Abstract
Background
Evidence in the musculoskeletal rehabilitation literature suggests that psychosocial factors can influence pain levels and functional outcome.
Objective
The purpose of this study was to examine changes in select psychosocial factors and their association with knee pain and function over 12 weeks after anterior cruciate ligament (ACL) reconstruction.
Design
This was a prospective, longitudinal, observational study.
Methods
Patients with ACL reconstruction completed self-report questionnaires for average knee pain intensity (numeric rating scale [NRS]), knee function (International Knee Documentation Committee Subjective Knee Form [IKDC-SKF]), and psychosocial factors (pain catastrophizing [Pain Catastrophizing Scale], fear of movement or reinjury [shortened version of the Tampa Scale for Kinesiophobia (TSK-11)], and self-efficacy for rehabilitation tasks [modified Self-Efficacy for Rehabilitation Outcome Scale (SER)]). Data were collected at 4 time points after surgery (baseline and 4, 8, and 12 weeks). Repeated-measures analyses of variance determined changes in questionnaire scores across time. Hierarchical linear regression models were used to examine the association of psychosocial factors with knee pain and function.
Results
Seventy-seven participants completed the study. All questionnaire scores changed across 12 weeks. Baseline psychosocial factors did not predict the 12-week NRS or IKDC-SKF score. The 12-week change in modified SER score predicted the 12-week change in NRS score (r2=.061), and the 12-week change in modified SER and TSK-11 scores predicted the 12-week change in IKDC-SKF score (r2=.120).
Limitations
The psychometric properties of the psychosocial factor questionnaires are unknown in people with ACL reconstruction. The study focused on short-term outcomes using only self-report measures.
Conclusions
Psychosocial factors are potentially modifiable early after ACL reconstruction. Baseline psychosocial factor levels did not predict knee pain or function 12 weeks postoperatively. Interventions that increase self-efficacy for rehabilitation tasks or decrease fear of movement or reinjury may have potential to improve short-term outcomes for knee pain and function.
Anterior cruciate ligament (ACL) rupture is a common knee injury, particularly in sports that require cutting, jumping, or pivoting.1 In the United States, surgical reconstruction is commonly used to manage ACL injuries,2 presumably because surgery restores mechanical knee stability, which, in turn, is thought to promote optimal knee function. Functional outcome after ACL reconstruction is not uniform though, and up to 60% of the population does not return to preinjury, high-demand activities.3,4 Reduced knee function postsurgery has been attributed to a variety of residual impairments, including knee symptoms (eg, swelling, pain or instability),5,6 loss of knee motion,6 and thigh muscle weakness.6,7 Although some authors have speculated that altered psychosocial factors, such as elevated fear of reinjury, can reduce functional level,8 this area has not been extensively explored. As evidence linking fear of pain and reinjury with functional outcome in musculoskeletal conditions continues to grow,9 interest in understanding the contribution of psychosocial factors to reduced functional level following ACL reconstruction is increasing.
Although there are numerous psychosocial factors to explore, psychosocial constructs within the fear-avoidance model (FAM) are of distinct interest to this patient population. The FAM is a biopsychosocial model proposed to explain the development of chronic disability after musculoskeletal injury.9 The FAM proposes that when pain is perceived as a threat following musculoskeletal injury, various psychosocial constructs, such as increased pain catastrophizing and fear of movement or reinjury, are altered, leading to disuse, depression, disability, and higher pain levels. Figure 1 presents an abbreviated version of the FAM; readers interested in the full model are encouraged to consult a recent topical review.9
Figure 1.
The fear-avoidance model for musculoskeletal pain modified from Leeuw et al.9
Pain catastrophizing and fear of movement or reinjury are commonly measured with self-report questionnaires such as the Pain Catastrophizing Scale (PCS)10 and the Tampa Scale for Kinesiophobia (TSK),11 respectively. Tripp and colleagues12 found that PCS scores were higher in adolescents compared with adults in the first 24 hours after ACL reconstruction. Although the functional implications of an elevated PCS score were not explored, the investigators reported that group differences in pain scores were no longer significant after controlling for PCS score, indicating that pain catastrophizing influenced knee pain levels. Tampa Scale for Kinesiophobia scores have been reported to be elevated and associated with a lower self-report of function and rate of return to sports activity following ACL reconstruction.6,13–15 In a cross-sectional study across the first year after ACL reconstruction, Chmielewski et al13 found that TSK scores decreased over time after surgery. Interestingly, TSK scores were associated with self-report of function only when patients were at least 6 months postsurgery, the time frame when return to sports activity is allowed, whereas knee pain intensity was associated with self-report of function at all time frames.13 Further research that investigates the influence of FAM psychosocial constructs on knee pain levels and function in the early postsurgical time frame will provide insight into the relevance of the FAM on early ACL reconstruction rehabilitation outcomes.
Self-efficacy is another psychosocial construct of interest that is not explicitly addressed in the current FAM. Self-efficacy has been defined as a judgment of a person's potential ability to carry out a task rather than a measure of whether the task can be or is performed,16 and it can be described for any task. Thomee and colleagues17 developed the Knee Self-Efficacy Scale for ACL injury to assess self-efficacy in 4 domains (daily activities, sports and leisure activities, physical activities, and knee function in the future). Although preoperative scores on the Knee Self-Efficacy Scale were found to predict functional measures 1 year after ACL reconstruction,18 the questionnaire contains items that may not be relevant to some people, particularly if the questionnaire is administered early after surgery. For example, patients may not have the opportunity to perform some tasks (eg moving around in a small rocking boat), and some tasks (eg, doing one-leg hops on the injured leg) may be too difficult to perform. The Self-Efficacy for Rehabilitation Outcome Scale (SER) examines beliefs about participating in rehabilitation after hip or knee surgery19 and, therefore, is appropriate for an early postsurgical time frame. Self-Efficacy for Rehabilitation Outcome Scale scores have been found to be predictive of performance on the Functional Independence Measure and of walking speed in patients with total hip or total knee arthroplasty.20 Although the SER has not been assessed in patients with ACL reconstruction, the questionnaire targets self-efficacy for activities that are common in ACL reconstruction rehabilitation.
There are promising trends in the literature for the association of FAM constructs and self-efficacy with knee function after ACL reconstruction. However, most studies have used a cross-sectional design, so the temporal aspects of psychosocial influence have not been widely reported, and studies often examine a single psychosocial factor, so the relative importance of various factors is unknown. Moreover, little is known about the association between psychosocial factors and knee pain levels, and knee pain levels are potentially important in knee function after ACL reconstruction. Therefore, the purpose of this prospective, longitudinal study was to examine changes in selected psychosocial factors and the association with knee pain and function over 12 weeks in people with ACL reconstruction. We chose to examine the first 12 weeks postoperatively because supervised physical therapy typically is received during this time frame, meaning there is potential to intervene on any psychosocial constructs identified as rehabilitation targets. We hypothesized that psychosocial factors would improve over this time frame and that they would be associated with self-report of knee pain and function.
Method
Participants
Patients with an ACL reconstruction who began rehabilitation at Shands Rehab, Orthopaedics and Sports Medicine Institute, University of Florida, Gainesville, Florida, from September 2007 to April 2010 were eligible to participate in this study. An attempt was made to recruit consecutive patients during this period but these data were not tracked by the researchers, so this should be considered a convenience sample. The inclusion criteria were: (1) unilateral ACL reconstruction, (2) age between 15 and 45 years, and (3) time from injury to surgery of 12 months or less. Exclusion criteria were: (1) bilateral injury and (2) concomitant ligamentous injury greater than grade I. All surgical procedures were performed by board-certified orthopedic surgeons (P.A.I. or M.W.M.). Rehabilitation was not controlled in this study; however, the standard ACL reconstruction rehabilitation protocol used in the facility allows for immediate weight bearing and knee motion as tolerated. The emphasis of the first 6 weeks of rehabilitation is on decreasing knee effusion, developing quadriceps muscle control, and regaining full knee motion. The next 6 weeks of rehabilitation are focused on increasing lower-extremity muscle strength (force-generating capacity) and endurance and on neuromuscular control. Patients are allowed to perform open-chain quadriceps muscle strengthening through full knee range of motion at 10 weeks postoperatively. Participants provided written informed consent to use their clinical data on a form approved by the University of Florida Institutional Review Board.
Data Collection Overview
Two physical therapists (G.Z. and T.A.L.) supervised the collection of data across the caseloads of 6 physical therapists. Data were collected at 4 time points after surgery (baseline and 4, 8, and 12 weeks). Therapists were given verbal or electronically generated reminders at each data collection time point. Demographic data were collected at the initial physical therapy visit only, and self-report questionnaires for knee pain intensity, psychosocial constructs, and knee function were administered at all 4 time points. Data were collected on standardized forms and then entered into an electronic database (Microsoft Office Access 2007).*
Demographic Data
A variety of demographic information relevant to ACL injuries was collected. The variables included: age, sex, mechanism of injury, injury situation, time from injury to surgery, graft type, graft source, accompanying surgical procedures, and previous knee injuries or surgeries. The mechanism of injury was categorized as “contact” or “noncontact” and was considered to be the former only if there was contact with another athlete, regardless of where on the body the contact occurred. Injury situation was categorized as “sports” or “non-sports,” based on whether the individual was participating in sports at the time of injury. Graft type was categorized as “allograft” or “autograft.” The autograft sources were bone-patellar tendon-bone or semitendinosus and gracilis tendons. The allograft sources were tibilalis anterior, posterior tibialis, or Achilles tendon. Accompanying surgical procedures and previous knee injuries or surgeries were coded as “yes” or “no.” Accompanying surgical procedures generally included menisectomy, meniscal repair, chondroplasty, or microfracture.
Self-Report Questionnaires
Knee pain intensity was measured with an 11-point numeric rating scale (NRS). Participants verbally rated their worst and best knee pain intensity in the previous 24 hours as well as their current knee pain intensity on a scale from 0 (“no pain”) to 10 (“worst pain imaginable”) points. The ratings on these 3 items were averaged for analysis. Test-retest reliability coefficients (intraclass correlation coefficient) for the NRS have been reported to be .74 and .76 and the minimum detectable change has been reported to be 2.5 and 2.1 points in patients with shoulder and neck pain, respectively.21,22 Although the NRS is a widely used clinical method for assessing knee pain intensity, to our knowledge reliability and responsiveness of this measure have not been assessed in patients with ACL reconstruction.
Fear of movement or reinjury, or kinesiophobia, was measured with the shortened version of the Tampa Scale for Kinesiophobia (TSK-11).11 The TSK-11 is an 11-item questionnaire that eliminates psychometrically poor items from the original version of the TSK to create a shorter questionnaire with comparable internal consistency. Items relate to somatic sensations (eg, “Pain always means I have injured my body”) or activity avoidance (eg, “I'm afraid that I might injure myself if I exercise”) and are scored from 1 (“strongly disagree”) to 4 (“strongly agree”). The item scores are summed to create a total score that ranges from 11 to 44 points, with higher scores indicating greater pain-related fear of movement or reinjury. In patients with chronic low back pain, test-retest reliability coefficients (intraclass correlation coefficient) of .81 and .93,11,23 a standardized response mean of −1.11,11 and a minimal detectable change of 4.8 points23 have been reported for the TSK-11. The reliability and responsiveness of the TSK-11 questionnaire have not been assessed in patients with ACL reconstruction.
Pain catastrophizing was measured with the 13-item PCS.10 Items relate to rumination (eg, “When I'm in pain, I keep thinking about how much it hurts”), magnification (eg, “When I'm in pain, I become afraid that the pain will get worse”), and helplessness (eg, “When I'm in pain, I feel I can't stand it anymore”). Each item on the questionnaire is scored from 0 (“not at all”) to 4 (“all the time”). The items scores are summed to create a total score that ranges from 0 to 52 points, with higher scores indicating higher levels of pain catastrophizing. In patients with chronic low back pain, test-retest reliability (intraclass correlation coefficient) is .93 and the minimal detectable change is 9.1 points for the PCS.23 The reliability and responsiveness of the PCS questionnaire have not been assessed in patients with ACL reconstruction.
The SER is a 12-item questionnaire that measures patients' beliefs about their ability to perform behaviors typical in physical rehabilitation for knee and hip surgery.19 Each item is scored on an 11-point Likert scale (0=“I cannot do it” and 10=“Certain I can do it”), and the items scores are summed to create a total score that ranges from 0 to 120 points. We modified the SER by removing 2 items (item 8 [“The exercises my therapists say I should do, even if I don't understand how it helps me”] and item 9 [“My therapy no matter how I feel emotionally”]) to create a briefer, 10-item questionnaire with a total score that ranges from 0 to 100 points. The internal consistency coefficient (Cronbach alpha) is .94 for the original SER, presumably in a population of patients with hip and knee replacement.19 The reliability and responsiveness of the original and modified versions of the SER have not been determined in patients with ACL reconstruction.
Knee function was measured with the 18-item International Knee Documentation Committee Subjective Knee Form (IKDC-SKF), which includes questions about knee symptoms and functional limitations. Point values for each item vary depending on the number of responses possible. Item responses are summed, divided by the total points possible, and multiplied by 100 to create a total score. Higher scores indicate less disability. In a sample of patients with knee problems, including ACL injury, a test-retest reliability value (intraclass correlation coefficient) of .94,24 a minimal detectable change of 12.8 points,25 and a standardized response mean of 0.9426 were obtained.
Data Management
Sex was dummy coded (0=male, 1=female). If an item response was missing on any of the self-report questionnaires, the total number of items on that questionnaire was reduced when computing the score. Questionnaires were required to have at least 90% of the items completed in order to be used in analysis.26
Considering the large amount of information that was transferred from standardized forms to the electronic database, the accuracy of the data was verified in several steps. First, demographic variables were reviewed for each participant. Second, item responses were reviewed and confirmed for the self-report questionnaire scores that were considered outliers. Finally, 3 participants were randomly selected from each block of 10 participants for review of each data point.
Data Analysis
Descriptive statistics were generated for demographic variables and self-report questionnaire scores. Independent t tests and chi-square statistics were used, as appropriate, to compare demographic variables between participants who completed all testing sessions and those who missed one or more testing sessions. Longitudinal changes in self-report questionnaire scores were examined with repeated-measures analyses of variance using Bonferroni adjustment of the confidence interval.
The associations of psychosocial factors with knee pain intensity and knee function were examined with separate hierarchical linear regression models. These dependent variables were appropriate for the regression models because they approximated a normal distribution as determined by one-sample Kolmogorov-Smirnov tests.
A 3-step regression model was used to examine the association of baseline psychosocial factors with knee pain intensity at 12 weeks. In the hierarchical regression model, age and sex followed by baseline NRS score were forced into the model, and baseline TSK-11, PCS, and modified SER scores were entered using the forward selection method. A 2-step model was used to examine the association of the 12-week change in psychosocial factors and change in knee pain intensity. All change scores were computed as 12-week score minus baseline score, meaning scores that decreased across 12 weeks (ie, NRS, TSK-11, and PCS scores) had a negative result and scores that increased across 12 weeks (ie, IKDC-SKF and modified SER scores) had a positive result. Age and sex were forced into the model, and then 12-week change in TSK-11, PCS, and modified SER scores were entered using the forward selection method. We used the NRS as a dependent variable for our regression models, and there is some debate over its use as such. Some studies have indicated that the NRS may not exhibit linear properties for thermal stimuli27 or pain conditions28 compared with the visual analog scale for pain intensity. However, other authors have found the NRS to have measure properties comparable to those of the visual analog scale29,30 and to be sensitive enough to change for use in statistical analyses.31 Therefore, we felt its use as a dependent variable was appropriate for our planned analyses.
A 3-step regression model was used to examine the association of baseline psychosocial factors with knee function at 12 weeks. Age and sex followed by baseline NRS and IKDC-SKF scores were forced into the model, and then baseline TSK-11, PCS, and modified SER scores were entered using the forward selection method. A 3-step regression model was used to examine the association of the 12-week change in psychosocial factors with the 12-week change in knee function. Age and sex followed by baseline NRS scores were forced into the model, and then 12-week change in TSK-11, PCS, and modified SER scores were entered using the forward selection method.
The regression models for knee pain intensity and function were constructed this way to determine the unique contribution of psychosocial factors after accounting for the contribution of demographic variables. In addition, the baseline score of the response variable was entered into models predicting the 12-week outcome because the baseline level is expected to strongly predict 12-week outcomes. We did not include the baseline score of the response variable in models predicting the 12-week change score because the change score is computed using the baseline score, and we wanted to avoid potential redundancy in our models. Finally, the baseline NRS score was entered in the model when the IKDC-SKF score was the response variable because our previous cross-sectional research indicated that knee pain intensity has significant influence on function in this time frame,13 and we wanted to determine whether the psychosocial factors contributed additional variance to function after controlling for knee pain intensity. The regression models for this study were very similar to what has been used to investigate the influence of psychosocial factors for patients with chronic low back pain.32–35 For psychosocial variables, the criterion for entry into the model was P=.05, and the criterion for removal from the model was P=.10. Alpha was set at P<.05 for all other statistical tests.
The sample size chosen for this study was based on the number of participants needed to avoid overfitting of the regression models. It has been suggested that 10 participants are needed for each predictor variable included in a regression model.36 Because the greatest number of predictor variables in any regression model was 7, a minimum sample size of 70 participants was necessary.
Role of the Funding Source
Dr Chmielewski's effort on this project was supported by a grant from the National Institutes of Health (K01-HD052713).
Results
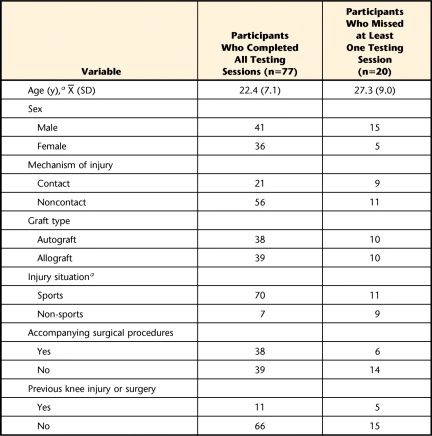
A total of 97 participants were enrolled in this study, and 77 individuals participated in all testing sessions (Fig. 2). Demographic characteristics for the entire sample are summarized in Table 1, with delineation for those who participated and those who did not participate in all testing sessions. Compared with participants who completed all testing sessions, those with missing data were older (P=.011) and showed a greater frequency of being injured in non-sports-related situations (P=.001). Only participants who completed all testing sessions were analyzed further. The mean number of days after surgery (standard deviation) to each testing session was: 6.0 (SD=4.4) at baseline, 30.4 (SD=5.4) at the 4-week time point, 59.6 (SD=6.2) at the 8-week time point, and 88.9 (SD=10.2) at the 12-week time point.
Figure 2.
Flow chart for participant enrollment.
Table 1.
Demographic Information for All Participants Enrolled in the Study
a Significant difference between groups (P<.05).
Longitudinal Changes in Questionnaire Scores
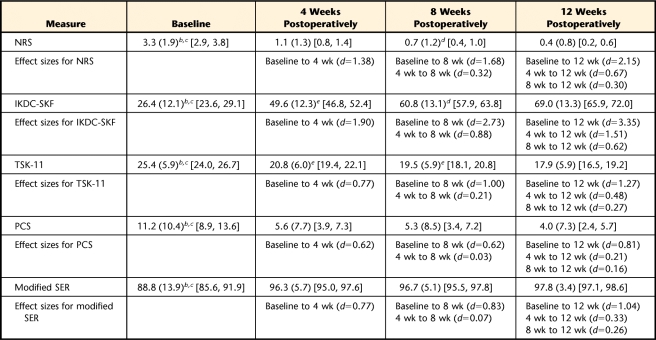
Descriptive data and effect sizes for longitudinal changes in questionnaire scores are reported in Table 2. Self-report questionnaires scores showed significant changes across the 12-week time interval (P<.001), with the greatest change between baseline and 4 weeks postoperatively. Significant decreases in TSK-11 scores and increases in IKDC-SKF scores were observed at all time points. The NRS scores showed significant decreases between baseline and 4 weeks postoperatively and between 8 and 12 weeks postoperatively. The PCS score showed a significant decrease and the modified SER score showed a significant increase between baseline and 4 weeks postoperatively.
Table 2.
Mean Scores With Standard Deviation (in Parentheses) and Confidence Interval (in Brackets) for All Self-Report Questionnaires at Each Testing Time Pointa
NRS=numeric rating scale for average knee pain intensity, TSK-11=shortened version of the Tampa Scale for Kinesiophobia, PCS=Pain Catastrophizing Scale, modified SER=modified version of the Self-Efficacy for Rehabilitation Outcome Scale, IKDC-SKF=International Knee Documentation Committee Subjective Knee Form. All effect sizes calculated using Cohen d method.
b Baseline is significantly different from 12 weeks postoperatively (P<.05).
c Baseline is significantly different from 4 weeks postoperatively (P<.05).
d 8 weeks postoperatively is significantly different from 12 weeks postoperatively (P<.05)
e 4 weeks postoperatively is significantly different from 8 weeks postoperatively (P<.05).
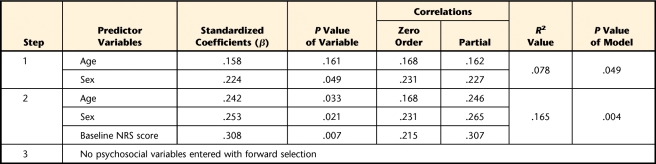
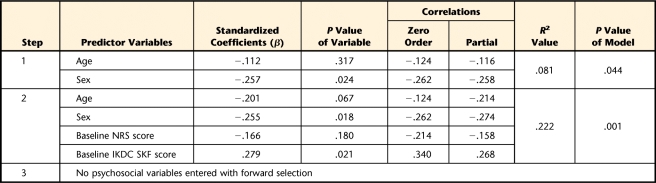
Association of Psychosocial Factors With Knee Pain Intensity
Baseline TSK-11, PCS, and modified SER scores were not associated with the 12-week NRS score (Tab. 3). The 12-week change in the modified SER score was associated with the 12-week change in NRS score (r2=.061, Tab. 4). The negative standardized beta (−0.253) indicates that an increase in self-efficacy for rehabilitation tasks was associated with a decrease in knee pain intensity.
Table 3.
Hierarchical Linear Regression Analysis Results Using the 12-Week Numeric Rating Scale for Average Knee Pain Intensity (NRS) Score as the Response Variable
Table 4.
Hierarchical Linear Regression Analysis Results Using the Baseline to 12-Week Change in Numeric Rating Scale for Average Knee Pain Intensity (NRS) Score as the Response Variablea
Modified SER=modified version of the Self-Efficacy for Rehabilitation Outcome Scale.
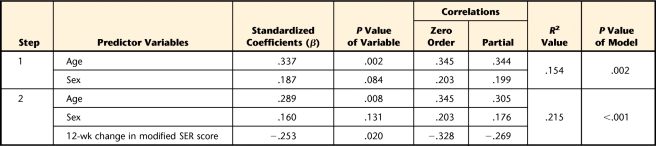
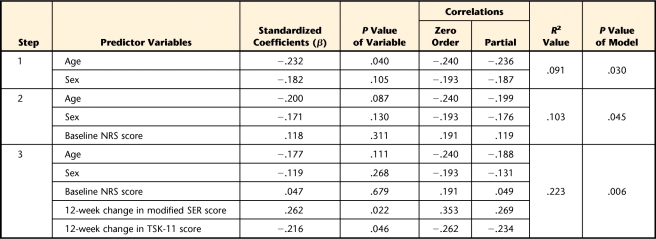
Association of Psychosocial Factors With Knee Function
Baseline NRS, TSK-11, PCS, and modified SER scores were not associated with the 12-week IKDC-SKF score (Tab. 5). The 12-week change in modified SER and TSK-11 scores contributed to the 12-week change in IKDC-SKF score (r2=.120, Tab. 6). The standardized betas for the modified SER (0.262) and TSK-11 (−0.216) indicate that an increase in self-efficacy for rehabilitation tasks and a decrease in fear of movement or reinjury were associated with an increase in knee function.
Table 5.
Hierarchical Linear Regression Analysis Results Using the 12-Week International Knee Documentation Committee Subjective Knee Form (IKDC SKF) as the Response Variablea
NRS=numeric rating scale for average knee pain intensity.
Table 6.
Hierarchical Linear Regression Analysis Results Using the Baseline to 12-Week Change in International Knee Documentation Committee Subjective Knee Form (IKDC-SKF) Score as the Response Variablea
NRS=numeric rating scale for average knee pain intensity, modified SER=modified version of the Self-Efficacy for Rehabilitation Outcome Scale, TSK-11=shortened version of the Tampa Scale for Kinesiophobia.
Discussion
This study investigated changes in psychosocial factors, including those consistent with the FAM and self-efficacy theory, and their association with knee pain and function over 12 weeks after ACL reconstruction. As we hypothesized, all psychosocial factors changed across this time frame and in a manner that indicated an improvement in psychological status. Unexpectedly, none of the baseline psychosocial factors were associated with knee pain or function at 12 weeks. On the other hand, the 12-week improvement in self-efficacy for rehabilitation tasks was associated with reduced knee pain and improvement in knee function, and the 12-week improvement in fear of movement or reinjury was associated with the improvement in knee function only. Taken together, these findings suggest that during the 12 weeks after ACL reconstruction: (1) psychosocial factors are modified in a favorable manner, (2) baseline levels do not foretell knee pain or functional levels at 12 weeks, and (3) interventions aimed at increasing self-efficacy for rehabilitation tasks or decreasing fear of movement or reinjury have the potential to improve short-term outcomes for knee pain and function.
Although psychosocial questionnaire scores changed across the 12-week time interval, the rate of change was not uniform across the questionnaires. All psychosocial questionnaire scores showed the largest magnitude of change in the first 4 weeks following surgery. After that time point, the PCS and modified SER scores did not change further, whereas TSK-11 scores continued to decrease through 12 weeks postoperatively. The longitudinal results suggest that following ACL reconstruction, fear of movement or reinjury improves more slowly than pain catastrophizing and self-efficacy for rehabilitation. However, one reason why PCS and modified SER scores may not have changed after 4 weeks is that the questionnaires had floor and ceiling effects, respectively. More specifically, at 4 weeks postoperatively, the mean score on the PCS was 5.6 points (minimum score=0 points) and the mean score on the modified SER was 96.3 points (maximum score=100 points). Despite a low PCS score and high modified SER score by 4 weeks after surgery, the questionnaires may still provide important information at later time points. For example, at 12 weeks postoperatively, 8 participants (9% of the sample) had PCS scores of at least 15 points, which is an average score in people with chronic low back pain.23 Similarly, at 12 weeks postoperatively, 6 participants scored below 90 points on the modified SER. Future research could be directed at identifying how outcomes are affected for patients who do not make timely progress on these psychosocial factors.
When compared with PCS and TSK-11 scores in people with chronic pain,23,37 the scores at 12 weeks after ACL reconstruction appear to be lower. Therefore, we can interpret the PCS and TSK-11 scores of participants in this study as being lower in comparison with those of people with chronic pain. However, we do not know the overall context of PCS and TSK-11 scores for the ACL reconstruction population. Recent research suggests that fear of reinjury is one of the most common reasons for not returning to preoperative sports participation.14,38 Thus, future research is needed to define the threshold for elevated PCS and TSK-11 scores in patients with ACL reconstruction that may indicate a higher risk for not returning to preoperative sports participation.
We previously reported that knee pain has a significant influence on self-report of knee function after ACL reconstruction, even though knee pain levels are generally low.6,13 The average knee pain intensity in this sample was 3.3 points at baseline and decreased to 0.4 point at 12 weeks postsurgery. Other authors also have found low knee pain levels following ACL reconstruction.5,39,40 Based on our previous research, we expected that baseline knee pain intensity would be a significant contributor to the regression models with IKDC-SKF score as a response variable, but the NRS score was not a significant contributor to either model. The low variability in knee pain intensity at baseline may explain our results. From the results of our previous research and the present study, it appears that knee pain influences function at a given time point, but the magnitude of knee pain immediately after surgery may not have any bearing on future knee function. Thus, clinical protocols should focus on the resolution of knee pain throughout the course of rehabilitation.
Even though knee pain levels are generally low in patients with ACL reconstruction, the FAM may still have relevance for clinical decision making in this patient population. According to the FAM it is the interpretation of the pain experience, not just the level of pain intensity, that can lead to increased fear and catastrophizing about pain.9 Supporting this concept for the FAM, at 12 weeks postsurgery, one participant had an average NRS score of 0 points (low pain) coupled with a high PCS score of 47 points and a high TSK-11 score of 26 points. Interestingly, the IKDC-SKF score was 59.8 points for this participant, providing indirect evidence that the high psychological distress may be related to lower function. This example underscores previous findings that knee pain intensity and psychosocial factors (fear of movement or reinjury) can independently influence knee function.13
Baseline levels of these selected psychosocial factors were not associated with 12-week outcomes for knee pain and function, which has important clinical implications. The finding suggests that patients with high scores on the PCS or TSK-11, or low scores on the modified SER, cannot be identified at baseline as being at risk for high pain levels or low self-report of function at the end of the early phase of ACL reconstruction rehabilitation. Therefore, at this time, we cannot recommend using the questionnaires as screening tools in this patient population. It should be noted that baseline testing occurred an average of 6 days postoperatively, and most participants had already completed at least one physical therapy appointment. Although patients in this study did not receive specific interventions to target the psychosocial factors studied, routine education given prior to questionnaire administration (both presurgically and postsurgically) may have affected the baseline scores. Further research is needed to determine whether obtaining psychosocial factor scores preoperatively is more useful in predicting postsurgical knee pain and function.
The 12-week change in the modified SER score was the only psychosocial variable to be associated with the 12-week improvement in knee pain and function. Previous research has shown that high self-efficacy is associated with better adherence to rehabilitation protocols8 and greater effort toward goal attainment during a strenuous activity.41 These behaviors would bode well for both decreasing knee pain and improving knee function and are a possible mechanism underlying the association. To our knowledge, this is the first study to investigate self-efficacy for rehabilitation tasks using the modified SER questionnaire. This sample of patients with ACL reconstruction demonstrated high modified SER scores by 12 weeks postoperatively, but this psychosocial construct appears to have clinical relevance because of its association with knee pain and function.
The 12-week change in TSK-11 score contributed to the 12-week improvement in knee function. Our previous cross-sectional study showed no association between TSK-11 and IKDC-SKF scores in the interval from immediately post-ACL reconstruction up to 12 weeks postoperatively,13 and we postulated a reason for the result is that patients had not yet been able to physically assess their readiness for high-demand activities. In contrast, the findings of the current study indicate that a failure to reduce fear of movement or reinjury levels throughout the early postoperative phase may be associated with lower knee function. Pizzari and colleagues42 reported that patients who were nonadherent to rehabilitation after ACL reconstruction cited fear of reinjury as a reason, providing support for the importance of decreasing fear of movement or reinjury postsurgically. Continued investigation of fear of movement or reinjury in the early period after ACL reconstruction is warranted. Moreover, because a large amount of variance in IKDC-SKF scores was unexplained in the final regression model, additional factors (psychosocial and physical) should be considered for inclusion in future research.
At this time, impairments in self-efficacy and fear of movement or reinjury are not routinely addressed in ACL reconstruction rehabilitation protocols. Possible reasons are that the assessment of psychosocial factors has not been widely implicated as a barrier to recovery after ACL reconstruction and that there is little research to guide intervention selection for clinicians who acknowledge psychosocial influence. Imagery and cognitive-behavioral methods are potential interventions to address impairments in self-efficacy and fear of movement or reinjury. Evans and colleagues43 interviewed 4 athletes with different injuries and found that cognitive-specific imagery (imagining the execution of a motor skill) was associated with increased confidence, or self-efficacy. McArdle44 initiated cognitive-behavioral methods (disputing, systematic desensitization, and time projection) at 3 months postoperatively to address negative psychological responses in an athlete with ACL and medial collateral ligament reconstruction. After 5 sessions over the course of 4 months, fear of reinjury was diminished, although not completely resolved.44 These case reports provide a starting point for more rigorous research investigating the effect of interventions geared toward directly addressing relevant psychosocial factors, such as self-efficacy and fear of movement or reinjury.
The strengths of this study are the prospective, longitudinal design; the large sample of a relatively homogenous population; and the simultaneous examination of multiple psychosocial factors. There are, however, limitations to this study that should be considered when interpreting the results and addressed in future research. The primary limitation of this study is the use of validated psychosocial questionnaires whose psychometric properties have not yet been tested in patients with ACL reconstruction. The reliability of specific items and the total score may differ in people with ACL reconstruction. Moreover, by modifying the SER, we likely altered its psychometric properties, and the same reliability cannot be inferred from the original questionnaire. Despite accruing a large sample size, we did not track patients who were eligible for the study but did not consent to participate. Thus, this was a sample of convenience, and we cannot interpret how our recruited patient pool may have differed from those not participating in the study. The majority of our patients were injured during sports activity, consistent with the epidemiology of ACL injury. However, we did not determine the level of sports participation (eg, recreational, organized, elite), which could influence psychosocial response or psychosocial association with pain and knee function. Our results may not generalize to samples with differing levels of sports participation.
We chose self-report of knee pain and function as the outcome measures for this study because they are clinically relevant and can be easily collected along with the psychosocial self-report questionnaires. Other relevant outcomes in the early period of ACL reconstruction are the recovery of quadriceps muscle strength and knee range of motion—physical impairments that often are used to guide clinical decision making. Future research could be designed to examine whether psychosocial factors influence these physical impairments. Furthermore, we studied the early period after ACL reconstruction, whereas 6 months postoperatively and later is also of interest because patients begin to stratify into those who do or do not return to preinjury activities. Future research also could examine whether baseline psychosocial factors have any bearing on knee pain and function in later time periods.
In conclusion, this study demonstrated that psychological status for fear of movement or reinjury, pain catastrophizing, and self-efficacy for rehabilitation tasks improved over the early postoperative period after ACL reconstruction. Baseline levels of these psychosocial factors did not influence knee pain or function at 12 weeks postoperatively. However, improvements in self-efficacy for rehabilitation tasks and fear of movement or reinjury were predictors of improvements in knee pain and function. This study provides information about psychosocial factors following ACL reconstruction that can be used to inform future research and rehabilitation protocols.
The Bottom Line
What do we already know about this topic?
Cross-sectional studies of musculoskeletal conditions have shown that psychosocial factors are associated with pain levels and function.
What new information does this study offer?
This study investigated longitudinal changes over early postoperative anterior cruciate ligament reconstruction rehabilitation. All psychosocial factors changed in a positive manner, with the largest decline at 4 weeks. Baseline psychosocial factors did not predict 12-week knee pain and function levels. However, increased self-efficacy for rehabilitation tasks contributed to improved knee pain levels and, in combination with decreased fear of movement or reinjury, contributed to improved knee function.
If you're a patient, what might these findings mean for you?
Improving self-efficacy for rehabilitation tasks and reducing fear of movement or reinjury might lead to lower knee pain and higher function at the end of early postoperative anterior cruciate ligament reconstruction rehabilitation.
Footnotes
Dr Chmielewski, Dr Moser, Dr Indelicato, and Dr George provided concept/idea/research design. Dr Chmielewski and Dr George provided writing and data analysis. Mr Zeppieri, Mr Lentz, and Ms Tillman provided data collection. Dr Chmielewski and Mr Zeppieri provided project management. Mr Zeppieri, Mr Lentz, Ms Tillman, Dr Moser, and Dr Indelicato provided participants. Mr Zeppieri, Mr Lentz, Ms Tillman, Dr Moser, Dr Indelicato, and Dr George provided consultation (including review of manuscript before submission).
The authors acknowledge Sarah Weisbruch, Michael Rademaker, Kari Colville, Deena Cilien, Caroline Davis, and Brittney Herder for their assistance with data entry. They also acknowledge Jason Goss, PT, Scott Greenberg, PT, DPT, Michael Hodges, PT, CSCS, OCS, Debi Jones, PT, DPT, Derek Miles, PT, DPT, and Brent Williams, PT, CSCS, from Shands Rehab, Orthopaedics and Sports Medicine Institute, for their assistance with data collection.
This study was approved by the University of Florida Institutional Review Board.
A platform presentation of the results of this study was made at the Combined Sections Meeting of the American Physical Therapy Association; February 17–20, 2010; San Diego, California.
Dr Chmielewski's effort on this project was supported by a grant from the National Institutes of Health (K01-HD052713) and by the National Center for Medical Rehabilitation Research.
Microsoft Corporation, One Microsoft Way, Redmond, WA 98052-6399.
References
- 1. Beynnon BD, Johnson RJ, Abate JA, et al. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33:1579–1602 [DOI] [PubMed] [Google Scholar]
- 2. Marx RG, Jones EC, Angel M, et al. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770 [DOI] [PubMed] [Google Scholar]
- 3. Fithian DC, Paxton EW, Stone ML, et al. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33:335–346 [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606 [DOI] [PubMed] [Google Scholar]
- 5. Risberg MA, Holm I, Tjomsland O, et al. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:400–412 [DOI] [PubMed] [Google Scholar]
- 6. Lentz TA, Tillman SM, Indelicato PA, et al. Factors associated with function after anterior cruciate ligament reconstruction. Sports Health: A Multidisciplinary Approach. 2009;1:47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilk KE, Romaniello WT, Soscia SM, et al. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60–73 [DOI] [PubMed] [Google Scholar]
- 8. Brand E, Nyland J. Patient outcomes following anterior cruciate ligament reconstruction: the influence of psychological factors. Orthopedics. 2009;32:335. [DOI] [PubMed] [Google Scholar]
- 9. Leeuw M, Goossens ME, Linton SJ, et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94 [DOI] [PubMed] [Google Scholar]
- 10. Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–532 [Google Scholar]
- 11. Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117:137–144 [DOI] [PubMed] [Google Scholar]
- 12. Tripp DA, Stanish WD, Reardon G, et al. Comparing postoperative pain experiences of the adolescent and adult athlete after anterior cruciate ligament surgery. J Athl Train. 2003;38:154–157 [PMC free article] [PubMed] [Google Scholar]
- 13. Chmielewski TL, Jones D, Day T, et al. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38:746–753 [DOI] [PubMed] [Google Scholar]
- 14. Lee DY, Karim SA, Chang HC. Return to sports after anterior cruciate ligament reconstruction: a review of patients with minimum 5-year follow-up. Ann Acad Med Singapore. 2008;37:273–278 [PubMed] [Google Scholar]
- 15. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393–397 [DOI] [PubMed] [Google Scholar]
- 16. Bandura A. Self-efficacy: towards a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215 [DOI] [PubMed] [Google Scholar]
- 17. Thomee P, Wahrborg P, Borjesson M, et al. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports. 2006;16:181–187 [DOI] [PubMed] [Google Scholar]
- 18. Thomee P, Wahrborg P, Borjesson M, et al. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:118–127 [DOI] [PubMed] [Google Scholar]
- 19. Waldrop D, Lightsey OR, Ethington CA, et al. Self-efficacy, optimism, health competence, and recovery from orthopedic surgery. J Couns Psychol. 2001;48:233–238 [Google Scholar]
- 20. van den Akker-Scheek I, Stevens M, Groothoff JW, et al. Preoperative or postoperative self-efficacy: which is a better predictor of outcome after total hip or knee arthroplasty? Patient Educ Couns. 2007;66:92–99 [DOI] [PubMed] [Google Scholar]
- 21. Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74 [DOI] [PubMed] [Google Scholar]
- 22. Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18:920–926 [DOI] [PubMed] [Google Scholar]
- 23. George SZ, Valencia C, Beneciuk JM. A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. J Orthop Sports Phys Ther. 2010;40:197–205 [DOI] [PubMed] [Google Scholar]
- 24. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2001;29:600–613 [DOI] [PubMed] [Google Scholar]
- 25. Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145 [DOI] [PubMed] [Google Scholar]
- 26. Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567–1573 [DOI] [PubMed] [Google Scholar]
- 27. Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217–226 [DOI] [PubMed] [Google Scholar]
- 28. Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3:310–316 [DOI] [PubMed] [Google Scholar]
- 29. Breivik EK, Bjornsson GA, Skovlund E. A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain. 2000;16:22–28 [DOI] [PubMed] [Google Scholar]
- 30. Li L, Liu X, Herr K. Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med. 2007;8:223–234 [DOI] [PubMed] [Google Scholar]
- 31. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804 [DOI] [PubMed] [Google Scholar]
- 32. Woby SR, Watson PJ, Roach NK, Urmston M. Adjustment to chronic low back pain: the relative influence of fear-avoidance beliefs, catastrophizing, and appraisals of control. Behav Res Ther. 2004;42:761–774 [DOI] [PubMed] [Google Scholar]
- 33. Woby SR, Watson PJ, Roach NK, Urmston M. Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? Eur J Pain. 2004;8:201–210 [DOI] [PubMed] [Google Scholar]
- 34. Costa Lda C, Maher CG, McAuley JH, et al. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain. 2011;15:213–219 [DOI] [PubMed] [Google Scholar]
- 35. Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7:261–271 [DOI] [PubMed] [Google Scholar]
- 36. Kleinbaum DG, Kupper LL, Muller KE, Nizam A. Applied Regression Analysis and Multivariable Methods. 3rd ed. New York, NY: Duxbury Press; 1997 [Google Scholar]
- 37. Roelofs J, Sluiter JK, Frings-Dresen MH, et al. Fear of movement and (re)injury in chronic musculoskeletal pain: evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain. 2007;131:181–190 [DOI] [PubMed] [Google Scholar]
- 38. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606 [DOI] [PubMed] [Google Scholar]
- 39. Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96 [DOI] [PubMed] [Google Scholar]
- 40. Brewer BW, Cornelius AE, Sklar JH, et al. Pain and negative mood during rehabilitation after anterior cruciate ligament reconstruction: a daily process analysis. Scand J Med Sci Sports. 2007;17:520–529 [DOI] [PubMed] [Google Scholar]
- 41. Bandura A, Cervone D. Self-evaluative and self-efficacy mechanisms governing the motivational effects of goal systems. J Pers Soc Psychol. 1983;45:1017–1028 [Google Scholar]
- 42. Pizzari T, McBurney H, Taylor NF, Feller JA. Adherence to anterior cruciate ligament rehabilitation: a qualitative analysis. J Sport Rehab. 2002;11:90–102 [Google Scholar]
- 43. Evans L, Hare R, Mullen R. Imagery use during rehabilitation from injury. J Imagery Research Sport Physical Activity. 2006;1:1–19 [Google Scholar]
- 44. McArdle S. Psychological rehabilitation from anterior cruciate ligament-medial collateral ligament reconstructive surgery: a case study. Sports Health: A Multidisciplinary Approach. 2010;2:73–77 [DOI] [PMC free article] [PubMed] [Google Scholar]