Abstract
Rift Valley fever (RVF) is a zoonotic disease endemic in Africa and the Arabian Peninsula caused by the highly infectious Rift Valley fever virus (RVFV) that can be lethal to humans and animals and results in major losses in the livestock industry. RVF is exotic to the United States; however, mosquito species native to this region can serve as biological vectors for the virus. Thus, accidental or malicious introduction of this virus could result in RVFV becoming endemic in North America. Such an event would likely lead to significant morbidity and mortality in humans, and devastating economic effects on the livestock industry. Currently, there are no licensed vaccines for RVF that are both safe and efficacious. To address this issue, we developed two recombinant RVFV vaccines using vaccinia virus (VACV) as a vector for use in livestock. The first vaccine, vCOGnGc, was attenuated by the deletion of a VACV gene encoding an IFN-γ binding protein, insertional inactivation of the thymidine kinase gene, and expression of RVFV glycoproteins, Gn and Gc. The second vaccine, vCOGnGcγ, is identical to the first and also expresses the human IFN-γ gene to enhance safety. Both vaccines are extremely safe; neither resulted in weight loss nor death in severe combined immunodeficient mice, and pock lesions were smaller in baboons compared with the controls. Furthermore, both vaccines induced protective levels of antibody titers in vaccinated mice and baboons. Mice were protected from lethal RVFV challenge. Thus, we have developed two safe and efficacious recombinant vaccines for RVF.
Rift Valley fever virus (RVFV) is a member of the Phlebovirus genus of the Bunyaviridae family of viruses (1, 2). It has a tripartite negative-stranded RNA genome consisting of small (S), medium (M), and large (L) segments encoding the N, NSs (3), Gn (G2), Gc (G1), NSm (4, 5), and L genes, respectively (6, 7). RVFV is spread primarily by infected Aedes mosquitoes and is the causative agent of Rift Valley fever (RVF), originally described following an outbreak of enzootic hepatitis on a farm in the Rift Valley of Kenya in 1931 (8). A disease of both humans and livestock, RVF can cause a hemorrhagic fever with potentially fatal consequences. Mortality in adult cattle and sheep is ∼10% and 20%, respectively. However, the mortality rate in neonatal sheep and spontaneous abortion rates in pregnant ewes are close to 100% (9–10). The mortality rate in humans is estimated at less than 1%, but some outbreaks have significantly higher rates (11). Introduction of RVFV into nonendemic areas, such as the United States, whether accidental or intentional, would have devastating consequences (12). Thus, RVFV has enormous potential to be used as a bioterrorist agent (13).
Currently, there are no RVFV vaccines approved for general use in humans, and those in use in livestock either lack efficacy or have substantial side effects, especially in pregnant animals (14–16). Thus, we have used our considerable experience in developing recombinant vaccinia viruses (rVACVs) (17, 18) to construct two safe and efficacious, livestock vaccines for RVF. These vaccines express the two surface glycoproteins (Gn and Gc) to induce protective immunity to RVFV; one vaccine also expresses the human IFN-γ gene to enhance safety for vaccinators. We used the Copenhagen (vCO) strain of VACV with two virulence genes deleted to provide a safe, heat-stable, and inexpensive vector for the vaccine.
Results
Construction and Characterization of rVACV Vaccines.
We constructed two recombinant RVF vaccines for use in livestock with the Copenhagen strain (vCO) of VACV (17) with two virulence genes (B8R and thymidine kinase, TK) inactivated. An intermediate rVACV (vCOΔB8R) was constructed by deleting the B8R gene (Fig. 1) using homologous recombination (19) and transient dominant selection (20). One rVACV expresses the RVFV glycoproteins (Gn and Gc) under the control of a strong VACV synthetic promoter (vCOGnGc) (17, 21) and the second expresses the human IFN-γ (HuIFNγ) gene in addition to the two RVFV glycoproteins (vCOGnGcγ). The HuIFNγ gene was added to enhance safety for human vaccinators (22, 23). These genes were inserted into the VACV TK gene, resulting in insertional inactivation of this virulence gene and enhancing safety of the vaccines. A third rVACV, used as a control, was engineered with an inactivated TK gene and a deleted B8R gene (vCOΔB8RTK−) but lacked the RVFV glycoprotein and HuIFNγ genes (Fig. 1).
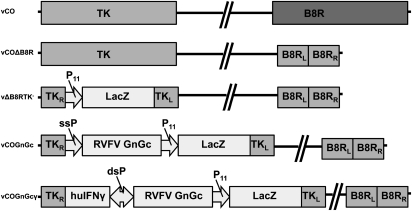
Fig. 1.
Diagram of rVACVs and plasmid transfer vectors. Schematic representation of the rVACVs used in this study, including the insertion sites (TK, B8R genes), VACV promoters used (P11, a natural late VACV promoter; ssP, a single synthetic promoter; dsP, a double synthetic promoter), and a corresponding diagram of the parental vCO. B8RL and B8RR are labeled in the diagrams of the rVACVs as indicators of gene location; however, these sequences are actually in the region flanking the B8R gene, which has been completely deleted from the rVACV genomes. This finding is in contrast to the inactivation of the TK gene by insertion rather than by deletion.
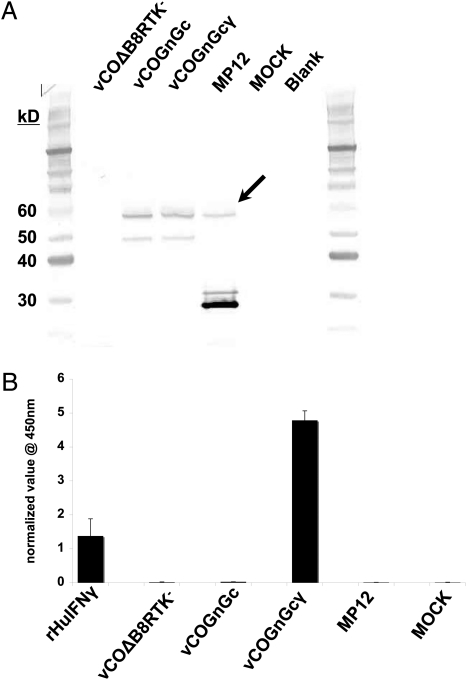
Heterologous protein expression from the rVACV constructs was confirmed by Western blot analysis (Fig. 2A) to detect the RVFV glycoproteins with expected sizes of Gc (56 kD) and Gn (54 kD) in vCOGnGc, vCOGnGcγ, and a live attenuated RVF vaccine (MP-12) but not in the control construct, vCOΔB8RTK. The two proteins are similar in size and the Gc band is faint, so that only one band is easily seen. The expression and biological activity of HuIFNγ was confirmed by ELISA (Fig. 2B) and a bioassay (3.9 × 104 units/mL), indicating high-level expression of the cytokine. The presence of IFN-γ was only detected in the supernatant of vCOGnGcγ-infected cells.
Fig. 2.
Characterization of protein expression by recombinant vaccinia viruses. (A) Western blot analysis of Vero cells infected with vCOΔB8RTK−, vCOGnGc, vCOGnGcγ, or MP-12 using anti-RVF polyclonal serum as a primary antibody and goat anti-mouse AP-conjugated secondary antibody (BioRad). The arrow highlights the bands representing the Gn (56 kD) and Gc (54 kD) glycoproteins of RVFV in lanes 3 to 5. The prominent lower band in lane 5 (MP-12) is the nucleoprotein. (B) Culture supernatants from cell cultures used for the Western blot in A were assayed for the presence of IFN-γ using a commercially available ELISA (eBioscience) and a bioassay.
Attenuation and Safety of rVACVs.
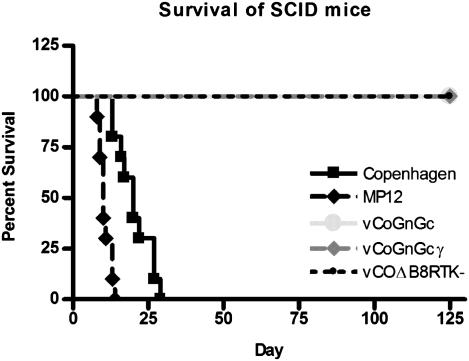
Previously, we demonstrated that deletion of the B8R and inactivation of the TK genes greatly reduced the virulence of rVACV constructs for normal and immunodeficient mice (24). To evaluate the attenuation of our RVF vaccine constructs, we inoculated SCID mice intraperitoneally with 107 pfu of VACV. Inoculation of SCID mice with parental vCO resulted in the development of numerous pock lesions; animals were killed because of weight loss (30%) at a median time of 20 d postinfection (Fig. 3). In contrast, all SCID mice inoculated intraperitoneally with 107 pfu of the three rVACVs survived 125 d without weight loss, although some animals had pock lesions. In comparison, SCID mice inoculated intraperitoneally with MP-12 (6.5 × 105 pfu) had a median time to killing because of neurological signs of 10 d (Fig. 3). These data indicate that our rVACV vaccines are highly attenuated compared with the parental VACV and MP-12.
Fig. 3.
Safety of recombinant vaccinia viruses in a SCID mouse model. Seven- to 8-wk-old male SCID mice were challenged intraperitoneally with 107 pfu of the indicated VACV or 6.5 × 105 pfu of MP-12. Length of survival following inoculation is shown in the graph.
Protection Against Lethal Challenge.
Vaccines that induce virus-neutralizing (VN) antibodies against RVFV have been shown to be protective (25). Levels of VN antibodies were determined using an 80% plaque-reduction neutralization test (PRNT80). To assess efficacy of the rVACVs, six groups of CB6F1 mice (10 per group) were immunized once or twice intramuscularly with MP-12, vCOGnGc, or vCOGnGcγ. A seventh group of 10 naive mice was used as a challenge control group (Table 1). All animals were challenged at 22 wk postvaccination with 103 pfu (intraperitoneally) of the virulent ZH501 strain of RVFV. All naive control mice succumbed to peracute death by day 3. Mice vaccinated once with MP-12 survived challenge without signs of illness. Two of the 10 animals in this group were eliminated because of causes unrelated to the vaccination or challenge. Animals vaccinated once with the rVACVs were partially protected; 10% of vCOGnGcγ and 50% of vCOGnGc-vaccinated mice survived challenge, despite showing clinical signs (Table 1). The efficacy of the rVACV vaccines was improved significantly in animals vaccinated twice. As expected, 100% of mice in the MP-12 group survived, although one mouse did present with clinical signs. In the vCOGnGcγ-vaccinated group, 60% of the mice survived lethal challenge and 90% survived in the vCOGnGc-vaccinated group (Table 1). None of the survivors in the vCOGnGc-vaccinated group had clinical signs. These data indicate that our rVACV vaccines protected mice from a highly lethal challenge with the virulent ZH501 RVFV strain.
Table 1.
Responses to prime/boost vaccination and virulent RVFV challenge in mice
| Mean neutralizing antibody titers* |
|||||||
| Group | Vaccine† | Survival‡ | Illness§ | 2 wpv | 8 wpv | 16 wpv | 25 wpv (3,wpc) |
| 1 | MP-12, 1X | 100% | 0% | 80 | 320 | 400 | 820 |
| 2 | MP-12, 2X | 100% | 10% | 40 | 160 | 800 | 720 |
| 3 | vCOGnGc, 1X | 50% | 100% | 20 | 20 | 40 | 3,586 |
| 4 | vCOGnGc, 2X | 90% | 10% | 20 | 20 | 80 | 10,240 |
| 5 | vCOGnGcγ, 1X | 10% | 100% | 10 | 20 | 10 | 10,240 |
| 6 | vCOGnGcγ, 2X | 60% | 50% | 10 | 10 | 40 | 6,400 |
| 7 | None | 0% | 100% | N/A | N/A | N/A | N/A |
N/A, not applicable; wpc, weeks postchallenge; wpv, weeks postvaccination.
*Antibody titers were determined by PRNT80.
†Vaccine administered to that group. 1X designates the groups receiving only a single vaccination and 2X designates the groups that received both primary and secondary vaccinations before challenge.
‡Percentage of mice surviving lethal challenge.
§Percentage of mice showing signs of illness after lethal challenge.
Studies in a Nonhuman Primate Model.
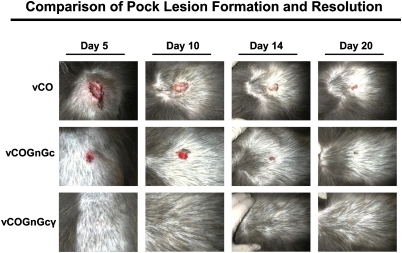
To evaluate the immunogenicity and safety of the rVACVs in primates, three groups of baboons (Papio cynocephalus anubis; four per group) were inoculated via scarification with a bifurcated needle with ∼5 × 107 pfu of vCO, vCOGnGc, or vCOGnGcγ. Relative attenuation of the rVACVs was determined by measuring pock lesion size at days 5, 10, 14, and 20 postinoculation. As expected, lesions in the vCO-inoculated control group were large and ulcerative, measuring 2.5 ± 0.41 cm by day 5, and were not fully resolved in all animals by day 20 (Fig. 4). In contrast, the vCOGnGc-inoculated baboons developed smaller lesions with almost no ulceration, measuring 1.3 ± 1.1 cm by day 5 (P > 0.05) that were almost fully resolved by day 14. Lesions in the vCOGnGcγ-vaccinated group were significantly smaller than the control group on day 5 (0.33 ± 0.15 cm, P < 0.01) and day 10 (0.17 ± 0.1 cm, P < 0.05), and mostly resolved by day 5 (Fig. 4).
Fig. 4.
Comparison of pock lesion formation and resolution in vaccinated baboons. Photographs of representative pock lesions in baboons at days 5, 10, 14, and 20 postvaccination with vCO, vCOGnGc, or vCOGnGcγ. Baboons were vaccinated with ∼5 × 107 pfu of the indicated virus via scarification with a bifurcated needle.
VN antibody titers were measured by RVFV PRNT80. To evaluate anamnestic immune responses to the rVAVCs, baboons were given an intramuscular booster immunization at day 28 with 1 × 109 pfu. Antibody responses to RVFV were obtained following inoculation with the rVACVs but not with vCO. The VN antibody titers were higher in baboons given vCOGnGc than those inoculated with vCOGnGcγ, correlating with the results found in the mouse studies (Table 2). In addition, an anamnestic antibody response was observed following the intramuscular boost at levels considered protective in all baboons (25).
Table 2.
Humoral immune responses to prime/boost vaccination in baboons
| Neutralizing antibody* |
||||||||||||
| vCO |
vCOGnGc |
vCOGnGcγ |
||||||||||
| Day† | 3108 | 10207 | 4408 | 7407 | 10007 | 608 | HK82 | 2108 | 1308 | HL25 | 2208 | 6707 |
| 0 | <4 | <4 | <4 | <4 | <4 | 4 | 4 | 4 | 4 | 4 | 4 | <4 |
| 5 | <4 | <4 | <4 | <4 | <4 | 4 | 4 | 4 | 4 | 4 | 4 | <4 |
| 10 | <4 | <4 | <4 | <4 | 16‡ | 8 | 4 | 16 | 8 | 64 | 4 | <4 |
| 15 | <4 | <4 | <4 | <4 | 16 | 32 | 16 | 16 | 4 | 4 | 4 | 16 |
| 20 | <8 | <8 | <8 | <8 | 8 | 16 | 8 | 64 | 8 | 16 | 8 | <8 |
| 28 | <8 | <8 | <8 | <8 | 16 | 16 | 16 | 64 | 16 | 8 | 8 | <8 |
| 35 | <8 | <8 | <8 | <8 | 512 | 1,024 | 1,024 | 4,096 | 16 | 16 | 32 | 32 |
| 46 | <8 | <8 | <8 | <8 | 256 | 2,048 | 512 | 1,024 | 16 | 64 | 128 | 32 |
| 56 | <8 | <8 | <8 | <8 | 128 | 512 | 512 | 1,024 | 64 | 64 | 512 | 16 |
*Antibody titers (PRNT80) were determined on Vero cells using the MP-12 strain of RVFV.
†Initial vaccination was administered by scarification on day 0, and the intramuscular booster inoculation was given on day 28.
‡Titers shown in boldface are those that are high enough to meet protection standards; titers as low as 1:12 have previously been shown to be protective.
Discussion
The introduction and establishment of West Nile virus in North America has demonstrated the urgent need to develop strategies for preventing a similar occurrence with other vector-borne viruses, such as RVFV. Unfortunately, there are currently no safe and efficacious vaccines against RVF licensed for use in either humans or livestock. To address this concern, we developed and tested two rVACV vaccines for RVF for use in animals. Other vaccines in development for RVF include attenuated RVFV strains with deletions in the NSs gene (25), DNA, and subunit (27–30). Recombinant poxvirus vaccines have been previously developed using the lumpy skin disease virus or the WR strain of VACV as vectors (31, 32). However, lumpy skin disease virus vectors can only be used in areas endemic for lumpy skin disease. Similarly, the WR strain, the neurovirulent laboratory strain of VACV, cannot be used as a vaccine (33). For this reason, we used a vaccine strain of VACV that was used in the smallpox eradication campaign and is currently being used as a vector for eradication of rabies.
Our laboratory has extensive experience in developing rVACVs for the control of a number of human and animal diseases (17, 18, 22, 24, 34, 35). Multiple approaches have been used to enhance the safety of poxviruses, including deletion or insertional inactivation of genes that enhance virulence, expression of cytokines, development of replication-deficient VACVs, such as MVA and NYVAC, or host cell-restricted vectors, such as canarypox and fowlpox (39–42). All of these approaches increase attenuation and subsequently enhance safety. Replication-deficient vectors, however, are difficult to propagate to high titers and are often poorly immunogenic, especially when used as heterologous vaccine vectors. To address these issues, we have developed a number of rVACV with deletions in virulence and immunomodulating genes and expressing cytokines (34, 35, 38). These rVACVs are highly attenuated, immunogenic, and replicate to high titers in vitro.
We developed a rVACV vaccine for RVF with deletions in TK and B8R genes and expressing the two glycoproteins of RVFV (vCOGnGc) that have been shown to induce VN antibodies and protective immunity to the disease (31). A second vaccine for RVF, identical to the first vaccine except for expressing HuIFNγ (vCOGnGcγ), was also developed. The HuIFNγ gene was included to enhance safety for individuals vaccinating livestock. In our previous studies, we have shown that replication-competent VACV can be attenuated by more than a million-fold by this method (34, 35, 38).
All three rVACVs were highly attenuated for mice compared with the parental virus (vCO). SCID mice inoculated with 107 pfu of rVACV survived for 125 d without weight loss, whereas mice given the parental virus had severe weight loss and a median time to killing of 20 d. This finding indicates that the modifications to the vaccine vector resulted in a significant increase in attenuation. Additionally, inoculation of MP-12 in SCID mice resulted in a median time to killing of 10 d, demonstrating the enhanced safety of the rVACV vaccines.
In previous studies, VN antibody titers as low as 1:12 have been shown to be protective, and a mean titer of 1:40 is recommended for protection against RVF (27). Mice vaccinated with either rVACV generated VN antibodies to RVFV, although those immunized with vCOGnGcγ had lower antibody responses compared with mice given vCOGnGc. Neither rVACV vaccine induced antibodies to the same levels as MP-12. Mice vaccinated with MP-12 had no anamnestic responses to either booster immunization with MP-12 or after challenge with virulent virus, indicating a sterilizing immune response. In contrast, those immunized with rVACV vaccines had strong anamnestic responses to booster immunization and challenge with virulent virus. A single vaccination with rVACV resulted in 50% protection in the vCOGnGc-vaccinated group and 10% in mice immunized with vCOGnGcγ. In contrast, animals immunized twice with vCOGnGc had a 90% survival rate after challenge, compared with a rate of 60% in mice vaccinated twice with vCOGnGcγ. Mice vaccinated with MP-12 once or twice had a 100% survival rate. None of the naive control animals survived beyond 3 d postchallenge, indicating a very strong challenge. It is interesting to note that HuIFNγ appeared to reduce the immune responses of mice to the rVACV. This result is most likely because of reduced replication caused by the attenuating effects of HuIFNγ on rVACVs, even in a heterologous species such as mice (35), in addition to the lack of functional B8R and TK genes. Furthermore, the reduced immune response in mice vaccinated with rVACVs in comparison with MP-12 could be a result of the level of expression of Gn and Gc.
The GnGc polyprotein can be expressed from one of five start codons (4) of segment M of RVFV before being cleaved into the separate proteins. This process enables production of another viral protein, NSm, a virulence factor for RVFV (4). To avoid expression of this protein, we used the fourth start codon for the expression of GnGc polyprotein. However, use of one of the first three start codons or expression of Gn and Gc separately might lead to higher expression levels of the glycoproteins, and thus induce more protective immune responses. Further research will be needed to test this hypothesis.
Baboons immunized with rVACVs also generated VN antibodies to RVFV; again, those immunized with vCOGnGcγ had lower antibody responses, similar to the results obtained in mice. All baboons immunized with rVACV vaccines had strong anamnestic responses to booster immunization. As expected, control animals that received parental virus (vCO) had no antibody response to RVFV.
Safety studies of the rVACVs were conducted in SCID mice and baboons. The parental VACV was highly virulent for SCID mice, with a median time of only 20 d to reach the endpoint of 30% weight loss. SCID mice inoculated with any of the three rVACVs survived for more than 100 d without measureable weight loss (Fig. 3), demonstrating that the recombinants are highly attenuated and safe for use. MP-12 was also highly virulent for SCID mice, with a median survival time of 10 d. As anticipated, baboons inoculated with the highly attenuated vCOGnGcγ had significantly smaller pock lesions compared with those vaccinated with vCO (Fig. 4). Human and baboon IFN-γ have 93% identity at the protein level, and HuIFNγ is active in the baboon. Similarly, baboons vaccinated with vCOGnGc had smaller lesions and no ulcerations, although not to same degree as those vaccinated with vCOGnGcγ. In contrast, there was no detectable difference in attenuation between the two rVACVs in mice, probably because of the use of human instead of murine IFN-γ.
The two rVACV vaccines appear to be highly safe and reasonably efficacious compared with other RVF vaccines currently available. Many live-attenuated vaccines for RVF, including MP-12, have major safety concerns, including abortions in ewes and teratogenic effects in lambs (43, 44). We also showed that MP-12 was highly pathogenic for SCID mice, resulting in a median time to death of only 10 d. An additional advantage of our rVACVs is that they permit the use of a simple test to distinguish infected from vaccinated animals using the N protein of RVFV. Other attenuated vaccines, such as Clone 13, have the capability to distinguish infected from vaccinated using the NSs protein; however, NSs is not highly immunogenic as the N protein, leading to reduced sensitivity (45, 46). Inactivated RVFV vaccines, such as TGI-GSD-200, are safe for use in pregnant and young animals but are less immunogenic (27). Similarly, subunit and DNA vaccines are also safe but poorly immunogenic, requiring multiple immunizations (27–29). Another significant advantage of the rVACVs is their heat stability, thus eliminating the need for maintaining the cold chain. In addition, VACV propagates to a very high titer in cell culture, unlike replication-deficient VACVs, such as modified vaccinia virus Ankara (40), thus facilitating the large-scale production of the vaccine. In conclusion, we have developed a highly safe and relatively efficacious vaccine for RVF that provided up to 90% protection against a robust challenge in a mouse model. Future studies in target species (ruminants) will help further evaluate the safety and efficacy of the vaccine. Other goals include enhancing both the safety and efficacy of the rVACVs. To further enhance safety, we will delete more immunoregulatory VACV genes, such as B13R and B22R, as we have demonstrated previously (24, 38, 47). To enhance efficacy, we will explore strategies to increase expression levels of GnGc in rVACV, including codon optimization, using different VACV promoters, or expression of Gn and Gc separately.
Methods
Viruses and Cell Culture.
Vero cells were grown in OptiPro serum-free medium (Invitrogen). BS-C-1, HeLa S3, and L929 cells were grown in DMEM with 10% FBS. All cell cultures were grown at 37 °C with 5% CO2. VACVs were propagated in Vero and HeLa S3 cells and titered in BS-C-1 cells. The MP-12 strain of RVFV was propagated and titered in Vero cells.
Transfer Vectors.
Plasmid pT7-7 contains the M-segment of the ZH-501 strain and was used as a source for the RVFV Gn/Gc glycoprotein ORF. Two plasmids based on p2SC11 (48) were developed to insert the Gn/Gc ORF with (pΔTKGNGCγ) or without (pΔTKGNGC) the huIFNγ gene into the VACV TK gene. pT7-7 was digested with NcoI/EcoRI, resulting in a 3.4-kb fragment that was blunted with T4 DNA polymerase and subcloned into the SnaBI site of p2SC11 to generate p2SC11GNGC. The huIFNγ ORF, (Ultimate ORF Clone library; Invitrogen) was PCR-amplified with Vent DNA polymerase (New England Biolabs) with the primers: F:5′-AAAGCACCCGGGATGAAATATACA-3′ and R:5′-GAAAGCCCGGGTTACTGGGATGC-3′ (XmaI sites underlined), cloned into the unique XmaI site of p2SC11GnGc, and sequenced for integrity to generate pΔTKGnGcγ. This plasmid vector contains the lacZ gene under the VACV promoter P11, as a marker gene. pΔTKGnGc was developed by deleting half of the p2SC11 dsP using specifically designed 66-mer oligos (5′-GGCCGCTACGTAGAGCTCGAGCTTATTTATATTCCAAAAAAAAAAAATAAAATTTCAATTTTTAAC-3, and 5′-CCGGGTTAAAAATTGAAATTTTATTTTTTTTTTTTGGAATATAAATAAGCTCGAGCTCTACGTAGC-3′). The annealed oligos had an XmaI restriction site in the 5′ end and a NotI restriction site in the 3′ end and were subcloned into the XmaI/NcoI cut p2SC11 generating p1SC11. The Gn/Gc ORF was then subcloned into the unique SnaBI site of p1SC11 to generate pΔTKGNGC and sequenced. The transfer vector used to delete the B8R gene of VACV, pΔB8R, was developed by subcloning a blunted PSEL-gpt/GUS expression cassette into the blunted Kpn I site of pUCB8R (24, 49, 50).
Generation of rVACVs.
The intermediate rVACV, vCOΔB8R, with the B8R gene deleted, was generated by standard homologous recombination by transfection of pΔB8R into Vero cell monolayers infected with vCO at a multiplicity of infection (MOI) of 0.05. Transient dominant selection (20) was used to generate vCOΔB8R. The gpt/GUS-positive rVACVs were plaque-purified on Vero cells eight times with gpt selection medium (25 μg/mL mycophenolic acid, 250 μg/mL xanthine, 15 μg/m hypoxanthine); blue plaques were visualized with substrate 5-bromo-4-chloro-3-indolyl glucuronide (50). After four rounds of limiting dilution without selection, vCOΔB8R was confirmed free of vCO using standard PCR techniques. Primer pairs used to differentiate wild-type VACV from rVACVs were: F:5′-GCAGAGGGAAAATGCTATAAAGGA-3′ and R:5′-TGGAAATGCGGATATGTCGTATG-3′. The reverse primer is within the deleted B8R region, thus not amplifying rVACVs. The reverse primer R:5′-CACAACCCTATTTTCAATCCCCAT-3′, which spans the entire deleted regions, was used with the forward primer to distinguish rVACVs and parental VACVs by band size. The B8R region of vCOΔB8R was also sequenced to confirm integrity. vCOΔB8R was used as a parental VACV to develop vCOΔB8RTK−, vCOGnGc, and vCOGnGcγ. The rVACVs were generated using standard homologous recombination techniques with the transfer vectors pΔTK, pΔTKGnGc, or pΔTKGnGcγ transfected into Vero cell monolayers infected with an MOI of 0.05 of vCOΔB8R. rVACV plaques were visualized with 5-bromo-4-chloro-3-indolyl-d-galactopyranoside. The rVACVs were plaque-purified 12 times and confirmed free of wild-type virus using cytochemical staining for the presence of the lacZ marker gene, as previously described (48).
Protein Expression Characterization.
Gn and Gc expression by rVACVs was confirmed using Western blot analysis by standard procedures (35). Proteins were separated by SDS/PAGE (NuPAGE minigels; Invitrogen), transferred to a nylon membrane (Invitrogen iBlot system), and incubated with mouse anti-RVFV polyclonal serum (1:200 dilution). Proteins were visualized with an AP-conjugated goat anti-mouse IgG secondary antibody (1:2,000 dilution; Bio-RAD, cat# 170–6520). IFN-γ expression from VACVs was confirmed by ELISA by a commercial ELISA (huIFNγ ELISA Ready-SET-Go!, eBioScience); bioactivity of the cytokine was confirmed by an IFN-γ bioassay (47). Samples for both assays were obtained from BS-C-40 cells infected with rVACVs at a MOI of 10, incubated for 24 h, and supernatants filtered with 0.2-μm filters. Samples for the bioassay were serially diluted (1:3) in DMEM with 5% FBS and added to 96-well plates seeded with L929 cells. After 24 h, encephalomyocarditis virus (1 × 103 pfu) was added; cells were stained with Crystal violet 24 h later. IFN-γ titers (in units per milliliter) were expressed as the reciprocal of the dilution of sample that gave 50% protection against the challenge virus. Recombinant huIFNγ was obtained from R&D Systems (cat#285-IF/CF).
Safety Studies in Immunodeficient Mice.
C.B-17 SCID (C.B-Igh-1b/IcrTac-Prkdcscid) mice were purchased from Taconic. The animals were housed and used in accordance with the guidelines and approved protocols of the Institutional Animal Care and Use Committee and the Institutional Biosafety Committee at the University of California at Davis. Pock-lesion formation, weight-loss, and survival were measured in SCID mice (10 per group, 7- to 8-wk-old males) given 107 pfu i.p. of each rVACV in a final volume of 100 μL PBS. Mice were inoculated intraperitoneally with MP-12 (6.5 × 105 pfu). Animals were examined twice daily.
Vaccination and Challenge.
CB6F1 mice were purchased from Harlan Laboratories. Animals were housed and used in accordance with the guidelines and approved protocols of the Institutional Animal Care and Use Committee and the Institutional Biosafety Committee at the University of California at Davis (UC Davis) and University of Texas, Medical Branch, Galveston, TX (UTMB). Seven groups of CB6F1 mice (10 per group, 7- to 8-wk-old females) were vaccinated intramuscularly with 107 pfu of the respective rVACV, 6.5 × 105 pfu of MP-12, or PBS (mock). Mice were bled on day 0 and weeks 4, 8, 16, and 25. Three of the seven groups received a second intramuscular vaccination on week 8 of the same rVACV or MP-12. All groups were challenged intraperitoneally at week 22 after the primary vaccination with 103 pfu of the ZH501 strain of RVFV in a volume of 100 μL. Clinical signs and survival were monitored twice daily. Challenge studies were carried out in the animal biosafety level 4 laboratory at UTMB.
Plaque-Reduction Neutralization Tests.
RVFV PRNT80 assays for mouse sera after challenge were performed in the biosafety level 4 laboratory at UTMB, as previously described (51). The same procedure was used at UC Davis to analyze the prechallenge mouse and baboon sera. Briefly, duplicate samples of sera (50 μL) were diluted twofold and mixed with 70 pfu of MP-12 in 50 μL, incubated at 37 °C for 1 h, and then added to monolayers of Vero cells in 24-well plates. After 1 h at room temperature, the samples were removed, the plates overlaid with 1% agarose in medium, and incubated for 48 h at 37 °C in a 5% CO2 incubator. Plates were stained with Neutral red and the number of plaques counted 16 to 20 h later. The titer was recorded as the reciprocal of the highest serum dilution that reduced the number of plaques by 80% (PRNT80) compared with the negative-serum controls.
Baboon Studies.
Papio cynocephalus anubis baboons (n = 12) were obtained from the Oklahoma Baboon Research Resource at the University of Oklahoma Health Sciences Center (Gary White, Director). The baboons were female, ∼2 to 3 y old, and tuberculosis-free. The animals were housed and used in accordance with the guidelines and approved protocols of the Institutional Animal Care and Use Committee and the Institutional Biosafety Committee at the University of Oklahoma Health Sciences Center. Baboons were fasted overnight before each procedure, with free access to water. Baboons were sedated intramuscularly with a mix of ketamine (10 mg/kg) and acepromazine (1 mg/kg). Baseline serum samples were obtained before vaccination; scarification was performed in the middle of the back between the scapulae in accordance with the Centers for Disease Control protocol. This site was first shaved and cleaned with betadine and isopropanol. Using a bifurcated needle, ∼5 × 107 pfu of vCO, vCOGnGc, or vCOGnGcγ (four baboons per group) was inoculated by scarification. Blood samples and photographs of induced lesions were obtained on days 5, 10, 14, and 20. Once the pock lesions had resolved, blood samples were taken and all baboons were given an intramuscular booster immunization (109 pfu in 1 mL) on day 28. Blood samples were also obtained on days 35, 46, and 56. PRNT80 assays were performed as described above.
Statistics.
One-way ANOVA was used to determine the statistical significance between measurements obtained from different groups on any given day.
Acknowledgments
The authors thank Dr. Robert Tesh for antibodies to Rift Valley fever virus (RVFV) and the MP12 strain of RVFV; Dr. Michael Parker for pT7-7 containing the M segment of RVFV; and members of the International Laboratory of Molecular Biology for Tropical Disease Agents, especially S. Liu, S. Yim, and T. DiManno for their assistance. This work was supported by Department of Homeland Security Subcontract N00014-04-1-0660 (Texas A & M, Foreign Animal and Zoonotic Disease Defense Center) (to T.D.Y.); National Institutes of Health Grant ARRA1089460 (to T.D.Y.); and National Institutes of Health Grant 5P40RR012317 (to Dr. Gary L. White PI/Director of the Oklahoma Baboon Research Resource and J.F.P., Co-Investigator), which helped fund the baboon work.
Footnotes
The authors declare no conflict of interest.
References
- 1.Fauquet C. Virus Taxonomy: Classification and Nomenclature of Viruses: Eighth Report of the International Committee on the Taxonomy of Viruses. San Diego, CA: Elsevier Academic Press; 2005. pp viii, 1259 pp. [Google Scholar]
- 2.Fields BN, Knipe DM, Howley PM. Fields Virology. 5th Ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 3.Giorgi C, et al. Sequences and coding strategies of the S RNAs of Toscana and Rift Valley fever viruses compared to those of Punta Toro, Sicilian Sandfly fever, and Uukuniemi viruses. Virology. 1991;180(2):738–753. doi: 10.1016/0042-6822(91)90087-r. [DOI] [PubMed] [Google Scholar]
- 4.Collett MS. Messenger RNA of the M segment RNA of Rift Valley fever virus. Virology. 1986;151(1):151–156. doi: 10.1016/0042-6822(86)90114-5. [DOI] [PubMed] [Google Scholar]
- 5.Collett MS, et al. Complete nucleotide sequence of the M RNA segment of Rift Valley fever virus. Virology. 1985;144(1):228–245. doi: 10.1016/0042-6822(85)90320-4. [DOI] [PubMed] [Google Scholar]
- 6.Müller R, Poch O, Delarue M, Bishop DH, Bouloy M. Rift Valley fever virus L segment: Correction of the sequence and possible functional role of newly identified regions conserved in RNA-dependent polymerases. J Gen Virol. 1994;75(6):1345–1352. doi: 10.1099/0022-1317-75-6-1345. [DOI] [PubMed] [Google Scholar]
- 7.Zamoto-Niikura A, Terasaki K, Ikegami T, Peters CJ, Makino S. Rift valley fever virus L protein forms a biologically active oligomer. J Virol. 2009;83(24):12779–12789. doi: 10.1128/JVI.01310-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daubney R, Hudson JR, Garnham PC. Enzootic hepatitis or Rift Valley fever. An undescribed virus disease of sheep cattle and man from East Africa. J Path Bact. 1931;34(2):545–579. [Google Scholar]
- 9.Easterday BC. Rift Valley fever. Adv Vet Sci. 1965;10:65–127. [PubMed] [Google Scholar]
- 10.Coetzer JA. The pathology of Rift Valley fever. I. Lesions occurring in natural cases in new-born lambs. Onderstepoort J Vet Res. 1977;44(4):205–211. [PubMed] [Google Scholar]
- 11.Madani TA, et al. Rift Valley fever epidemic in Saudi Arabia: Epidemiological, clinical, and laboratory characteristics. Clin Infect Dis. 2003;37(8):1084–1092. doi: 10.1086/378747. [DOI] [PubMed] [Google Scholar]
- 12.Birtch SC, Linthicum KJ. Developing a research agenda and a comprehensive national prevention and response plan for Rift Valley fever in the United States. Emerg Infect Dis. 2007;13 Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2828099/ [Google Scholar]
- 13.Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J Am Vet Med Assoc. 2009;234(7):883–893. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- 14.Smithburn KC. Rift Valley fever; The neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br J Exp Pathol. 1949;30(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 15.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66(10):2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 16.Vialat P, Muller R, Vu TH, Prehaud C, Bouloy M. Mapping of the mutations present in the genome of the Rift Valley fever virus attenuated MP12 strain and their putative role in attenuation. Virus Res. 1997;52(1):43–50. doi: 10.1016/s0168-1702(97)00097-x. [DOI] [PubMed] [Google Scholar]
- 17.Verardi PH, et al. Long-term sterilizing immunity to rinderpest in cattle vaccinated with a recombinant vaccinia virus expressing high levels of the fusion and hemagglutinin glycoproteins. J Virol. 2002;76(2):484–491. doi: 10.1128/JVI.76.2.484-491.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yilma T, et al. Inexpensive vaccines and rapid diagnostic kits tailor-made for the global eradication of rinderpest, and technology transfer to Africa and Asia. Dev Biol (Basel) 2003;114:99–111. [PubMed] [Google Scholar]
- 19.Mackett M, Smith GL, Moss B. Vaccinia virus: A selectable eukaryotic cloning and expression vector. Proc Natl Acad Sci USA. 1982;79(23):7415–7419. doi: 10.1073/pnas.79.23.7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Falkner FG, Moss B. Transient dominant selection of recombinant vaccinia viruses. J Virol. 1990;64(6):3108–3111. doi: 10.1128/jvi.64.6.3108-3111.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakrabarti S, Sisler JR, Moss B. Compact, synthetic, vaccinia virus early/late promoter for protein expression. Biotechniques. 1997;23(6):1094–1097. doi: 10.2144/97236st07. [DOI] [PubMed] [Google Scholar]
- 22.Yilma T. Genetically engineered vaccines for animal viral diseases. J Am Vet Med Assoc. 1994;204(10):1606–1615. [PubMed] [Google Scholar]
- 23.Yilma T, McGuire TC, Perryman LE. Preliminary characterization of equine interferons and their antiviral activities on bovine, ovine, and human cells. J Interferon Res. 1982;2(3):363–370. doi: 10.1089/jir.1982.2.363. [DOI] [PubMed] [Google Scholar]
- 24.Verardi PH, Jones LA, Aziz FH, Ahmad S, Yilma TD. Vaccinia virus vectors with an inactivated gamma interferon receptor homolog gene (B8R) are attenuated In vivo without a concomitant reduction in immunogenicity. J Virol. 2001;75(1):11–18. doi: 10.1128/JVI.75.1.11-18.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Niklasson BS, Meadors GF, Peters CJ. Active and passive immunization against Rift Valley fever virus infection in Syrian hamsters. Acta Pathol Microbiol Immunol Scand [C] 1984;92(4):197–200. doi: 10.1111/j.1699-0463.1984.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 26.Dungu B, et al. Evaluation of the efficacy and safety of the Rift Valley Fever Clone 13 vaccine in sheep. Vaccine. 2010;28(29):4581–4587. doi: 10.1016/j.vaccine.2010.04.085. [DOI] [PubMed] [Google Scholar]
- 27.Pittman PR, et al. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: A 12-year experience. Vaccine. 1999;18(1–2):181–189. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- 28.Schmaljohn CS, et al. Baculovirus expression of the M genome segment of Rift Valley fever virus and examination of antigenic and immunogenic properties of the expressed proteins. Virology. 1989;170(1):184–192. doi: 10.1016/0042-6822(89)90365-6. [DOI] [PubMed] [Google Scholar]
- 29.Näslund J, et al. Vaccination with virus-like particles protects mice from lethal infection of Rift Valley Fever Virus. Virology. 2009;385(2):409–415. doi: 10.1016/j.virol.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 30.Spik K, et al. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine. 2006;24(21):4657–4666. doi: 10.1016/j.vaccine.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 31.Wallace DB, et al. Protective immune responses induced by different recombinant vaccine regimes to Rift Valley fever. Vaccine. 2006;24(49–50):7181–7189. doi: 10.1016/j.vaccine.2006.06.041. [DOI] [PubMed] [Google Scholar]
- 32.Collett MS, et al. Protective subunit immunogens to Rift Valley fever virus from bacteria and recombinant vaccinia virus. In: Mahy BWJ, Kolakofsky D, editors. Biology of Negative Strand Viruses. Amsterdam: Elsievier Science Publishers; 1987. pp. 321–329. [Google Scholar]
- 33.Buller RM, Smith GL, Cremer K, Notkins AL, Moss B. Decreased virulence of recombinant vaccinia virus expression vectors is associated with a thymidine kinase-negative phenotype. Nature. 1985;317(6040):813–815. doi: 10.1038/317813a0. [DOI] [PubMed] [Google Scholar]
- 34.Chan KS, Verardi PH, Legrand FA, Yilma TD. Nef from pathogenic simian immunodeficiency virus is a negative factor for vaccinia virus. Proc Natl Acad Sci USA. 2005;102(24):8734–8739. doi: 10.1073/pnas.0503542102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giavedoni LD, et al. Vaccinia virus recombinants expressing chimeric proteins of human immunodeficiency virus and gamma interferon are attenuated for nude mice. Proc Natl Acad Sci USA. 1992;89(8):3409–3413. doi: 10.1073/pnas.89.8.3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones L, et al. Enhanced safety and efficacy of live attenuated SIV vaccines by prevaccination with recombinant vaccines. J Med Primatol. 2000;29(3–4):231–239. doi: 10.1034/j.1600-0684.2000.290316.x. [DOI] [PubMed] [Google Scholar]
- 37.Jones L, Tenorio E, Gorham J, Yilma T. Protective vaccination of ferrets against canine distemper with recombinant pox virus vaccines expressing the H or F genes of rinderpest virus. Am J Vet Res. 1997;58(6):590–593. [PubMed] [Google Scholar]
- 38.Legrand FA, et al. Induction of potent humoral and cell-mediated immune responses by attenuated vaccinia virus vectors with deleted serpin genes. J Virol. 2004;78(6):2770–2779. doi: 10.1128/JVI.78.6.2770-2779.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Earl PL, et al. Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature. 2004;428(6979):182–185. doi: 10.1038/nature02331. [DOI] [PubMed] [Google Scholar]
- 40.Moss B. Genetically engineered poxviruses for recombinant gene expression, vaccination, and safety. Proc Natl Acad Sci USA. 1996;93(21):11341–11348. doi: 10.1073/pnas.93.21.11341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ober BT, et al. Immunogenicity and safety of defective vaccinia virus lister: Comparison with modified vaccinia virus Ankara. J Virol. 2002;76(15):7713–7723. doi: 10.1128/JVI.76.15.7713-7723.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor J, et al. Nonreplicating viral vectors as potential vaccines: Recombinant canarypox virus expressing measles virus fusion (F) and hemagglutinin (HA) glycoproteins. Virology. 1992;187(1):321–328. doi: 10.1016/0042-6822(92)90321-f. [DOI] [PubMed] [Google Scholar]
- 43.Hunter P, Erasmus BJ, Vorster JH. Teratogenicity of a mutagenised Rift Valley fever virus (MVP 12) in sheep. Onderstepoort J Vet Res. 2002;69(1):95–98. [PubMed] [Google Scholar]
- 44.Saluzzo JF, Smith JF. Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine. 1990;8(4):369–375. doi: 10.1016/0264-410x(90)90096-5. [DOI] [PubMed] [Google Scholar]
- 45.Bird BH, et al. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J Virol. 2008;82(6):2681–2691. doi: 10.1128/JVI.02501-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pepin M, Bouloy M, Bird BH, Kemp A, Paweska J. Rift Valley fever virus (Bunyaviridae: Phlebovirus): An update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet Res. 2010;41(6):61. doi: 10.1051/vetres/2010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Legrand FA, et al. Vaccinia viruses with a serpin gene deletion and expressing IFN-gamma induce potent immune responses without detectable replication in vivo. Proc Natl Acad Sci USA. 2005;102(8):2940–2945. doi: 10.1073/pnas.0409846102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chakrabarti S, Brechling K, Moss B. Vaccinia virus expression vector: Coexpression of beta-galactosidase provides visual screening of recombinant virus plaques. Mol Cell Biol. 1985;5(12):3403–3409. doi: 10.1128/mcb.5.12.3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cao JX, Upton C. gpt-gus fusion gene for selection and marker in recombinant poxviruses. Biotechniques. 1997;22(2):276–278. doi: 10.2144/97222bm17. [DOI] [PubMed] [Google Scholar]
- 50.Hammond JM, Oke PG, Coupar BE. A synthetic vaccinia virus promoter with enhanced early and late activity. J Virol Methods. 1997;66(1):135–138. doi: 10.1016/s0166-0934(97)00045-1. [DOI] [PubMed] [Google Scholar]
- 51.Mandell RB, et al. A replication-incompetent Rift Valley fever vaccine: Chimeric virus-like particles protect mice and rats against lethal challenge. Virology. 2010;397(1):187–198. doi: 10.1016/j.virol.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]