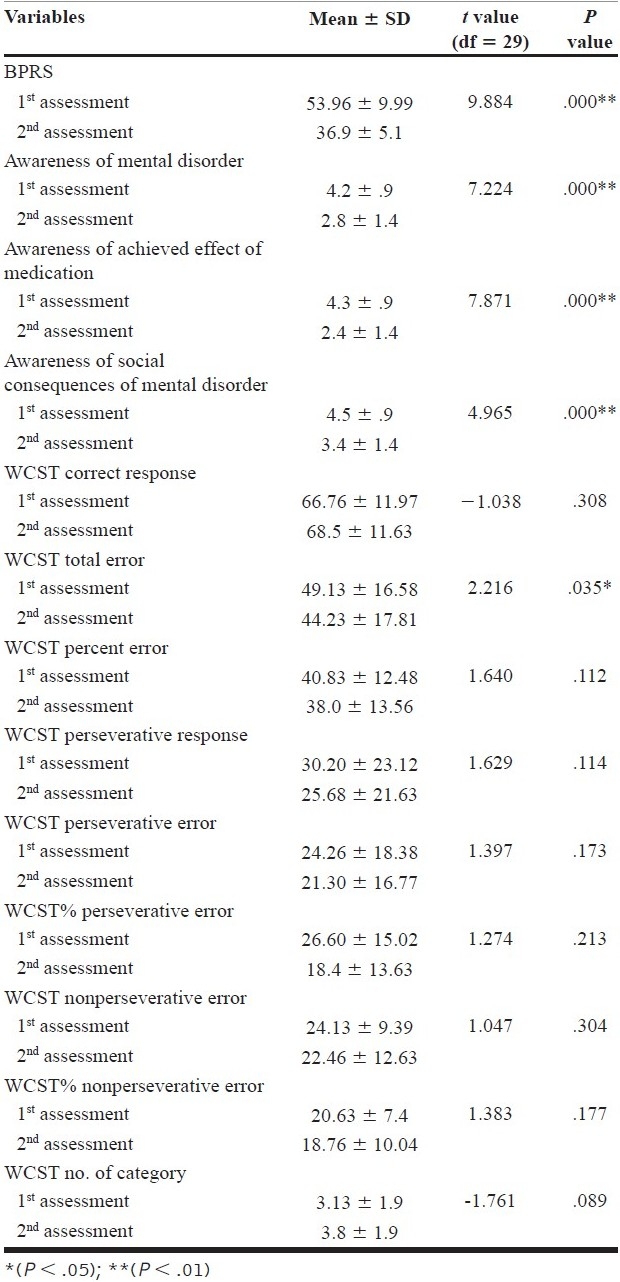
Table 6 shows that there was significant difference in psychopathology (BPRS scores), awareness of mental disorder, awareness of achieved effect of medication and awareness of social consequences of mental disorder between 1st assessment phase and 2nd assessment phase. This suggests that the psychopathology and level of insight had improved significantly in the subjects during hospitalization. But there was no significant difference in the WCST results between the two phases of assessment. Only WCST total error had significantly decreased from the 1st assessment phase to the 2ndassessment phase.
Table 6.
Difference in study variables between 1st assessment and 2nd assessment (n = 30)
DISCUSSION
Deficit of insight or awareness has recently been viewed as a complex and multidimensional phenomenon. The relationship between neuropsychological deficit and lack of awareness is obviously a matter of theoretical and practical importance. If a significant relationship exists between lack of awareness and neuropsychological dysfunction, support would be given to the hypothesis that unawareness may essentially be a cognitive deficit with an organic etiology.
The present study shows that around 70% of the subjects possessed poor awareness of mental disorder and of achieved effect of medication, and 80% of the subjects showed poor awareness of social consequences of mental disorder. This result is consistent with several findings. An earlier study found 69% of schizophrenic patients to have no insight.[3] A similar rate of 65% was obtained in a sample of chronic schizophrenics who had tardive dyskinesia.[22] In a study of medication compliance, 76% of “drug refusers” versus 40% of “drug compliers” had no insight into the presence of illness.[4,23]
When difference in performance on WSCT in both assessment phases was explored, it was seen that there was no significant difference between the two assessment phases. Apparently it indicated that performance in WCST remained stable over time. When the relationship between insight and WCST was explored, it was seen that there was no significant correlation between insight and poor performance in WCST in 1st assessment. However, the result of 2nd assessment phase indicated that there was a significant relationship between awareness of mental disorder and WCST measures (correct response, total error, percent error, perseverative response, perseverative error, percent perseverative error).
Further regression analysis showed that these independent variables were able to predict 42% of the variance in awareness of mental disorder.
This result poses a question: If there was no significant improvement in WCST scores over time, then how was it possible that only 2nd assessment phase showed significant association between insight and WCST scores? The probable answer of this question could be the standard deviation of WCST scores. The high standard deviation of WCST scores in both assessment phases indicated high variability in the sample group. On the other hand, insight had improved significantly, which may have had effect on the overall functioning of the individual. Hence it was highly possible that those who had better insight performed better in WCST; but due to high variability within the group, overall group performance was not found to have improved significantly in the 2nd assessment phase. Hence it was seen that WCST scores had significant impact on awareness of mental disorder.
This finding is consistent with several previous findings. For example, one study (Young et al., 1993) found a significant association between neuropsychological deficit as measured by the WCST and lack of awareness of illness in chronic schizophrenia.[6] It is noteworthy that they had also studied different measures of executive functions other than WCST (trail making tests A and B and verbal fluency test), but only the WCST showed a significant statistical relationship with lack of awareness of illness. Similarly Collins et al. showed significant relationship between neuropsychological functions (measured by WCST) and awareness of mental disorder.[18] Their results demonstrated that 44% of the variance in the awareness of mental disorder could be explained by the neuropsychological functions. As WCST performance reflects the ability to demonstrate mental flexibility through the generation, maintenance and switching of mental sets, along with the capacity to use feedback to correct errors, it would appear that such executive functions are most related to the dimension of awareness of illness.
CONCLUSION
From the findings, it can be concluded that subjects with schizophrenia possessed significantly poor awareness of (i) mental disorders, (ii) the achieved effect of medication for mental disorder and (iii) social consequences of mental disorder.
The present study had several limitations, such as:
Sample size was small; especially the number of females was very small in comparison to the number of males. Hence it is difficult to generalize the findings, particularly among women.
The underlying effect of typical/atypical drug was not ruled out.
As Wisconsin Card Sorting Test is the major tool to assess executive functioning, it can also be concluded that executive functioning could explain 42% of the total variance in insight; hence unawareness of mental illness has a cognitive etiology.
Footnotes
Source of Support: Nil,
Conflict of Interest: None.
REFERENCES
- 1.Carpenter WT, Bartko JJ, Carpenter CL, Strauss JS. Another view of schizophrenia subtypes. Arch General Psychiatry. 1976;33:508–16. doi: 10.1001/archpsyc.1976.01770040068012. [DOI] [PubMed] [Google Scholar]
- 2.Williams CC. Re-reading the IPSS research record. Soc Sci Med. 2003;56:501–15. doi: 10.1016/s0277-9536(02)00051-5. [DOI] [PubMed] [Google Scholar]
- 3.Lin IE, Spiga R, Fortsch W. Insight and adherence to medication in chronic schizophrenics. J Clin Psychiatry. 1979;40:430–2. [PubMed] [Google Scholar]
- 4.van Putten T, Crumpton E, Yale C. Drug referral in schizophrenia and wish to be crazy. Arch Gen Psychiatry. 1976;33:1443–6. doi: 10.1001/archpsyc.1976.01770120047004. [DOI] [PubMed] [Google Scholar]
- 5.David AS. Insight and psychosis. Br J Psychiatry. 1990;161:599–602. doi: 10.1192/bjp.161.5.599. [DOI] [PubMed] [Google Scholar]
- 6.Amador XF, Strauss DH, Yale SA, Gorman JM. Awareness of illness in schizophrenia. Schizophr Bull. 1991;17:113–32. doi: 10.1093/schbul/17.1.113. [DOI] [PubMed] [Google Scholar]
- 7.Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. Assessment of insight in psychosis. Am J Psychiatry. 1993;150:873–9. doi: 10.1176/ajp.150.6.873. [DOI] [PubMed] [Google Scholar]
- 8.Young , DA , Davila R, Scher H. Unawareness of illness and neuropsychological performance in chronic schizophrenia. Schizophr Res. 1993;10:117–24. doi: 10.1016/0920-9964(93)90046-l. [DOI] [PubMed] [Google Scholar]
- 9.Lysaker PH, Bell MD. Insight and cognitive impairment in schizophrenia: Performance of repeated administration of the Wisconsin Card Sorting Test. J Nerv Mental Dis. 1994;182:656–70. doi: 10.1097/00005053-199411000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Barrera A, McKenna PJ, Berrios GE. Formal thought disorder, neuropsychology and insight in schizophrenia. Psychopathology. 2009;42:264–9. doi: 10.1159/000224150. [DOI] [PubMed] [Google Scholar]
- 11.Barrett SL, Mulholland CC, Cooper SJ, Rushe TM. Pattern urocognitive impairments of ne in first-episode bipolar disorder and schizophrenia. Br J Psychiatry. 2009;195:67–72. doi: 10.1192/bjp.bp.108.054874. [DOI] [PubMed] [Google Scholar]
- 12.Owashi T, Iwanami A, Nakagome K, Higuchi T, Kamijima K. Thought disorder and executive dysfunction in patients with schizophrenia. Int J Neurosci. 2009;119:105–23. doi: 10.1080/00207450802324127. [DOI] [PubMed] [Google Scholar]
- 13.Cuesta MJ, Peralta V. Cognitive disorders in the positive, negative and disorganization syndromes of schizophrenia. Psychiatr Res. 1995;58:227–35. doi: 10.1016/0165-1781(95)02712-6. [DOI] [PubMed] [Google Scholar]
- 14.Barta A. ICD-10-CM official coding guidelines. J AHIMA. 2009;80:70–1. [PubMed] [Google Scholar]
- 15.Thomas A, Donnell AJ, Young TR. Factor structure and differential validity of the expanded brief psychiatric rating scale. Assessment. 2004;11:177–87. doi: 10.1177/1073191103262893. [DOI] [PubMed] [Google Scholar]
- 16.Amador XF, Gorman JM. Psychopathologic domains and insight in schizophrenia. Psychiatr Clin North Am. 1998;21:27–42. doi: 10.1016/s0193-953x(05)70359-2. [DOI] [PubMed] [Google Scholar]
- 17.Monika TB, Antoni F, Piotr G, Marian M, Krzysztof Z. Wisconsin Card Sorting Test in psychological examination of patients with psychiatric disorders. Pol Merkur Lekarski. 2008;25:51–2. [PubMed] [Google Scholar]
- 18.Collins AA, Remington GJ, Coulter K, Birkett K. Insight, neurocognitive function and symptom clusters in chronic schizophrenia. Schizophr Res. 1997;27:37–44. doi: 10.1016/S0920-9964(97)00075-3. [DOI] [PubMed] [Google Scholar]
- 19.Forbes NF, Carrick LA, McIntosh AM, Lawrie SM. Working memory in schizophrenia: a meta-analysis. Psychol Med. 2009;39:889–905. doi: 10.1017/S0033291708004558. [DOI] [PubMed] [Google Scholar]
- 20.Reichenberg A, Harvey PD. Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychol Bull. 2007;133:833–58. doi: 10.1037/0033-2909.133.5.833. [DOI] [PubMed] [Google Scholar]
- 21.Kolb B, Whishaw IQ. Performance of schizophrenic patients on tests sensitive to left or right frontal, temporal, or parietal function in neurological patients. J Nerv Ment Dis. 1983;171:435–43. doi: 10.1097/00005053-198307000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Caracci G, Mukherjee S, Roth SD, Decina P. Subjective awareness of abnormal involuntary movements in chronic schizophrenic patients. Am J Psychiatry. 1990;147:295–8. doi: 10.1176/ajp.147.3.295. [DOI] [PubMed] [Google Scholar]
- 23.Freudenreich O, Tranulis C. A prototype approach toward antipsychotic medication adherence in schizophrenia. Harv Rev Psychiatry. 2009;17:35–40. doi: 10.1080/10673220902724565. [DOI] [PubMed] [Google Scholar]