Abstract
Objective
Pressures on academic faculty to perform beyond their role as educators has stimulated interest in complementary approaches in resident medical education. While fellows are often believed to detract from resident learning and experience, we describe our preliminary investigations utilizing clinical fellows as a positive force in pediatric resident education. Our objectives were to implement a practical approach to engage fellows in resident education, evaluate the impact of a fellow-led education program on pediatric resident and fellow experience, and investigate if growth of a fellowship program detracts from resident procedural experience.
Methods
This study was conducted in a neonatal intensive care unit (NICU) where fellows designed and implemented an education program consisting of daily didactic teaching sessions before morning clinical rounds. The impact of a fellow-led education program on resident satisfaction with their NICU experience was assessed via anonymous student evaluations. The potential value of the program for participating fellows was also evaluated using an anonymous survey.
Results
The online evaluation was completed by 105 residents. Scores were markedly higher after the program was implemented in areas of teaching excellence (4.44 out of 5 versus 4.67, p<0.05) and overall resident learning (3.60 out of 5 versus 4.61, p<0.001). Fellows rated the acquisition of teaching skills and enhanced knowledge of neonatal pathophysiology as the most valuable aspects of their participation in the education program. The anonymous survey revealed that 87.5% of participating residents believed that NICU fellows were very important to their overall training and education.
Conclusions
While fellows are often believed to be a detracting factor to residency training, we found that pediatric resident attitudes toward the fellows were generally positive. In our experience, in the specialty of neonatology a fellow-led education program can positively contribute to both resident and fellow learning and satisfaction. Further investigation into the value of utilizing fellows as a positive force in resident education in other medical specialties appears warranted.
Keywords: resident education, fellow teaching, pediatrics
The traditional model of medical education gives the attending physician the primary responsibility for resident teaching (1). However, pressure on faculty at academic centers to increase scholarly productivity, maintain a high level of clinical care and documentation, and generate relative-value units limits opportunities for faculty-led teaching activities (2). Furthermore, with ongoing restrictions to resident work hours potentially curtailing clinical experience, alternative strategies to enhance both the quality and efficiency of resident education are needed (3–5).
In the United States there are growing numbers of medical residents undergoing additional postgraduate training in subspecialty fields, commonly referred to as ‘fellows’ (6). Fellows are expected to contribute positively to the academic productivity of the department, share on-call responsibilities, provide a high level of patient care and teach residents and medical students. However, there is evidence from adult residency programs that fellows may, in fact, detract from resident education and experience (7). To date, no studies have investigated the impact of an increasing ‘fellow’ presence on pediatric resident education.
The American College of Graduate Medical Education (ACGME) requires that fellowship programs provide fellows with an opportunity to enhance their teaching skills throughout their training (8). However, the best methods to incorporate fellows into pediatric resident education, and the impact on resident experience, have not been previously explored. Here we describe our preliminary investigations using fellows, in a clearly defined teaching role, as a positive force in pediatric resident education. We hypothesized that fellows’ efforts to improve resident educational experiences will be positively received by pediatric residents; utilizing fellows as teachers improves the educational experience for residents and fellows; and the growth of a fellowship program does not detract from resident clinical and procedural experience.
At our academic institution, the neonatal intensive care unit (NICU) rotation in 2007–2008 was rated by pediatric residents as one of the least positive during the course of their training (ranked 65th out of 67 possible rotations, bottom 5%). In particular, residents poorly rated the rotation for overall teaching and education. This finding is consistent with previous literature showing that the complex learning environment of the NICU, including high patient acuity and resident workload, often limits opportunities for formal resident education (9). Thus the NICU rotation represented an area of residency training with tremendous opportunity for positive change and an ideal setting to implement a fellow-led education program.
Methods
This study was conducted at a large Midwestern academic institution. The pediatric residency program at our institution trains over 40 residents per year, with modules in general pediatrics and combined medicine-pediatric pathways. The hospital also supports one of the largest NICUs in the country, with 168 neonatal beds and 15 board-certified neonatology faculty.
Prior to 2009, resident teaching responsibilities in the NICU were placed solely on faculty during their clinical care (‘ward’) month, with no formal involvement from neonatology fellows. In light of poor resident satisfaction with their NICU experiences in the 2007 and 2008 academic years, the NICU fellows were invited by faculty to design and implement an education program at the beginning of the 2009 academic year. The basic tenet of the fellow-led program was to improve the resident educational experience in the NICU. Additional goals, as outlined in collaboration with participating faculty, were to provide fellows with an opportunity to develop and enhance their teaching skills and promote interest in a career in academic medicine and teaching. Faculty believed that participation in this program would provide a practical introduction for fellows in creating an interactive learning environment for medical education. Although all fellows in our program had successfully graduated from pediatric residency programs and expressed interest in teaching residents, none had prior experience in formal classroom instruction.
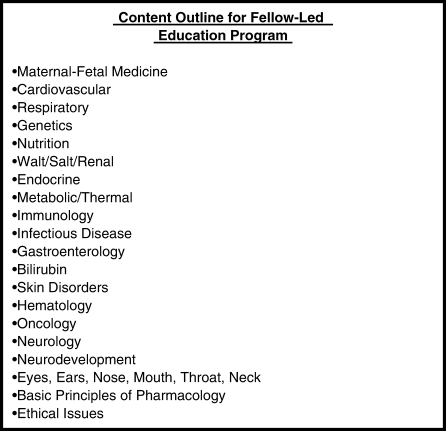
Development and implementation of the fellow-led educational program
Prior to the start of the program, the fellows met with faculty to develop learning objectives for the educational series (Fig. 1). The objectives were based on topics outlined by the American Academy of Pediatrics (AAP) on the care of the newborn and fetus. In addition, the fellows created an institutional database of NICU-related questions to be used during teaching sessions (10). The questions were developed to guide the content of discussion and stimulate the learning environment. For a given month, individual fellows typically were assigned two to four learning topics. At each session, fellows were expected to review current literature on their respective topic, with the goal of promoting active discussion and exchange of information with the residents. Although each session had specific teaching content to be addressed, the lectures were designed to be interactive, with the goal of providing residents with enough time to ask questions. The daily sessions were conducted before morning NICU rounds and typically lasted 45 to 60 minutes. Faculty were available to review learning objectives, clarify conflicting evidence in the literature on a particular topic and provide insight on strategies to teach the residents more effectively in a classroom setting. The education program was a natural by-product of the growing fellowship presence at our institution, with the total number of neonatology fellows increasing from four in 2007 to eight in 2009.
Fig. 1.
Content outline for fellow-led education program.
Source: Adapted from AAP 2008 guidelines on the care of the newborn and fetus.
We employed four strategies, itemized here, to evaluate the potential value of the fellow-led education program on resident and fellow satisfaction and experience.
Assessment of resident perceptions of the NICU rotation
Following institutional requirements for resident graduation, and consistent with recommendations provided by the ACGME, residents completed a rotation evaluation at the end of their NICU rotation. This generalized evaluation is completed online (E-value, Minneapolis, MN). The questions included the following items.
Did the organization of the rotation facilitate your learning?
Were the rotation's expectations clear to you during the month?
Was the rotation well organized?
Was the rotation valuable for your development as a general pediatrician?
Rate the overall teaching excellence in the rotation.
Responses were reported using a categorical variable scale ranging from one to five (1=strongly disagree; 2=somewhat disagree; 3=neutral; 4=somewhat agree; 5=strongly agree).
Responses were maintained in a confidential manner by the residency program. Scores on the evaluation were assessed over three consecutive academic years (2007–2009) to evaluate the potential impact of the 2009 fellow-led program on resident responses. Residents are assigned to this rotation only once during their training, thus minimizing the chance of repeat responses before and after program implementation. The E-value online tool we used in the assessment of resident satisfaction with their NICU rotation represents a standardized method for evaluating resident experience that has been in place at our institution since 2005. Data were also obtained on age and practice plans following completion of pediatric training over the 2007–2009 academic years.
Assessment of fellow perceptions on participating in the education program
Fellows completed an anonymous survey that addressed the usefulness of their participation in the program. Fellows respondents rated the educational value across four areas (understanding of basic neonatal pathophysiology, preparation for specialty board examinations, enhancement of teaching skills and enhancement of clinical skills) using a five-point scale (1=little or no value, 3=moderate value, 5=great value). An assessment of the overall educational experience of participation in the program was conducted by asking fellows to rate the following statements: education program should continue next year; time devoted to course was acceptable given benefits; greater interest in neonatal pathophysiology; increased interest in career in academic medicine; faculty interaction was viewed positively; resident feedback was viewed positively. Responses were evaluated using a five-point scale (1=strongly agree, 3=unsure/neutral, 5=strongly agree). This survey was adapted from a previously published survey instrument (11).
Assessment of resident-fellow relationship in the NICU
A separate and unique voluntary survey was designed to assess the relationship between pediatric residents and fellows in the setting of a growing fellow presence at our institution. The survey was sent to residents following completion of their NICU rotation. Data from this survey were only available during the 2009 academic year. The survey consisted of the following statements.
The NICU fellows were very effective teachers.
The NICU fellows were interested in your learning and development.
The NICU fellows did not compete or limit your ability to perform procedures.
The distinction of clinical responsibilities between you and the NICU fellows was very clear.
Overall, the NICU fellows were very important to your NICU training.
Responses were reported using a categorical variable ranging from one to five (as described above). The survey we used was adapted from a previously validated survey on fellow-resident interactions (12).
Assessment of the impact of increasing number of neonatology fellows on resident procedural experience in the NICU
In line with ACGME requirements, our institution maintains a database of all procedures performed by residents throughout their pediatric training. A review of the resident procedural case-logs during the neonatology rotation from 2007 to 2009 was performed. We calculated the total number of procedures performed by residents during their neonatology rotation in five primary areas of procedural competency: endotracheal intubation; umbilical arterial catheter (UAC); umbilical venous catheter (UVC); arterial puncture; and lumbar puncture. The total number of procedures was divided by the number of residents, which provided an index of the average number of procedures per resident for any given year.
Data analyses
Responses on the resident rotation evaluation (Fig. 2) were assessed using a Mann-Whitney test. Responses to the fellow survey on the usefulness of their participation in the education program were described by their mean and standard deviation (Fig. 3). Responses to the resident survey on resident-fellow interactions were described by their overall percentile (Fig. 4). The sample size was one of convenience and represented all residents who completed the NICU rotation over the years 2007–2009. The sample size was not powered to answer specific hypothetical questions.
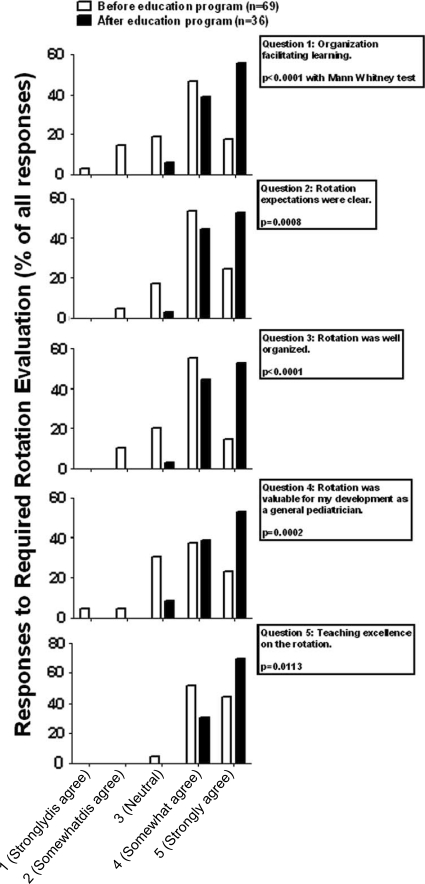
Fig. 2.
Resident rotation evaluation: improved resident satisfaction after program implementation.
Note: At the end of their NICU rotation, residents (N=105; 69 before education program and 36 after program) completed an online evaluation (E-value). Scores 1=strongly disagree; 2=somewhat disagree; 3=neutral; 4=somewhat agree; and 5=strongly agree. Unpaired t-test with Mann-Whitney was performed on average score for each of five possible questions.
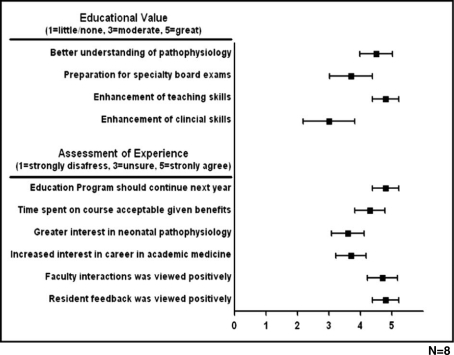
Fig. 3.
Fellow survey: positive responses from fellows regarding participation in the education program.
Note: All eight NICU fellows in the education program completed the online survey at the end of the 2009 academic year following one year of teaching responsibilities (100% response rate). Responses to questions on the educational value of the program were reported using a categorical variable ranging from 1 to 5 (1=little or no value, 3=moderate value, 5=great value). Responses to questions on the overall experience of participating in the program were evaluated using a five-point scale (1=strongly disagree, 3=unsure/neutral, 5=strongly agree).
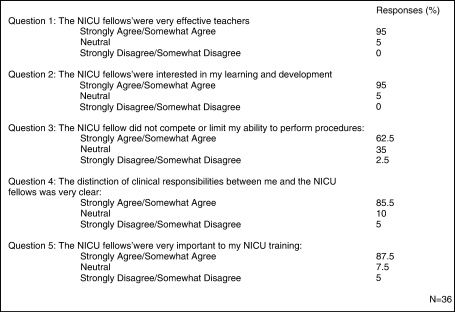
Fig. 4.
Survey of resident-fellow interaction: positive responses from residents regarding the resident-fellow relationship in the NICU.
Note: Thirty-six residents completed the online survey at the end of the 2009 academic year (36 out of a possible 40, 90% response rate). Responses were reported using a categorical variable ranging from one to five (1=strongly disagree; 2=somewhat disagree; 3=neutral; 4=somewhat agree; 5=strongly agree).
Results
General implementation
The neonatology fellows invested over 300 hours in resident teaching during the 2009 academic year. All NICU fellows (N=8) actively participated in all aspects of the program's development and implementation. Five faculty members in the field of neonatology were involved in the development of the AAP-based curriculum and provided constant oversight throughout the process. A review of the program revealed that less than 5% of scheduled lessons were cancelled due to resident, fellow or faculty conflict.
Resident perceptions
Over the course of the three academic years in review, responses were available from 105 of 113 residents who completed the NICU rotation (92.9% response rate). Demographics between the two groups of residents before and after program implementation were similar with respect to age, gender, race and future plans. Specifically, a similar number of residents before and after the program planned on pursuing a NICU fellowship following graduation (12% before program versus 11% after program).
Fig. 2 shows the perceptions of residents on the NICU rotation before and after the fellow-led education program was initiated. On the overall rotation evaluation, mean scores between the cohorts were markedly improved after program implementation for all questions posed. Specifically, when asked if the organization of the rotation facilitated their learning (question 1), residents in the NICU responded with a mean score of 3.60 out of 5 before the education program and a mean score of 4.51 out of 5 after initiation of the program (p<0.001). When asked if the rotation expectations were clear during their NICU month (question 2) and the rotation was well organized (question 3), residents’ response improved from mean scores of 4.00 and 3.74 before implementation of the program to mean scores of 4.50 and 4.60 after its initiation (p<0.001 and p<0.001, respectively). Of note, when asked about the value of the NICU rotation for their development as a general pediatrician (question 4), there was a significantly higher score among residents exposed to the education program than among those completing their NICU rotation before the program's introduction, with the mean score improving from 3.71 to 4.44 (p<0.001). Finally, when residents rated the overall teaching excellence during their NICU rotation, scores were higher after the program was in place, with mean scores improving from 4.44 to 4.67 (p<0.05).
Fellow perceptions
Fig. 3 shows responses from neonatology fellows on the educational value and overall benefits of their participating in the program. All NICU fellows who participated in the program provided responses. Fellows rated the development of teaching skills and improved understanding of neonatal pathophysiology as the most valuable aspects of participation. Nearly all the fellows (88%) noted that the education program was of ‘great value’ in improving their teaching skills. Additionally, a majority (88%) believed that the program should continue next year. Interestingly, despite the considerable amount of time spent in developing and implementing the program, most fellows (63%) responded that they ‘strongly agree’ this effort was acceptable given the mutual benefits to residents and fellows.
Resident satisfaction with their interactions with neonatology fellows
A separate, voluntary survey was conducted to assess resident attitudes toward the growing NICU fellow presence at our institution (Fig. 4). Results on the anonymous survey were available from 36 out of a possible 40 residents (90% response rate). When asked questions about NICU fellows’ effectiveness as teachers and interest in resident learning and development, over 95% of residents responded positively (strongly agree/somewhat agree). However, only 62.5% strongly agreed or somewhat agreed with the statement ‘The NICU fellows did not compete or limit your ability to perform procedures.’ Interestingly, when asked if the distinction of clinical responsibilities between resident and NICU fellow was clear, 85.5% responded positively. Finally, when asked if the NICU fellows were very important to their overall NICU training and education, 87.5% responded positively, with only 5% of residents reporting a negative influence of NICU fellows on their training.
Impact of neonatology fellows on resident procedural experience in the NICU
Table 1 shows resident procedural case-logs from 2007 through 2009. We calculated the total number of procedures performed by residents during their neonatology rotation in five primary areas of procedural competency (intubation, UAC, UVC, arterial puncture, lumbar puncture). Despite an increase in the number of neonatology fellows from four in 2007 to eight in 2009, the NICU procedures per resident did not change in any of the core areas we reviewed.
Table 1.
Resident procedural experience in setting of increasing number of neonatology fellows
| Procedure (average/resident) | 2007 | 2008 | 2009 |
|---|---|---|---|
| Intubation | 4.8 | 4.7 | 4.4 |
| UAC insertion | 2.6 | 2.5 | 2.4 |
| UVC insertion | 4.3 | 4.5 | 4.4 |
| Arterial puncture | 6.2 | 6.4 | 6.5 |
| Lumbar puncture | 5.4 | 5.6 | 5.9 |
Notes:
Total residents: N=113.
Number of NICU fellows=4 (2007 academic year); 4 (2008 academic year); 8 (2009 academic year).
Discussion
In light of restrictions to resident work hours potentially limiting clinical exposure, as well as increased demands on academic faculty outside their role as teachers, efforts to develop complementary models of residency education are well founded (3–5, 13). The role of fellows as a positive force in pediatric resident education may offer advantages for residents, fellows and faculty; however, the best methods to organize and accomplish this have received little attention until now. Here, we described our initial efforts to use fellows in a defined teaching role to optimize resident educational experience.
At our institution, the NICU rotation in 2007–2008 was rated by pediatric residents as one of the least favorable during the course of their pediatric training (65th out of 67 possible rotations, bottom 5%). In an effort to improve resident satisfaction in the NICU rotation, a fellow-led education program was initiated in 2009. We found that this approach, although requiring a time investment from faculty and fellows in planning, was generally easy to implement. Prior to the program's induction, meetings of fellows and faculty helped to define the content and format for the program. This effort not only provided stability of teaching content, but also gave an opportunity for fellows to interact positively with potential faculty mentors.
The success of the fellow-led education program on resident educational experience is shown by improvements across multiple areas of resident satisfaction (Fig. 2). Not surprisingly, these results corresponded with an overall improvement in the residents’ review of the NICU rotation during the 2009 academic year to 26th out of 67 rotations – a marked improvement from previous years. Importantly, the benefits of the educational program were not limited to residents, as fellows also rated the overall experience favorably. Specifically, fellows noted the acquisition of teaching skills and enhanced knowledge of neonatal pathophysiology as among the most useful aspects of their participation (Fig. 3).
Considering that the fellow-led education program represented a new initiative in our NICU, the number of teaching hours between faculty and residents did not change with its inception. Of note (personal communication), many faculty reported that the program allowed them to direct their resident teaching efforts to more advanced topics, with the understanding that the basic tenets are being taught by the fellows. As such, we feel that the education program not only enhanced resident-fellow interaction, but also likely supported teaching efforts between residents and faculty.
This is the first study to evaluate the potential value of utilizing pediatric fellows in resident medical education. In contrast to previous work reporting that a strong fellow presence may dilute the educational experience for residents, the present study found that NICU fellows being active in a defined teaching role results in an increased level of resident satisfaction with their NICU experience (14, 15). An unexpected effect was that residents almost uniformly responded that NICU fellows were ‘very important’ to their overall training in the NICU (87.5% positive response).
The importance of fellows accepting a teaching role in residency education is becoming more recognized. The ACGME program requirements in neonatology identify teaching skills among a group of core competencies that fellows must become effective at during their training (8). However, recent evidence suggests that fellows are considered the primary personnel responsible for resident supervision and education in the NICU less than 15% of the time (1). In our study, it is notable that over 95% of residents responded positively (strongly agree or somewhat agree) when asked about the effectiveness of the NICU fellows as teachers and the fellows’ interest in their learning and education.
Results of the fellow survey suggest that development of a structured educational program provides fellows with the opportunity to enhance their teaching skills and develop their understanding of basic pathophysiology within their discipline. We believe the fellow-led program provides a potential model for fellows to fulfill the ACGME requirement for teaching, and that broad participation by fellows in a leadership role enhances the depth and quality of the educational experience of the fellows. This suggests that the traditional model of education, one that places neonatology faculty as the sole teachers in the NICU, may be significantly enhanced by the incorporation of fellows into existing educational paradigms.
The resident survey provides information on potential competition between fellows and residents for procedures, a common challenge in procedure-oriented practices such as neonatology. Despite a majority of residents responding that fellows do not compete or limit their ability to perform procedures in the NICU, over 35% had a negative (somewhat disagree/strongly disagree) or neutral response to the question. However, despite an increase in the number of neonatology fellows from four to eight, the NICU procedures documented by residents did not change over the three-year period in review (Table 1). This suggests that while the actual number of NICU procedures performed by the residents has not changed with the growth of the fellowship program, there is an underlying perception by some residents of competition with fellows for procedures. This finding is consistent with previous literature showing that residents often perceive fellows as detractors from their procedural experience (7). Therefore, program directors must clearly define the program's expectations for resident involvement in procedures, as well as discussing the role of fellows in supporting and supervising residents in achieving procedural competency. Although over 85% of residents answered positively (strongly agree/somewhat agree) to the question regarding distinction of clinical responsibilities between the resident and fellows, we believe that the maintenance of clear and consistent guidelines for procedural responsibilities is also warranted.
It is important to address the limitations of the present study. First, we recognize that these data represent the opinions of resident physicians from a single academic institution, and regional and national differences may exist. However, as the first to address this issue in the pediatric literature, we hope our findings will be the springboard for future scholarly investigation into the potential role of fellows in pediatric resident education. Second, the success of a fellow-led education program relies heavily on the interest, enthusiasm and commitment of fellows to teaching. Given the relatively large size of our neonatology fellowship program this was not a major obstacle for implementation, although such barriers may become more apparent in smaller programs. Third, we cannot account for the fact that improvements in resident satisfaction on the survey can be partly explained by the increased number of NICU fellows from four in 2007 to eight in 2009, such that more opportunities for resident-fellow interaction in the NICU improved the residents’ overall experience with the rotation. However, only one NICU fellow was assigned to clinical care duties in the NICU at any given time from 2007 to 2009. To that end, while the number of total NICU fellows increased, the number assigned to clinical care duties with the pediatric residents remained unchanged.
It is also important to recognize that while fellows had faculty oversight throughout the development and implementation of the educational series, there was no formal assessment of the fellows’ performance as teachers. We are currently developing an evaluation process (scheduled to be implemented in July 2011) wherein both faculty and residents evaluate the fellows’ overall teaching effectiveness and provide feedback on ways to refine their teaching skills. We believe this effort will allow fellows to maximize their teaching abilities.
The resident survey provides valuable information on resident-fellow interaction in the setting of a growing fellow presence at our institution. However, data from the NICU survey were only available during the 2009 academic year, thus we are not able to evaluate changes in resident opinion on the survey before and after the education program was in place. Additionally, while we have shown that the residents’ perceptions of their NICU educational experience markedly improved with the new educational model, the ultimate measure of the efficacy of this approach will be the knowledge and competency of these residents as they become pediatricians in the community.
To our knowledge this is the first study to address the impact of a fellow-led education program on pediatric resident education. In summary, our findings support the concept that utilizing fellows in a defined teaching role results in an increased level of resident satisfaction with their educational experience. Also, such educational models provide fellows with an opportunity to develop teaching skills, consistent with the ACGME's practice-based iearning and improvement competencies for fellowship training programs (8). While such efforts require cooperation and coordination between residency and fellowship program personnel in design and implementation, there are clear benefits for residents, fellows and faculty. Further refinement and evaluation of this teaching model, an investigation of this approach in other medical subspecialties and a more rigorous assessment of educational outcomes are warranted.
Disclosures
No conflicts of interest or corporate sponsors to disclose.
References
- 1.Halamek LP, Kaegi DM. Who's teaching neonatal resuscitation to housestaff? Results of a national survey. Pediatrics. 2001;107:249–55. doi: 10.1542/peds.107.2.249. [DOI] [PubMed] [Google Scholar]
- 2.Marusic B. Academic medicine: one job or three? Croat Med J. 2004;45:243–4. [PubMed] [Google Scholar]
- 3.Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288:1112–4. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 4.Charap M. Reducing resident work hours: unproven assumptions and unforeseen outcomes. Ann Intern Med. 2004;140:814–5. [PubMed] [Google Scholar]
- 5.Sectish TC, Zalneraitis EL, Carraccio C, Behrman RE. The state of pediatrics residency training: a period of transformation of graduate medical education. Pediatrics. 2004;114:832–41. doi: 10.1542/peds.2004-0088. [DOI] [PubMed] [Google Scholar]
- 6.Pediatric Fellowships: American Academcy of Pediatrics. 2011. Available from: www.aap.org/sections/peds_fellowships.
- 7.Grober ED, Elterman DS, Jewett MA. Fellow or foe: the impact of fellowship training programs on the education of Canadian urology residents. Can Urol Assoc J. 2008;2:33–7. doi: 10.5489/cuaj.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ACGME program requirements for neonatal-perinatal medicine. 2007. Available from: www.aap.org/perinatal/ACGMENeonatal-PerinatalFellowshipGuidelines.pdf.
- 9.Griffith CH, III, Wilson JF, Rich EC, Pauly TH. House staff supervision, workload, and experience in the neonatal intensive care unit: results of a national survey. J Pediatr. 1998;132:889–91. doi: 10.1016/s0022-3476(98)70327-0. [DOI] [PubMed] [Google Scholar]
- 10.American Board of Pediatrics. Content outline in neonatal-perinatal medicine. 2010. Available from: https://www.abp.org/abpwebsite/certinfo/subspec/suboutlines/neon2010.pdf.
- 11.Kempainen RR, Hallstrand TS, Culver BH, Tonelli MR. Fellows as teachers: the teacher-assistant experience during pulmonary subspecialty training. Chest. 2005;128:401–6. doi: 10.1378/chest.128.1.401. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein AR, Reidy K, Norwood VF, Mahan JD. Factors influencing pediatric nephrology trainee entry into the workforce. Clin J Am Soc Nephrol. 2010;5:1770–4. doi: 10.2215/CJN.07071009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frank JE, Mullaney DM, Darnall RA, Stashwick CA. Teaching residents in the neonatal intensive care unit: a non-traditional approach. J Perinatol. 2000;20:111–3. doi: 10.1038/sj.jp.7200321. [DOI] [PubMed] [Google Scholar]
- 14.Metheny WP, Sherline DM. The effects of fellowships on residency training in obstetrics and gynecology. Obstet Gynecol. 1987;69:825–9. [PubMed] [Google Scholar]
- 15.Metheny WP, Sherline DM. The resident and fellow relationship in obstetrics and gynecology. Am J Obstet Gynecol. 1988;158:618–24. doi: 10.1016/0002-9378(88)90042-7. [DOI] [PubMed] [Google Scholar]