Abstract
Paranoia in methamphetamine (MA) users is not well characterized or understood. To investigate this phenomenon, we created the Methamphetamine Experience Questionnaire (MEQ), and tested its reliability and validity in assessing MA-induced paranoia. METHODS: We administered the MEQ to 274 MA-dependent subjects. RESULTS: 45% (123) subjects first experienced paranoia with MA use; 55% did not. Obtaining or using a weapon while paranoid was common (37% and 11% of subjects with MA-induced paranoia, respectively). Test-retest and inter-rater reliability for MA-induced paranoia showed substantial agreement (kappa = 0.77, p < 0.05 and kappa = 0.80, p < 0.05, respectively). First episodes of paranoia occurred more often with intravenous use of MA, and subsequent episodes at higher doses. There was modest correlation between paranoia on the MEQ and the BSI paranoid ideation scale (rho = 0.27, p < 0.05). As expected, there was a poor correlation between paranoia on the MEQ and the BSI depression scale (rho = 0.14, p = 0.07). The MEQ provides useful information on drug use variables that contribute to paranoia commonly associated with MA use.
Keywords: methamphetamine, paranoia, questionnaire
INTRODUCTION
There are as many MA users world-wide as either cocaine or opioid users.1 Despite a leveling in the prevalence of illicit drug use in general in the United States, methamphetamine (MA) use continues to be a problem. In the United States, the number of treatment admissions for MA as the primary substance of abuse more than tripled between 1996 and 2006, and MA use has grown from a regionalized endemic presence in the western United States to a problem affecting every state in the nation.2 Researchers are increasingly interested in the drug – for example, there have been steady increases from 2003-2007 in the number of MA-related citations in PubMed.
The link between MA use and symptoms of paranoia is well known.3-6 However, separating MA-induced paranoia (MIP) from paranoia attributable to other causes has been challenging. Several research groups in Japan have successfully studied MIP. This study is in part facilitated by a particular characteristic of the Japanese MA subculture: poly-drug use has been uncommon.3, 7 Large studies in other populations have faced greater challenges. For example, McKetin et al,8 building on an earlier study by Hall and colleagues,9 studied past-year psychosis and suspiciousness in a sample of 309 community poly-substance MA users. These investigators found that over half (56%) of the subjects were diagnosed with MA dependence, and 10% had been diagnosed with psychotic disorders. Sixty percent of the subjects presented with mild to clinically significant symptoms of suspiciousness, as measured by the Brief Psychiatric Rating Scale (BPRS). Furthermore, they were able to establish a strong correlation (odds ratio = 3.1) between MA dependence and clinically significant symptoms of psychosis as measured by the BPRS in the past year (but not a direct relationship between episodes of MA use and episodes of psychotic symptoms). Glasner-Edwards and colleagues10 studied current and past psychotic disorders in a 3-year follow-up of 526 MA-dependent, in-treatment subjects. Patients with psychiatric disorders requiring treatment were excluded from enrollment. They found a prevalence of 12.9% for current or past psychotic disorders, but were unable to distinguish between MIP and other psychotic disorders. Another study comparing cocaine- and MA-dependent subjects found high levels (67%) of lifetime symptoms of paranoia in a smaller sample of 43 non-treatment-seeking MA subjects.11 This study used the Psychotic Symptom Assessment Scale (PSAS), an instrument developed by senior members of their research group. The PSAS is a 32-item structured interview that separates symptoms occurring while intoxicated with MA from those that occur while abstinent. It was made publicly available subsequent to the data collected in the study reported here.12
A wide variety of instruments have been developed to measure paranoia, both in clinical and non-clinical populations13-19. Most of these instruments and methods, however, look at current or recent (within 30 days) symptoms. Two exceptions are the aforementioned PSAS and the Cocaine Experience Questionnaire (CEQ), which was developed to study cocaine-induced paranoia 20. The CEQ has been utilized and described in several studies.20-24 Since there are some similarities between cocaine and MA use, we adapted the Methamphetamine Experience Questionnaire (MEQ) from the CEQ to assess lifetime MIP. While the MEQ has also been employed in several studies,12, 25 its psychometric properties have not been fully described. In this paper, we describe the MEQ and present findings from its administration to a large population of MA-dependent subjects.
METHODS
Participants
The subjects were 274 MA users enrolled in larger ongoing studies of MA use in Sacramento and San Francisco, California. We required participants to be 18-65 years of age, fluent in English, MA dependent, but with no past-year dependence on substances other than nicotine. MA dependence was determined by the Structured Clinical Interview for DSM Axis I Disorders (SCID) substance use disorders module.26 Subjects were recruited from local treatment programs, by community advertising, and by word of mouth. All participants provided informed consent. The Institutional Review Boards at the investigators’ institutions approved the study.
Procedures and Measures
The structured interview format of the 42-item CEQ was maintained in developing the MEQ, but modified to apply to MA users. Drug amounts, routes of administration, use patterns and other items were converted to MA-relevant options. Questions were re-organized to streamline the questionnaire's administration, with additional definitions and clarifications added to increase understanding. Drafts were administered to a separate convenience sample of local community informants and recovered MA users in treatment and non-treatment settings, and revised to ensure face validity. The resultant MEQ is a structured interview comprised of 50 items with a number of branch and skip points. Paranoia is defined for the subject as:
You're feeling paranoid if you're feeling convinced that someone or something is out to get you or out to harm you, but you later realize that you'd blown it out of proportion or that it probably wasn't true.
Time needed to administer the questionnaire is approximately 15 minutes (range 1 – 30 minutes, depending on responses). The instrument first ascertains whether subjects ever experienced paranoia while using MA, and if so, inquires further about those experiences. During the study, 30 subjects were able to complete two MEQs on the same day with two different interviewers. Another 26 subjects were able to complete two MEQs with the same interviewer, but with an interval of one to ten days (mean 5.3 ± 2.4) between administrations. See the Appendix for a copy of the MEQ.
One hundred sixty two subjects also completed the Brief Symptom Inventory (BSI).27 The BSI was selected as the best available self-report instrument for a wide range of psychiatric symptoms. All interviewers were trained and observed on the instruments by at least one of the authors.
Statistical Analysis
For all statistical tests, alpha was set at the 0.05 level. Fisher's exact tests were used to compare categorical variables, and Mann-Whitney U tests were used to compare ranked variables. Statistical analysis was performed using the open source statistical software, R.28 To measure convergent validity, we analyzed whether paranoia on the MEQ correlated with the BSI paranoid ideation scale. To measure divergent validity, we hypothesized that paranoia as assessed by the MEQ would not correlate with the BSI depression scale. We analyzed these data using Spearman's rank correlation coefficient.
RESULTS
All 274 subjects were given the MEQ. They were predominantly male (61%, n = 140) and Caucasian (75%, n = 207) with Hispanic and African American subjects comprising 8.4% and 6.6% of the sample, respectively. The mean age was 37.5 (±9.1, range 19-64) years. Information on lifetime years of use of MA was available for 213 of the subjects, with a mean of 10.4 years (±9.3, range 0-47).
Forty-five percent (n = 123) of the 274 subjects first experienced paranoia with MA use (MIP group); 42% (n = 114) never experienced paranoia (P-); 12% (n = 34) first experienced paranoia without MA use, then subsequently with MA use (P+MIP); and 1% (n = 3) experienced paranoia, but never while using MA (P+). We excluded the 37 P+ and P+MIP subjects from further analyses because the paranoia they experienced may have been unrelated to their MA use.
Comparisons between MIP and P- subjects
No statistically significant differences were found between the P- and MIP groups for race (p = 0.26, Fisher's exact test) or age (p = 0.33, Mann-Whitney U test). There was a trend for the MIP group to include more males than the P- group (p = 0.06 Fisher's exact test).
Inter-rater reliability for MIP vs. P- categorizations showed good concordance when corrected for chance occurrence (kappa = 0.80, p < 0.05, n = 30), as did test-retest reliability (kappa = 0.77, p < 0.05, n = 26).
There was fair level of correlation between the MIP/P- categorization and the BSI paranoid ideation scale (rho = 0.29, p < 0.05) and several other BSI symptom scales (see Table 1). The strongest was for the phobic anxiety scale, and there was also moderate correlation with BSI scales for psychoticism, anxiety, and interpersonal sensitivity. As hypothesized, correlation was low between P-/MIP categorization and the BSI depression scale (rho = 0.14, p = 0.07).
TABLE 1.
Correlation between BSI scales and MA-induced paranoia (n = 162)
| BSI Symptom Scale | Rho | p |
|---|---|---|
| Phobic Anxiety | 0.39 | <0.001 |
| Psychoticism | 0.31 | <0.001 |
| Paranoid Ideation | 0.29 | <0.001 |
| Anxiety | 0.25 | 0.001 |
| Interpersonal Sensitivity | 0.20 | 0.010 |
| Somatization | 0.17 | 0.033 |
| Obsessive-Compulsive | 0.16 | 0.034 |
| Hostility | 0.16 | 0.042 |
| Depression | 0.14 | 0.069 |
Characteristics of Methamphetamine-Induced Paranoid Experiences
During subjects’ first occurrence of MIP the most common route of administration was IV (37%), the majority experienced extended sleeplessness (median = 48 h), and the median MA dose was 0.8 g. Median time between use of MA and onset of the first paranoia was 2 h, and the paranoia lasted a median of 6 h.
A large majority (86%) of the MIP group reported paranoia only after repeated MA use, and MIP commonly recurred (0 = never, 5 = always, mean = 2.6 ±1.5). The median quantity of MA used during these subsequent episodes of MIP was also 0.8 g. Paranoia was equally likely to occur in these later episodes when snorting, smoking, or using IV, was less likely when ingested, and most commonly occurred when subjects were alone or in new surroundings.
At the time of paranoia, 38% of the sample reported using other drugs along with MA, most commonly alcohol. Auditory hallucinations were the most frequently reported type of hallucination (67%), followed by visual (63%) and tactile (37%). A smaller number (15%) reported other unusual sensations or perceptions such as olfactory hallucinations or delusions of thought insertion and broadcasting.
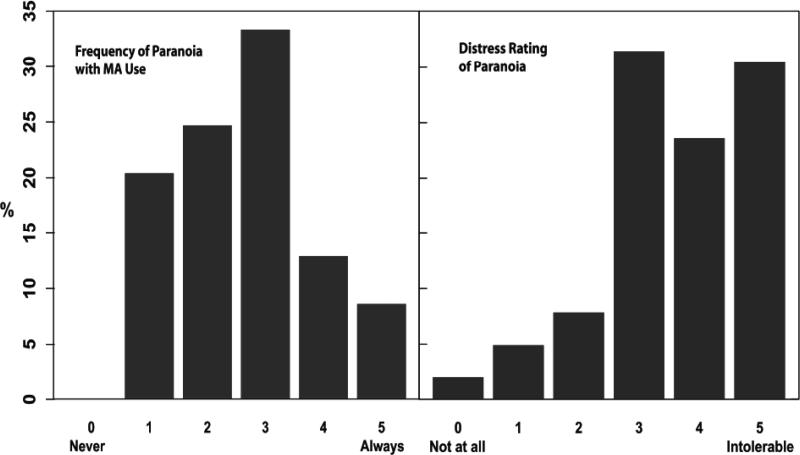
Paranoid experiences were very distressing to subjects (0 = not distressing at all, 5 = intolerable, mean = 3.5 ±1.3, see Figure 1). A considerable number of subjects (37%) reported acting on their paranoia by obtaining a weapon, 11% reported using a weapon, and 15% had attacked others. See Tables 2 and 3.
FIGURE 1.
Frequency of paranoia and distress associated with Methamphetamine-induced paranoia
TABLE 2.
Drug Use During Episodes of Methamphetamine-Induced Paranoia.
| 123 subjects experienced any MIP, 112 had more that one episode of MIP | |
|---|---|
| Amount of MA used, median | |
| • first episode | 0.8 g |
| • usual | 0.8 g |
| Route of MA administration | |
| • first episode1 | |
| • intravenous | 37% (n = 46) |
| • snort | 31% (n = 38) |
| • smoke | 24% (n = 30) |
| • ingest | 3% (n = 4) |
| • other2 | 2% (n = 3) |
| • any episode3 | |
| • intravenous | 48% (n = 60) |
| • snort | 52% (n = 64) |
| • smoke | 49% (n = 59) |
| • ingest | 20% (n = 25) |
| • other2 | 2% (n = 3) |
| Pattern of MA use at first episode4 | |
| • daily | 49% (n = 60) |
| • runs > 2 days | 27% (n = 33) |
| • several times a week | 14% (n = 17) |
| • once a week or less | 10% (n = 12) |
| Use of other drugs during any episode: | |
| • any other drug | 38% (n = 47) |
| • alcohol | 20% (n = 24) |
| • marijuana | 7% (n = 9) |
| • cocaine | 4% (n = 5) |
| • hallucinogens | 4% (n = 5) |
| • opiates | 1% (n = 1) |
| • MDMA | 1% (n = 1) |
| • barbiturates | 0% (n = 0) |
| • sedatives/benzodiazepines | 0% (n = 0) |
| • inhalants | 0% (n = 0) |
| • other | 2% (n = 2) |
| Paranoia more likely with MA amounts greater than usual amount used when experiencing paranoia | 68% (n = 84) |
| Paranoia occurred during first MA use | 8% (n = 10) |
No data available on 2 subjects (2%).
Two subjects reported rectal use, the rest were unspecified.
No data available on 7 subjects (6%).
No data available on 1 subject (< 1%).
TABLE 3.
Characteristics of Methamphetamine-Induced Paranoia.
| 123 subjects experienced MIP, of these, 112 had more that one episode of MIP | |
|---|---|
| Time to onset of paranoia after MA use, median | |
| • first episode | 2 h |
| • most recent episode | 2 h |
| Time awake at onset of paranoia after MA use, median | |
| • first episode | 48 h |
| • other episodes | 48 h |
| If more than one episode, paranoia more likely when1 | |
| • alone | 39% (n = 48) |
| • with others | 23% (n = 28) |
| • no difference | 25% (n = 31) |
| • don't know | 2% (n = 3) |
| If more than one episode, paranoia more likely when in2 | |
| • familiar settings | 28% (n = 35) |
| • new surroundings | 36% (n = 44) |
| • no difference | 24% (n = 30) |
| • don't know | 2% (n = 2) |
| Duration of paranoia after MA use, median | |
| • first episode | 6 h |
| • other episodes | 24 h |
| • longest | 108 h |
| Type of hallucinations | |
| • auditory | 67% (n = 83) |
| • visual | 63% (n = 77) |
| • tactile | 37% (n = 46) |
| • other | 15% (n = 19) |
| Acting on paranoia | |
| • hide, run, try to escape | 63% (n = 77) |
| • call for help | 33% (n = 40) |
| • attack others | 15% (n = 19) |
| • get a weapon | 37% (n = 46) |
| • use a weapon | 11% (n = 14) |
| Most extreme episode not different from typical episode | 51% (n = 63) |
| Vividness of most recent paranoid experience versus first episode1 | |
| • less vivid | 35% (n = 43) |
| • the same | 22% (n = 27) |
| • more vivid | 24% (n = 30) |
| • varies | 8% (n = 10) |
| Paranoia persisting after other effects of MA resolve | |
| • at least one episode | 23% (n = 28) |
| • frequency (0=never, 5 always) | 2.6 ± 1.4 |
No data available on 2 subjects (2%).
No data available on 1 subject (< 1%)..
DISCUSSION
The MEQ has adequate test-retest and inter-rater reliability for use in studies of MIP. The presence or absence of MIP was, as anticipated, not correlated with BSI depression scores, which supports its discriminant validity. There was a modest but significant correlation between the presence or absence of MIP and BSI paranoid ideation scores. Although a higher correlation would indicate greater validity, it is important to note the different time periods assessed by these instruments. While the MEQ assesses lifetime prevalence of paranoia, the BSI assesses paranoid ideation in the previous week.
The MEQ differs from other instruments that assess paranoia in that it inquires about lifetime symptoms, defines paranoia as a persecutory delusion, and emphasizes the difference between paranoia that occurs specifically during MA use and other types of paranoid experiences. The MEQ's definition of paranoia is consistent with the currently accepted concept, and so excludes other more vague or less well formulated ideas of reference that are included in the broader definitions of the term.17, 29 MA users can also differ in their assessment of “intoxication,” “under the influence,” “high,” “while using,” etc., particularly given the relatively long duration of MA effects and the wide range of use patterns from daily to binging. The careful attention of trained interviewers to classifying experiences as paranoid or not and methamphetamine-induced or not increases the face validity of the MEQ.
We found a different prevalence of MIP than that reported in other recent studies, but an exact comparison is not possible, given the different definitions of paranoia used and different subject selection methods.8, 10, 11 Other studies of MIP do not report results of persecutory delusions per se, but of a range of psychotic symptoms in general, so some symptoms we would classify as paranoid may have been classified differently (e.g., as “unusual beliefs” or such). In reviewing their results and attempting a rough reclassification in accordance with the definition of paranoia used in the CEQ, MEQ and other paranoia research, we show a higher rate than Mahoney et al. (45% versus an estimated 30%) but a lower rate than McKetin et al. (45% versus an estimated 60%). Some of the discrepancy may be due to differences in sample sizes and subject characteristics in the studies. In addition, particular characteristics of the MEQ may affect subjects’ reports of paranoia. For example, the MEQ uses introductory statements about paranoia to reduce the potential stigma of endorsing paranoia, and the instrument specifies and clarifies a definition of paranoia. The prevalence of paranoia in MA users seems similar to the prevalence in cocaine users, as the CEQ has yielded values of 68% and 54%.20, 23
We chose to focus on paranoia, rather than psychosis in general, out of the belief that delusions of persecution may lead to highly socially unacceptable behaviors such as violence. Our results suggest that this is so: 37% of MIP subjects acquired weapons while paranoid and almost half as many (15%) actually attacked others. While the social impact of attacking others may be high, it should be noted that it was a small number of MIP subjects who acted violently. These results seem consistent with measurements of hostility among MA users with psychosis reported elsewhere, despite differences in measures and methods.30
Study findings may have utility in clinical settings. The data may be used to normalize or validate the experiences of MA dependent clients. It may also be useful in evaluating such clients to ask specifically about past weapon acquisition and use, as well as current weapon availability, given the prevalence of these features in our sample. Given the different findings seen in studies with different assessment instruments, our study also highlights the importance of treatment providers asking specific, detailed questions about symptoms of psychosis, rather than inquiring generally or less completely about MA-induced psychotic symptoms. Our study was not designed to examine differences between participants with and without MA-induced psychosis (MIP and P- groups); this remains an area for active research.
The study has certain limitations. In inquiring about lifetime use, the MEQ requires a self-report of symptoms that may date back a number of years (mean years of MA use = 10.4) and it is not clear how reliable such reports may be. It is also possible that by recruiting community subjects we excluded MA users with more severe paranoia, e.g., those in controlled settings due to the extent of their paranoia, or those who might avoid participation in research studies because of their paranoia. Conversely, it is not known if treatment seeking persons might actually have a higher prevalence of MIP, and are motivated by their experience of paranoia to seek help. Lastly, unlike participants in the studies from Japan cited earlier, many of our subjects (38%) were using other substances during paranoid experiences, so how much other substances contributed to the induction of paranoia cannot be determined accurately. Future studies are needed to investigate the impact of these limitations.
Supplementary Material
ACKNOWLEDGMENTS
The authors wish to thank Joseph Cubells, MD, PhD, for developing the Cocaine Experience Questionnaire, Danielle E. Hubbard for assisting with the manuscript, the staff members who collected these data, and the subjects who provided them. This work was supported in part by NIH grants AA13736, DA10641, DA14359, and DA18179.
REFERENCES
- 1.United Nations Office on Drugs and Crime . World Drug Report 2008. United Nations, Publication #E.08.XI.1; Vienna: 2008. [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration Office of Applied Studies . Treatment Episode Data Set (TEDS). Highlights - 2006. National Admissions to Substance Abuse Treatment Services; Rockville, MD: 2008. [Google Scholar]
- 3.Sato M, Chen CC, Akiyama K, Otsuki S. Acute exacerbation of paranoid psychotic state after long-term abstinence in patients with previous methamphetamine psychosis. Biol Psychiatry. 1983 Apr;18(4):429–440. [PubMed] [Google Scholar]
- 4.Batki SL, Harris DS. Quantitative drug levels in stimulant psychosis: relationship to symptom severity, catecholamines and hyperkinesia. Am J Addict. 2004 Oct-Dec;13(5):461–470. doi: 10.1080/10550490490512834. [DOI] [PubMed] [Google Scholar]
- 5.Leamon MH, Gibson DR, Canning RD, Benjamin L. Hospitalization of patients with cocaine and amphetamine use disorders from a psychiatric emergency service. Psychiatr Serv. 2002 Nov;53(11):1461–1466. doi: 10.1176/appi.ps.53.11.1461. [DOI] [PubMed] [Google Scholar]
- 6.Nordahl TE, Salo R, Leamon M. Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. J Neuropsychiatry Clin Neurosci. 2003;15(3):317–325. doi: 10.1176/jnp.15.3.317. [DOI] [PubMed] [Google Scholar]
- 7.Iwanami A, Sugiyama A, Kuroki N, et al. Patients with methamphetamine psychosis admitted to a psychiatric hospital in Japan. A preliminary report. Acta Psychiatr Scand. 1994;89(6):428–432. doi: 10.1111/j.1600-0447.1994.tb01541.x. [DOI] [PubMed] [Google Scholar]
- 8.McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006 Oct;101(10):1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- 9.Hall W, Hando J, Darke S, Ross J. Psychological morbidity and route of administration among amphetamine users in Sydney, Australia. Addiction. 1996 Jan;91(1):81–87. doi: 10.1046/j.1360-0443.1996.9118110.x. [DOI] [PubMed] [Google Scholar]
- 10.Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, Rawson R. Clinical course and outcomes of methamphetamine-dependent adults with psychosis. J Subst Abuse Treat. 2008 Dec;35(4):445–450. doi: 10.1016/j.jsat.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Mahoney JJ, Kalechstein AD, De La Garza R, Newton TF. Presence and persistence of psychotic symptoms in cocaine-versus methamphetamine-dependent participants. Am J Addict. 2008 Mar-Apr;17(2):83–98. doi: 10.1080/10550490701861201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salo R, Nordahl TE, Possin K, et al. Preliminary evidence of reduced cognitive inhibition in methamphetamine-dependent individuals. Psychiatry Res. 2002 Aug 5;111(1):65–74. doi: 10.1016/s0165-1781(02)00111-7. [DOI] [PubMed] [Google Scholar]
- 13.Green CE, Freeman D, Kuipers E, et al. Measuring ideas of persecution and social reference: the Green et al. Paranoid Thought Scales (GPTS). Psychol Med. 2008 Jan;38(1):101–111. doi: 10.1017/S0033291707001638. [DOI] [PubMed] [Google Scholar]
- 14.Freeman D, Pugh K, Green C, Valmaggia L, Dunn G, Garety P. A measure of state persecutory ideation for experimental studies. J Nerv Ment Dis. 2007 Sep;195(9):781–784. doi: 10.1097/NMD.0b013e318145a0a9. [DOI] [PubMed] [Google Scholar]
- 15.Shryane NM, Corcoran R, Rowse G, et al. Deception and false belief in paranoia: modelling theory of mind stories. Cognit Neuropsychiatry. 2008 Jan;13(1):8–32. doi: 10.1080/13546800701748805. [DOI] [PubMed] [Google Scholar]
- 16.Mason OJ, Morgan CJ, Stefanovic A, Curran HV. The psychotomimetic states inventory (PSI): measuring psychotic-type experiences from ketamine and cannabis. Schizophr Res. 2008 Aug;103(1-3):138–142. doi: 10.1016/j.schres.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 17.Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007 May;27(4):425–457. doi: 10.1016/j.cpr.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Moutoussis M, Williams J, Dayan P, Bentall RP. Persecutory delusions and the conditioned avoidance paradigm: towards an integration of the psychology and biology of paranoia. Cognit Neuropsychiatry. 2007 Nov;12(6):495–510. doi: 10.1080/13546800701566686. [DOI] [PubMed] [Google Scholar]
- 19.Combs DR, Penn DL, Chadwick P, Trower P, Michael CO, Basso MR. Subtypes of paranoia in a nonclinical sample. Cognit Neuropsychiatry. 2007 Nov;12(6):537–553. doi: 10.1080/13546800701707306. [DOI] [PubMed] [Google Scholar]
- 20.Satel SL, Southwick SM, Gawin FH. Clinical features of cocaine-induced paranoia. Am J Psychiatry. 1991 Apr;148(4):495–498. doi: 10.1176/ajp.148.4.495. [DOI] [PubMed] [Google Scholar]
- 21.Satel SL, Edell WS. Cocaine-induced paranoia and psychosis proneness. Am J Psychiatry. 1991 Dec;148(12):1708–1711. doi: 10.1176/ajp.148.12.1708. [DOI] [PubMed] [Google Scholar]
- 22.Cubells JF, Feinn R, Pearson D, et al. Rating the severity and character of transient cocaine-induced delusions and hallucinations with a new instrument, the Scale for Assessment of Positive Symptoms for Cocaine-Induced Psychosis (SAPS-CIP). Drug Alcohol Depend. 2005 Oct 1;80(1):23–33. doi: 10.1016/j.drugalcdep.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 23.Gelernter J, Kranzler HR, Satel SL, Rao PA. Genetic association between dopamine transporter protein alleles and cocaine-induced paranoia. Neuropsychopharmacology. 1994 Nov;11(3):195–200. doi: 10.1038/sj.npp.1380106. [DOI] [PubMed] [Google Scholar]
- 24.Tang YL, Kranzler HR, Gelernter J, Farrer LA, Cubells JF. Comorbid psychiatric diagnoses and their association with cocaine-induced psychosis in cocaine-dependent subjects. Am J Addict. 2007 Sep-Oct;16(5):343–351. doi: 10.1080/10550490701525723. [DOI] [PubMed] [Google Scholar]
- 25.Salo R, Nordahl TE, Leamon MH, et al. Preliminary evidence of behavioral predictors of recurrent drug-induced psychosis in methamphetamine abuse. Psychiatry Res. 2008 Jan 15;157(1-3):273–277. doi: 10.1016/j.psychres.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 26.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- 27.Derogatis L. Brief Symptom Inventory (BSI) Administration, Scoring, and Procedures Manual. Third ed. National Computer Systems, Inc.; Minneapolis, MN: 1993. [Google Scholar]
- 28.R [computer program] Version 2.7.0: The R Project for Statistical Computing. 2008 [Google Scholar]
- 29.Edgerton JE, Campbell RJL, editors. American Psychiatric Glossary. American Psychiatric Press, Inc.; Washington, DC: 1994. [Google Scholar]
- 30.McKetin R, McLaren J, Lubman DI, Hides L. Hostility among methamphetamine users experiencing psychotic symptoms. Am J Addict. 2008 May-Jun;17(3):235–240. doi: 10.1080/10550490802019816. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.