Abstract
Aims and Context:
To evaluate the efficacy of adding clonidine to bupivacaine in bilateral infraorbital nerve block for hemodynamic changes, requirement of opioids, volatile agent, and muscle relaxants intraoperatively and relief of pain postoperatively
Setting and Design:
Prospective, randomized, double-blind study.
Methods:
Fifty pediatric patients aged less than 24 months undergoing elective cleft lip repair were randomly allocated to two groups of 25 each. After tracheal intubation, group A received bilateral infraorbital nerve block with 1 ml solution of clonidine (1 μg/kg) and bupivacaine 0.25%, and group B received 1 ml of 0.25% bupivacaine. Hemodynamic parameters, intraoperative requirement of volatile anesthetic agent, muscle relaxant, and analgesic were recorded. Pain was assessed postoperatively using the Face, Legs, Activity, Cry, Consolability scale till the first rescue drug was given.
Statistical Analysis:
Two sample unpaired t-test and the correlation r test.
Results:
The duration of analgesia from the time of administration of block in group A was 667.72 ± 210.74 min compared to 558.48 ± 150.28 min in group B (P<0.05).
Conclusion:
Addition of clonidine as an adjunct to local anesthetic significantly decreased the requirement of other anesthetic drugs and significantly prolonged the duration of postoperative analgesia without any adverse effects.
Keywords: Cleft lip surgery, clonidine, infraorbital nerve block
INTRODUCTION
Surgery for repair of cleft lip is a common procedure in infants and young children. In India, the incidence of defect is 1 in 781 of live birth.[1] Repair of primary cleft lip as early as possible is gaining popularity as this has many advantages like aesthetic improvement, improved parental bonding, improved development of the alveolar ridge, and ability to breast feed and hence improved nutrition.[2]
Alleviation of postoperative pain is important in these patients, as inadequate postoperative sedation with vigorous crying may lead to wound dehiscence, discomfort to the child and parents, accidental removal of surgical dressings, intravenous catheters and drains, requirement of extra nursing care and can have adverse physiological effects.[3–5] Good pain relief minimizes the oxygen requirement, reduces cardio-respiratory demands, and promotes early ambulation and recovery.[6]
The fear of respiratory depression using opioids has renewed the interest in regional anesthesia to provide safe and effective postoperative analgesia. Infraorbital nerve block has been advocated as a suitable local analgesic technique for cleft lip surgery and superficial surgery on the mid face.[7] The infraorbital nerve supplies the upper lip, lower eyelid, and adjacent skin of the cheek and nose. Unilateral or bilateral infraorbital nerve block has been performed with a very high success rate.
Various adjuvants to local anesthetics have been studied to improve the duration of block. One such agent which has regained popularity is clonidine. Clonidine is a mixed alpha-1 and alpha-2 adrenoceptor agonist with a predominant alpha-2 action. Traditionally, it has been used as an antihypertensive agent since the late sixties. Its primary effect is sympatholysis and it reduces peripheral norepinephrine release by stimulation of the prejunctional inhibitory alpha-2 adrenoceptors.[8] Clonidine has been studied for various nerve blocks. The use of clonidine as an adjuvant to local anesthetic for infraorbital nerve block has been studied in adults but not much literature is available regarding its use in infants.
We designed this study to evaluate the efficacy of adding clonidine to bupivacaine in bilateral infraorbital nerve block for relief of pain postoperatively following repair of cleft lip in children under two years of age. In this study, we evaluated whether adding clonidine to local anesthetics has effects on the hemodynamic changes, requirement of opioids, volatile agent, and muscle relaxants intraoperatively.
METHODS
The study protocol was approved by our hospital ethical committee, and informed consent was obtained from parents. This randomized prospective double-blind study was conducted on 50 American Society of Anesthesiologists (ASA) physical status I and II children aged less than 2 years undergoing elective cleft lip repair under general anesthesia. Patients with local infection at the site of injection of block, history suggestive of drug allergy, children with any systemic disease that compromises any cardiovascular, respiratory or neurological function, any other congenital anomaly, patient with history of upper and lower airway disease, coagulation disorders, and children with history of sleep apnea and in whom postoperative ventilation may be required were excluded from the study.
The study size was ascertained after reviewing the existing data as most of the studies[2,6,7,9,10] have taken a sample size of 25 in each group, further as the total duration of study was 9 months that include data collection (6 months), compilation, and analysis. The total patients that underwent surgery were 67 but after eliminating the confounding factors of age, associated anomalies, and other variables the investigator finally analyzed the sample of 50 patients.
A day prior to surgery all patients underwent pre-anesthetic check-up. After taking detailed history, thorough general, physical, and systemic examination was done and weight of the patient was recorded. For randomisation, computer-generated numbers equal to the number of patients who were scheduled for the study was put into serially labelled opaque sealed envelopes. Before surgery, an envelope containing the random number was drawn for each patient. If the number was even, clonidine from a 150 μg/ml ampoule was diluted and 1 μg/kg was drawn with a tuberculin syringe and added to 0.5 ml of 0.5% bupivacaine; the resulting mixture was reconstituted with saline to a volume of 1 ml to maintain a bupivacaine concentration of 0.25% (Group A; n = 25). If the number was odd, a solution of 1 ml 0.25% bupivacaine solution was prepared by adding 0.5 ml saline to 0.5 ml of 0.5% bupivacaine (Group B; n = 25) by one of the authors, who was no further involved in data collection and surgery. The patient, anesthesiologist who performed the block, and surgeon were blinded to which anesthetic agent would be used.
All the patients were premedicated with syrup phenargan (1 mg/kg) and standard guidelines for fasting were followed. In both the groups, children were induced with 50% oxygen and 50% nitrous oxide and incremental concentration of sevoflurane starting from 1% and gradually increasing to 5-6%, that is 1% every 6-8 breaths via Jackson Rees Circuit, following which intravenous cannulation took place and appropriate iv fluid was started. Routine monitors were placed. Pulse, blood pressure, colour, SpO2, EtCO2, blood loss, temperature, and fluid requirement was monitored. After taking baseline readings, hemodynamic parameters were noted at the time of induction, time of giving the block, start of volatile agent, start of surgery, and then every 10 min after till the end of surgery and then at the time of extubation.
All the patients received fentanyl 2 μg/kg intravenously before incision. Tracheal intubation was facilitated by atracurium 0.5 mg/kg. After confirming and fixing the tube, bilateral infraorbital nerve block was given to all the patients by the trained anesthetist. All the blocks were given by the same person to rule out any bias. Patient was placed in supine position with head in neutral position. Part was prepared by painting with povidone iodine and methylated spirit. For the block, the point of entry was an imaginary line connecting the pupil (in the neutral position) and angle of the mouth, which was bisected by the perpendicular line drawn from the alae nasi.[9] A 24-G needle was directed medially and cephalad from this point until it reached the foramen and in group A 1 μg/kg clonidine and 0.25% bupivacaine 0.5 ml was given, while in group B 0.25% bupivacaine 0.5 ml was injected. Pressure was applied for 2 min and the injection point massaged to prevent haematoma. The procedure was repeated on the other side. The block was considered to be effective if there were no significant hemodynamic changes to surgical stimulation intraoperatively and if there was no excessive cry on recovery.
All the patients were ventilated to normocapnia. The end tidal concentration of the isoflurane was adjusted to 1-1.5 Minimal alveolar concentration (MAC) in oxygen and nitrous oxide. Fresh gas flow was 1.5 l/min for all children. The administration of iv fluids was left to the discretion of the anesthetist. Operation theatre temperature was kept constant around 24°C and surface warming was done.
The nitrous oxide and volatile anaesthetic were discontinued simultaneously without tapering with the last surgical stimulus and the patient was allowed to wake up spontaneously with minimal handling. Ventilation with 100% oxygen was continued until the establishment of spontaneous ventilation. The independent observer timed the patient's emergence events from stoppage of anesthesia to
First gross limb movement
Eye opening
Establishment of regular breathing pattern
Extubation
Sedation at extubation was assessed using University of Michigan sedation scale (UMSS)[11]
-
0
Awake/alert
-
1
Minimally sedated: Tired/sleepy/appropriate response to verbal conversation and/or sound
-
2
Moderately sedated: Somnolent/sleepy easily arousable with light tactile stimulation
-
3
Deeply sedated: Deep sleep arousable with significant physical stimulation
-
4
Unarousable
The criteria for transferring the patient from operating room to recovery area were being awake, moving all limbs, normal oxygen saturation with no need for mandible support, patent airway and normal respiratory pattern, stable hemodynamic, normothermia, and pain free.
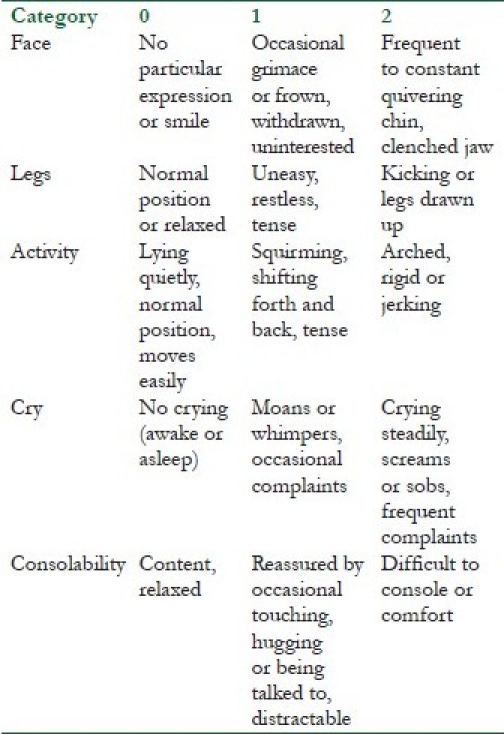
During the recovery period and postoperatively, the patient was observed for complications like nausea, vomiting, pain, delirium, dysarrhythmia, cyanosis, hypothermia, and shivering. Postoperative pain was assessed by a trained postoperative nurse who was unaware of the drug given usingFace, Legs, Activity, Cry, Consolability (FLACC) score.
The assessment of pain was done using FLACC score:[12]
The score was interpreted as:
0: Relaxed, comfortable
1-3: Mild discomfort
4-6: Moderate pain
7-10: Severe pain or discomfort or both
The readings were noted after every 20 min till the time first rescue drug was administered. Children with a score of 3 or more were given analgesia as per standard protocols and the time was recorded.
Descriptive statistics (mean, standard deviation, range) were used to summarize patient's demographic data and operative details. The statistical analysis was done using two sample unpaired t-test and the correlation r test. The comparison of the postoperative complications was done by using Microsoft Excel, Epi Info (CDC, Atlanta). For computing, the proportions and chi square, a P value of <0.05 was taken as a reference of significance.
RESULTS
Technique
Patients receiving block had no local or systemic undesirable effects and no complications of the technique were observed. There were no drop-outs in the study because of the failed block.
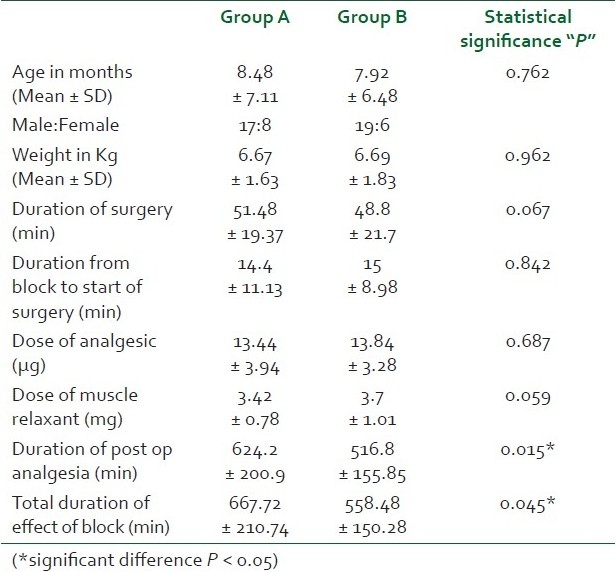
Demographic data and operative details
The groups were comparable in terms of demographic data and no significant difference was detected (P > 0.05) [Table 1]. It was observed that the dial concentration of isoflurane required to achieve the end tidal concentration of 1-1.5 MAC in group A was low, while higher dial concentration was required in group B to achieve the same MAC value. We observed a positive co-relation in the requirement of the volatile agent required intraoperatively and the type of drugs used in the block.
Table 1.
Demographic profile of the patients and the operative details
Hemodynamics
The difference in the baseline heart rate (P = 0.56), systolic (P = 0.62), diastolic (P = 0.44), and mean arterial pressure (P = 0.47) between the two groups up to the start of surgery was statistically not significant.
There was significant difference in systolic blood pressure between the two groups at the start of surgery (P = 0.004), at 10 minutes (P = 0.04), and at 20 minutes (P = 0.03), respectively. Thereafter, no significant difference was observed in the systolic blood pressure during the surgery. There was a significant difference in diastolic blood pressure at the start of surgery (P = 0.03) and after 10 minutes (P = 0.03) but no significant difference was observed later.
Significant difference was observed in mean arterial pressure at 10 min (P = 0.04), and 20 min (P = 0.03) after the start of surgery [Figure 1]. No change in peripheral oxygen saturation and arrhythmia was observed in any patient intra operatively.
Figure 1.
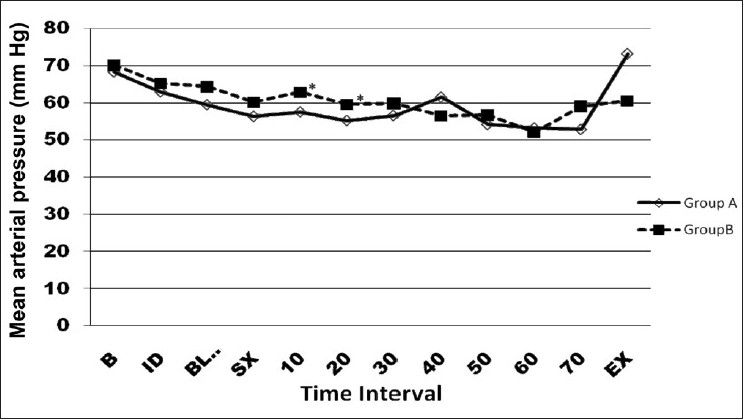
Comparison of mean arterial pressure at different time interval between the two groups (*significant difference) (B = Baseline, ID = Induction, BLOCK = At the time of block, SX = Start of surgery, 10 = 10 min after start of surgery, 20 = 20 min after start of surgery, 30 = 30 min after start of surgery, 40 = 40 min after start of surgery, 50 = 50 min after start of surgery, 60 = 60 min after start of surgery, EX = Extubation)
Postoperative recovery and complications
In both the groups the recovery endpoint first reached was limb movement followed by spontaneous respiration followed by spontaneous eye opening. Patients in group A patients achieved recovery milestones earlier than patients in group B, which was significant (P < 0.05) [Table 2].
Table 2.
Recovery milestones and comparison of UMSS score between the two groups
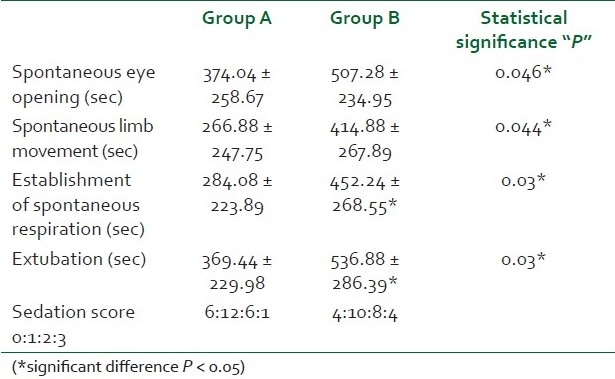
In group A, 1(4%) patient had laryngospasm soon after extubation, while in group B 2(8%) had laryngospasm. In group A, 1 (4%) patient and in group B 2(8%) patients were shifted with oropharyngeal airway to the recovery room. In both groups A and B, 1(4%) patient each had postoperative shivering and 1(4%) patient was agitated in group B. There was no significant difference in the incidence of postoperative complication between the two groups.
Postoperative sedation and analgesia
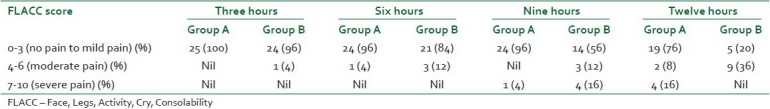
The number of patients having higher sedation scores were comparable between the two groups but was not significant statistically [Table 2]. Both groups had lower resting values of FLACC pain score which denote good analgesia [Table 3]. The qualitative pain relief was better with group A as at all times, and more patients in group A had lower scores. There was significant difference in the time of rescue drug requirement between the two groups (P = 0.015). Nineteen (76%) subjects did not require rescue analgesia in group A up to 12 hours postoperatively, while 5(20%) subjects in group B did not require rescue drug up to 12 hours.
Table 3.
Pain scores calculated using the FLACC scale in both the groups
DISCUSSION
The results of our study show significant prolongation of duration of postoperative analgesia and better quality of pain relief from infraorbital nerve block when clonidine was used as an adjuvant to local anesthetics. We also observed that clonidine did not cause much hemodynamic variation intraoperatively and sedation postoperative but it decreased the requirement of anesthetic agents intraoperatively.
We selected this age group as neonates and infants cannot effectively communicate the pain they feel. They may not be able to speak (preverbal) or may not have suitable words to express the degree of pain they suffer. The assessment of pain thus in a small child is mostly in an indirect way like either observing the physiological changes or the behavioural responses of the child to pain.[13]
In recent years, there has been a considerable change in the concept of postoperative pain relief in infants and young children. Local or regional analgesia is the platform of multimodal analgesia for pediatric patients, whatever be their age, type of surgery or of painful procedures, unless there is a specific contraindication. Local and regional analgesia provide dense intraoperative analgesia that continues into the postoperative period.[7,14]
Bupivacaine was chosen for the infraorbital nerve block in this study, as lignocaine leads to a shorter pain-free period. A peripheral nerve stimulator was not used to locate the infraorbital nerve as it is purely a sensory nerve; it can, however, be easily blocked at the point where it emerges from the infraorbital foramen. This foramen is either palpable or can be estimated from other palpable landmarks.[2] There are two well-known approaches to the infraorbital nerve: intraoral or extraoral.[2,15] The intraoral approach although is known to be as effective in producing upper-lip anesthesia as the percutaneous approach; but has also been associated with complications.[16] Extraoral approach for infraorbital block was thus chosen in this study as it is technically easier and safer.
Previous studies have shown that the duration of postoperative analgesia with bupivacaine ranges from 8-20 hours,[15,17] while in the present study the duration of post op analgesia with bupivacaine alone was 516.8 min. This difference in the duration of analgesia could be attributed to the higher concentration (0.25% 0.5%) and volume of bupivacaine (1 ml) on each side in the previous study while we used a lower concentration of bupivaciane (0.25%) and volume (0.5 ml) of bupivacaine on either side. Also, in the previous study the block was performed at the end of surgery and the duration of pain relief was observed from the end of surgery of adult patients.
When clonidine was added to the local anesthetic the duration of pain relief in our series increased by an average of 109.24 min (19.5%). The addition of clonidine to local anaesthetics increases the duration for peripheral nerve blocks by local mediated effects. There are two main theories on how clonidine may prolong sensory anesthesia. One of these suggests that clonidine may produce local vasoconstriction, resulting in a delayed absorption of local anesthetic and block prolongation. The second is that clonidine may directly bind to α2-adrenergic receptors to modify neuronal excitability.[18] It has also been suggested that clonidine may exert a peripheral analgesic action by releasing enkephalin-like substances.[19]
During single-dose peripheral nerve block with short or medium-acting local anesthetic, the minimum dose of clonidine required to significantly prolong the duration of both anesthesia and analgesia is 0.5 μg/kg but the results with long-acting local anesthetic the doses are not well defined.[20]
We did not observe a significant difference in heart rate and blood pressure between the two groups, which is in accordance to the previous studies[21,22] except a study by Adnan et al.[23] This difference could be because in these studies the blocks were administered as sole anesthetic and were not supplemented with any other drugs. In a study on haemodynamic parameters achieved by lidocaine with clonidine or epinephrine, administered for maxillary infiltration anesthesia, were studied. They observed a significant reduction in heart rate and systolic blood pressure in the lidocaine + clonidine group and significant increase in heart rate in the lidocaine + epinephrine group, 10 min after surgery. It has been shown clonidine produced an endothelium-independent vasocontractile effect on the isolated human infraorbital arteries.[24]
A positive correlation between the duration of volatile anaesthetic exposure and the emergence times was observed with group B, which was not present with group A. In both the groups, due to the block performed, there was no further requirement of any supplementation of muscle relaxant or analgesics intraoperatively.
Though not statistically significant patients in group B had higher sedation score a possible explanation could be that higher concentration of volatile anesthetics had been administered in group B to maintain the MAC of 1-1.5. The FLACC pain scores remained low throughout the period during which the infraorbital nerve block was effective. The maximum pain scores remained below 2 in most patients in both groups. Systemic analgesia was instituted as the FLACC scores increased to 3, at which time the study was terminated.
There were no systemic sedative effects such as sedation, nausea or vomiting with this dose of clonidine.
In group A we had a quiet, sleeping child, a contended mother and a relieved staff. The pain assessment scoring system is a convenient and good method. The limitation of this study was that we were unable to pinpoint the most sensitive criteria in the scoring system.
CONCLUSION
We conclude that bilateral infraorbital nerve block given with 0.25% bupivacaine and clonidine 1 μg/kg provides more prolonged postoperative analgesia than 0.25% bupivacaine alone in cleft lip repair. The quality of analgesia, intraoperative requirement of other anaesthetic agent, and recovery profile is better when clonidine is added to the local anesthetic. We recommend the use of clonidine as an adjuvant to local anaesthetic for infraorbital nerve block for paediatric population.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Radhakrishna U, Ratnamala U, Gaines M, Beiraghi S, Hutchings D, Golla J, et al. Genomewide Scan for Nonsyndromic Cleft Lip and Palate in Multigenerational Indian Families Reveals Significant Evidence of Linkage at 13q33.1-34. Am J Hum Genet. 2006;79:580–5. doi: 10.1086/507487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosenberg AT, Kimble FW. Infraorbital nerve block in neonates for cleft lip repair: Anatomical study and clinical application. Br J Anaesth. 1995;74:506–8. doi: 10.1093/bja/74.5.506. [DOI] [PubMed] [Google Scholar]
- 3.Smessaert A, Schehr CA, Artusio JF., Jr Observations in the immediate postanesthesia period II.Mode of recovery. Br J Anaesth. 1960;32:181–5. doi: 10.1093/bja/32.4.181. [DOI] [PubMed] [Google Scholar]
- 4.Vlajkovie GP, Sindjelie RP. Emergence Delirium in children: Many questions, few answers. Anesth Analg. 2007;104:84–91. doi: 10.1213/01.ane.0000250914.91881.a8. [DOI] [PubMed] [Google Scholar]
- 5.Chari P, Gupta S. Measurement and assessment of pain in children and adults. Indian J Pain. 1993;7:4–12. [Google Scholar]
- 6.Gaonkar V, Daftary SR. Comparison of preoperative infraorbital block with peri incisional infiltration for postoperative pain relief in cleft lip surgeries. Indian J Plast Surg. 2004;37:105–9. [Google Scholar]
- 7.Morton NS. Local and regional anesthesia in infants. Continuing Education in Anesthesia, Crit Care Pain. 2004;4:148–51. [Google Scholar]
- 8.Basker S, Singh G, Jacob R. Clonidine in Paediatric – A review. Indian J Anaesth. 2009;53:270–80. [PMC free article] [PubMed] [Google Scholar]
- 9.Eipe N, Choudhrie A, Pillai DA, Choudhrie R. Regional anesthesia for cleft lip repair: A preliminary study. Cleft Palate Craniofac J. 2006;43:138–41. doi: 10.1597/05-025.1. [DOI] [PubMed] [Google Scholar]
- 10.Jonnavithula N, Durga P, Kulkarni DK, Ramachandran G. Bilateral intra-oral, infra-orbital nerve block for postoperative analgesia following cleft lip repair in paediatric patients: comparison of bupivacaine vs bupivacaine-pethidine combination. Anesthesia. 2007;62:581–5. doi: 10.1111/j.1365-2044.2007.05028.x. [DOI] [PubMed] [Google Scholar]
- 11.Malviya S, Vopel Lewis T, Tait AR. A comparison of observational and objective measures to differentiate depth of sedation in children from birth to 18 years of age. Anesth Analg. 2006;102:389–94. doi: 10.1213/01.ANE.0000184045.01780.73. [DOI] [PubMed] [Google Scholar]
- 12.Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurse. 1997;23:293–7. [PubMed] [Google Scholar]
- 13.Tremlett M. Anesthesia for cleft lip and palate surgery. Curr Anaesth Crit Care. 2004;15:309–16. [Google Scholar]
- 14.Gehdoo RP. Post operative pain management in paediatric patient. Indian J Anaesth. 2004;48:406–14. [Google Scholar]
- 15.Prabhu KP, Wig J, Grewal S. Bilateral infraorbital nerve block is superior to peri-incisional infiltration for analgesia after repair of cleft lip. Scand J Plast Reconstr Surg Hand Surg. 1999;33:83–7. doi: 10.1080/02844319950159668. [DOI] [PubMed] [Google Scholar]
- 16.Lynch MT, Syverud SA, Schwab RA, Jenkins JM, Edlich R. Comparison of Intraoral and percutaneous approaches for Infraorbital nerve block. Acad Emerg Med. 1994;1:514–9. doi: 10.1111/j.1553-2712.1994.tb02543.x. [DOI] [PubMed] [Google Scholar]
- 17.Nicodemus , HF , Ferrer MJ, Cristobal VC, de Castro L. Bilateral infraorbital block with 0.5% bupivacaine as post-operative analgesia following cheiloplasty in children. Scand J Plast Reconstr Surg Hand Surg. 1991;25:253–7. doi: 10.3109/02844319109020629. [DOI] [PubMed] [Google Scholar]
- 18.Cucchiaro G, Ganesh A. The effects of clonidine on postoperative analgesia after peripheral nerve blockade in children. Anesth Analg. 2007;104:532–7. doi: 10.1213/01.ane.0000253548.97479.b8. [DOI] [PubMed] [Google Scholar]
- 19.Reuben SS, Steinberg RB, Klatt JL, Klatt ML. Intravenous regional anesthesia using lidocaine and clonidine. Anesthesiology. 1999;91:654–8. doi: 10.1097/00000542-199909000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Singelyn FJ, Gouvemeur JM, Robert A. A minimum dose of clonidine added to mepivacaine prolongs duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–50. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 21.Casati A, Magistris L, Fanelli G, Beccaria P, Cappelleri G, Aldegheri G, et al. Small-dose clonidine prolongs postoperative analgesia after sciatic-femoral nerve block with 0.75% ropivacaine for foot surgery. Anesth Analg. 2000;91:388–92. doi: 10.1097/00000539-200008000-00029. [DOI] [PubMed] [Google Scholar]
- 22.Duma A, Urbanek B, Sitzwohl C, Kreiger A, Zimpfer M, Kapral S. Clonidine as an adjuvant to local anaesthetic axillary brachial plexus block: a randomized, controlled study. Br J Anaesth. 2005;94:112–6. doi: 10.1093/bja/aei009. [DOI] [PubMed] [Google Scholar]
- 23.Adnan T, Elif AA, Ayşe K, Gülnaz A. Clonidine as an adjuvant for lidocaine in axillary brachial plexus block in patients with chronic renal failure. Acta Anaesthesiol Scand. 2005;49:563–8. doi: 10.1111/j.1399-6576.2005.00631.x. [DOI] [PubMed] [Google Scholar]
- 24.Brkovic B, Gardasevic M, Roganovic J, Jovic N, Todorovic L, Stojic D. Lidocaine+clonidine for maxillary infiltration anesthesia: Parameters of anesthesia and vascular effects. Int J Oral Maxillofac Surg. 2007;37:149–55. doi: 10.1016/j.ijom.2007.07.019. [DOI] [PubMed] [Google Scholar]


