Abstract
Central hypothyroidism is defined as hypothyroidism due to insufficient stimulation by thyroid stimulating hormone (TSH) of an otherwise normal thyroid gland. It has an estimated prevalence of approximately 1 in 80,000 to 1 in 120,000. It can be secondary hypothyroidism (pituitary) or tertiary hypothyroidism (hypothalamus) in origin. In children, it is usually caused by craniopharyngiomas or previous cranial irradiation for brain tumors or hematological malignancies. In adults, it is usually due to pituitary macroadenomas, pituitary surgeries or post-irradiation. Fatigue and peripheral edema are the most specific clinical features. Diagnosis is established by the presence of normal to low-normal TSH on the background of low-normal thyroid hormones, confirmed by the thyrotropin releasing hormone stimulation test. Therapy includes use of levothyroxine titrated to improvement in symptomology and keeping free T4 in the upper limit of normal reference range.
Keywords: Hypothyroidism, central hypothyroidism, secondary hypothyroidism, tertiary hypothyroidism, levothyroxine, hypopituitarism, panhypopituitarism, thyrotropin releasing hormone, thyroid stimulating hormone
INTRODUCTION
Central hypothyroidism is defined as hypothyroidism due to insufficient stimulation by thyroid stimulating hormone (TSH) of an otherwise normal thyroid gland. It can occur at the level of the hypothalamus or the pituitary gland.[1] The prevalence is estimated to be around 1 in 80,000 to 1 in 120,000 individuals,[2] is roughly equal in both sexes and can arise from a number of pathogenetic mechanisms involving the pituitary (secondary hypothyroidism) or hypothalamus (tertiary hypothyroidism). In children, this is usually cause by craniopharyngiomas or previous cranial irradiation for brain tumors or hematological malignancies.[3] In adults, it is more commonly due to pituitary macroadenomas, pituitary surgeries or irradiation.[4]
Central hypothyroidism is characterized by insufficient thyroid gland stimulation by TSH, resulting from hypothalamic and/or pituitary dysfunction. It is rarely isolated, and occurs more commonly in conjunction with other pituitary hormone deficiencies as well as neurological symptoms and signs resulting from the hypothalamic/pituitary lesion.[5]
With the use of serum TSH as an initial screening test for thyroid dysfunction, the diagnosis of central hypothyroidism may be delayed or even missed because most of these patients have normal or low TSH levels. Some may even have slightly high TSH levels. Hence, both free thyroxine and TSH should be examined concurrently.
PHYSIOLOGY OF THYROID SECRETION
The fetal thyroid does not become functional until the 12th week of gestation. The fetus is therefore dependant entirely on thyroid hormones of maternal origin during the first trimester. Maternally acquired thyroid hormone is therefore critical in the early fetal development (brain). The timing and severity of thyroid hormone insufficiency predicts the type and severity of the neurological deficits in the newborn. Diminished perceptual and motor ability, markedly short attention span, lower mental development indices, defects in specific cognitive abilities such as poorer attention, slower and more variable reaction times to visual stimuli and visual processing, have been described. Thyroid hormone insufficiency in the fetus still later in development is also associated with impaired neurodevelopment.[6–10]
Secretion of thyroid hormone by the thyroid gland is tightly regulated by the hypothalamic–pituitary axis. The hypothalamus secretes thyrotropin releasing hormone (TRH), which in turn regulates the release of TSH from the anterior pituitary. The TSH, in a potent negative-feedback system, regulates the release of thyroid hormone from the thyroid gland.
TRH is synthesized as a large pre-pro-TRH protein, secreted under the influence of TRH gene, located on chromosome 3, in the hypothalamus and in several tissues, such as the brain, the β cells of the pancreas, C-cells of the thyroid gland, myocardium, reproductive organs (prostate and testis), spinal cord, skin (epidermis) and in the anterior pituitary.[11–17] In the myocardium, overexpression has been associated with left ventricular hypertrophy in the animal model.[18] The human pre-pro-TRH molecule is a 29 kDa protein synthesized in the paraventricular nuclei (PVN) of the hypothalamus. In vivo studies have shown that, in the euthyroid state, TRH transcription is induced both in the PVH and in the anterior/lateral hypothalamus; however, in the hypothyroid state, transcription is activated in the PVH only, which can be switched off within 5 h of instituting exogenous thyroid hormone.[19] The pre-pro-TRH fragment stimulates TSH β gene expression in the pituitary gland, which enhances TRH-induced release of TSH and prolactin (PRL) from the pituitary.[11,20,21] There are two distinct regions of human TSH β gene that respond positively to TRH. This interaction is further dependent on the presence of other factors such as cAMP response element-binding protein (CREB)-binding protein (CBP) and Pit-1, which act synergistically with TRH to stimulate the TSH β gene promoter.[22,23]
TSH is a 28-kd heterodimer glycoprotein containing approximately 15% carbohydrate, consisting of α and β subunits, tightly, but non-covalently, bound. The α-subunit gene is located on chromosome 6 and the TSH β gene on chromosome 1. Thyroid-stimulating hormone is synthesized and secreted by the thyrotrophs of the anterior pituitary.[24–26] The (beta) subunit is unique and determines the biologic specificity. The (alfa) unit is identical to the (alfa) subunit of luteinizing hormone (LH), follicle stimulating hormone (FSH) and chorionic gonadotropin. TSH glycosylation is essential for it to attain normal bioactivity, a process that requires the interaction of TRH with its receptor on the thyrotroph.[27,28] Once TRH binds to its receptor on the thyrotroph, TSH gets glycosylated into a biologically potent molecule. Glycosylation of the TSH molecule also results in rapid clearance of TSH from the circulation, raising the concept of “qualitative regulation of TSH secretion,” which is mainly achieved through both transcriptional and post-transcriptional mechanisms involved in TSH glycosylation. TRH deficiency results in the production of biologically subpotent isoforms of TSH, which reverse to their active potent form on continuous TRH stimulation.[29–31] The bioactivity of TSH is influenced by specific amino acid sequences like 27CAGYC31 (cysteine-alanine-glycine-tyrosine-cysteine), which are highly conserved in the TSH β fragment, responsible for its efficacy. Mutations in the TSH β gene can result in familial isolated central hypothyroidism. The most frequent mutation is a homozygous single-base deletion in codon 105 (C105D, 114X), leading to unstable heterodimers.[31–39]
Etiology
Genetic defects
-
Pituitary-specific transcription factor defects such as PIT-1, PROP-1 LHX3 or HESX1 can be associated with multiple pituitary hormone deficiencies.
PIT-1 defect (combined deficiencies of growth hormone [GH], PRL and TSH)[40]
PROP-1 defect (deficiencies of LH, FSH, GH, PRL and TSH)[41]
Isolated TRH deficiency[42]
-
Mutations in the TSH-(beta) subunit gene
An inactivating mutation in the TRH receptor gene[45]
Biologically inactive TSH isoforms
Association with optic nerve hypoplasia in children[46]
Transient central hypothyroidism
Central hypothyroidism can be temporary in patients with severe non-thyroidal illness (major surgery, trauma, chronic renal failure, depression, anorexia and fasting), in the elderly, up to 1 month after treatment of hyperthyroidism and following withdrawal of T4 therapy in patients with multinodular goiter.
Tumors
Vascular
Hemorrhage, pituitary-apoplexy, subarachnoid hemorrhage.
Ischemic – post-partum pituitary necrosis (Sheehan syndrome), shock.
Aneurysm.
Empty sella syndrome
Inflammatory
Infectious – bacterial abscess, syphilis, tuberculosis, toxoplasmosis, neurobrucellosis, fungal disease, toxoplasmosis.[51–53]
Non-infectious – sarcoidosis, granulomatous (idiopathic, secondary), lymphocytic hypophysitis.[51]
Infiltrative
Hemochoromtosis, histiocytosis, lymphoma.[51]
Iatrogenic
Post-external radiation therapy – The GH axis is the most vulnerable to radiation damage. TSH deficiency starts to occur with radiation doses exceeding 30 Gy, with a long-term cumulative frequency of 3–6% when doses of 30–50 Gy are used.[54] External radiation therapy caused central hypothyroidism in 65% of the patients treated for brain tumors.[55,56]
Post-pituitary surgery.[56]
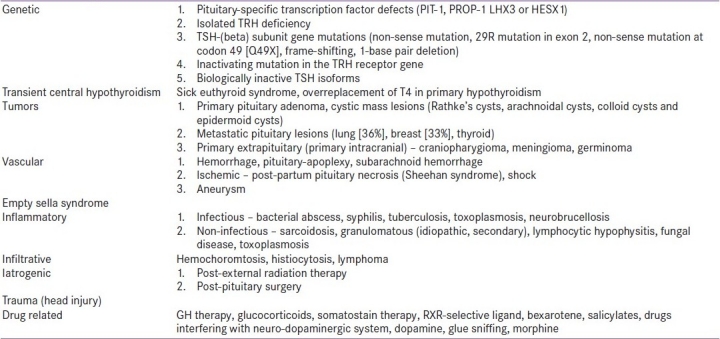
Trauma (Head injury) [Table 1][57]
Table 1.
Etiology of central hypothyroidism
Drug related
GH therapy, glucocorticoids, somatostain therapy, RXR-selective ligand, bexarotene, salicylates, drugs interfering with the neuro-dopaminergic system and dopamine.[58–60]
Addictions – glue sniffing,[61] morphine.
Clinical features
Thyroid hormone deficiency slows the body metabolism. In patients with complete athyreosis, body energy metabolism falls between 35 and 45% below normal. Body weight increases on average by 10% due to an increase of body fat and retention of water and salt. Serum leptin has been recognized as one of the factors modulating energy metabolism.[62] Biosynthesis of fatty acids and lipolysis are reduced. Hypothyroidism results in an increase in serum cholesterol, which is largely accounted for by an increase of low-density lipoprotein (LDL)-cholesterol. LDL-cholesterol is cleared less-efficiently from the circulation due to a decreased T3-dependent gene expression of the hepatic LDL-receptor.[63] Insulin resistance might be present in some patients in the fasting state, but is more frequent in the post-prandial state.
In patients who have hypothyroidism at birth, a goiter is not present and thyroid radioiodine uptake is low. Most infants with low FT 4 and low TSH (<20–25 μU/mL) levels are premature, manifesting transient hypothyroxinemia of prematurity. Children may present with short stature, failure to thrive or delayed skeletal maturation, which may also denote underlying concomitant GH deficiency.[47] If TSH deficiency is suspected, measurements of GH and cortisol may indicate panhypopituitarism. The presence of hypoglycemia in a term neonate should suggest GH and/or adrenocorticotrophic deficiency. Further evaluation should include a TRH test and imaging of the brain to identify hypothalamic–pituitary anomalies. In addition, DNA tests permit rapid identification of point mutations in the TSH-(beta) gene, as discussed.
Central hypothyroidism in adults is most frequently due to pituitary macroadenomas and iatrogenic causes (pituitary surgery or irradiation).[56] Clinical features may vary, depending on the cause, extent of thyroid hormone deficiency, number of associated pituitary hormone deficiencies and age of disease onset. Acquired central hypothyroidism tends to be less-severe than the congenital form.[2] Patients with central hypothyroidism have clinical features that are generally similar to patients with primary hypothyroidism, but they tend to be milder. In a study[64] reviewing the medical records of patients with central hypothyroidism, it was found that the most common symptoms were fatigue and headaches in patients with adult-onset central hypothyroidism and growth retardation in those who were diagnosed as children. In another study, the most frequent symptoms and signs observed were asthenia and edema, occurring in more than 50% of the patients, followed by drowsiness, adynamia and skin dryness.[65] Patients may complain of cold intolerance, constipation, generalized lethargy and weight gain. The skin may not be as dry and coarse, and features like periorbital edema and voice hoarseness are not as prominent.[66] Bradycardia, hypothermia, slow speech and delayed relaxation of deep tendon reflexes may be present.[47] The occurrence of TSH deficiency occurs usually after loss of GH and gonadotropin secretion in patients with secondary hypothyroidism. Features of other pituitary hormone insufficiencies such as amenorrhea, infertility, hypoglycemia, anorexia, weight loss and diabetes insipidus may be seen.
Thyroid hormones exert important influences on the skeleton, and thyroid-deficient children tend to have retarded skeletal development and delayed bone age.[67] Congenital and childhood-onset hypothyroidism severely delay skeletal development, causing growth arrest and impaired bone maturation.[68] T4 replacement induces a period of rapid “catch up” growth, but attainment of predicted adult height may not be achieved. The resultant height deficit in such cases is related to the duration of untreated hypothyroidism.[69] In the adult skeleton, thyroid hormone is required for bone maintenance. In hypothyroidism, there is reduced bone turnover, affecting both bone resorption and formation, and the prolonged formation phase leads to an increased mineralization phase.[70] The effects of adult hypothyroidism on bone turnover markers are inconclusive due to the small patient numbers studied, but histomorphometry data indicate that thyroid hormone deficiency prolongs the bone remodeling cycle and reduces bone turnover.[68] Large population studies have demonstrated that hypothyroidism is associated with a two- to three-fold increased fracture risk.[71]
Overt hypothyroidism has been linked to various types of cognitive dysfunction. In terms of mood, most studies indicate that hypothyroid patients have increased rates of anxiety and depression that may improve with L-T4 treatment.[72] In a study[73] comparing patients with overt hypothyroidism to controls, it was found that hypothyroid patients had specific deficits in verbal memory, and scored worse on depression rating scales.
Diagnosis
An inappropriately low serum TSH concentration in the presence of subnormal serum T4 and T3 concentrations is characteristic of central hypothyroidism. The diagnosis of congenital central hypothyroidism is frequently missed by current routine neonatal thyroid screening programmes as the TSH is usually in the low-normal to normal range. In about 11% cases, however, the TSH can be between 4.2 and 10, which is largely because of bioinactive but immunoactive TSH isoforms secreted by the pituitary.[73]
On the background of an appropriate clinical setting, i.e. symptomatic patient with absent goiter, diagnosis is established by biochemical testing:
Serum T3, T4, TSH
Use of serial T4 measurement[74]
Dynamic testing using the TRH-stimulation test. Serum TSH is measured serially post-TRH at 20 and 60 mts. Some authors advocate the use of the 180-mt value too. (Normal response is 20 mts TSH value higher than 60 mts TSH. A flat response is seen in pituitary disease and delayed response, with the 60-mt value higher than the 20-mt value, as seen in hypothalamic disease. This distinction is however not always clear.)[75,76]
Other biochemical markers have been studied in the evaluation of central hypothyroidism. These include cholesterol, sex hormone-binding protein, angiotensin-converting enzyme, carboxyl-terminal telopeptide of type I collagen, bone glucose-lowering agent protein and serum soluble IL-2 receptors.[65] However, they lack specificity. Anti-thyroid antibodies are invariably negative.
Appropriate neuroimaging such as magnetic resonance imaging of the pituitary gland and, less commonly, computed tomography should be employed to help identify any mass lesion as a possible cause.[47]
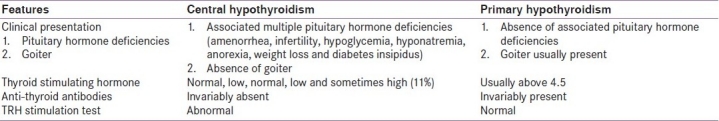
The most obvious differences between central and primary hypothyroidism have been outlined as follows [Table 2].
Table 2.
Differences between central and primary hypothyroidism
Management
Theoretically, TRH and TSH administration seem ideal; however, in view of the high costs and limited applicability, they have been abandoned.[1] Majority of the patients are treated with levothyroxine. The principles of treatment include replacement of thyroid hormone as well as treatment of co-existent pituitary hormone deficiencies, in particular glucocorticoid replacement, as administration of levothyroxine in a glucocorticoid-deficient individual may precipitate an adrenal crisis. The dose of levothyroxine required should be tailored to each individual. Children may require higher doses (around 4 mcg/kg daily) to meet the demands of growth and development. Normal infants and children have higher free-thyroid hormone levels.[77] Therefore, higher levothyroxine doses are recommended in this age group. Treatment should be started promptly in order to avoid adverse neurological sequelae associated with hypothyroidism.[78]
The recommended initial dose of T4 is 10–15 μg/kg per day, or 50 μg daily, for the average term infant weighing 3–4.5 kg. Therapy should be monitored at 4- to 6-week intervals during the first 6 months, at 2- to 3-month intervals between ages 6 and 24 months and at 3- to 6-month intervals thereafter. If the initial diagnosis cannot be established definitively, levothyroxine can be withdrawn for 30 days at age 2–3 years without compromising brain maturation to allow reassessment.[79]
The elderly patients may require lower doses (around 1 mcg/kg daily). Adults in general require around 1.6 mcg/kg of levothyroxine daily, but the optimum dose range is still unclear.[1] The aim of treatment is to achieve euthyroidism, but no consensus has been found regarding evaluation of the adequacy of replacement, as serum TSH cannot be used for diagnosis or monitoring.[80] The dose of T4 replacement should be titrated according to the patient's symptoms and serum-free T4 value, which should be kept in the upper end of the normal range.[64]
There has been a suggestion of the use of T4 plus T3 combination replacement therapy in hypothyroid patients, as it seems more physiological. However, no added superiority over T4 monotherapy was seen with regards improvement in mood and cognitive performance or metabolic parameters.[81]
An important adverse effect of thyroid replacement is hyperthyroidism from over-replacement. It is thought that more than 20% of the patients on treatment are clinically or subclinically thyrotoxic.[82] Depending on the degree of over-replacement, this can be associated with significantly increased risk of hip and vertebral fractures[83] and atrial fibrillation.[84]
Monitoring
The TSH is of no value in the follow-up of patients with central hypothyroidism, unlike primary hypothyroidism, where the TSH is the gold standard assessment. Therefore, monitoring needs to be frequent, initially at 1-2-monthly intervals, requiring:
Ft4 to be in the upper half of the reference range and
Improvement of clinical parameters while on T4 replacement, such as symptoms and heart rate response.[74]
CONCLUSION
Central hypothyroidism is most often caused by diseases of the pituitary or hypothalamus. The diagnosis is suspected by the finding of low FT4 and inappropriately low, normal or slightly increased TSH. A delayed TSH response to TRH (TRH stimulation test) supports the diagnosis. In neonates, central hypothyroidism goes undetected as most centers only use TSH evaluation. This can result in a delay in diagnosis and severe hypothyroidism, with mental and skeletal abnormalities. Fatigue can be the only presenting feature of central hypothyroidism in the absence of other pituitary hormone abnormalities. Treatment with levothyroxine is very reassuring, with dramatic improvement in symptoms. Monitoring of adequacy of therapy needs to be followed-up with serial serum T4 and T3 levels, with the aim of maintaining them in the upper range of normal. In case of associated hypocortisolism, steroid should be replaced prior to thyroid hormone replacement. Worsening of symptoms post-use of levothyroxine can serve as an indirect clue to the same (hypocortisolism).
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocr Metab. 2008;4:683–94. doi: 10.1038/ncpendmet0995. [DOI] [PubMed] [Google Scholar]
- 2.Lania A, Persani L, Beck-Peccoz P. Central hypothyroidism. Pituitary. 2008;11:181–6. doi: 10.1007/s11102-008-0122-6. [DOI] [PubMed] [Google Scholar]
- 3.Schmiegelow M, Feldt-Rasmussen U, Rasmussen AK, Poulsen HS, Müller J. A Population-based study of thyroid function after radiotherapy and chemotherapy for a childhood brain tumor. J Clin Endocr Metab. 2003;88:136–40. doi: 10.1210/jc.2002-020380. [DOI] [PubMed] [Google Scholar]
- 4.Rose SR. Cranial irradiation and central hypothyroidism. Trends Endocr Metab. 2001;12:97–104. doi: 10.1016/s1043-2760(00)00359-3. [DOI] [PubMed] [Google Scholar]
- 5.Samuels MH, Ridgway EC. Central hypothyroidism. Endocr Metab Clin North Am. 1992;21:903. [PubMed] [Google Scholar]
- 6.Morreale de Escobar G, Obregon MJ, Escobar del Rey F. Research in Congenital Hypothyroidism. New York NY: Plenum Press; 1988. Transfer of thyroid hormones from the mother to the fetus; pp. 15–28. [Google Scholar]
- 7.Pacaud D, Huot C, Gattereau A, Brown RS, Glorieux J, Dussault JH, et al. Outcome in three siblings with antibody-mediated transient congenital hypothyroidism. J Pediatr. 1995;127:275–7. doi: 10.1016/s0022-3476(95)70308-x. [DOI] [PubMed] [Google Scholar]
- 8.Francis G, Riley W. Congenital familial transient hypothyroidism secondary to transplacental thyrotropin-blocking autoantibodies. Am J Dis Child. 1987;141:1081–3. doi: 10.1001/archpedi.1987.04460100059025. [DOI] [PubMed] [Google Scholar]
- 9.Rovet JF, Hepworth SL. Dissociating attention deficits in children with ADHD and congenital hypothyroidism using multiple CPTs. J Child Psychol Psychiatr. 2001;42:1049–56. doi: 10.1111/1469-7610.00804. [DOI] [PubMed] [Google Scholar]
- 10.Zoeller RT, Rovet J. Timing of thyroid hormone action in the developing brain: Clinical observations and experimental findings. J Neuroendocr. 2004;16:809–18. doi: 10.1111/j.1365-2826.2004.01243.x. [DOI] [PubMed] [Google Scholar]
- 11.Jackson IM. Thyrotropin-releasing hormone. N Engl J Med. 1982;306:145. doi: 10.1056/NEJM198201213060305. [DOI] [PubMed] [Google Scholar]
- 12.Martino E, Lernmark A, Seo H, Steiner DF, Refetoff S. High concentration of thyrotropin-releasing hormone in pancreatic islets. Proc Natl Acad Sci U S A. 1978;75:4265. doi: 10.1073/pnas.75.9.4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gkonos PJ, Tavianini MA, Liu CC, Roos BA. Thyrotropin-releasing hormone gene expression in normal thyroid parafollicular cells. Mol Endocr. 1989;3:2101. doi: 10.1210/mend-3-12-2101. [DOI] [PubMed] [Google Scholar]
- 14.Jeffcoate SL, White N, Hokfelt T, Fuxe K, Johansson O. Proceedings: Localization of thyrotrophin releasing hormone in the spinal cord of the rat by immunohisto-chemistry and radioimmunoassay. J Endocr. 1976;69:9. [PubMed] [Google Scholar]
- 15.Bruhn TO, Rondeel JM, Bolduc TG, Jackson IM. Thyrotropin-releasing hormone (TRH) gene expression in the anterior pituitary, I: Presence of pro-TRH messenger ribonucleic acid and pro-TRH-derived peptide in a subpopulation of somatotrophs. Endocrinology. 1994;134:815. doi: 10.1210/endo.134.2.8299576. [DOI] [PubMed] [Google Scholar]
- 16.Bilek R. TRH-like peptides in prostate gland and other tissues. Physiol Res. 2000;49:S19. [PubMed] [Google Scholar]
- 17.Bodó E, Kany B, Gáspár E, Knüver J, Kromminga A, Ramot Y, et al. Thyroid-stimulating hormone: A novel, locally produced modulator of human epidermal functions, is regulated by thyrotropin-releasing hormone and thyroid hormones. Endocrinology. 2010;151:1633–42. doi: 10.1210/en.2009-0306. [DOI] [PubMed] [Google Scholar]
- 18.Schuman ML, Landa MS, Toblli JE, Peres Diaz LS, Alvarez AL, Finkielman S, et al. Cardiac thyrotropin-releasing hormone mediates left ventricular hypertrophy in spontaneously hypertensive rats. Hypertension. 2011;57:103–9. doi: 10.1161/HYPERTENSIONAHA.110.161265. [DOI] [PubMed] [Google Scholar]
- 19.Sugrue ML, Vella KR, Morales C, Lopez ME, Hollenberg AN. The thyrotropin-releasing hormone gene is regulated by thyroid hormone at the level of transcription in vivo. Endocrinology. 2010;151:793–801. doi: 10.1210/en.2009-0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nillni EA, Sevarino KA. The biology of pro-thyrotropin-releasing hormone-derived peptides. Endocr Rev. 1999;20:599. doi: 10.1210/edrv.20.5.0379. [DOI] [PubMed] [Google Scholar]
- 21.Pekary AE. Is Ps4 (prepro-TRH [160-169]) more than an enhancer for thyrotropin-releasing hormone? Thyroid. 1998;8:963. doi: 10.1089/thy.1998.8.963. [DOI] [PubMed] [Google Scholar]
- 22.Zanger K, Cohen LE, Hashimoto K, Radovick S, Wondisford FE. A novel mechanism for cyclic adenosine 3’,5’-monophosphate regulation of gene expression by CREB-binding protein. Mol Endocr. 1999;13:268. doi: 10.1210/mend.13.2.0245. [DOI] [PubMed] [Google Scholar]
- 23.Hashimoto K, Zanger K, Hollenberg AN, Cohen LE, Radovick S, Wondisford FE. cAMP response element-binding protein-binding protein mediates thyrotropin-releasing hormone signaling on thyrotropin subunit genes. J Biol Chem. 2000;275:33365. doi: 10.1074/jbc.M006819200. [DOI] [PubMed] [Google Scholar]
- 24.Shupnik MA, Ridgway EC, Chin WW. Molecular biology of thyrotropin. Endocr Rev. 1989;10:459. doi: 10.1210/edrv-10-4-459. [DOI] [PubMed] [Google Scholar]
- 25.Grossmann M, Weintraub BD, Szkudlinski MW. Novel insights into the molecular mechanisms of human thyrotropin action: Structural, physiological, and therapeutic implications for the glycoprotein hormone family. Endocr Rev. 1997;18:476. doi: 10.1210/edrv.18.4.0305. [DOI] [PubMed] [Google Scholar]
- 26.Naylor SL, Chin WW, Goodman HM, Lalley PA, Grzeschik KH, Sakaguchi AY. Chromosome assignment of genes encoding the alpha and beta subunits of glycoprotein hormones in man and mouse. Somatic Cell Genet. 1983;9:757. doi: 10.1007/BF01539478. [DOI] [PubMed] [Google Scholar]
- 27.Amir SM, Kubota K, Tramontano D, Ingbar SH, Keutmann HT. The carbohydrate moiety of bovine thyrotropin is essential for full bioactivity but not for receptor recognition. Endocrinology. 1987;120:345. doi: 10.1210/endo-120-1-345. [DOI] [PubMed] [Google Scholar]
- 28.Menezes-Ferreira MM, Petrick PA, Weintraub BD. Regulation of thyrotropin (TSH) bioactivity by TSH-releasing hormone and thyroid hormone. Endocrinology. 1986;118:2125. doi: 10.1210/endo-118-5-2125. [DOI] [PubMed] [Google Scholar]
- 29.Petersen VB, McGregor AM, Belchetz PE, Elkeles RS, Hall R. The secretion of thyrotrophin with impaired biological activity in patients with hypothalamic-pituitary disease. Clin Endocr Oxf. 1978;8:397. doi: 10.1111/j.1365-2265.1978.tb02174.x. [DOI] [PubMed] [Google Scholar]
- 30.Beck-Peccoz P, Amr S, Menezes-Ferreira MM, Faglia G, Weintraub BD. Decreased receptor binding of biologically inactive thyrotropin in central hypothyroidism. Effect of treatment with thyrotropin-releasing hormone. N Engl J Med. 1985;312:1085. doi: 10.1056/NEJM198504253121703. [DOI] [PubMed] [Google Scholar]
- 31.Dacou-Voutetakis C, Feltquate DM, Drakopoulou M, Kourides IA, Dracopoli NC. Familial hypothyroidism caused by a nonsense mutation in the thyroid-stimulating hormone beta-subunit gene. Am J Hum Genet. 1990;46:988. [PMC free article] [PubMed] [Google Scholar]
- 32.Medeiros-Neto G, Herodotou DT, Rajan S, Kommareddi S, de Lacerda L, Sandrini R, et al. A circulating, biologically inactive thyrotropin caused by a mutation in the beta subunit gene. J Clin Invest. 1996;97:1250. doi: 10.1172/JCI118540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doeker BM, Pfaffle RW, Pohlenz J, Andler W. Congenital central hypothyroidism due to a homozygous mutation in the thyrotropin beta-subunit gene follows an autosomal recessive inheritance. J Clin Endocr Metab. 1998;83:1762. doi: 10.1210/jcem.83.5.4780. [DOI] [PubMed] [Google Scholar]
- 34.Heinrichs C, Parma J, Scherberg NH, Delange F, Van Vliet G, Duprez L, et al. Congenital central isolated hypothyroidism caused by a homozygous mutation in the TSH-beta subunit gene. Thyroid. 2000;10:387. doi: 10.1089/thy.2000.10.387. [DOI] [PubMed] [Google Scholar]
- 35.Bonomi M, Proverbio MC, Weber G, Chiumello G, Beck-Peccoz P, Persani L. Hyperplastic pituitary gland, high serum glycoprotein hormone alpha- subunit, and variable circulating thyrotropin (TSH) levels as hallmark of central hypothyroidism due to mutations of the TSH beta gene. J Clin Endocr Metab. 2001;86:1600. doi: 10.1210/jcem.86.4.7411. [DOI] [PubMed] [Google Scholar]
- 36.Vallette-Kasic S, Barlier A, Teinturier C, Diaz A, Manavela M, Berthezène F, et al. PROP1 gene screening in patients with multiple pituitary hormone deficiency reveals two sites of hypermutability and a high incidence of corticotroph deficiency. J Clin Endocr Metab. 2001;86:4529. doi: 10.1210/jcem.86.9.7811. [DOI] [PubMed] [Google Scholar]
- 37.Pohlenz J, Dumitrescu A, Aumann U, Koch G, Melchior R, Prawitt D, et al. Congenital secondary hypothyroidism caused by exon skipping due to a homozygous donor splice site mutation in the TSH beta-subunit gene. J Clin Endocr Metab. 2002;87:336–9. doi: 10.1210/jcem.87.1.8154. [DOI] [PubMed] [Google Scholar]
- 38.McDermott MT, Haugen BR, Black JN, Wood WM, Gordon DF, Ridgway EC. Congenital isolated central hypothyroidism caused by a “hot spot” mutation in the thyrotropin-beta gene. Thyroid. 2002;12:1141. doi: 10.1089/105072502321085252. [DOI] [PubMed] [Google Scholar]
- 39.Deladoey J, Vuissoz JM, Domene HM, Malik N, Gruneiro-Papendieck L, Chiesa A, et al. Congenital secondary hypothyroidism due to a mutation C105Vfs114X thyrotropin-beta mutation: Genetic study of five unrelated families from Switzerland and Argentina. Thyroid. 2003;13:553–9. doi: 10.1089/105072503322238818. [DOI] [PubMed] [Google Scholar]
- 40.Radovick S, Nations M, Du Y, Berg LA, Weintraub BD, Wondisford FE. A mutation in the POU-homeodomain of Pit-1 responsible for combined pituitary hormone deficiency. Science. 1992;257:1115–8. doi: 10.1126/science.257.5073.1115. [DOI] [PubMed] [Google Scholar]
- 41.Fofanova O, Takamura N, Kinoshita E, Parks JS, Brown MR, Peterkova VA, et al. Compound heterozygous deletion of the PROP-1 gene in children with combined pituitary hormone deficiency. J Clin Endocr Metab. 1998;83:2601–4. doi: 10.1210/jcem.83.7.5094. [DOI] [PubMed] [Google Scholar]
- 42.Prieto-Tenreiro A, Diaz-Guardiola P. Isolated idiopathic central hypothyroidism in an adult, possibly caused by thyrotropin releasing hormone (TRH) deficiency. Hormones (Athens) 2010;9:176–80. doi: 10.14310/horm.2002.1268. [DOI] [PubMed] [Google Scholar]
- 43.Hayashizaki Y, Hiraoka Y, Endo Y, Matsubara K. Thyroid-stimulating hormone (TSH) deficiency caused by a single base substitution in the CAGYC region of the b-subunit. EMBO J. 1989;8:2291–6. doi: 10.1002/j.1460-2075.1989.tb08355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baquedano MS, Ciaccio M, Dujovne N, Herzovich V, Longueira Y, Warman DM, et al. Two novel mutations of the TSH-beta subunit gene underlying congenital central hypothyroidism undetectable in neonatal TSH screening. J Clin Endocr Metab. 2010;95:E98–103. doi: 10.1210/jc.2010-0223. [DOI] [PubMed] [Google Scholar]
- 45.Collu R, Tang J, Castagne J, Lagacé G, Masson N, Huot C, et al. A novel mechanism for isolated central hypothyroidism: Inactivating mutations in the thyrotropin-releasing hormone receptor gene. J Clin Endocr Metab. 1997;82:1561–5. doi: 10.1210/jcem.82.5.3918. [DOI] [PubMed] [Google Scholar]
- 46.Ma NS, Fink C, Geffner ME, Borchert M. Evolving central hypothyroidism in children with optic nerve hypoplasia. J Pediatr Endocr Metab. 2010;23:53–8. doi: 10.1515/jpem.2010.23.1-2.53. [DOI] [PubMed] [Google Scholar]
- 47.Gudmundsdottir A, Schlechte JA. Central hypothyroidism 2002;12:218-23. Endocrinologist. 2002;12:218–23. [Google Scholar]
- 48.Vagenakis AG, Braverman LE, Azizi F, Portinay GI, Ingbar SH. Recovery of pituitary thyrotropic function after withdrawal of prolonged thyroid suppression therapy. N Engl J Med. 1975;293:681–4. doi: 10.1056/NEJM197510022931402. [DOI] [PubMed] [Google Scholar]
- 49.Morita A, Meyer FB, Laws ER., Jr Symptomatic pituitary metastases. J Neurosurg. 1998;89:69–73. doi: 10.3171/jns.1998.89.1.0069. [DOI] [PubMed] [Google Scholar]
- 50.Simon N, Quyyumi SA, Rothman JG. Follicular thyroid cancer presenting as a sellar mass: Case report and review of the literature. Endocr Pract. 2004;10:62–6. doi: 10.4158/EP.10.1.62. [DOI] [PubMed] [Google Scholar]
- 51.Saeger, Wolfgang Tumor-like lesions of the pituitary and sellar region. Endocrinologist. 2002;12:300–14. [Google Scholar]
- 52.Sturniolo G, Mondello P, Bruno S, Bonfatto OE, Frattima S, Albanese A, et al. Neurobrucellosis associated with syndrome of inappropriate antidiuretic hormone with resultant diabetes insipidus and hypothyroidism. J Clin Microbiol. 2010;48:3806–9. doi: 10.1128/JCM.00721-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Basaria S, Ayala AR, Guerin C, Dobs AS. A rare pituitary lesion. J Endocr Invest. 2000;23:189–92. doi: 10.1007/BF03343705. [DOI] [PubMed] [Google Scholar]
- 54.Darzy KH, Shalet SM. Hypopituitarism as a consequence of brain tumours and radiotherapy. Pituitary. 2005;8:203–11. doi: 10.1007/s11102-006-6042-4. [DOI] [PubMed] [Google Scholar]
- 55.Constine LS, Woolf PD, Cann D, Mick G, McCormick K, Raubertas RF, et al. Hypothalamic-pituitary dysfunction after radiation for brain tumors. N Engl J Med. 1993;328:87–94. doi: 10.1056/NEJM199301143280203. [DOI] [PubMed] [Google Scholar]
- 56.Rose SR. Cranial irradiation and central hypothyroidism. Trends Endocr Metab. 2001;12:97–104. doi: 10.1016/s1043-2760(00)00359-3. [DOI] [PubMed] [Google Scholar]
- 57.Benvenga S, Campenmi A, Ruggeri RM, Trimarchi F. Hypopituitarism secondary to head trauma. J Clin Endocr Metab. 2000;85:1353–6. doi: 10.1210/jcem.85.4.6506. [DOI] [PubMed] [Google Scholar]
- 58.Adams SR, Chen H, Rotblatt M. Salicylate toxicity and central hypothyroidism. The dramatic effect of salsalate on thyroid function tests? J Gen Intern Med. 2005;20:262. [Google Scholar]
- 59.Haugen BR. Drugs that suppress TSH or cause central hypothyroidism. Best Pract Res Clin Endocr Metab. 2009;23:793–800. doi: 10.1016/j.beem.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kaptein EM, Spencer CA, Kamile MB, Nicoloff JT. Prolonged dopamine administration and thyroid hormone economy in normal and critically ill subjects. J Clin Endocrinol Metab. 1980;51:387–93. doi: 10.1210/jcem-51-2-387. [DOI] [PubMed] [Google Scholar]
- 61.Chen HF, Chen SW, Chen P, Su MC, See TT, Lee HY. Chronic glue sniffing with transient central hypothyroidism and hypergonadotropism. J Chin Med Assoc. 2005;66:747–51. [PubMed] [Google Scholar]
- 62.Diekman MJ, Romijn JA, Endert E, Sauerwein H, Wiersinga WM. Thyroid hormones modulate serum leptin levels: observations in thyrotoxic and hypothyroid women. Thyroid. 1998;8:1081–6. doi: 10.1089/thy.1998.8.1081. [DOI] [PubMed] [Google Scholar]
- 63.Walton KW, Scott PJ, Dykes PW, Davies JW. The significance of alterations in serum lipids in thyroid dysfunction, II: Alterations of the metabolism and turnover of 131I low-density lipoproteins in hypothyroidism and thyrotoxicosis. Clin Sci. 1965;29:217. [PubMed] [Google Scholar]
- 64.Alexopoulou O, Beguin C, De Nayer P, Maiter D. Clinical and hormonal characteristics of central hypothyroidism at diagnosis and during follow-up in adult patients. Eur J Endocr. 2004;150:1–8. doi: 10.1530/eje.0.1500001. [DOI] [PubMed] [Google Scholar]
- 65.Ferretti Elisabetta, Persani Luca, Jaffrain-Rea Marie-Lise, Giambona Salvatore, Tamburrano Guido, Beck-Peccoz Paolo. evaluation of the adequacy of levothyroxine replacement therapy in patients with central hypothyroidism. J Clin Endocr Metab. 1999;84:924–9. doi: 10.1210/jcem.84.3.5553. [DOI] [PubMed] [Google Scholar]
- 66.Martino E, Bartalena L, Pinchera A. Central hypothyroidism. In: Braverman LE, editor. Werner and Ingbar's the Thyroid. Philadelphia: Lippincott Williams and Wilkins; 2000. p. 762. [Google Scholar]
- 67.Bassett JH, Williams GR. Critical role of the hypothalamic-pituitarythyroid axis in bone. Bone. 2008;43:418–26. doi: 10.1016/j.bone.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 68.Gogakos AI, Duncan Bassett JH, Williams GR. Thyroid and bone. Arch Biochem Biophys. 2010;503:129–36. doi: 10.1016/j.abb.2010.06.021. [DOI] [PubMed] [Google Scholar]
- 69.Rivkees SA, Bode HH, Crawford JD. Long-term growth in juvenile acquired hypothyroidism: the failure to achieve normal adult stature. N Engl J Med. 1998;318:599–602. doi: 10.1056/NEJM198803103181003. [DOI] [PubMed] [Google Scholar]
- 70.Eriksen EF, Mosekilde L, Melsen F. Kinetics of trabecular bone resorption and formation in hypothyroidism: Evidence for a positive balance per remodeling cycle. Bone. 1986;7:101–8. doi: 10.1016/8756-3282(86)90681-2. [DOI] [PubMed] [Google Scholar]
- 71.Vestergaard P, Mosekilde L. Fractures in patients with hyperthyroidism and hypothyroidism: A nationwide follow-up study in 16,249 patients. Thyroid. 2002;12:411–9. doi: 10.1089/105072502760043503. [DOI] [PubMed] [Google Scholar]
- 72.Samuels MH. Cognitive function in untreated hypothyroidism and hyperthyroidism. Curr Opin Endocrinol Diabetes Obesit. 2008;15:429–33. doi: 10.1097/MED.0b013e32830eb84c. [DOI] [PubMed] [Google Scholar]
- 73.Miller KJ, Parsons TD, Whybrow PC, Van Herle K, Rasgon N, Van Herle A, et al. Verbal memory retrieval deficits associated with untreated hypothyroidism. J Neuropsychiatry Clin Neurosci. 2007;19:132–6. doi: 10.1176/jnp.2007.19.2.132. [DOI] [PubMed] [Google Scholar]
- 74.Mehta A, Hindmarsh PC, Stanhope RG, Brain CE, Preece MA, Dattani MT. Is the thyrotropin-releasing hormone test necessary in the diagnosis of central hypothyroidism in children. J Clin Endocr Metab. 2003;88:5696–703. doi: 10.1210/jc.2003-030943. [DOI] [PubMed] [Google Scholar]
- 75.Ormston BJ, Cryer RJ, Garry R, Besser GM, Hall R. Thyrotrophinreleasing hormone as a thyroid-function test. Lancet. 1971;2:10–4. doi: 10.1016/s0140-6736(71)90005-5. [DOI] [PubMed] [Google Scholar]
- 76.van Tijn DA, de Vijlder JJ, Vulsma T. Role of the thyrotropinreleasing hormone stimulation test in diagnosis of congenital central hypothyroidism in infants. J Clin Endocrinol Metab. 2008;93:410–9. doi: 10.1210/jc.2006-2656. [DOI] [PubMed] [Google Scholar]
- 77.Baloch Z, Carayon P, Conte-Devolx B, Demers LM, Feldt-Rasmussen U, Henry JF, et al. Laboratory medicine practice guidelines: Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid. 2003;13:3–126. doi: 10.1089/105072503321086962. [DOI] [PubMed] [Google Scholar]
- 78.Selva KA, Mandel SH, Rien L, Sesser D, Miyahira R, Skeels M, et al. Initial treatment dose of L-thyroxine in congenital hypothyroidism 2002;141:786-92. J Pediatr. 2002;141:786–92. doi: 10.1067/mpd.2002.128887. [DOI] [PubMed] [Google Scholar]
- 79.Fisher DA. Management of congenital hypothyroidism. J Clin Endocrinol Metab. 1991;72:523–9. doi: 10.1210/jcem-72-3-523. [DOI] [PubMed] [Google Scholar]
- 80.Helfand M, Crapo LM. Monitoring therapy in patients taking levothyroxine. Ann Intern Med. 1990;113:450–4. doi: 10.7326/0003-4819-113-6-450. [DOI] [PubMed] [Google Scholar]
- 81.Siegmund W, Spieker K, Weike AI, Giessmann T, Modess C, Dabers T, et al. Replacement therapy with levothyroxine plus triiodothyronine (bioavailable molar ratio 14: 1) is not superior to thyroxine alone to improve well-being and cognitive performance in hypothyroidism. Clin Endocrinol Oxf. 2004;60:750–7. doi: 10.1111/j.1365-2265.2004.02050.x. [DOI] [PubMed] [Google Scholar]
- 82.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526–34. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 83.Bauer DC, Ettinger B, Nevitt MC, Stone KL. Study of Osteoporotic Fractures Research Group. Risk for fracture in women with low serum levels of thyroid-stimulating hormone. Ann Intern Med. 2001;134:561–8. doi: 10.7326/0003-4819-134-7-200104030-00009. [DOI] [PubMed] [Google Scholar]
- 84.Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994;331:1249–52. doi: 10.1056/NEJM199411103311901. [DOI] [PubMed] [Google Scholar]


