Abstract
This study examined the association among caregivers’ five-factor personality traits and subjective health with particular emphasis on the role of two theoretically implicated mediators: multi-domain self-efficacy and caregiver strain. The sample comprised 536 informal caregivers (mean age = 62.9 years, SD = 19.9, 72% female, 98% White) of community-dwelling older adults with multiple functional impairments. Both physical health and mental health were negatively associated with neuroticism and positively associated with extraversion and conscientiousness. Agreeableness and openness were associated with better subjective mental health and physical health, respectively. Multiple mediation analyses indicated that self-efficacy mediated all observed associations between personality and subjective health, whereas caregiver strain selectively mediated the associations of neuroticism and agreeableness with mental health.
Keywords: five-factor model personality traits, subjective health, self-rated health, self efficacy, caregiver strain
As life expectancy lengthens, informal caregiving for parents, spouses, and other relatives has become an increasingly normative experience (Rosenthal, Matthews, & Marshall, 1989). Adult child caregivers typically enter the caregiving relationship in late middle age, when they are coming to terms with the first overt signs of their own aging, whereas spousal caregivers are simultaneously facing age-related challenges in themselves and in their loved one. Insights into the predictors and outcomes of the caregiving experience therefore contribute to our understanding of the aging process as a whole.
Although caring for a loved one can be empowering and rewarding (Koerner, Kenyon, & Shirai, 2009), recent meta-analyses document a considerable toll on caregivers’ physical and mental health (Pinquart & Sörensen, 2003, 2004, 2007; Vitaliano, Zhang, & Scanlan, 2003). In fact, caregiving has been considered as a prototypic example for the negative health consequences of chronic stress (Hooker, Monahan, Bowman, Frazier, & Shifren, 1998), and caregivers are sometimes described as the “hidden patients” (Fengler & Goodrich, 1979).
Nevertheless, there is considerable variability in individual experiences, and caregivers are not at equal risk for adverse health outcomes (Pinquart & Sörensen, 2007). Theoretical frameworks of caregiving-related stress (Lawton, Moss, Kleban, Glicksman, & Rovine, 1991; Pearlin, Mullan, Semple, & Skaff, 1990) have conceptualized such differences in terms of background and contextual factors (e.g., age and other demographic characteristics, caregiving duration), objective stressors (e.g., care recipients’ impairment and problem behavior), subjective appraisals of the stress-response (e.g., burden, strain), and resilience-promoting resources (e.g., coping, social support, and self-efficacy). Empirical studies guided by these models have found that a considerable portion of the variance in caregiving outcomes is linked to demographic characteristics such as caregiver age, socioeconomic status, sex, and ethnicity (for meta-analyses see Pinquart & Sörensen, 2005, 2006, 2007). Psychological characteristics of the caregiver, in contrast, are mostly discussed in terms of caregiving appraisals (e.g., caregiver strain) and outcomes (e.g., mental health and depression) but rarely considered as antecedents of the stress process.
One notable exception to this trend is a limited body of research examining the association of caregivers’ personality traits with their mental and physical health (e.g., Bookwala & Schulz, 1998; Campbell et al., 2008; Hooker, Monahan, Shifren, & Hutchinson, 1992; Kim, Duberstein, Sörensen, & Larson, 2005). However, the observed associations are inconsistent across samples and appear to be complex. As discussed below, seemingly contradictory results may be linked to methodological limitations, under-identification of mediators, and restrictions in sampling.
To address these concerns, the present study extends previous research by examining the relation between personality traits and caregivers’ subjective mental and physical health in a sample of long-term caregivers of physically impaired older adults. Specifically, we (1) use comprehensive and well-validated measures of personality and subjective health, (2) systematically compare and contrast effects across different aspects of personality and subjective health, (3) examine two theoretically implicated mediators: caregiver strain and multi-domain self-efficacy, and (4) examine relevant covariates including caregivers’ age and other demographic characteristics as well as care recipients’ mental and physical impairments.
Definitions
As a widely replicated model of personality dispositions, we adopt the five-factor structure of personality traits (Goldberg, 1990; Paunonen, Zeidner, Engvik, Oosterveld, & Maliphant, 2000). According to this model, personality can be comprehensively described along the broad dimensions of neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness.
With regard to caregiver’s health outcomes, previous research has used a variety of measures ranging from single-item ratings of subjective health to comprehensive assessments of objective physical status (Pinquart & Sörensen, 2007; Vitaliano, Zhang, & Scanlan, 2003). In the context of the present study, we focus on subjective health, which is thought to show stronger associations with personality than objective health assessments (Costa & McCrae, 1987) and was found to be a potent predictor of mortality (e.g., Benyamini & Idler, 1999). Following Ware and colleagues (McHorney, Ware, Lu, & Sherbourne, 1994), we adopt a broad differentiation between physical and mental aspects of subjective health.
Caregiver strain, defined as the negative psychological consequences of caring for an individual with mental or physical impairments (Hooker et al., 1998), is one of the most widely researched elements of the caregiver stress process. Following Pearlin et al. (1990) we adopt a broad conceptualization that encompasses worry and concern about the care recipients as well as feelings of overload and the impression of being trapped in one’s role as a caregiver.
Self-efficacy is defined as an individual’s belief in his or her capability to organize and execute the necessary actions to achieve a desired attainment (Bandura, 1997). Because caregiving-related stressors are thought to spill over into most aspects of life (Pearlin et al., 1990), we adopted a comprehensive assessment approach (Rodin & McAvay, 1992) that measures efficacy beliefs over a variety of domains ranging from basic health and safety to social relations.
Personality Traits and Subjective Health
Research in non-caregiving populations provides ample evidence for links between personality traits and subjective mental and physical health. The pattern of these associations differs systematically across the five-factors:
People who score high on neuroticism are characterized by negative emotions and feel easily overwhelmed by stressful experiences (e.g., Costa & McCrae, 1992; McCrae & Costa, 2003). With regard to subjective health, these characteristics translate into substantially worse physical and mental health (Duberstein et al., 2003; Jerram & Coleman, 1999; Kempen, Jelicic, & Ormel, 1997; Kempen et al., 1999; Löckenhoff, Sutin, Ferrucci, & Costa, 2008).
Extraversion is associated with high levels of activity, sociability, and a greater tendency to experience positive emotions (Costa & McCrae, 1992; McCrae & Costa, 2003). Not surprisingly, highly extraverted individuals appear to be in better mental health as evidenced by higher subjective well-being (Steel, Schmidt, & Shultz, 2008) and lower rates of depression (Jylha & Isometsa, 2006). Although several studies show links between extraversion and self-rated global health (Jerram & Coleman, 1999; Korotkov & Hannah, 2004), associations with physical health are less consistent across studies than for neuroticism.
Recent years have seen increasing interest in the role of the remaining three personality dimensions, with a particular emphasis on conscientiousness. Individuals who score high on this trait are self-disciplined and organized, which is linked to greater health-promoting behaviors (for a meta-analysis see Bogg & Roberts, 2004) and, in turn, better subjective and objective health, lower risk of cognitive impairment (Wilson, Schneider, Arnold, Bienias, & Bennett, 2007), and – ultimately – lower mortality (Friedman, 2000; Iwasa et al., 2008; Löckenhoff, Sutin et al., 2008; Taylor et al., 2009; Terracciano, Löckenhoff, Zonderman, Ferrucci, & Costa, 2008; Weiss & Costa, 2005). Highly conscientious individuals also report a sense of competence and confidence, and this may partially account for their apparently better mental health (Jerram & Coleman, 1999; Löckenhoff, Sutin et al., 2008).
Research on the health implications of openness and agreeableness is comparatively scarce, although the greater mental flexibility of open individuals may facilitate adjustment to novel situations and thus promote cognitive, emotional, and physical well-being (Duberstein et al., 2003; Jerram & Coleman, 1999; Steel, Schmidt, & Shultz, 2008; Duberstein et al., in press) as well as lower mortality (Iwasa et al., 2008; Taylor et al., 2009). Agreeableness primarily describes an interpersonal tendency towards altruism and a willingness to cooperate with others. Associations with physical health are therefore relatively small, although multiple studies have linked it to better mental health (Löckenhoff, Sutin et al., 2008; Steel, Schmidt, & Shultz, 2008).
As this brief review suggests, five-factor personality traits appear to be associated with subjective mental and physical health in the general population. However, it is not clear whether these findings extend to the special situation of caregivers. Recent studies suggest that the association between psychosocial characteristics and health depends on sample characteristics such as chronological age and contextual factors (Duberstein et al., 2003; Löckenhoff, C. E., Sutin, A. R., Ferrucci, L., & Costa, P. T., 2008; Quinn, Johnson, Poon, & Martin, 1999; Staudinger & Fleeson, 1996). The specific association of personality with subjective health in caregiver populations therefore warrants further examination.
Personality and Subjective Health Among Caregivers
On the one hand, being a caregiver could exacerbate the health risks or benefits of personality traits. For example, increased vulnerability to stressors among neurotic individuals may have more deleterious effects when confronting the chronic stressors of caregiving as compared to the more benign hassles of everyday life. Similarly, a conscientious person’s high levels of organization and confidence may be particularly beneficial when juggling the multiple demands of caregiving. On the other hand, caregiving-related demands may become so pervasive that their influence overshadows the advantages or disadvantages conveyed by personality traits. From this point of view, personality traits might matter less for subjective health among caregivers as compared to the general population.
So far, empirical evidence for the health implications of personality traits among caregivers remains relatively scarce. A search of the relevant literature including caregivers of older adults, cancer patients, and disabled adult children found only 18 publications based on 15 different samples. Only three of these samples assessed all of the five-factor dimensions (Hollis-Sawyer, 2003; Hooker, Frazier, & Monahan, 1994; Renzetti et al., 2001). This stands in stark contrast to hundreds of publications examining other correlates of caregiver health (Pinquart & Sörensen, 2007).
Within the limited literature, neuroticism, which was assessed in all of the 15 samples, has garnered the largest amount of attention. Among caregivers, high levels on this trait were found to be associated with negative emotional states and depression (Gallant & Connell, 2003; Jang, Clay, Roth, Haley, & Mittelman, 2004; Nijboer, Tempelaar, Triemstra, van den Bos, & Sanderman, 2001; Patrick & Hayden, 1999; Rabins, Fitting, Eastham, & Zabora, 1990), lower perceptions of caregiving-related benefits (Hollis-Sawyer, 2003; Kim et al., 2005), greater caregiver burden and distress (Markiewicz, Reis, & Gold, 1997; Reis, Gold, Gauthier, Andres, & Markiewicz, 1994; Renzetti et al., 2001), greater sensitivity to caregiving-related stressors (Bookwala & Schulz, 1998; Koerner, Kenyon, & Shirai, 2009; Koerner & Kenyon, 2007), maladaptive coping strategies (Hooker, Frazier, & Monahan, 1994; Patrick & Hayden, 1999), worse subjective mental health (Hooker et al., 1992; Hooker et al., 1998), worse subjective physical health (Hooker et al., 1992; Monahan & Hooker, 1995; Reis et al., 1994), and fewer health promoting behaviors (Gallant & Connell, 2003).
Much less is known about the remaining personality dimensions of the five-factor model. Measures of extraversion were available for 9 of the 15 samples, and findings suggest that more extraverted caregivers exhibit lower negative emotions and depression (Nijboer et al., 2001; although see also Kim et al., 2005; Rabins et al., 1990), more adaptive coping strategies (Hooker, Frazier, & Monahan, 1994), more benefit-finding (Hollis-Sawyer, 2003; Koerner, Kenyon, & Shirai, 2009), lower sensitivity to caregiving-related stressors (Koerner & Kenyon, 2007), lower burden and strain (Markiewicz, Reis, & Gold, 1997), and better mental and physical health (Hooker et al., 1992; Reis et al., 1994; although see also Renzetti et al., 2001).
Caregivers’ levels of conscientiousness (assessed in five of the samples) were associated with more adaptive coping strategies (Hooker, Frazier, & Monahan, 1994), more caregiving-related benefit-finding (Hollis-Sawyer, 2003; although see also Koerner, Kenyon, & Shirai, 2009), a better relationship with the care recipient (Hollis-Sawyer, 2003; Koerner, Kenyon, & Shirai, 2009), lower sensitivity to care-related stressors (Koerner & Kenyon, 2007), and fewer chronic health conditions (Hooker et al., 1992). However, two studies failed to find any associations between conscientiousness and caregiving-related outcomes (Markiewicz, Reis, and Gold, 1997; Renzetti et al., 2001).
Finally, higher levels of agreeableness (assessed in five samples) were found to be associated with less maladaptive coping (Hooker, Frazier, & Monahan, 1994), a better relationship with the care recipient (Hollis-Sawyer, 2003), and more benefit-finding (Koerner, Kenyon, & Shirai, 2009), whereas higher levels of openness (included in four samples) were found to be associated with more positive perceptions of the caregiving relationship and caregiving-related growth (Hollis-Sawyer, 2003). Only a few studies (Hooker et al., 1992; Rabins et al., 1990; Renzetti et al., 2001) examined the effects of openness and agreeableness on subjective physical health among caregivers. None of them reported any significant effects, although given the small sample sizes (ns < 60) the lack of findings might have been attributable to a lack of power.
Overall, the observed associations between caregiver personality and various health outcomes appear to be fairly consistent with those reported for the general population. Higher neuroticism is linked to worse mental and physical health, greater extraversion and conscientiousness are linked to better mental and physical health, and agreeableness and openness show weak associations. However, many inconsistencies remain.
In part, these inconsistencies can be explained by methodological concerns. The available samples are very diverse (e.g., dementia caregivers vs. caregivers of adult children with developmental disabilities), and many are small in size: half of the caregiving-related studies cited above are based on samples with ns < 100. Further, measures of personality and health vary widely across investigations. Some of the measures relied on single-item health ratings (Bookwala & Schulz, 1998), and others differ in the theoretical conceptualization of the variables under investigation. Extraversion, for example, is conceptualized quite differently in the model proposed by Eysenck (Eysenck & Eysenck, 1975; used in Nijboer et al., 2001) as compared to the model proposed by McCrae and Costa (McCrae & Costa, 2003; used in Hooker, Frazier, & Monahan, 1994). Also, studies differ in their attention to relevant covariates including caregivers’ demographic characteristics as well as care recipients’ levels of impairment. Chronological age, for instance, was found to affect the association between personality and subjective health in non-caregiving populations (e.g., Duberstein et al., 2003; Quinn et al., 1999), but similar effects among caregivers remain to be explored.
In addition to the methodological concerns outlined above, other open questions remain. Perhaps the most important of these issues concerns the underlying mechanisms by which caregiver personality translates into health outcomes.
What Mediates the Relationship Between Personality and Caregivers’ Subjective Health?
Theoretical models of the caregiver stress process (Lawton et al., 1991; Pearlin et al., 1990) point towards several possible mediators of the observed links between personality and subjective health including coping strategies, social support, and differences in stress appraisal.
So far, only a few studies have empirically examined such effects (Gallant & Connell, 2003; Hooker et al., 1992; Hooker et al., 1998; Kim et al., 2005; Koerner & Kenyon, 2007; Patrick & Hayden, 1999). With regard to mental health outcomes, these studies consistently suggest that neuroticism has not only direct effects on mental health but also indirect effects via perceived stress and burden. In addition, Gallant and Connell (2003) found an indirect effect of neuroticism on poorer mental health via health behaviors, and Patrick and Hayden (1999) found an indirect effect via coping strategies. In contrast, two studies examining the role of social support (Hooker et al., 1998; Kim et al., 2005) found little evidence that social support mediates the link between personality and mental health.
Even less is known about mediators of the relationship between caregiver personality and physical health. Findings by Hooker et al. (1998) suggest that effects of caregiver neuroticism and optimism are mediated by stress. Further, Koerner and Kenyon (2007) found that neuroticism, extraversion, and conscientiousness are associated with caregivers’ physical symptoms in response to daily fluctuations in caregiving stressors.
Overall, previous research on the role of mediators is generally consistent with existing theoretical models of the caregiver stress process (e.g., Pearlin et al., 1990). However, most studies focused on a subset of personality traits (typically including neuroticism) and were limited to mental health outcomes. This is problematic because mediators of health effects might differ for mental versus physical health and across specific personality traits. Also, even though coping, health behaviors, and strain were found to mediate the association between neuroticism and mental health, significant direct effects remained in each of the studies (Gallant & Connell, 2003; Hooker et al., 1992; Hooker et al., 1998; Kim et al., 2005; Patrick & Hayden, 1999). This suggests that there may be additional mediators that were not considered in previous work.
In the search for potential mediators, it is important to acknowledge that personality traits may not only influence sensitivity towards stressors but also convey resources that promote resilience (McCrae & Costa, 2003). One promising candidate in this regard is self-efficacy. Theoretically, self-efficacy perceptions are thought to influence caregiver’s appraisal of caregiving demands (e.g., care recipients’ impairment levels) and thus influence responses to the caregiving experience (Martire & Schulz, 2000). In support of this notion, self-efficacy beliefs have been linked to caregivers’ mental and physical health (Fortinsky, Kercher, & Burant, 2002; Rabinowitz, Mausbach, Thompson, & Gallagher- Thompson, 2007). Importantly, self-efficacy beliefs are also associated with personality traits including neuroticism (e.g., Judge, Erez, Bono, & Thoresen, 2002) and conscientiousness (Lee & Klein, 2002). Moreover, self-efficacy was found to mediate the relationship between personality traits and health-related outcomes such as weight management (Hayashi et al., 2008). Although these findings implicate self-efficacy as a potential mediator of the link between personality traits and caregiver health, there have been no empirical tests of this association.
The Present Study
In summary, previous research indicates that personality traits are linked to caregivers’ mental and physical health. However, a deeper understanding of this association is hampered by a scarcity of studies, sampling issues, measurement concerns, and limited exploration of relevant mediators. To address some of the gaps in the literature, the present study examined the association among personality traits and subjective health in a sample of more than 500 long-term caregivers of older adults with physical disabilities. To address the shortcomings of assessment tools used in previous work, we used well-validated and comprehensive measures of five-factor personality traits [i.e., the NEO Personality Inventory Revised (NEO-PI-R), Costa & McCrae, 1992] and subjective mental and physical health (i.e., the SF-36, Ware, Snow, Kosinski, & Gandek, 1993). We also assessed two theoretically implicated mediators, caregiver strain and multi-domain self-efficacy, and examined the extent to which they account for the observed pattern of associations.
Based on the existing literature, we expected that subjective mental and physical health among caregivers would be negatively related to neuroticism and positively related to extraversion and conscientiousness. Few studies have examined the health effects of agreeableness and openness among caregivers. However, based on the pattern of findings in the general population (e.g., Löckenhoff, Sutin et al., 2008), we expected to find associations between higher agreeableness and better mental health and between higher openness and better mental and physical health.
We also predicted that associations between caregivers’ personality traits and their subjective health would be mediated by multi-domain self-efficacy and caregiver strain. Specifically, we expected that caregiver strain, which captures emotional responses to the caregiving role, would be particularly relevant in predicting subjective mental health. We further expected that caregiver strain would be most relevant for mediating the effects of extraversion and neuroticism (because these traits encompass dispositional aspects of emotional reactivity) and agreeableness (which captures interpersonal tendencies and may matter for people’s adjustment to the caregiving role). In contrast, we expected that multi-domain self-efficacy, which captures people’s belief in their ability to manage life’s challenges, would equally predict mental and physical health and would mediate the effects of conscientiousness (which is characterized by a confident and deliberate approach to problem solving) and neuroticism (which is characterized by feelings of helplessness and vulnerability).
Finally, we explored the role of covariates that were previously linked to caregiver health, including caregiver demographics (i.e., age, sex, and education, Pinquart & Sörensen, 2006, 2007) and care recipients’ physical and cognitive impairment (Bookwala & Schulz, 1998; Pinquart & Sörensen, 2007). Because previous research suggests that associations between personality and subjective health may differ by age (Duberstein et al., 2003; Quinn et al., 1999), supplemental analyses examined the role of age as a moderator.
Method
Participants
The present analyses are based on dyads of caregivers and care recipients drawn from the Medicare Primary and Consumer-Directed Care Demonstration (Medicare PCDC), a randomized, controlled trial of primary and consumer-directed care that was conducted from 1998 to 2002 (Meng, Friedman, Wamsley, Mukamel, & Eggert, 2005).1 Data were collected at multiple sites in Ohio, New York State, and West Virginia.
To be eligible for initial enrollment, care recipients had to be community-dwelling, enrolled in Medicare Part A and Part B, and report needing or receiving help with at least two activities of daily living (ADLs) or at least three instrumental activities of daily living (IADLs). They also had to present with recent health service utilization (i.e., hospital, nursing home, home healthcare, or emergency department).
Caregivers were selected based on an adapted version of the rules for identifying the primary informal caregiver used for the Medicare Alzheimer’s Disease Demonstration (Newcomer, Yordi, DuNah, Fox, & Wilkinson, 1999). For further details regarding eligibility criteria and recruitment strategies see Friedman, Wamsley, Liebel, Saad, & Eggert (2009).
Medicare PCDC participants were followed over a 24-month period. Comprehensive measures of caregiver personality traits, subjective health, strain, and multi-domain self-efficacy, which are essential for the present study, were assessed at follow-up appointments in a two-month period between month 20 and month 22 of the study and treated as contemporaneous indicators. Thus, all caregivers in the present study had performed their role for at least 20 months.
Of the 1,176 dyads who participated in the baseline assessment, 491 (41.8%) were lost by the 24-month follow-up. Comprehensive attrition analyses are presented in Weiss & Costa (2005) and suggest that attrition was largely attributable to death or institutionalization of the care recipient. Among the remaining 685 dyads, 536 (78.2%) had complete data for the main variables of interest in the present study (i.e., caregiver personality traits, subjective health, strain, and multi-domain self-efficacy). Caregivers who participated in the follow-up but were not included in the present analyses because of missing data on the core variables did not differ in sex (65% vs.72% female, χ2 = 2.49, n.s.) or age (M = 63.32, SD = 13.18 vs. M = 62.86, SD = 13.65 t = 0.35, n.s.), but they were less likely to be spouses (30% vs. 42%, χ2 = 6.77, p < 0.01).
Measures
Caregiver personality
Caregiver personality was assessed with the NEO Personality Inventory Revised (NEO-PI-R, Costa & McCrae, 1992). Based on the five-factor model of personality (McCrae & Costa, 2003), its 240 items consist of short, self-descriptive statements answered on a five-point Likert scale. Responses are considered invalid if participants report that they did not respond honestly and accurately to all items. The NEO-PI-R provides scores for the five basic personality dimensions or factors (neuroticism, extraversion, openness, agreeableness, and conscientiousness) as well as 30 facet scores, with each factor composed of six individual facets. For the present analyses, factor scores for each of the five traits were computed as a weighted combination of all 30 facet scales (for the specific formulas see Costa & McCrae, 1992). The resulting scores are more orthogonal and have better external validity than simple summary scores (Costa & McCrae, 1992). Factor scores were t-standardized based on U.S. combined sex norms (Costa & McCrae, 1992).
The NEO-PI-R has been used across more than 50 cultures worldwide (McCrae, Terracciano, & The Personality Profiles of Cultures Project, 2005). For evidence on convergent and discriminant validity see McCrae, Terracciano, & The Personality Profiles of Cultures Project (2005).
Caregiver subjective health
We assessed subjective mental and physical health with the SF-36 Health Survey (Ware et al., 1993). The items of this measure use several different response formats ranging from binary responses to six-item Likert scales. Responses yield four mental health scales (vitality, social functioning, role-emotional, and mental health) and four physical health scales (physical functioning, role physical, bodily pain, and general health). For the present analyses, we computed summary scores for physical and mental health which were t-standardized using U.S. Norms (Ware, Kosinski, & Keller, 1994). Like the NEO-PI-R factor scores, each of these summary scores combines weighted information from all eight scales to remove variance attributable to physical health from the mental score and vice versa.
The SF-36 is one of the most widely used measures of subjective health and is endorsed by the United States Food and Drug Administration for the purpose of monitoring patient-reported outcomes (Ware, Kosinski, & Keller, 1994). For information on psychometric characteristics see Ware, Kosinski, & Keller (1994), and for evidence on validity see McHorney et al. (1994).
Caregiver strain
Caregiver strain was measured using 21 items adapted from Pearlin et al.’s measurement model of the caregiver stress process (Pearlin et al., 1990). Specifically, the items were drawn from measures of overload (e.g., “I have more things to do than I can handle”), worry and strain (e.g., “I feel more and more tense as the day goes on”), and role captivity (e.g., “I wish I could just run away”; Leitsch, Zarit, Townsend, & Greene, 2001). All items were answered on four-point Likert-scales from “never” to “all of the time.” We first computed the three separate scales proposed by Leitsch et al. (2001) but found them to be strongly intercorrelated (mean r = 0.54). For the present analyses, we therefore combined all items into a single scale with high internal consistency (Cronbach’s α = 0.89).
Caregiver multi-domain self-efficacy
Multi-domain self-efficacy was assessed with a measure by Rodin and McAvay (1992), which consists of eight Likert-type items assessing an individual’s self-efficacy across the following domains: health, transportation, relationships with family, financial situation, safety, relationships with friends, living arrangements, and productivity. The health item, for example, was worded as follows: “You’ve been feeling this month that keeping healthy depends on things that you can do.” Answers were provided on a four-point scale from “strongly disagree” to “strongly agree.” A ninth item assessing self-efficacy about the relationship with one’s significant other was excluded because not all caregivers were currently in a relationship. In the present sample, this scale showed moderate levels of internal consistency (Cronbach’s α = 0.60).
Care recipient’s physical impairment
Assessments of ADL impairments were drawn from the Medicare Health of Seniors Survey, and assessments of IADL impairments were drawn from Medicare’s OASIS survey (Shaughnessy, Crisler, & Schlenker, 1997). ADLs included walking, transferring, dressing, eating/feeding, toileting, grooming, and bathing. IADLs included meal preparation, ordinary housework, managing finances, managing medications, telephone use, shopping, and transportation. Difficulty performing the activities (“no difficulty” versus “some difficulty” or “great difficulty”) was assessed 22 months into the study. Previous research indicates that personality may influence caregivers’ reporting of care recipients’ impairment status (Bookwala & Schulz, 1998). It is therefore important to note that caregivers were not the main source of information regarding impairment levels. Instead, trained interviewers integrated information provided by care recipient and caregiver as well as cues from the recipients’ home environment to arrive at a final determination about impairment status. ADL and IADL scores were highly correlated (r = 0.69, p < 0.01). We therefore computed a single index summarizing the number of ADL and IADL impairments for the purpose of mediation analyses. To address concerns about skewness, we used a quartile split before inclusion in further analyses.
Care recipient’s mental impairment
As a cognitive screen, care recipients were asked to recall three words—book, watch, table—that had been presented five minutes earlier. Importantly, although this measure represents the short-term memory component of the widely used Mini Mental State Examination (Folstein, Folstein, & McHugh, 1975), it has not been previously validated in this format and cannot yield a formal diagnosis of dementia. For the present purpose, it nevertheless provides a useful distinction between care recipients with higher and lower levels of cognitive functioning. Because of skewness, we used a dichotomization between those care recipients who recalled all three items and those who recalled fewer than three items.
Data Screening and Statistical Analyses
All caregiver-care recipient dyads had complete data on the core variables of personality traits, subjective health, caregiver multidomain self-efficacy, and caregiver strain. As shown in Table 1, there were some missing data on the covariates, particularly with regard to care recipient characteristics. Because missing data status was unrelated to the core outcome variables of the present study, we did not attempt to estimate missing data but simply excluded those dyads from analyses controlling for covariates. Thus, degrees of freedom are somewhat lower for these analyses.
Table 1.
Participant Characteristics
| Variable | Mean/% | SD | Minimum | Maximum | n |
|---|---|---|---|---|---|
| Caregiver demographics | |||||
| Age | 62.9 | (13.7) | 22.0 | 96.0 | 532 |
| Education level | 3.6 | (1.2) | 1.0 | 6.0 | 535 |
| Sex (% female) | 72% | 533 | |||
| Relationship status (% spouse) | 42% | 535 | |||
| Ethnicity (% White) | 98% | 536 | |||
| Care recipients’ impairment | |||||
| ADL/IADL impairment | 2.5 | 1.1 | 1 | 4 | 470 |
| Short-term memory impairment | 15.5% | — | — | — | 476 |
| Caregiver characteristics | |||||
| Neuroticism | 51.7 | (9.5) | 26.0 | 89.5 | 536 |
| Extraversion | 48.1 | (8.6) | 17.8 | 75.6 | 536 |
| Openness | 46.0 | (9.8) | 16.5 | 81.2 | 536 |
| Agreeableness | 54.0 | (9.7) | 9.4 | 80.8 | 536 |
| Conscientiousness | 49.3 | (9.8) | 12.4 | 86.0 | 536 |
| Self-efficacy | 2.8 | (0.3) | 1.6 | 4.0 | 536 |
| Caregiver strain | 2.0 | (0.4) | 1.1 | 3.4 | 536 |
| SF-36 physical | 44.9 | (11.5) | 12.2 | 66.8 | 536 |
| SF-36 mental | 50.3 | (10.0) | 13.1 | 69.8 | 536 |
Note. Education levels 1 = less than high school, 2 = some high school, 3 = high school graduate, 4 = some college, 5 = college degree, 6 = more than college degree. ADL/IADL impairments are split into quartiles.
Given the moderately large size of the sample, even slight deviations from normality were likely to reach statistical significance using Kolmogorov-Smirnov’s test. Following recommendations by Kline (2005), we therefore examined the absolute values of standardized skewness and kurtosis and found that they were well within the limits (i.e., skewness < 3.0 and kurtosis < 10) found to be acceptable in simulation studies (Curran, West, & Finch, 1996). For all variables in the model, the absolute values for skewness were below 2, and absolute values for kurtosis were below 4.
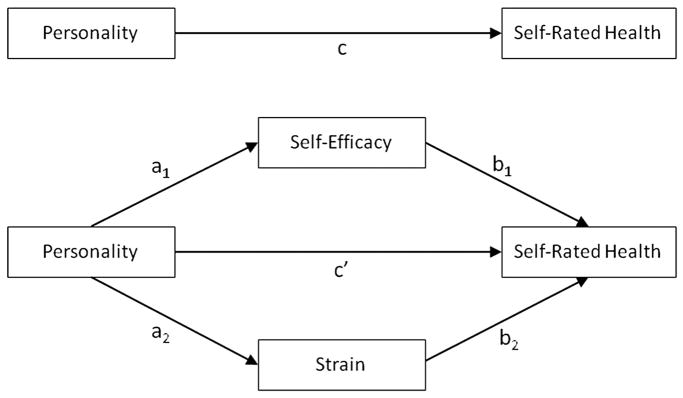
Predictions regarding the specific pattern of associations between personality and subjective health were tested using correlational analyses. Moderated regression analyses examined the role of chronological age as a moderator of personality-health links. Predictions regarding the mediating role of caregiver strain and multi-domain self-efficacy were tested via multiple mediation analyses using the statistical software package SPSS and following the model depicted in Figure 1. Separate analyses were conducted for each of the personality traits and for physical versus mental health as the dependent variables. We focus our presentation of indirect effects on traditional estimates based on normal theory and Sobel tests (Baron & Kenny, 1986). Complementary analyses report findings based on bootstrapping (Preacher & Hayes, 2008), a nonparametric approach to effect-size estimation that is robust to deviations from normality and yields lower Type 1 error rates (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). Supplemental analyses examined the influence of relevant covariates on patterns of mediation.
Figure 1.
Schematic for proposed mediation models.
Results
Descriptive Analyses
Table 1 provides descriptive characteristics for the present sample. Although caregivers spanned a wide age range, the majority of them were in late middle age or early old age and almost three quarters were female. Forty-two percent were spouses; the remainder were other relatives (predominantly adult children) or friends. This pattern of characteristics is fairly typical for caregivers in the United States (Hong, 2010). Further, consistent with the population distribution of the Medicare PCDC (19 counties in New York State, West Virginia, and Ohio), caregivers in the present sample were mostly white and not educated beyond high school.
Compared to U.S. norms of personality traits, caregivers scored somewhat lower on openness and higher on agreeableness, but they did not differ on the remaining traits (see Table 1). With regard to SF-36 scores, subjective mental health was average whereas subjective physical health was markedly lower than in the U.S. normative sample, indicating that some of the caregivers were facing some physical health concerns themselves. Care recipients had high rates of ADL/IADL impairment (M = 6.78, SD = 3.62, on a 14-point scale), and one in eight showed evidence of cognitive impairment.
Correlational Analyses
Correlations of caregivers’ personality traits with ratings of subjective health as well as the proposed mediators and covariates are reported in Table 2.
Table 2.
Correlations Among Personality Traits, Subjective Health, Proposed Mediators, and Relevant Covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Caregiver demographics | |||||||||
| 1. Age | |||||||||
| 2. Education | −0.17** | ||||||||
| 3. Female | −0.27** | 0.02 | |||||||
| Care recipients’ impairment | |||||||||
| 4. ADL/IADL | 0.06 | 0.06 | 0.01 | ||||||
| 5. Memory impairment | 0.01 | 0.09* | 0.01 | 0.51** | |||||
| Caregiver characteristics | |||||||||
| 6. Self-efficacy | −0.19** | 0.18** | −0.06 | −0.13** | −0.12** | ||||
| 7. Strain | 0.07 | 0.02 | 0.10* | 0.32** | 0.18** | −0.35** | |||
| 8. SF-36 physical | −0.29** | 0.23** | 0.06 | 0.05 | 0.16** | 0.31** | −0.20** | ||
| 9. SF-36 mental | 0.08 | 0.02 | −0.03 | −0.06 | −0.01 | −0.40** | −0.35** | 0.14** | |
| 10. Neuroticism | −0.08 | −0.09* | 0.14** | 0.01 | −0.03 | −0.32** | 0.30** | −0.17** | −0.44** |
| 11. Extraversion | −0.19** | 0.09* | 0.13** | −0.05 | −0.04 | 0.15** | −0.04 | 0.13** | 0.11* |
| 12. Openness | −0.22** | 0.38** | 0.16** | 0.01 | 0.05 | 0.15* | 0.05 | 0.14** | 0.03 |
| 13. Agreeableness | 0.15** | −0.02 | 0.18** | 0.02 | −0.06 | 0.09* | −0.10* | −0.06 | 0.13** |
| 14. Conscientiousness | 0.03 | 0.18** | 0.03 | −0.01 | 0.01 | 0.17** | −0.02 | 0.18** | 0.16** |
Note. For dichotomous variables (sex, memory impairment) point-biserial correlations are reported.
p < 0.05.
p < 0.01.
Associations between personality traits and subjective health were largely consistent with our hypotheses. As expected, both subjective physical health and subjective mental health were negatively associated with neuroticism and positively associated with extraversion and conscientiousness, whereas agreeableness was associated with subjective mental health but not with physical health. Openness, in contrast, was found to be associated with better physical but not mental health among caregivers.
The proposed mediators (i.e., caregivers’ multi-domain self-efficacy and caregiver strain) were associated with both personality traits and subjective health. Self-efficacy was negatively associated with neuroticism and positively associated with the remaining personality traits, whereas caregiver strain was positively associated with neuroticism and negatively associated with agreeableness. In addition, high multi-domain self-efficacy and low caregiver strain showed moderate associations with better subjective mental and physical health.
Several of the covariates showed significant associations with the variables included in the mediation model. Consistent with the literature on demographic differences in personality traits (Löckenhoff, Terracciano et al., 2008; Roberts, Walton, & Viechtbauer, 2006; Terracciano, McCrae, Brant, & Costa, 2005), age was negatively associated with extraversion and openness and positively associated with agreeableness; females scored higher on all traits except conscientiousness, and more educated individuals scored markedly higher on openness and conscientiousness and somewhat higher on neuroticism and extraversion. In addition, subjective physical health and multi-domain self-efficacy were negatively associated with age and positively associated with education, whereas subjective mental health and caregiver strain were unrelated to demographic characteristics. Consistent with theoretical models of the caregiver stress process (Pearlin et al., 1990), care recipients’ impairments were associated with higher caregiver strain and lower multi-domain self-efficacy. Because of their associations with personality, subjective health, and the proposed mediators, demographic covariates and care recipients’ impairment levels were considered in subsequent mediation analyses.
Supplemental analyses examined whether chronological age moderated the association between personality traits and indicators of mental and physical health. None of the moderation effects reached statistical significance.
Mediation Analyses
To further explore the complex association among caregivers’ personality, subjective health, and the proposed mediators, we conducted mediation analyses following the model depicted in Figure 1. Analyses were limited to those combinations of variables that showed significant intercorrelations (see Table 2) and thus met a basic prerequisite for mediation. Therefore, caregiver strain was only included as a potential mediator in analyses involving neuroticism and agreeableness, openness was selectively examined as a predictor of physical health, and agreeableness was selectively examined as a predictor of mental health.
Tables 3 and 4 show the results of multiple mediation analyses for physical and mental health, respectively. Results in these tables are based on normal theory and use a regression approach. Following Baron and Kenny’s (1986) four-step process, step 1 predicts subjective health based on personality (c paths), step 2 predicts potential mediators based on personality (a paths), step 3 predicts subjective health based on each of the mediators while including personality as a predictor in the same equation (b paths), and step 4 predicts subjective health based on personality while including the mediators in the same equation (c′ paths). Note that steps 3 and 4 were tested in the same regression equations. The significance of the indirect effects (ab paths) was determined using Sobel tests. Supplemental analyses using a non-parametric bootstrapping approach advocated by Preacher and Hayes (Preacher & Hayes, 2008) yielded a comparable pattern of results. All of the proposed mediation models reached statistical significance, although the percentage of variance explained was somewhat higher for mental health (16–29%) than for physical health (around 10%).
Table 3.
Subjective Physical Health: Multiple Mediation Analyses
| Neuroticism | Extraversion | Openness | Conscientiousness | |||||
|---|---|---|---|---|---|---|---|---|
| Model | ||||||||
| F(3, 531) | 21.345 | 30.262 | 31.019 | 33.910 | ||||
| Adjusted R2 | 0.103 | 0.100 | 0.101 | 0.101 | ||||
| p | <0.001 | <0.001 | <0.001 | <0.001 | ||||
|
| ||||||||
| Effects (paths in model) | b | SE | b | SE | b | SE | b | SE |
|
| ||||||||
| Personality to mediators | ||||||||
| Personality to self-efficacy (a1) | −0.011** | 0.001 | 0.006** | 0.002 | 0.005** | 0.001 | 0.006** | 0.001 |
| Personality to strain (a2) | 0.012** | 0.002 | — | — | — | — | — | — |
| Mediators to mental health | ||||||||
| Self-efficacy to physical health (b1) | 0.920** | 0.160 | 1.050** | 0.15 | 1.047** | 0.147 | 1.014** | 0.147 |
| Strain to physical health (b2) | −0.270* | 0.134 | — | — | — | — | — | — |
| Indirect personality to physical health | ||||||||
| Self-efficacy (ab1) | −0.010** | 0.002 | 0.006** | 0.002 | 0.005** | 0.002 | 0.006** | 0.002 |
| Strain (ab2) | −0.003 | 0.002 | — | — | — | — | — | — |
| Total personality to physical health (c) | −0.020** | 0.005 | 0.017** | 0.006 | 0.016** | 0.005 | 0.021** | 0.005 |
| Direct personality to physical health (c′) | −0.007 | 0.005 | 0.011 | 0.006 | 0.011* | 0.005 | 0.015** | 0.005 |
Note. Agreeableness is not included because correlational analyses revealed no statistically significant association with subjective physical health.
p < 0.05.
p < 0.01.
Table 4.
Subjective Mental Health: Multiple Mediation Analyses
| Neuroticism | Extraversion | Agreeableness | Conscientiousness | |||||
|---|---|---|---|---|---|---|---|---|
| Model | ||||||||
| F(3, 531) | 72.677 | 50.635 | 48.418 | 53.143 | ||||
| Adjusted R2 | 0.287 | 0.157 | 0.210 | 0.163 | ||||
| p | <0.001 | <0.001 | <0.001 | <0.001 | ||||
|
| ||||||||
| Effects (paths in model) | b | SE | b | SE | b | SE | b | SE |
|
| ||||||||
| Personality to mediators | ||||||||
| Personality to self-efficacy (a1) | −0.011** | 0.001 | 0.006** | 0.002 | 0.003* | 0.001 | 0.006** | 0.001 |
| Personality to strain (a2) | .012** | 0.002 | — | — | −0.004* | 0.002 | — | — |
| Mediators to mental health | ||||||||
| Self-efficacy to mental health (b1) | .787** | 0.135 | 1.303** | 0.135 | 1.027** | 0.138 | 1.273** | 0.135 |
| Strain to mental health (b2) | −0.501** | 0.113 | — | — | −0.665** | 0.117 | — | — |
| Indirect personality to mental health | ||||||||
| Self-efficacy (ab1) | −0.009** | 0.002 | 0.007** | 0.002 | 0.003* | 0.002 | 0.007** | 0.002 |
| Strain (ab2) | −0.006** | 0.002 | — | — | 0.003* | 0.001 | — | — |
| Total personality to mental health (c) | −0.050** | 0.004 | 0.014* | 0.005 | 0.015** | 0.005 | 0.018** | 0.005 |
| Direct personality to mental health (c′) | −0.035** | 0.005 | 0.006 | 0.005 | 0.009* | 0.004 | 0.011* | 0.004 |
Note. Openness is not included because correlational analyses revealed no statistically significant association with subjective mental health.
p < 0.05.
p < 0.01.
With regard to the association between personality traits and physical health (Table 3), caregivers’ multi-domain self-efficacy emerged as a significant mediator for neuroticism, extraversion, openness, and conscientiousness (see significant ab paths). As indicated by the non-significant c′ paths, we found full mediation for the effects of neuroticism and extraversion on physical health. For openness and conscientiousness, the c′ paths remained significant indicating only partial mediation. Caregiver strain, in contrast, did not emerge as a significant mediator.
Regarding the association between personality traits and mental health, multi-domain self-efficacy was found to be a significant mediator for neuroticism, extraversion, agreeableness, and conscientiousness. Caregiver strain significantly mediated the effects of neuroticism and agreeableness on mental health. Multi-domain self-efficacy fully mediated the effects of extraversion on subjective mental health. For neuroticism, agreeableness, and conscientiousness we found only partial mediation.
In a final step, we included caregivers’ demographic characteristics as well as indicators of care recipients’ impairment as covariates in the mediation analyses. Under these circumstances, multi-domain self-efficacy was no longer a significant mediator of the associations of extraversion with mental and physical health. All other mediation effects remained significant.
Discussion
The present study contributes to the scarce literature on personality-health links among caregivers by systematically examining the role of two theoretically implicated mediators: caregiver strain and multi-domain self-efficacy. In addition to replicating the mediating role of strain (Gallant & Connell, 2003; Hooker et al., 1992; Hooker et al., 1998), our study is the first to demonstrate a significant role of self-efficacy. We also add to the small body of studies that examined the full range of five-factor traits among caregivers (Hollis-Sawyer, 2003; Hooker, Frazier, & Monahan, 1994; Renzetti et al., 2001), and our study is the first to use comprehensive and well-validated measures of both personality traits and subjective health. Finally, the present sample is about 50% larger than those used in previous studies and fairly homogenous in demographic structure and caregiving experience, which addresses concerns about power and sample heterogeneity in prior research.
Overall, the observed associations between caregiver personality and subjective health converge with those found in the general population. Consistent with prior studies, mental and physical health were positively associated with extraversion and negatively associated with neuroticism. Our findings further suggest that whereas conscientiousness is linked to both mental and physical aspects of subjective health, agreeableness and openness are selectively linked to mental and physical health, respectively. In terms of effect size, the observed strength of the associations resembles those reported by Löckenhoff and colleagues (Löckenhoff, Sutin, et al., 2008) for a general population sample drawn from the Baltimore Longitudinal Study of Aging, with moderate effects for neuroticism and conscientiousness but fairly small effects for the remaining traits. In contrast to prior studies, however, age did not moderate the associations between personality and subjective health. Conceivably, the shared caregiving responsibilities in the present sample may have served as a homogenizing force that overshadowed any differences across age groups.
Consistent with our hypotheses, both caregiver strain and multi-domain self-efficacy were found to play a role in mediating the observed associations between personality and health. In fact, the role of multi-domain self-efficacy was much more pervasive than we had hypothesized. It mediated not only the effects of neuroticism and conscientiousness but every single significant association between personality traits and subjective health that was observed in the correlational analyses. This suggests that one reason why personality traits matter for caregivers’ mental and physical health is that they influence caregivers’ perceptions of their ability to successfully manage the challenges of everyday life. With regard to specific personality dimensions, efficacy beliefs may reflect emotion-regulatory skills, dispositional mood, and energy levels (as captured by neuroticism and extraversion), but also interpersonal skills (agreeableness), organization and self-management (conscientiousness), as well as the ability to accommodate to novel situations (openness).
In this context, it is important to note that we used a comprehensive self-efficacy scale (Rodin & McAvay, 1992) that spans multiple domains of functioning ranging from health and safety to finances and interpersonal relationships. Given the all-encompassing influence of the caregiving experience on virtually all aspects of life (Pearlin et al., 1990), this approach may be at least as relevant for understanding caregiver well-being as the use of caregiving-specific self-efficacy scales (Fortinsky, Kercher, & Burant, 2002; Rabinowitz et al., 2007). Consistent with the view that the multi-domain efficacy measure captures some caregiving-related variance, we observed a moderate negative association with caregiver strain in the present sample. Nevertheless, caregiving-specific self-efficacy measures are of course better suited to capture caregivers’ responses to the unique challenges of caring for a dependent loved one. Ideally, future research should include multidomain and caregiving-specific assessments of both strain and self-efficacy to explore their relative association with caregivers’ personality traits and health-related outcomes. At a more general level, the pronounced association between multi-domain self-efficacy and caregivers’ subjective health highlights the need for further research that investigates protective and resilience-promoting factors in caregiving contexts.
In contrast to the pervasive role of multi-domain self-efficacy, caregiver strain selectively mediated the association of neuroticism and agreeableness with subjective mental health. This suggests that the stress response and associated detriments in mental health are not only positively associated with caregivers’ general propensity to experience negative emotions (i.e., neuroticism), but also negatively associated with altruistic and cooperative tendencies (i.e., agreeableness). Contrary to our hypotheses, caregiver strain did not mediate the effects of extraversion on mental health. This could be attributable to the fact that extraversion is focused on positive emotions whereas caregiver strain is selectively focused on negative emotional responses.
Importantly, only three of the eight mediation models were indicative of full mediation. The remaining models merely suggested partial mediation. Thus, although multi-domain self-efficacy and strain appear to explain some of the associations of personality traits with caregiver health, they do not fully account for the observed findings. Also, as in previous studies (e.g., Monahan & Hooker, 1995; Hooker et al., 1998; Bookwala & Schulz, 1998), the percentage of variance in caregiver health that was explained by personality traits was only small to moderate in size. To address this issue, future research should include additional mediators that have been implicated in prior research (including coping and health behaviors; Gallant & Connell, 2003; Hooker et al., 1992; Hooker et al., 1998; Kim et al., 2005; Patrick & Hayden, 1999) and identify previously overlooked variables (e.g., resilience-related concepts such as mindfulness) that may play a mediating role as well.
In interpreting the results of this study, several important limitations need to be acknowledged. First, our data are cross-sectional in nature and do not allow for the testing of temporal relationships or causal hypotheses. So far, only a handful of studies have examined longitudinal associations between personality traits and caregiver health (Jang et al., 2004; Nijboer et al., 2001; Rabins et al., 1990; Reis et al., 1994), and their results are equivocal. Ideally, future research would assess personality traits at the onset of the caregiving relationship and examine lagged effects on potential mediators and subjective health.
Another limitation is the exclusive focus on subjective health ratings. Although subjective health has been linked to a plethora of objective health outcomes (Benyamini & Idler, 1999; Branch & Ku, 1989; Idler & Benyamini, 1997; Kaplan, Strawbridge, Camacho, & Cohen, 1993; Maddox & Douglass, 1973), future studies need to include measures of both objective and subjective health. Moreover, more comprehensive measures of care recipients’ characteristics such as behavioral problems and required hours of care should be considered.
Finally, there are some concerns about the nature of the sample. Although the present sample is fairly representative of the population in the Medicare PCDC study area, its selective nature does not reflect the racial and ethnic diversity of the U.S. population. Importantly, a recent meta-analysis indicates that stress and resilience in response to caregiving-related demands differ across ethnic groups (Pinquart & Sörensen, 2005). Future studies should therefore aim to recruit more diverse samples with particular emphasis on the inclusion of racial/ethnic minorities. Another sampling consideration that is harder to address concerns the possibility that individuals self-select into the caregiving role based on their personality characteristics (Anthony-Bergstone, Gatz, & Zarit, 1988). To address this issue, more information about the conditions of entry into the caregiving role as well as the availability of alternative caregivers is needed.
In spite of these limitations, the present study makes important contributions to the scarce literature on personality-health links among caregivers by addressing methodological limitations of previous studies and by systematically examining the mediating role of caregiver strain and multi-domain self-efficacy. Because personality traits are relatively stable over time (Roberts, Walton, & Viechtbauer, 2006; Terracciano et al., 2005), personality assessments can help in identifying at-risk populations for health-promoting interventions. At the same time, a better understanding of mediators can inform the development of specific intervention strategies. Our findings suggest that interventions ought to focus on modifying self-efficacy beliefs, which are susceptible to change as a result of verbal instruction, personal experience, and observation of others (Bandura, 1977). As the experience of caregiving can make vulnerable individuals feel particularly ineffective and reduce sense of mastery (Skaff, Pearlin, & Mullan, 1996), setting challenging but highly achievable goals in caregiving or leisure contexts could have salutary effects. Similarly, caregiver strain may be mitigated through social support, respite care, and other services (Wolff et al., 2009). Thus, although each caregiver has a relatively stable profile of personality traits that predisposes towards or protects from caregiving-related health risks, the mechanisms by which personality translates into subjective health can be addressed through appropriate interventions. To maximize success, such interventions could be tailored to the individual personality profile of a given care provider. For instance, caregivers high in extraversion might benefit more from social support groups, whereas those low in extraversion might prefer one-on-one settings. Thus, our findings set the stage for future research exploring how information about caregivers’ personality traits can be leveraged to identify at-risk individuals and guide individually tailored strategies for intervention.
Acknowledgments
Paul T. Costa, Jr. receives royalties from the Revised NEO Personality Inventory. This research was supported in part by National Institutes of Health Grants DAO26652 and MH072712. We acknowledge the Centers for Medicare and Medicaid Services for sponsoring “A Randomized Controlled Trial of Primary and Consumer-Directed Care for People With Chronic Illnesses” (CMS 95-C-90467).
Footnotes
The Medicare PCDC was designed as a randomized controlled trial examining the benefits of two healthcare interventions on multiple aspects of mental and physical well-being, service utilization, and health outcomes among physically impaired individuals and their caregivers. The specific interventions were: (1) a voucher for health supplies or support services, and (2) regular home visits from a disease-management/health-promotion nurse. Participants were randomly assigned to one of four groups: (1) nurse visits, (2) voucher, (3) both nurse visits and voucher, or (4) no intervention control (for further detail see Meng et al., 2005; Meng et al., 2006). Preliminary analyses found that intervention conditions were not significantly related to any of the measures examined in the present study. Also, there is no theoretical reason to assume that the intervention conditions would affect personality traits or the pattern of associations among personality traits, mediators, and subjective health. The intervention variable was therefore dropped from further analyses.
Contributor Information
Corinna E. Löckenhoff, Department of Human Development, Cornell University
Paul R. Duberstein, Department of Psychiatry, University of Rochester
Bruce Friedman, Departments of Community and Preventive Medicine, and Psychiatry, University of Rochester.
Paul T. Costa, Jr., Department of Mental Health, Johns Hopkins Bloomberg School of Public Health
References
- Anthony-Bergstone CR, Gatz M, Zarit SH. Symptoms of psychological distress among dementia patients. Psychology and Aging. 1988;3:245–248. doi: 10.1037/0882-7974.3.3.245. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy - toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological research. Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality - Additional studies, 1995 to 1998. Research on Aging. 1999;21:392–401. doi: 10.1177/0164027599213002. [DOI] [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. The role of neuroticism and mastery in spouse caregivers’ assessment of and response to a contextual stressor. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 1998;53:P155–P164. doi: 10.1093/geronb/53b.3.p155. [DOI] [PubMed] [Google Scholar]
- Branch LG, Ku L. Transition probabilities to dependency, institutionalization, and death among the elderly over a decade. Journal of Aging and Health. 1989;1:370–408. doi: 10.1177/089826438900100306. [DOI] [Google Scholar]
- Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P, Lendon C. Determinants of burden in those who care for someone with dementia. International Journal of Geriatric Psychiatry. 2008;23:1078–1085. doi: 10.1002/gps.2071. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Neuroticism, somatic complaints, and disease - is the bark worse than the bite? Journal of Personality. 1987;55:299–316. doi: 10.1111/j.1467-6494.1987.tb00438.x. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Professional manual: Revised NEO five-factor inventory. Lutz, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Curran PJ, West SG, Finch J. The robustness of test statistics to non-normality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. doi: 10.1037/1082-989X.1.1.16. [DOI] [Google Scholar]
- Duberstein PR, Chapman BP, Tindle HA, Sink K, Bamonti P, Robbins J, Franks P. Personality and risk for Alzheimer’s disease in adults 72 years of age and older: A six-year follow up. Psychology and Aging. doi: 10.1037/a0021377. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein PR, Sörensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, Caine ED. Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging. 2003;18:25–37. doi: 10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual of the Eysenck personality questionnaire. London, UK: Hodder & Stoughton; 1975. [Google Scholar]
- Fengler AP, Goodrich N. Wives of elderly disabled men: The hidden patients. Gerontologist. 1979;19:175–183. doi: 10.1093/geront/19.2.175. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Kercher K, Burant CJ. Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging and Mental Health. 2002;6:153–160. doi: 10.1080/13607860220126763. [DOI] [PubMed] [Google Scholar]
- Friedman B, Wamsley BR, Liebel DV, Saad ZB, Eggert GM. Patient satisfaction, empowerment, and health and disability status effects of a disease management-health promotion nurse intervention among Medicare beneficiaries with disabilities. The Gerontologist. 2009;49:778–792. doi: 10.1093/geront/gnp090. [DOI] [PubMed] [Google Scholar]
- Friedman HS. Long-term relations of personality and health: Dynamisms, mechanisms, tropisms. Journal of Personality. 2000;68:1089–1107. doi: 10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- Gallant MP, Connell CM. Neuroticism and depressive symptoms among spouse caregivers: Do health behaviors mediate this relationship? Psychology and Aging. 2003;18:587–592. doi: 10.1037/0882-7974.18.3.587. [DOI] [PubMed] [Google Scholar]
- Goldberg LR. An alternative description of personality - the big-five factor structure. Journal of Personality and Social Psychology. 1990;59:1216–1229. doi: 10.1037/0022-3514.59.6.1216. [DOI] [PubMed] [Google Scholar]
- Hayashi Y, Okano R, Hirabayashi M, Katayama Y, Numao S, Matsuo T, Tanaka K. Personality and self-efficacy factors in weight maintenance after weight reduction program. Japanese Journal of Physical Fitness and Sports Medicine. 2008;57:197–206. [Google Scholar]
- Hollis-Sawyer LA. Mother-daughter eldercare and changing relationships: A path-analytic investigation of factors underlying positive, adaptive relationships. Journal of Adult Development. 2003;10:41–52. doi: 10.1023/A:1020738804030. [DOI] [Google Scholar]
- Hong SI. Understanding patterns of service utilization among informal caregivers of community older adults. Gerontologist. 2010;50:87–99. doi: 10.1093/geront/gnp105. [DOI] [PubMed] [Google Scholar]
- Hooker K, Frazier LD, Monahan DJ. Personality and coping among caregivers of spouses with dementia. Gerontologist. 1994;34:386–392. doi: 10.1093/geront/34.3.386. [DOI] [PubMed] [Google Scholar]
- Hooker K, Monahan D, Shifren K, Hutchinson C. Mental and physical health of spouse caregivers - the role of personality. Psychology and Aging. 1992;7:367–375. doi: 10.1037/0882-7974.7.3.367. [DOI] [PubMed] [Google Scholar]
- Hooker K, Monahan DJ, Bowman SR, Frazier LD, Shifren K. Personality counts for a lot: Predictors of mental and physical health of spouse caregivers in two disease groups. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 1998;53:P73–P85. doi: 10.1093/geronb/53b.2.p73. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Iwasa H, Masui Y, Gondo Y, Inagaki H, Kawaai C, Suzuki T. Personality and all-cause mortality among older adults dwelling in a Japanese community: A five-year population-based prospective cohort study. American Journal of Geriatric Psychiatry. 2008;16:399–405. doi: 10.1097/JGP.0b013e3181662ac9. [DOI] [PubMed] [Google Scholar]
- Jang Y, Clay OJ, Roth DL, Haley WE, Mittelman MS. Neuroticism and longitudinal change in caregiver depression: Impact of a spouse-caregiver intervention program. Gerontologist. 2004;44:311–317. doi: 10.1093/geront/44.3.311. [DOI] [PubMed] [Google Scholar]
- Jerram KL, Coleman PG. The big five personality traits and reporting of health problems and health behaviour in old age. British Journal of Health Psychology. 1999;4:181–192. doi: 10.1348/135910799168560. [DOI] [Google Scholar]
- Judge TA, Erez A, Bono JE, Thoresen CJ. Are measures of self-esteem, neuroticism, locus of control, and generalized self-efficacy indicators of a common core construct? Journal of Personality and Social Psychology. 2002;83:693–710. doi: 10.1037/0022-3514.83.3.693. [DOI] [PubMed] [Google Scholar]
- Jylha P, Isometsa E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depression and Anxiety. 2006;23:281–289. doi: 10.1002/da.20167. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Strawbridge WJ, Camacho T, Cohen RD. Factors related to change in physical functioning in the elderly: Results from a six-year prospective study. Journal of Aging and Health. 1993;5:140–154. doi: 10.1177/089826439300500107. [DOI] [Google Scholar]
- Kempen G, Jelicic M, Ormel J. Personality, chronic medical morbidity, and health-related quality of life among older persons. Health Psychology. 1997;16:539–546. doi: 10.1037/0278-6133.16.6.539. [DOI] [PubMed] [Google Scholar]
- Kempen G, van Heuvelen MJG, van Sonderen E, van den Brink RHS, Kooijman AC, Ormel J. The relationship of functional limitations to disability and the moderating effects of psychological attributes in community-dwelling older persons. Social Science & Medicine. 1999;48(9):1161–1172. doi: 10.1016/S0277-9536(98)00427-4. [DOI] [PubMed] [Google Scholar]
- Kim Y, Duberstein PR, Sörensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46:123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. Guilford; New York: 2005. [Google Scholar]
- Koerner SS, Kenyon DB, Shirai Y. Caregiving for elder relatives: Which caregivers experience personal benefits/gains? Archives of Gerontology and Geriatrics. 2009;48:238–245. doi: 10.1016/j.archger. 2008.01.015. [DOI] [PubMed] [Google Scholar]
- Koerner SS, Kenyon DYB. Understanding “good days” and “bad days”: Emotional and physical reactivity among caregivers for elder relatives. Family Relations. 2007;56:1–11. doi: 10.1111/j.1741-3729.2007.00435.x. [DOI] [Google Scholar]
- Korotkov D, Hannah TE. The five-factor model of personality: Strengths and limitations in predicting health status, sick-role and illness behaviour. Personality and Individual Differences. 2004;36:187–199. doi: 10.1016/S0191-8869(03)00078-3. [DOI] [Google Scholar]
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. Journals of Gerontology. 1991;46:P181–P189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- Lee S, Klein HJ. Relationships between conscientiousness, self-efficacy, self-deception, and learning over time. Journal of Applied Psychology. 2002;87:1175–1182. doi: 10.1037/0021-9010.87.6.1175. [DOI] [PubMed] [Google Scholar]
- Leitsch SA, Zarit SH, Townsend A, Greene R. Medical and social adult day service programs: A comparison of characteristics, dementia clients, and their family caregivers. Research on Aging. 2001;23:473–498. doi: 10.1177/0164027501234005. [DOI] [Google Scholar]
- Löckenhoff CE, Sutin AR, Ferrucci L, Costa PT. Personality traits and subjective health in the later years: The association between NEO-PI-R and SF-36 in advanced age is influenced by health status. Journal of Research in Personality. 2008;42:1334–1346. doi: 10.1016/j.jrp.2008.05.006. [DOI] [Google Scholar]
- Löckenhoff CE, Terracciano A, Bienvenu OJ, Patriciu NS, Nestadt G, McCrae RR, Costa PT., Jr Ethnicity, education, and the temporal stability of personality traits in the East Baltimore Epidemiologic Catchment Area study. Journal of Research in Personality. 2008;42:577–598. doi: 10.1016/j.jrp.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox GL, Douglass EB. Self-assessment of health: A longitudinal study of elderly subjects. Journal of Health and Social Behavior. 1973;14:87–93. doi: 10.2307/2136940. [DOI] [PubMed] [Google Scholar]
- Markiewicz D, Reis M, Gold DP. An exploration of attachment styles and personality traits in caregiving for dementia patients. International Journal of Aging & Human Development. 1997;45:111–132. doi: 10.2190/T4Q4–E8F0-JWT5-DBAG. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R. Informal caregiving to older adults: Health effects of providing and receiving care. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Mahwah, NJ: Lawrence Erlbaum; 2000. [Google Scholar]
- McCrae RR, Costa PT. Personality in adulthood. 2. New York, NY: Guilford; 2003. [DOI] [Google Scholar]
- McCrae RR, Terracciano A Personal Profiles Cultures, P. Universal features of personality traits from the observer’s perspective: Data from 50 cultures. Journal of Personality and Social Psychology. 2005;88:547–561. doi: 10.1037/0022-3514.88.3.547. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Lu JFR, Sherbourne CD. The MOS 36-item short form health survey (SF36). I. Conceptual framework and item selection. Medical Care. 1994;30:473–483. [PubMed] [Google Scholar]
- Meng HD, Friedman B, Dick AW, Wamsley BR, Eggert GM, Mukamel D. Effect of a voucher benefit on the demand for paid personal assistance. Gerontologist. 2006;46:183–192. doi: 10.1093/geront/46.2.183. [DOI] [PubMed] [Google Scholar]
- Meng HD, Friedman B, Wamsley BR, Mukamel D, Eggert GM. Effect of a consumer-directed voucher and a disease-management- health-promotion nurse intervention on home care use. Gerontologist. 2005;45:167–176. doi: 10.1093/geront/45.2.167. [DOI] [PubMed] [Google Scholar]
- Monahan DJ, Hooker K. Health of spouse caregivers of dementia patients - the role of personality and social support. Social Work. 1995;40:305–314. [PubMed] [Google Scholar]
- Newcomer R, Yordi C, DuNah R, Fox P, Wilkinson A. Effects of the Medicare Alzheimer’s disease demonstration on caregiver burden and depression. Health Services Research. 1999;34:669–689. [PMC free article] [PubMed] [Google Scholar]
- Nijboer C, Tempelaar R, Triemstra M, van den Bos GAM, Sanderman R. The role of social and psychologic resources in caregiving of cancer patients. Cancer. 2001;91:1029–1039. doi: 10.1002/1097-0142(20010301)91:5:: AID-CNCR10943.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Patrick JH, Hayden JM. Neuroticism, coping strategies, and negative well-being among caregivers. Psychology and Aging. 1999;14:273–283. doi: 10.1037/0882-7974.14.2.273. [DOI] [PubMed] [Google Scholar]
- Paunonen SV, Zeidner M, Engvik HA, Oosterveld P, Maliphant R. The nonverbal assessment of personality in five cultures. Journal of Cross-Cultural Psychology. 2000;31:220–239. doi: 10.1177/0022022100031002005. [DOI] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process - an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A metaanalysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of caregiver stressors and uplifts with subjective well-being and depressive mood: A meta-analytic comparison. Aging & Mental Health. 2004;8:438–449. doi: 10.1080/13607860410001725036. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2006;61:P33–P45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2007;62:P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Quinn ME, Johnson MA, Poon LW, Martin P. Psychosocial correlates of subjective health in sexagenarians, octogenarians, and centenarians. Issues in Mental Health Nursing. 1999;20:151–171. doi: 10.1080/016128499248727. [DOI] [PubMed] [Google Scholar]
- Rabinowitz YG, Mausbach BT, Thompson LW, Gallagher-Thompson D. The relationship self-efficacy and between cumulative health risk associated with health behavior patterns in female caregivers of elderly relatives with Alzheimer’s dementia. Journal of Aging and Health. 2007;19:946–964. doi: 10.1177/0898264307308559. [DOI] [PubMed] [Google Scholar]
- Rabins PV, Fitting MD, Eastham J, Zabora J. Emotional adaptation over time in care-givers for chronically ill elderly. Age and Ageing. 1990;19:185–190. doi: 10.1093/ageing/19.3.185. [DOI] [PubMed] [Google Scholar]
- Reis MF, Gold DP, Gauthier S, Andres D, Markiewicz D. Personality traits as determinants of burden and health complaints in caregiving. International Journal of Aging & Human Development. 1994;39:257–271. doi: 10.2190/6LYN-YFWQ-P87D-MKWX. [DOI] [PubMed] [Google Scholar]
- Renzetti C, Iacono S, Pinelli M, Marri L, Modugno M, Neri M. Living with dementia: Is distress influenced by carer personality? Archives of Gerontology and Geriatrics. 2001;7:333–340. doi: 10.1016/S0167-4943(01)00157-1. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rodin J, McAvay G. Determinants of change in perceived health in a longitudinal study of older adults. Journals of Gerontology. 1992;47:P373–P384. doi: 10.1093/geronj/47.6.p373. [DOI] [PubMed] [Google Scholar]
- Rosenthal CJ, Matthews SH, Marshall VW. Is parent care normative – the experiences of a sample of middle-aged women. Research on Aging. 1989;11:244–260. doi: 10.1177/0164027589112006. [DOI] [PubMed] [Google Scholar]
- Shaughnessy PW, Crisler KS, Schlenker RR. Medicare’s OASIS: Standardization outcome and assessment information set for home health care: OASIS B. Denver, CO: Center for Health Services and Policy Research; 1997. [Google Scholar]
- Skaff MM, Pearlin LI, Mullan JT. Transitions in the caregiving career: Effects on sense of mastery. Psychology and Aging. 1996;11:247–57. doi: 10.1037/0882-7974.11.2.247. [DOI] [PubMed] [Google Scholar]
- Staudinger UM, Fleeson W. Self and personality in old and very old age: A sample case of resilience? Development and Psychopathology. 1996;8:867–885. doi: 10.1017/S0954579400007471. [DOI] [Google Scholar]
- Steel P, Schmidt J, Shultz J. Refining the relationship between personality and subjective well-being. Psychological Bulletin. 2008;134:138–161. doi: 10.1037/0033-2909.134.1.138. [DOI] [PubMed] [Google Scholar]
- Taylor MD, Whiteman MC, Fowkes GR, Lee AJ, Allerhand M, Deary IJ. Five factor model personality traits and all-cause mortality in the Edinburgh Artery Study cohort. Psychosomatic Medicine. 2009;71:631–641. doi: 10.1097/PSY.0b013e3181a65298. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Zonderman AB, Ferrucci L, Costa PT. Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine. 2008;70:621–627. doi: 10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, McCrae RR, Brant LJ, Costa PT. Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore longitudinal study of aging. Psychology and Aging. 2005;20:493–506. doi: 10.1037/0882-7974.20.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Zhang JP, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: A user’s manual. Boston: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey - manual and interpretation guide. Boston: The Health Institute; 1993. [Google Scholar]
- Weiss A, Costa PT. Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Schneider JA, Arnold SE, Bienias JL, Bennett DA. Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Archives of General Psychiatry. 2007;64:1204–1212. doi: 10.1001/archpsyc.64.10.1204. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Rand-Giovannetti E, Palmer S, Wegener S, Reider L, Frey K, Boult C. Caregiving and chronic care: The guided care program for families and friends. Journals of Gerontology Series a-Biological Sciences and Medical Sciences. 2009;64:785–791. doi: 10.1093/gerona/glp030. [DOI] [PMC free article] [PubMed] [Google Scholar]