Abstract
Background and objective:
The ready availability of blood in Surat city has resulted in its liberal use. Surat Raktadan Kendra and Research Centre (SRKRC) is 30 years old blood bank having license to supply blood components. In spite of publishing quarterly bulletin and organizing seminars to update clinicians’ knowledge still we have not achieved rational use of blood. Present study has evaluated the use of single unit as well as whole blood transfusion for adult surgery cases.
Materials and Methods:
A total of 8470 surgery cases in the age group of 19 years to 95 years receiving 13070 units of whole blood and 3761 units of red cell concentrate (RCC) during surgery were analyzed on the basis of incidence of single unit and whole blood transfusions, sex and Hb values using Microsoft Excel.
Results:
Analysis revealed that 38.9% cases received single unit and 77.7% whole blood transfusions. Females more frequently received single unit transfusion than males (p< 0.001). The highest incidence of single unit (62.2%) and whole blood transfusion (95.2%) was observed for urogenital surgeries. The lowest incidence (22.9%) of single unit transfusion was for cancer surgeries. There was no significant difference in the mean Hb level at which male and female cases, received single unit transfusion (p>0.5). Mean Hb concentration was about 10.0 g/dl for patients receiving single unit of whole blood and 8 g/dl for those who received single unit of RCC.
Conclusion:
Surgery patients are receiving inappropriate transfusions. Continuous awareness programmes are needed to achieve judicious use of blood.
Keywords: Whole blood, red cell concentrate, single unit of blood, judicious use of blood, surgery
Any healthy adult can donate one unit of blood (350ml or 450 ml) without the need of any replacement fluid. Under such circumstances is it necessary to transfuse a healthy adult with a single unit of transfusion during elective surgery? This question has been raised again and again and the literature reports have expressed controversial opinions.[1–3] A Single unit of red blood cells transfusion can increase Hb by approximately 1 to 1.5 g in a 70 kg adult, which is therapeutically insignificant rise.[1,4] Moreover considering the risks associated with transfusion it is beneficial to prevent such transfusions.
Surat Raktadan Kendra and Research Centre (SRKRC) is a stand-alone blood bank, supplying blood to needy patients of Surat city since last 30 years and has license to supply whole blood and various components. In Surat there is an awareness regarding voluntary blood donation and most of the time there is an adequate stock of blood. We find it difficult to prevent single unit transfusions or whole blood transfusions as a large number of doctors and several hospitals send requisitions.
We analyzed 39 months’ data of red cell transfusions given to patients undergoing different types surgeries, to evaluate the transfusion practice in surgery cases.
Material and Methods
Analysis of data generated by our blood bank from January 2002 to March 2005, on utilization of whole blood/Red cell concentrate (RCC) for surgery patients was carried out. Study includes adult patients in the age group of 19 to 95 years. Patient's details provided by the doctor, like sex, age, diagnosis, type of surgery, hemoglobin (Hb) etc. were entered in the Excel software of Microsoft Office 2000. Simultaneously details like patient's blood group, number of blood units issued etc were also entered. All the entries were double-checked using markers like full name, hospital name, blood group, age and sex. If more than one requisition forms were received then all the supplied units were pooled together. Care was taken to make an authentic list of patients receiving single unit transfusion. Since blood reserved for transfusion is generally kept in the blood bank itself and released only when transfusion is needed, the possibility of issued blood not being used is remote.
Most of the surgeries were planned, except for the obstetric patients and trauma cases. For the purpose of analysis, surgery cases were divided into groups mentioned below:
Abdominal: Intestinal obstruction, peptic ulcer, laparotomy, cholecystostomy, colectomy splenectomy etc.
Amputation: Majority of the cases are of diabetes requiring foot amputation
Cancer: Involving organs like breast, prostrate, bladder, pancreas, liver, tongue, lips, cheek, larynx, esophagus etc and different types tumors.
Obstetrics and Gynecology: Medical termination of pregnancy, ectopic pregnancy, cesarean section, dilatation and curettage, vesicular mole, hysterectomy etc.
Orthopedic: Majority are the trauma cases having different types of fractures and a few cases of knee or hip replacement
Urogenital: Transurethral resection prostatectomy, open prostatectomy, nephrolithotomy, cystotomy, ureterolithotomy etc.
Other surgeries: This group includes cases of hernia, fistula, piles, neurosurgery, cardiothoracic and vascular surgeries. It was not possible to make individual group of each type of surgery, as the number of cases was small to carry out statistical analysis.
Unknown: In large number of requisitions clinicians just wrote "Surgery" without giving any details regarding type of surgery.
Analysis of mean and standard deviation of hemoglobin values was carried out on Microsoft Excel.
Results
During 39 months period 8470 adult patients (>18 years) consisting 4485 females and 3985 males received 13070 units of whole blood and 3761 units of RCC during surgery. Majority (77.7%) of the patients received whole blood. The average rate of blood utilization for surgery was two units per case.
Single unit transfusions were given to 3294 (38.9%) cases. Of them 2960 (89.9%) received the whole blood. Out of 4485 female patients 549 (12.24%) were given single unit transfusion while out of 3985 males 394 (9.88 %) received. There was significant difference in the incidence of single unit transfusion to male and female patients (P< 0.001).
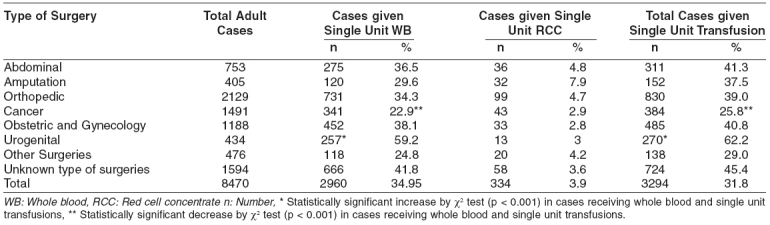
Table 1 gives the incidence of single unit transfusions in different types of surgeries. The incidence of single unit transfusion was the highest (62.2%) for Urogenital surgeries particularly for the cases of benign enlargement of prostate and urinary stones (P < 0.001). Cancer surgeries had the lowest incidence of single unit transfusions (P < 0.001). Incidence of single unit whole blood transfusion was maximum i.e., 257 (95.2%) out of 270 cases, for Urogenital surgeries and minimum i.e., 120 (78.9%) out of 152 cases for amputation surgeries on diabetic patients.
Table 1.
Incidence of Single Unit Transfusion for Different Surgeries
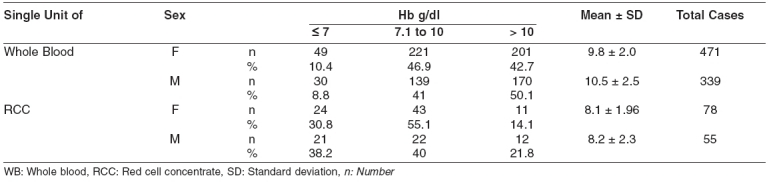
Cases receiving single unit transfusion were further analyzed on the basis of Hb and sex. Hemoglobin (Hb) value, at which the doctor ordered single unit of blood, was available for 943 (28.62%) out of 3294 cases. Table 2 presents the correlation between Hb concentration and type of red cell product given, with respect to sex. The Hb trigger for giving whole blood was about 10 g/dl and for RCC transfusion it was 8 g/dl. RCC was more frequently transfused to patients having Hb less than 7g/dl. 212 (38.6%) females and 182 (46.2%) males received single unit transfusion of whole blood or red cell concentrate when Hb level was greater then 10 g/dl. There was no significant difference in the mean Hb level at which male and female cases received single unit transfusion (p>0.5).
Table 2.
Hb level of surgery cases receiving single unit with respect to sex
Discussion
Even though worldwide there is a big gap in demand and supply of blood, the ready availability of blood and blood components in Surat has resulted in liberal use of blood transfusions. In adult blood loss up to 20% (about one liter in 70 kg person) is well tolerated provided the circulatory volume is maintained with colloids or crystalloids.[5,6] Transfusion of red cell concentrate is recommended only if there is >30% blood loss. Recognition in 1980 that blood transfusion carries a risk of HIV infection forced the reevaluation of indications for transfusion. Therefore the transfusion trigger has shifted from optimal Hb level of 10 g/dl to the level necessary to meet patient's tissue oxygen demands.[7] Current evidence[2,8] indicate that for most patients more restrictive transfusion is more effective.
WHO[1] strongly discourages single unit transfusions in adults. In the past many countries regarded single unit transfusions as a bad practice.[3,9] In the 1980s and early 1990s hospital based transfusion committees reviewed single unit transfusions. To prevent transfusion audits clinicians started ordering two units and hence clinical practice is now dominated with two unit transfusions. In the present study the average utilization per case was two units. A survey[10] in Canada showed that > 90% of physicians administered two units of packed red cells. Many scientists currently feel that a single unit transfusion would be adequate for large number of patients.[2,11] This will reduce the allogenic blood exposure. Our data presented in table 1 shows that about 31.8% transfusions given to surgical patients are of single units. The highest incidence is observed in urogenital surgeries in patients having benign enlargement of prostate or renal stones. These surgeries do not result in sufficient blood loss to justify blood transfusion. Hence in our opinion single unit transfusions to these patients were given only to impress patients’ relatives. Shulman[11] has recommended a single unit transfusion for patients having symptoms of ischemia or hypotension with anemia or other conditions like renal failure or heart failure for which additional blood units were contraindicated. Most of the subjects undergoing elective surgery are healthy and above conditions are not associated with them.
Surgeons often reserve the blood for surgery but it may not be required. Since hospitals don′t have blood bank refrigerator we advise doctors to keep reserved blood in our blood bank. In Surat most of the hospitals are within 5 to 15 minutes distance by vehicle, from SRKRC. Thus as soon as an emergency arises blood bank can issue the blood. Therefore the possibility that the supplied blood not being used for transfusion is remote.
Hb values of the patients who received single unit of whole blood were analyzed. Unfortunately the values were available for only 28.6% patients. Since clinicians always estimate Hb prior to transfusion the reason for non-availability of Hb values could be reluctance of clinicians to fill up requisition form properly. However blood bank cannot reject the requisition just because Hb value is not written. It is reasonable to assume that the Hb distribution among the patients whose values were not available was the same as those patients whose Hb values were available, as there was no other bias.
An expert consensus conference convened by United States Food and Drugs Administration opined that transfusion was likely to be necessary when the Hb level dropped below 7 g/dl and unlikely to be necessary when it was greater than 10 g/dl.[12] As seen in Table 2 only 124 (13%) out of 943 cases had Hb value below 7 g/dl and hence justified in receiving transfusion of single unit. 394 (41.8%) cases had Hb value greater than 10 g/dl and there was no justification for single unit transfusion.
In the present study out of 3294 transfusions 2960 (89.8%) were whole blood transfusions. Since the red cell mass is the same in whole blood and RCC and considering the adverse effects due to plasma and cellular components like white blood cells and platelets in whole blood, it is advisable to use red cell concentrate. Most of the diabetic patients undergoing amputation were anemic but still only 21.1% of them received RCC and remaining were given whole blood.
In Surat city there is a lot of awareness regarding voluntary blood donation. Therefore except during the vacation when there may be crisis, through out the year all blood banks in Surat have an adequate stock of blood. Sometimes doctors use this blood inappropriately by transfusing just a single unit or by using the whole blood. They should understand that whole blood is a raw material consisting red cells, platelets, white cells and more than 200 proteins. It poses a risk of alloimmunisation, transmission of infections, graft versus host disease, transfusion related acute lung injury etc. SRKRC publishes a quarterly bulletin “Raktadan” and also organizes seminars to educate clinicians regarding judicious use of blood. But a very few clinicians are interested in accepting guidelines from the blood bank.
Conclusion
This study concludes that more awareness programmes are necessary for surgeons/anesthetists to prevent inappropriate use of blood.
References
- 1.New Delhi: WHO; 1998. WHO publication number SEA/HLM/31: Blood safety and clinical technology: Strategy for rational use of blood; pp. 24–31. [Google Scholar]
- 2.Ma M, Eckert K, Ralley F, Chin-Yee I. A retrospective study evaluating single-unit red blood cell transfusions in reducing allogeneic blood exposure. Transfusion Med. 2005;15:307–12. doi: 10.1111/j.0958-7578.2005.00592.x. [DOI] [PubMed] [Google Scholar]
- 3.Reece RL, Beckett RS. Epidemiology of single-unit transfusion. A one-year experience in a community hospital. JAMA. 1966;195:801–16. doi: 10.1001/jama.1966.03100100053014. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy MS, Julius C. Transfusion therapy. In: Harmening DM, editor. Modern blood banking and transfusion practices. 3rd ed. Jaypee Brothers: New Delhi; 1998. pp. 316–33. [Google Scholar]
- 5.Geneva: WHO Blood Transfusion Safety; 2001. WHO publication number WHO/BTS/99-3: The clinical use of blood: Handbook. [Google Scholar]
- 6.Hogman CF, Bagge L, Thoren L. The use of blood components in surgical transfusion therapy. World J Surg. 1987;11:2–13. doi: 10.1007/BF01658452. [DOI] [PubMed] [Google Scholar]
- 7.McFraland JC. Preoperative blood transfusions: Indications and options. Chest. 1999;115:113–21. doi: 10.1378/chest.115.suppl_2.113s. [DOI] [PubMed] [Google Scholar]
- 8.Carson JL, Hill S, Carless P, Hebert P, Henry D. Transfusion triggers: A systematic review of the literature. Transfus Med Rev. 2002;16:187–99. doi: 10.1053/tmrv.2002.33461. [DOI] [PubMed] [Google Scholar]
- 9.Crispen JF. The single-unit transfusion. A continuing problem. Pa Med. 1966;69:44–8. [PubMed] [Google Scholar]
- 10.Hebert PC, Wells G, Martin C, Marshall J, Blajchman MA, Pagliarello G, et al. A Canadian survey of transfusion practices in critically ill patients. Crit Care Med. 1998;26:482–7. doi: 10.1097/00003246-199803000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Shulman IA. Are single unit transfusion still considered suboptimal care.E Network Forum? California Blood Bank Society. 2 [Google Scholar]
- 12.Gettinger A. Transfusion in the preoperative period: A consideration of the risks and benefits as a guide to determine when and who to transfuse. IT ACCS. 2005:158–62. [Google Scholar]


