Abstract
Objectives:
Ropivacaine is a long-acting amide local anesthetic, which is structurally very similar to bupivacaine but produces less motor block and less cardiac and central nervous system toxicity. It is also about 40% less potent than bupivacaine. Our double blind study was designed to compare the clinical efficacy of the equipotent doses of ropivacaine 0.75% and bupivacaine 0.5% for epidural anesthesia and ropivacaine 0.2% and bupivacaine 0.125% for post-operative analgesia in patients undergoing bilateral mesh hernioplasty.
Methods:
Sixty-one patients were randomized to receive 15 ml of 0.75% ropivacaine or 0.5% bupivacaine. Sensory and motor block characteristics were compared. Changes in heart rate, mean arterial blood pressure, and adverse effects were noted. For post-operative analgesia, 0.2% ropivacaine and 0.125% bupivacaine were given as continuous epidural infusion. Analgesia using VAS scores, motor block, volume of local anesthetic used and patient satisfaction was assessed.
Results:
There was no significant variation in the sensory block profile. A greater intensity of motor block was achieved with bupivacaine in the beginning but by 30 minutes the difference was not significant. Duration of motor block was similar in the two groups. Visual analog scale scores were similar in both groups during the post-operative period, with a similar motor block profile. No major side effects were noted in any group.
Conclusion:
The equipotent doses of ropivacaine and bupivacaine provided good quality epidural anesthesia and post-operative analgesia.
Keywords: Bilateral inguinal mesh hernioplasty, bupivacaine, epidural anesthesia, post-operative analgesia, ropivacaine
INTRODUCTION
Ropivacaine is one of the newer long-acting amide local anesthetic agents used in regional anesthesia which is similar to bupivacaine in chemical structure and anesthetic action.[1] Ropivacaine differs from most other amide-type local anesthetics in that it is a pure S-enantiomer, instead of a racemate. This feature improves the safety of ropivacaine, and studies have shown ropivacaine to have less cardiovascular and central nervous system toxicity than bupivacaine.[2] Sensory and motor blocking characters of equal concentrations of ropivacaine and bupivacaine have been compared previously[3,4] and as we know ropivacaine is about 40% less potent than bupivacaine.[5–7] So we decided to compare 0.75% ropivacaine with 0.5% bupivacaine, and 0.2% ropivacaine with 0.125% bupivacaine which should be equipotent.
Epidural bupivacaine is a commonly used technique for anesthesia and post-operative analgesia. 0.75% Ropivacaine when compared to 0.5% bupivacaine produced equally effective anesthesia when administered epidurally for elective caesarean section.[8] The more favorable toxicity profile of ropivacaine as compared to bupivacaine makes it a good choice for post-operative epidural analgesia also. A dose finding study for post-operative analgesia in patients undergoing abdominal surgery demonstrated that 0.2% ropivacaine provided the best balance between analgesia and motor block.[9]
The aim of the present prospective randomized controlled double blind study was to compare the clinical efficacy of epidural ropivacaine 0.75% and bupivacaine 0.5% for bilateral inguinal mesh hernioplasty, followed by 0.2% ropivacaine and 0.125% bupivacaine for post-operative analgesia.
METHODS
After obtaining institutional Ethics Committee approval and written informed consent, 61 ASA physical status I or II male patients were enrolled in this randomized, double blind study. All were aged 30–60 years, body weight 50–90 kg and height >150 cm. Exclusion criteria were any contraindication to epidural anesthesia, allergy to local anesthetics of the amide type, and communication difficulties that would prevent reliable assessment. All patients were kept fasting for 6 h and premedicated with oral ranitidine 150 mg, ondansetron 4 mg and diazepam 5 mg and preloaded with 750 ml Ringer lactate solution. They were then allocated randomly to receive epidural anesthesia using either 0.75% ropivacaine (Group R) or 0.5% bupivacaine (Group B). Randomization was based on a computer-generated code that was prepared at a remote site and sealed in opaque, sequentially numbered envelopes. The study drug for anesthesia and post-operative analgesia was prepared by a separate anesthesiologist. The anesthesiologist doing the study, the surgeon, the patient, and the staff were blinded to the drug used.
In the lateral decubitus position, a 20G epidural catheter with multiple lateral orifices was inserted in a cephalad direction at L2-4 space via an 18-gauge Touhy needle. The epidural space was identified by loss of resistance to air. After negative aspiration for cerebrospinal fluid and blood, a 3 ml test dose of 2% lignocaine with adrenaline was given over 15 s through the catheter. If there were no untoward effects after 3 min, the main dose of 15 ml of study drug was injected over 4 min. Surgery was not commenced until analgesia to pinprick was achieved bilaterally to T6. If it did not reach T6 within 30 min, an additional 5 ml of study drug was administered. If the block did not reach T6, or if surgical anesthesia was still not achieved, the patient was withdrawn from further efficacy assessment and received an anesthetic regimen at the discretion of the investigator.
SpO2 was monitored with a pulse oximeter, heart rate with ECG, and systolic and diastolic arterial blood pressure with an automated non-invasive blood pressure cuff. Recordings were made every 5 min until the end of surgery. Hypotension (defined as fall in Mean arterial pressure more than 20% of baseline value) was treated with bolus doses of 3 mg ephedrine and increased infusion of Ringer lactate. Bradycardia (defined as heart rate <50/min) was treated with 0.6 mg atropine.
The upper limits of sensory block to pinprick and motor block were determined bilaterally at 5 min intervals for 30 min after the main dose of study drug.
The onset of sensory block was taken as the time to reach T6 level. The motor block was assessed using the modified Bromage scale: Grade 0 = no weakness; Grade 1 = inability to raise extended leg; Grade 2 = inability to flex knee; Grade 3 = inability to move any joint in legs. At the end of the surgery, the patient was transferred to post anesthesia care unit (PACU) and motor block checked every 15 min till the block receded to Grade 1. The duration of motor block was from the time of absence of knee flexion to return of knee flexion.
The overall quality of anesthesia was judged by the anesthesiologist, and the surgeon on a numeric rating scale (NRS 1-3 unsatisfactory, 4-6 good, 7-10 excellent). Adverse events such as nausea, vomiting, shivering, and urinary retention were recorded.
Post-operatively, the patients’ vital signs were monitored continuously and analgesia was assessed using the visual analog scale (VAS) (0- no pain to 10- maximum pain). Epidural infusion was started only when the patient complained of pain, i.e. VAS of >3. The duration of analgesia was taken as time of achieving T6 level to VAS >3. Using blinded syringes, patients in group B received 0.125% bupivacaine and Group R received 0.2% ropivacaine. All patients received an initial loading dose of 6 ml of the study drug. This was followed by an infusion of 7 ml/h with top-ups of 5 ml as required for breakthrough pain. Intramuscular injection Ketarolac was prescribed for pain that did not respond to top-ups of the study drugs. VAS scores at rest and movement, i.e. after coughing were recorded and overall satisfaction with epidural were obtained 24 h after surgery by the investigator. Patients’ satisfaction was graded on the NRS. The total volume of local anesthetic used as top up and the use of rescue analgesic were also noted. Motor block was assessed using the modified Bromage scale.
Statistical analysis
Sample size was estimated before the study using duration of motor block as the primary outcome using a pilot study. A sample size of 27 subjects in each group was required at α = 0.05, and power of 90%. Continuous variables are presented as the mean ± SD and categorical variables are presented as frequencies (percentage of patients.) Statistical analyses were performed using the SPSS system (SPSS Inc., Chicago, IL). Normal scale variables were described by relative and absolute frequencies, and differences between groups were assessed by using the χ2 test. The Mann-Whitney U test was used for nonparametric variables. A t-test for independent variables or a repeated-measures analysis of variance was used to compare the two groups. The P value < 0.05 was considered as statistically significant.
RESULTS
A total of 61 patients were enrolled in the study. One patient was excluded from the study as the epidural block was inadequate for surgery even after top up dose of 5 ml at 30 min after the main dose. There was no incidence of accidental dural puncture.
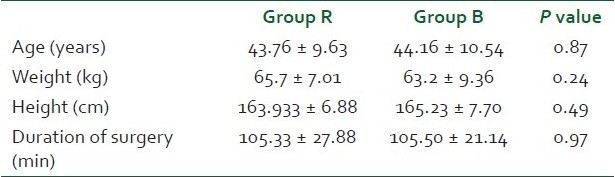
The demographic data were comparable in both the groups. The duration of surgery was also not different in the two groups. Baseline Heart rate and mean arterial blood pressure and SpO2 were similar in both groups [Table 1].
Table 1.
Demographic data and baseline hemodynamic parameters
The onset time for sensory block to T6 varied between 10 and 25 min in both the groups. It was slightly faster with the ropivacaine group though the difference was not statistically significant. The duration of analgesia varied between 5 and 7.5 h for ropivacaine and 4.6 and 7.0 h for bupivacaine [Table 2]. The frequency of various degrees of motor block at 10, 20, and 30 min are shown in Figure 1. A greater intensity of motor block was achieved at an earlier stage in the group B (P = 0.06 at 10 min, P = .008 at 20 min), but by about 30 min the difference was not significant (P = .468). After the main dose of study drug 40% of patients in the ropivacaine group and 50% of patients in the bupivacaine group achieved grade 3 block within 30 min. About 5% of patients in Group R had only grade 1 block by 30 min. The time to recovery of motor block to grade 1 was similar in both groups [Table 2].
Table 2.
Sensory & motor block and NRS scores
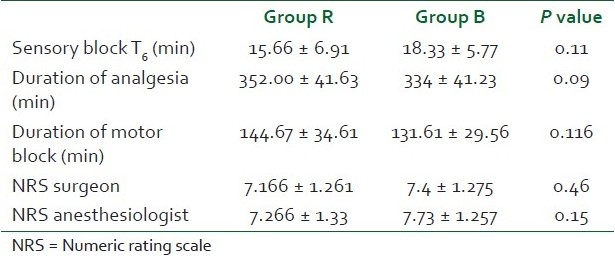
Figure 1.
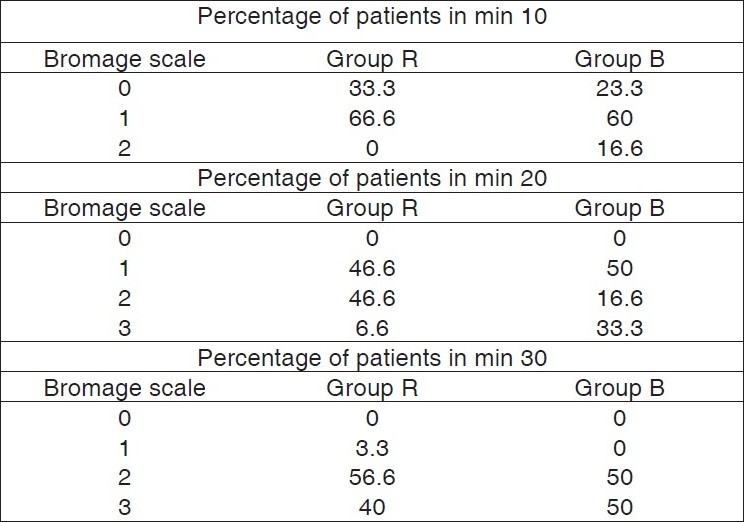
Analysis of degree of motor block in 10, 20 and 30 minutes using modified Bromage scale. Percentage of patients—Y axis. Time in minutes—X axis
All patients in the study had satisfactory relaxation for surgery. The anesthesiologist and surgeon rated the anesthesia as excellent [Table 2].
The adverse effects were very few and are mentioned in [Table 3].
Table 3.
Incidence of adverse effects
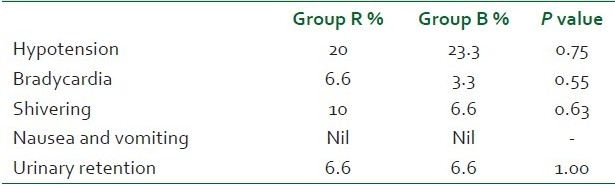
Hypotension was the most common adverse effect in both groups. Six patients in group R and seven patients in group B had mild hypotension which responded to a bolus dose of 3 mg ephedrine and fluids. Bradycardia occurred in two patients in the ropivacaine group and 1 patient in the bupivacaine group and required a single dose of 0.6 mg atropine.
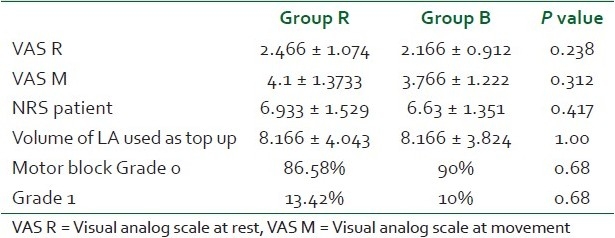
Regarding post-operative analgesia, the VAS score at rest was similar in both groups. During movement VAS scores were higher in the ropivacaine group though the difference was not statistically significant. The degree and frequency of motor block was similar in both groups. Only three patients in group R and two patients in group B had inability to lift the extended leg. None of the patients had a higher degree of motor block. The mean volume of local anesthetic used as top up when patients complained of pain was 8.166 ± 4.043 in group R and 8.166 ± 3.824 in group B [Table 4] (P value = 1). One patient in each group required intramuscular Ketorolac.
Table 4.
Data for post-operative analgesia
DISCUSSION
Ropivacaine is a long-acting amide-type local anesthetic, released for clinical use in 1996. In comparison with bupivacaine, it is equally effective for subcutaneous infiltration, epidural, and peripheral nerve block for surgery, obstetric procedures, and post-operative analgesia. Ropivacaine because of its pure S-enantiomer form is less cardio toxic than Bupivacaine. Various studies have shown that it is less potent than Bupivacaine.[5–7] For the same reason the motor blocking characteristics of ropivacaine is less intense and of lesser duration.[10] This can lead to a decrease in the quality of anesthesia especially in surgeries where good muscle relaxation is required.[11,12] Increasing the concentration of ropivacaine resulted in greater degree and longer duration of motor block and a positive correlation between the total dose of ropivacaine and the sensory block profile has also been demonstrated.[13] The wider safety margin of ropivacaine allows the use of higher concentrations and doses compared with bupivacaine with less risk of systemic toxicity, ensuring better surgical anesthesia.[14]
In this study, both 0.75% ropivacaine and 0.5% bupivacaine produced excellent epidural anesthesia in patients undergoing bilateral inguinal mesh hernioplasty.
The equipotent doses of ropivacaine and bupivacaine compared in the study produced a sensory block profile that was not different statistically. All patients in the study groups achieved T6 level within 30 min. The duration of sensory anesthesia with 0.75% ropivacaine has also been determined in open-label studies of ropivacaine, and the total duration found in our study is similar to prior reports.[15,16] The duration and intensity of motor block with 0.75% ropivacaine in our study was comparable to 0.5% bupivacaine and the motor block characteristics of the two drugs appear to be clinically indistinguishable.
Hypotension was the most common side effect and the decrease in blood pressure was transient, quickly resolved by increasing infusion of Ringer lactate and a single bolus dose of 3 mg ephedrine.
Epidural analgesia with local anesthetics is one of the most effective techniques used for post-operative pain relief and may improve patient outcome.[17] Finding the balance between motor block and analgesia is the major challenge in epidural analgesia.
The quality of post-operative analgesia in both groups was good. Vital signs were stable in all patients throughout the study period. A similar degree of pain relief was observed in the two groups without differences in volume of local anesthetic consumption and need for rescue analgesia. Patient from each group reported similar pain scores at rest. During mobilization and while coughing the pain scores were higher in the ropivacaine group though it did not reach significant values. Previous studies also have shown lower pain scores with bupivacaine 0.125%.[18,19] There were no significant differences among the groups with regard to the incidence of motor block. None of the patients had motor block with Bromage scale >1. Liu et al.[20] reported more frequent and more intense motor block when the same dose of ropivacaine was given as a 0.2% solution as compared with a 0.1% solution. In their study, an increased incidence of motor block in the ropivacaine 0.2% group was clinically evidenced only when patients were tested for their ability to ambulate, which we did not assess. No significant differences were observed between the 0.1% and 0.2% solutions when they used the Bromage scale, as in our study.
The volume of local anesthetic consumed above the baseline infusion was similar in the two groups. Even though the total volume of both drugs used in 24 h is almost the same, the amount of drug used is significantly more in the ropivacaine group. This adds to the argument that ropivacaine is less potent than bupivacaine. Addition of opioids to local anesthetic can decrease the local anesthetic requirement by approximately 25%.[21] This can further decrease the amount of ropivacaine used as shown in other studies[19] and warrants further investigation.
CONCLUSION
Ropivacaine 0.75% and bupivacaine 0.5% provided good quality epidural anesthesia for bilateral inguinal mesh hernioplasty. Ropivacaine 0.2% and bupivacaine 0.125% provided good quality post-operative analgesia with a minimal motor block. Motor block and sensory block profile of both the drugs were similar in the study and hence the concentrations compared can be considered equipotent.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Whiteside JB, Wildsmith JA. Developments in local anaesthetic drugs. Br J Anaesth. 2001;87:27–35. doi: 10.1093/bja/87.1.27. [DOI] [PubMed] [Google Scholar]
- 2.Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of iv infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–14. doi: 10.1093/bja/78.5.507. [DOI] [PubMed] [Google Scholar]
- 3.Bariskaner H, Ayaz M, Bayramoglu FB, Dalkilic N, Guney O. Bupivacaine and Ropivacaine.Comparative effects on nerve conduction block. Methods Find Exp Clin Pharmacol. 2000;29:337–41. doi: 10.1358/mf.2007.29.5.1117558. [DOI] [PubMed] [Google Scholar]
- 4.Zaric D, Nydahl PA, Philipson L, Samuelsson L, Heierson A, Axelsson K. The effect of continuous lumbar epidural infusion of ropivacaine (0.1%, 0.2% and 0.3%) and 0.25% bupivacaine on sensory and motor block in volunteers. A double blind study. Reg Anaesth. 1996;21:14–25. [PubMed] [Google Scholar]
- 5.Lacassie HJ, Habib AS, Lacassie HP, Columb MO. Motor blocking minimum local anaesthetic concentration of bupivacaine, levobupivacaine and ropivacaine in labor. Reg Anesth Pain Med. 2007;32:323–9. doi: 10.1016/j.rapm.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Capogna G, Celleno D, Fusco P, Lyons G, Columb M. Relative potencies of bupivacaine and ropivacaine for analgesia in labour. Br J Anaesth. 1999;82:371–3. doi: 10.1093/bja/82.3.371. [DOI] [PubMed] [Google Scholar]
- 7.Polley LS, Columb MO, Naughton NN, Wagner DS, van de Ven CJ. Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labour: Implications for therapeutic indexes. Anesthesiology. 1999;90:944–50. doi: 10.1097/00000542-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Kampe S, Tausch B, Paul M, Kasper SM, Bauer K, Diefenbach C, et al. Epidural Block With Ropivacaine and Bupivacaine for Elective Caesarean section: Maternal Cardiovascular Parameters, Comfort, and Neonatal Well-Being. Curr Med Res Opin. 2004;20:7–12. doi: 10.1185/030079903125002649. [DOI] [PubMed] [Google Scholar]
- 9.Scott DA, Chamley DM, Mooney PH, Deam RK, Mark AH, Hägglöf B. Epidural ropivacaine infusion for post operative analgesia after major lower abdominal surgery: A dose finding study. Anesth Analg. 1995;81:982–6. doi: 10.1097/00000539-199511000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Brown DL, Carpenter RL, Thompson GE. Comparison of 0.5% ropivacaine and 0.5% bupivacaine for epidural anesthesia in patients undergoing lower-extremity surgery. Anesthesiology. 1990;72:633–6. doi: 10.1097/00000542-199004000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Crosby E, Sandler A, Finucaine B, Writer D, Reid D, McKenna J, et al. Comparison of epidural anaesthesia with ropivacaine 0.5% and bupivacaine 0.5% for Caesarean section. Can J Anaesth. 1998;45:1066–71. doi: 10.1007/BF03012393. [DOI] [PubMed] [Google Scholar]
- 12.Griffin RP, Reynolds F. Extradural anaesthesia for Caesarean section: A double-blind comparison of 0.5% ropivacaine with 0.5% bupivacaine. Br J Anaesth. 1995;74:512–6. doi: 10.1093/bja/74.5.512. [DOI] [PubMed] [Google Scholar]
- 13.Finucane BT, Sandler AN, Mckenna J, Reid D, Milner AL, Friedlander M, et al. A double blind comparison of ropivacaine 0.5%, 0.75%, 1.0% and bupivacaine 0.5% injected epidurally in patients undergoing abdominal hysterectomy. Can J Anaesth. 1996;43:442–9. doi: 10.1007/BF03018104. [DOI] [PubMed] [Google Scholar]
- 14.Stienstra R. The place of ropivacaine in anaesthesia. Acta Anaesthesiol Belg. 2003;54:141–8. [PubMed] [Google Scholar]
- 15.Morton CP, Bloomfield S, Magnusson A, Jozwiak H, McClure JH. Ropivacaine 0.75% for epidural anaesthesia in elective Casarean section: An open clinical and pharmacokinetic study in mother and neonate. Br J Anaesth. 1997;79:3–8. doi: 10.1093/bja/79.1.3. [DOI] [PubMed] [Google Scholar]
- 16.Chriselis N, Harrad J, Howell PR. A comparison of epidural ropivacaine 0.75% and bupivacaine 0.5% with fentanyl for elective caesarean section. Int J Obstet Anesth. 2005;14:212–18. doi: 10.1016/j.ijoa.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomized trials. BMJ. 2000;321:1493. doi: 10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pouzeratte Y, Delay J JM, Brunat G, Boccara G, Vergne C, Jaber S, et al. Patient-controlled epidural analgesia after abdominal surgery: Ropivacaine versus Bupivacaine. Anesth Analg. 2001;93:1587–92. doi: 10.1097/00000539-200112000-00055. [DOI] [PubMed] [Google Scholar]
- 19.Kanai A, Nakahara R, Okamoto H, Hoka S. Postoperative analgesia using continuous lumbar epidural infusion of Ropivacaine in comparison with bupivacaine. Masui. 2003;52:832–9. [PubMed] [Google Scholar]
- 20.Liu SS, Moore JM, Luo AM, Trautman WJ, Carpenter RL. Comparison of three solutions of ropivacaine/fentanyl for postoperative patient -controlled epidural analgesia. Anesthesiology. 1999;90:727–33. doi: 10.1097/00000542-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 21.D’Angelo R, Gerancher JC, Eisenach JC, Raphael BL. Epidural fentanyl produces labor analgesia by a spinal mechanism. Anesthesiology. 1998;88:1519–23. doi: 10.1097/00000542-199806000-00016. [DOI] [PubMed] [Google Scholar]


