Abstract
Aim:
The study was designed to find out the incidence of thrombocytopenia in leptospirosis and to correlate thrombocytopenia with other parameters like renal failure, hepatic failure and bleeding manifestation like adult respiratory distress syndrome and to assess the role of platelet transfusion.
Materials and Methods:
50 cases of leptospirosis during the month of July and August 2005 were retrospectively analyzed. Criteria for selection were Lepto Tek Dri - dot test positive cases of the clinically suspected cases of Leptospirosis. Degree of thrombocytopenia was categorized as severe, moderate and mild. Presence of thrombocytopenia was clinically correlated with parameters like renal dysfunction, hepatic dysfunction and hemorrhagic manifestations (mainly ARDS). Role of platelet transfusion was assessed with reference to presence and degree of thrombcytopenia and hemorrhagic manifestations.
Results:
Out of total 50 patients 26 were male and 24 were females. Major bleeding manifestation in the form of ARDS was seen in 15 (30%) of patients. 28 (56%) patients had thrombocytopenia and 22 (44%) patients had normal platelet counts. Total number of patients with renal dysfunction was 24 (48%). Only four (18.18%) patients with normal platelet counts had renal dysfunction while 20 (71.42%) patients with thrombocytopenia had renal dysfunction. Only two (9.09%) patients with normal platelet counts and 48 (46.42%) patients with thrombocytopenia had hepatorenal dysfunction. Total number of patients with ARDS was 15 (30%). Of these two (13.33%) had normal platelet count while 13 (86.6%) patients were thrombocytopenic. Total 47 units of platelets were transfused to 12 patients in our study. Of these seven patients with severe thrombocytopenia required total 28 units, two patients with moderate thrombocytopenia required total seven units and patients with mild thrombocytopenia were transfused total 12 units of platelets.
Conclusion:
It is important to anticipate and recognize thrombocytopenia early in the course of leptospirosis so that appropriate steps can be taken to prevent it and to treat it with platelet transfusion when it develops
Keywords: ARDS, hepatic dysfunction, leptospirosis, platelet transfusion, renal dysfunction, thrombocytopenia
Introduction
Leptospirosis is a zoonosis with worldwide distribution. It is more prevalent in the developing countries. Hemorrhagic manifestations constitute the common clinical feature in leptospirosis.[1–3] The basic cause of bleeding manifestation in leptospirosis is the disruption of integrity of cell membranes of the endothelial cells lining of the small blood vessels in all parts of the body. Blood clotting mechanisms are also affected by liver cell injury. Thrombocytopenia is a consistent finding in patients with leptopirosis.[4] The suggested mechanisms for thrombocytopenia include peripheral platelet consumption due to widespread hemorrhages, immune mediated platelet destruction caused by antiplatelet antibodies and inhibited platelet production by bone marrow.[1,5–9] Hemorrhagic manifestations seen in leptospirosis are aggravated by thrombocytopenia. Acute renal failure and hepatic dysfunction are also known to be frequently associated with thrombocytopenia in letospirosis.[1,10–12]
With this background in mind, the present study was retrospectively designed to find out the incidence of thrombocytopenia in leptospirosis and to correlate thrombocytopenia with other parameters like renal failure, hepatic failure and bleeding manifestation like adult respiratory distress syndrome and to assess the role of platelet transfusion with reference to thrombocytopenia and hemorrhagic manifestations in patients with leptospirosis.
Materials and Methods
During the July 2005 floods in Mumbai there was an abrupt increase in the leptospirosis patients presenting with severe hemorrhagic manifestations with accompanying thrombocytopenia. The demand of platelets had gone up to 250 units per day as compared to the routine demand of 50 units per day. Patients with leptospirosis comprised the major bulk of this demand.
50 cases of leptospirosis during the month of July and August 2005 retrospectively analyzed. Data was obtained from the medical records section. Criteria for selection were Lepto Tek Dri - dot test positive cases of the clinically suspected cases of Leptospirosis. This is a screening test, which detects lgG and lgM antibodies against leptospira with a sensitivity of 90% and specificity of 92%. Incidence of thrombocytopenia was assessed among these 50 cases. Degree of thrombocytopenia was categorized as severe ≤ 20 × 109 / L, moderate between 20 to 50 × 109 / L and mild between 50 to 100 × 109 / L.15 Presence of thrombocytopenia was clinically correlated with other parameters renal dysfunction, hepatic dysfunction and hemorrhagic manifestations, mainly ARDS. Role of platelet transfusion was assessed with reference to presence and degree of thrombcytopenia and hemorrhagic manifestations. Renal dysfunction was defined as the any degree of increase in the levels of blood urea nitrogen or serum creatinine or both above normal range. Normal reference range - BUN: 10-15 mg%, Creatinine: 1 - 2 mg% or associated oliguria or anuria. Hepatic dysfunction was defined as any degree of increase in the level of bilirubin or liver enzymes. Normal reference range of bilirubin: up to 1 mg% SGOT -Up to 40 IU/L. Hemorrhagic manifestations were categorized as major and minor as follows. Major were adult respiratory distress syndrome, gastrointestinal bleeding, hematuria and intracranial bleeding. Minor were rash, conjunctival hemorrhages, petechial hemorrhages and epistaxis.
Results
Of the total 50 patients, 26 were male and 24 females. The age group of 11 to 20 years was most commonly affected. 31 patients (62%) were from 11 to 40 years of age. Fever and myalgia were the most common clinical manifestation followed by conjunctival suffusion and renal dysfunction. Major bleeding manifestation in the form of ARDS was seen in 30% of patients. 28 (56%) had thrombocytopenia and 22 (44%) patients had normal platelet counts. Total number of patients with renal dysfunction was 24 (48%). Only 18.18% (4) of patients with normal platelet counts had renal dysfunction while 71.42% (20) of patients with thrombocytopenia had renal dysfunction. Only 9.09% patients with normal platelet counts and 46.42% of patients with thrombocytopenia had hepatorenal dysfunction. Total number of patients with ARDS was 15 (30%). Of these 2(13.33%) had normal platelet count while 13(86.6%) patients were thrombocytopenic. There was no linear correlation between the degree of thrombocytopenia and the severity of renal failure, hepatorenal dysfunction and ARDS.
Out of 50 patients, 12 received platelet transfusion. Out of these 12 patients, 10 had major bleeding in the form of ARDS. One patient had minor bleeding episode in the form of epistaxis but had severe thrombocytopenia (< 20,000/-cu ml). One patient had no bleeding episode but his platelet count was markedly reduced (< 20,000/cu ml).
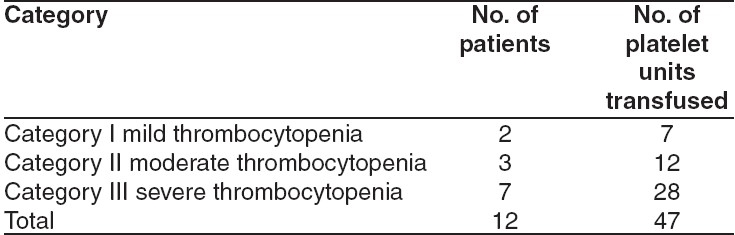
Total 47 units of platelets ware transfused to 12 patients in our study. Of these seven patients with severe thrombocytopenia required total 28 units, two patients with moderate thrombocytopenia required total seven units and patients with mild thrombocytopenia were transfused total 12 units of platelets. There was no linear correlation between the degree of thrombocytopenia and number of platelets units transfused [Table 1].
Table 1.
No of patients who received platelet transfusion
Those patients with milder form of leptospirosis were treated with oral amoxycilline or oral doxycyline for seven days. Most of the patients presented with moderate to severer form of leptospirosis and were treated with crystalline penicillin. None of them developed Jarisch Herxheimer reaction during treatment. For pain relief and fever, analgesics and antipyretics were given. Patient with severe leptospirosis were given intensive care. Fluid therapy and renal function monitoring was required for those patients with associated renal dysfunction. Two of these presented with acute renal failure and anuria required dialysis.
Seven out of 50 admitted patients of leptospirosis died, of which five had thrombocytopenia and died due to ARDS [Table 2].
Table 2.
Patients who died
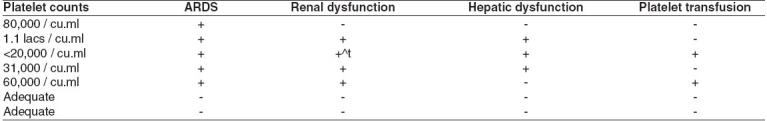
Two of these five received platelet transfusion. Remaining two patients with normal platelet counts had no bleeding manifestations and died due to unrelated causes. One died due to meningoencephalitis and other due to septicemia.
Discussion
In the present study of 50 patients, 26 (52%) were males and 24 (48%) were females. This is in contrast to other studies where males were predominantly affected owing to more outdoor activities and occupational exposure.[13] The most commonly affected age group in present study was first three decades comprising 62% of the total patients. More than half of the patients had history of prolonged contact with floodwater that hit Mumbai in July 2005. Many leptospirosis outbreaks in past have followed floods.[1,4,14]
Leptospirosis is characterized by a broad spectrum of clinical manifestations varying from unapparent infection to fulminant fatal disease.[1,2] Patients in our study showed a similar spectrum of clinical manifestations. Mild influenza like illness with fever, myalgia and headache was present in 60% of the patients. Others presented with conjunctival suffusion, rash, petechiae, along with fever, chills and myalgia. Jaundice was observed in 30(15%) patients most of whom also had renal failure as well as severe bleeding episodes in the form of adult respiratory distress syndrome.
Analysis of the platelet counts revealed normal platelet counts in 22 patients (44%) and thrombocytopenia in 28 (56%) patients. Of the total 28 thrombocytopenic patients 17 (61%) were males and 11 (39%) were females, while 24 (86%) were adult and four (14%) were pediatric patients. Various studies in past have reported thrombocytopenia in 50 to 93% of patients with leptospirosis.[4,6,12,15]
Acute renal failure has been documented in 16% to 40% cases of leptospirosis.[1] Thrombocytopenia has been described as the significant predictor of the development of acute renal failure.[1,10–12] Of the 50 patients under study, renal dysfunction was noted in 48% cases (24). Of these, only four had normal platelet counts while 20 were thrombocytopenic. So renal failure was evident in only 18.18% of the patients with normal platelet counts while it was found in 71.42% of the thrombocytopenic patients. Yang et al. have reported renal failure of up to 86.4% in leptosplrosis.[10] Study by Edwards et al. have reported renal failure up to 72.2% in thrombocytopenic patients and 21.4% in patients with normal platelet counts.[11]
Of the 50 patients studied, 15 patients showed hepatic dysfunction. Of these 15, two had normal platelet counts and 13 had thrombocytopenia. So hepatic dysfunction was found only in 9% of patients with normal platelet count, while 46% of the thrombocytopenic patients serum bilirubin and or transaminases (SGOT and SGPT) were raised. In various studies in past hepatic dysfunction in the form of hyperbilirubinaemia has been reported in up to 92% patients with leptospirosis.[16] Study by Yang et al. reported hepatic failure in 63.6% of patients with leptospirosis.[10]
Combined hepatic and renal involvement was observed in 15 (30%) of the 50 studied patients. Of the 15 patients involved, two had normal count and 13 were thrombocytopenic. Only 9% of the patients with normal platelet counts suffered hepatorenal dysfunction while 46% of the total 15 patients with thrombocytopenia suffered hepatorenal dysfunction.
Hemorrhagic manifestations constitute the common clinical features in Leptospirosis. Elizabeth De Francesco et al. reported 50% of deaths in severe cases of leptospirosis due to severe pulmonary hemorrhages.[4] In our study of the total 50 patients, 15 patients (30%) developed adult respiratory distress syndrome. Of these 15, only two(13%) had normal platelet counts, while 13(86%) patients had thrombocytopenia. Although thrombocytopenia is a consistent finding in patients with hemorrhagic manifestations, some patients without thrombocytopenia do present with bleeding manifestations. In our study, two patients with normal platelet counts developed ARDS. This explains the basic pathogenesis of bleeding diasthesis in Leptospirosis, which is vasculitis.[1,7,17] Although vasculitis is the most important cause of bleeding in leptospirosis, thrombocytopenia, uremia and coagulation disturbances, individually or as a group should be included among the contributing factors that lead to and worsen the bleeding episodes which represent the leading cause of death in this disease.[4,6]
Out of 15 patients with hepatorenal dysfunction, six patients (40%) suffered major bleeding episode in the form of ARDS. All of these patients were thrombocytopenic. Two of these six patients died due to ARDS. This explains the multisystemic affection in leptopsirosis associated with high mortality.
11 patients with bleeding diasthesis with thrombocytopenia were treated with platelet transfusion and fresh plasma. One patient, who had severe thrombocytopenia without bleeding, was given platelet transfusion. 15 patients developed acute respiratory distress syndrome with renal and hepatic failure. They were ventilated (mechanical ventilation), were treated with IV methylprednisolone along with crystalline penicillin and ionotropic support. Platelet transfusion has crucial role to play. Respiratory failure in leptospirosis managed by early platelet transfusion, mechanical ventilation, steroids in patients with platelet count < 50,000/- cumm or those who presented in short period of time with extensive reduction in the platelet count helps to reduce morbidity.[18] Total of 47 units of platelets were transfused to 12 patients in our study. Out of these, seven patients with severe thrombocytopenia required total 28 units, two patients with moderate thrombocytopenia were transfused total 12 units. There was no linear correlation between the degree of thrombocytopenia and number of platelets units transfused.
Seven out of 50 admitted patients of leptosplrosis died. Of which five had thrombocytopenia and died due to ARDS in spite of receiving mechanical ventilation, steroid and platelet transfusion. The other two died of unrelated cause viz septicemia and meningoencephalitis.
Conclusion
Thrombocytopenia is an important contributory factor in the pathogenesis of bleeding diasthesis in leptospirosis, which is the leading cause of death in this disease. It is important to anticipate and recognize this entity early in the course of leptospirosis so that appropriate steps can be taken to prevent it and to treat it with platelet transfusion when it develops.
Footnotes
Source of Support: We have not taken any financial support from anybody since it is a retrospective study. there was no need for taking any financial support for this study.
Conflict of Interest: Myself and Moushumi Suryavanshi have carried out this study and written this article. I declare that nobody will claim any authorship for this article.
References
- 1.Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14:296–326. doi: 10.1128/CMR.14.2.296-326.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Speelman P, editor. Leptospirosis. 14th ed. Harrison's principles of internal medicine; pp. 1036–8. [Google Scholar]
- 3.Karande S, Satam N, Kulkarni M, Bharadwaj R, Pol S. Leptospiral pneumonia. Indian J Pediatr. 2005;72:86. doi: 10.1007/BF02760593. [DOI] [PubMed] [Google Scholar]
- 4.Daher Ede F, Brunetta DM, de Silva Júnior GB, Puster RA, Patrocínio RM. Pancreatic involvement in fatal human leptospirosis: Clinical and histopathological features. Rev Inst Med Trop Sao Paulo. 2003;45:307–13. doi: 10.1590/s0036-46652003000600002. [DOI] [PubMed] [Google Scholar]
- 5.Davenport A, Rugman FP, Desmond MJ, Ganta R. Is thrombocytopenia seen in patients with leptospirosis immunologically mediated? J Clin Pathol. 1989;42:439–40. doi: 10.1136/jcp.42.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicodemo AC, Del Negro G, Amato Neto V. Thrombocytopenia and leptospirosis. Rev Inst Med Trop Sao Paulo. 1990;32:252–9. doi: 10.1590/s0036-46651990000400004. [DOI] [PubMed] [Google Scholar]
- 7.Lsogai E, Kimura K, Haryashi S, Kubota T, Fujii N, Lsogai H. Role of platelet activating factor (PAF) on cellular responses after stimulation with leptospire lipopolysaccharide. Microbial Immunol. 1997;41:271–5. doi: 10.1111/j.1348-0421.1997.tb01200.x. [DOI] [PubMed] [Google Scholar]
- 8.Law-Koune, Picard JD, Van Den Linden A, Michalt JC. Thrombocytopenia in leptospirosis: Role of antiplatelet antibodies. Press Med. 1998;17:1315–6. [PubMed] [Google Scholar]
- 9.Faine S. Factors affecting the development of carrier state in leptospirosis. J Hyg (Cambridge) 1962;60:427–34. doi: 10.1017/s0022172400020556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang HY, Hsu PY, Pam MJ, Wu MS, Lee CH, Yu CC, et al. Clinical distinction and evaluation of leptospinosis in Taiwan: A case control study. J Nephrol. 2005;18:45–53. [PubMed] [Google Scholar]
- 11.Edwards CN, Nicholson GD, Everard CO. Thrombocytopenia in leptospirosis. Am J Trop Med Hyg. 1982;31:827–9. doi: 10.4269/ajtmh.1982.31.827. [DOI] [PubMed] [Google Scholar]
- 12.Turgut M, Sunbul M, Bayirli D, Bilge A, Leblebienglu H, Haznedaraglu I. Thrombocytopenia complicating the clinical course of leptospiral infection. J Int Med Res. 2002;30:535–40. doi: 10.1177/147323000203000511. [DOI] [PubMed] [Google Scholar]
- 13.Karande S, Satam N, Kulkarni M, Bharadwaj R, Pol S. Leptospiral pneumonia. Indian J Pediatr. 2005;72:86. doi: 10.1007/BF02760593. [DOI] [PubMed] [Google Scholar]
- 14.Vintez JM. Detection of leptospirosis in India. Arch Dis Child. 2003;88:1033. doi: 10.1136/adc.88.12.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edwards CN, Nicholson GD, Hassell TA, Everard CO, Callender J. Thrombocytopenia in leptospirosis: The absence of evidence for disseminated intravascular coagulation. Am J Trop Med Hyg. 1986;35:352–4. doi: 10.4269/ajtmh.1986.35.352. [DOI] [PubMed] [Google Scholar]
- 16.Peces R. Acute renal failure in severe leptospirosis. Nephrol Dial Transplant. 2003;18:1235–6. doi: 10.1093/ndt/gfg110. [DOI] [PubMed] [Google Scholar]
- 17.Dobrina A, Nardon E, Vecile E, Cinco M, Patriarca P. Leptospira icterohemorrhagiae and leptospire peptidolgycans induce endothelial cell adhesiveness for polymorphonuclear leukocytes. Infect Immun. 1995;63:2995–9. doi: 10.1128/iai.63.8.2995-2999.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva JJ, Dalston MO, Carvalho JE, Setúbal S, Oliveira JM, Pereira MM. Clinicopathological and immunohistochemical features of the severe pulmonary form of leptospirosis. Rev Soc Bras Med Trop. 2002;35:395–9. doi: 10.1590/s0037-86822002000400017. [DOI] [PubMed] [Google Scholar]


