The supply of oncologists is predicted to fall short of demand in decades to come. Addressing this workforce shortage by employing nonphysician practitioners as a routine part of practice can substantially benefit both patients and providers.
Abstract
Purpose:
ASCO projects a shortfall of oncologists in the next decade. The study was designed to address the workforce shortage by exploring collaborative oncology practice models that include nonphysician practitioners (NPPs).
Methods:
ASCO contracted with Oncology Metrics, a division of Altos Solutions, to conduct a national survey of NPP integration and identify collaborative practice models and services provided by NPPs, as the first phase of the ASCO Study of Collaborative Practice Arrangements. Results of the national survey were used to identify practices for the next phase, in which selected practices participated in a more detailed data survey and satisfaction surveys. Focus groups or interviews were conducted with NPPs to collect additional subjective information to inform the project.
Results:
The incident-to practice model was the predominant model. Satisfaction was universally high for patients and generally high for physicians and NPPs. In virtually all cases (98%), patients recognized they were seeing an NPP rather than a physician. Practices in which the NPP worked with all practice physicians showed significantly higher productivity than those practices in which the NPP worked exclusively with a specific physician or group of physicians.
Conclusion:
The use of NPPs in oncology practices increases productivity for the practice and provides high physician and NPP satisfaction. Patients were aware when care was provided by an NPP and were very satisfied with all aspects of the collaborative care that they received. The integration of nonphysician practitioners into oncology practice offers a reliable means to address increased demand for oncology services without adding physicians.
Introduction
ASCO projects a shortfall of oncologists in the next decade, with the demand for oncologists outpacing the supply of new oncologists going into clinical practice. Demand for visits to oncologists is expected to increase 48% by 2020, whereas supply will rise by only 14%. The doubling of the number of Americans 65 years and older and an 81% increase in people living with, or surviving, cancer will drive this demand.1
ASCO's Workforce Advisory Group has suggested that expanded use of nonphysician practitioners (NPP)—generally nurse practitioners and physician assistants in the oncology practice setting—has the potential to extend the supply of oncologist services, particularly in the context of ongoing care and care for the growing number of cancer survivors. Better integration of NPPs also could improve practice quality and efficiency and, by better balancing workload and skills, may increase professional satisfaction for providers.
The ASCO Study of Collaborative Practice Arrangements (SCPA) was designed to address the workforce shortage by exploring collaborative practice models between oncologists and NPPs. The goals of the SCPA were to inventory and describe model practices for collaboration between oncologists and NPPs; document the impact of collaborative practice models on practice productivity and efficiency; and document the impact of collaborative practice models on patient, oncologist, and NPP satisfaction. ASCO contracted with Oncology Metrics, a division of Altos Solutions (Los Altos, CA), to conduct this study.
Methods
The SCPA was launched in March 2009 with a national survey of oncology practices. This brief survey identified practices that have integrated NPPs across a range of practice types (eg, physician-owned private practice, hospital-owned practice, academic) and identified the collaborative practice model and services provided by the NPPs in each of the responding practices. A total of 226 practices participated in the survey (“survey group”).
Results of the national survey were used to identify practices for the next phase of the SCPA, a more in-depth study of practices. The primary goal of practice selection was diversity. In an attempt to increase the number of hospital-owned practices in the study, we reached out to the Association of Cancer Executives, a national organization whose members are primarily cancer program administrators in institution-based programs, and with their assistance added several practices to the survey group. Practice size, geographic location, and collaborative practice model were evaluated, and selected practices were then invited to participate in the study. Thirty-three practices were initially chosen for participation (“study group”). Study requirements included submission of practice data such as staffing information, visit volumes, and practice expense data; completion of physician and NPP satisfaction surveys; and distribution of patient satisfaction surveys. The SCPA was granted an exemption from review by the New England Institutional Review Board in Cambridge, MA.
A second survey was administered to the study group to further refine the practice information and begin analysis of practice efficiency measures. Data were collected for a discrete 6-month period. Objective data elements collected in this survey included units of service provided, total practice expense, and total drug expense.
Satisfaction with the collaborative practice model in each practice was measured through surveys of physicians, NPPs, and patients. Physicians and NPPs were invited to participate in a brief online satisfaction survey. Several follow-up contacts were made to the practitioners to increase participation. Patient satisfaction was measured by using an anonymous paper-based survey instrument that was provided to each practice in the study group for distribution. Practices were instructed to have NPPs distribute the surveys to all patients being seen by the NPP on a given day. This ensured that the patients participating in the study were indeed receiving care in a collaborative practice model. Patients were instructed to complete the survey at home and return it in a stamped, self-addressed envelope. Patient surveys were mailed to an independent third-party survey organization for data aggregation. At the completion of the data collection phase of the study, focus groups and individual interviews were completed with NPPs from the study group practices to collect qualitative information to further inform the project.
Results and Discussion
Demographics
The survey group included respondents from 226 practices in 43 states. The majority (73%) of the respondents were from physician-owned private practices; academic practices (8%), hospital-owned practices (12%) and other types (7%) were also represented. As a first step in identifying practices appropriate for the study group, respondents were asked whether they employ NPPs in their medical oncology practice; 58% of the survey group respondents said yes.
Although not a primary goal of the project, respondents who did not use NPPs were asked to indicate their primary reason for not doing so. The most prevalent responses included “physicians are not interested in working with NPPs,” “we do not have the patient volume to support an NPP,” and “we have worked with NPPs in the past and it didn't work out.”
Practices in the study group were selected from the survey group. The primary goal of practice selection was to achieve variety in practice size, structure, and geographic distribution. Thirty-three practice sites in 24 states agreed to participate. Approximately 40% of the study group practices were from the midwest, 30% from the east coast, 20% from the west, and 10% from the south. Two sites withdrew very early in the study, one small practice because their only NPP left the practice, the second because of reluctance to share data required for the study. Of the 31 remaining practice sites, 27 provided complete data for the study.
Similar to the survey group, the majority (84%) of the study group practices were physician-owned private practices; 16% were hospital-owned practices. Academic practices were excluded from the study group at the direction of the Workforce Advisory Group.
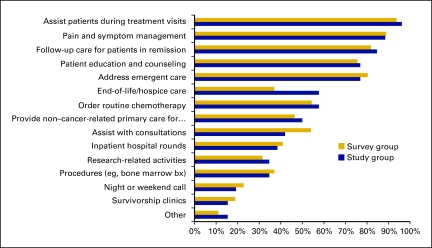
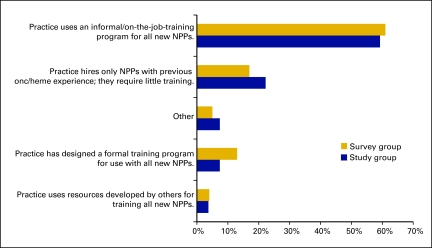
Practices were instructed to indicate the services routinely provided by NPPs from a list of 15 options. Figure 1 shows the percentage of respondents providing services in each of the listed categories for both the survey group and the study group. As can be observed here, results for the two groups are remarkably consistent, particularly for the services most frequently provided. Figure 2 shows the training model used by both the survey and study groups, and once again the results are remarkably consistent between the two. Other data in the study showed these same similarities. Although the study group data set is small, we believe the study group is representative of the larger survey group.
Figure 1.
Services provided by nonphysician practitioners. bx, biopsy.
Figure 2.
Training for new nonphysician practitioners (NPPs).
Practice Models
Buswell et al2 reported results from a single-institution academic practice study of provider practice models in July 2009. In that article, the authors defined three practice models: the independent visit model, the shared visit model, and the mixed visit model. We revised these models to apply more closely to practice style in the physician office and hospital settings. Survey respondents were asked to identify their practice model from three descriptive options; responses were then categorized into one of three collaborative practice models.
In the incident-to practice model (ITPM), NPPs routinely see patients independent of the physician. The physician is generally present in the office suite but does not routinely see patients with the NPP.
In the shared practice model, NPPs always see patients in conjunction with the physician.
In the independent practice model, NPPs see patients completely independent of the physician. Patients are assigned to the NPP and not assigned to an oncologist.
The ITPM is the prevalent model in both the survey group and the study group (Appendix Table A1, online only). This is clearly a response to the increasingly challenging economic environment for oncology practices today. In the ITPM, NPPs see patients independent of the physician but with a physician present and available in the office if needed. The NPPs follow a care plan developed by the physician and consult with the physician as necessary. In many practices that use this model, patients alternate visits between the NPP and the physician on a predetermined schedule. This allows both the NPP and physician to maximize their patient schedules. Importantly, in the private practice setting, the ITPM allows practices to bill Medicare for NPP services as though they were rendered by the physician and to receive reimbursement at the full physician fee schedule rate, rather than at 85% of the physician fee schedule as would be required if the services were billed under the NPP's own provider number. The ITPM not only provides access to both the NPP and physician at alternating visits, but also maximizes reimbursement, an important consideration for today's oncology practice.
In addition to the collaborative practice model, respondents were also asked to report on their collaborative style. Collaborative styles were characterized as “all” when the NPPs work with all practice physicians and see a wide variety of patients (approximately 60% of the study group practices), or “exclusive” when the NPPs work exclusively with a specific physician (or physicians) and see only their patients (35% of study group practices). The remaining 5% indicated that their NPPs generally work with specific physicians but there is not exclusivity.
Satisfaction
As previously stated, one goal of the SCPA was to document the impact of collaborative practice models on patient, oncologist, and NPP satisfaction. Patient satisfaction was measured through the use of an anonymous paper-based survey instrument that was distributed to patients by NPPs in the study group practices during patient visits. Surveys were completed and returned by 1,538 patients in the original 33 practice sites; data are presented for 1,237 patients in the 27 sites that provided complete data for the study.
Patients were first surveyed to assess the level of their awareness that an NPP was providing clinical service to them. The average of patient awareness for the study group was 98%. The data reveal that in every study site the overwhelming majority of the patients who responded to this question were aware that they received treatment from an NPP.
Eight dimensions of patient satisfaction with their care in a collaborative practice model were measured in the survey. Each response was assigned a numerical value ranging from +2 for “highly satisfied, ” “excellent,” or “highly likely to recommend” to −2 for “highly dissatisfied, ” “poor,” or “highly unlikely to recommend.” For each of these questions, adding the ratings of each respondent from the practice to each question and then dividing the sum by the total number of respondents generated a weighted satisfaction score. Because +2 would indicate that every respondent rated at the highest possible level of satisfaction, a score of 16 represents perfect satisfaction on every dimension. The average overall satisfaction score for patients in all study sites was 14.8 or 92.5%; patients were extremely satisfied with the service that they received at every study site.
Six dimensions of physician satisfaction with their collaborative practice model were measured by using an online satisfaction survey tool. As with the patient satisfaction survey, each response was assigned a numerical value for analysis. Responses for four questions ranged from +2 to −2, with the same rating descriptors used for patient satisfaction; two questions had a three-point range, with +1 as the highest possible score and −1 the lowest. The physician score for each question was added to calculate a total for all physicians at each study site. That sum was then divided by the number of physicians to get the average for the responding physicians at the site. A score of 10 represents perfect satisfaction. Although patient satisfaction was universally high in every dimension at every study site, physician satisfaction varied from site to site. The average overall physician satisfaction score for the study group was 7.98, or 79.8%.
Five dimensions of NPP satisfaction with the collaborative practice model were measured. As with the patient and physician satisfaction scores, the NPP score for each question was added to calculate a total for all NPPs at each study site. That sum was then divided by the number of NPPs to get the average for the responding NPPs at the site. For each of the five questions, 10 represents perfect satisfaction on every dimension measured. As was observed with the measurement of physician satisfaction, there is some variation in NPP satisfaction; the average overall NPP satisfaction score was 7.82, or 78.2%. There is no correlation (coefficient of correlation = 0.16) between the physician and NPP satisfaction scores.
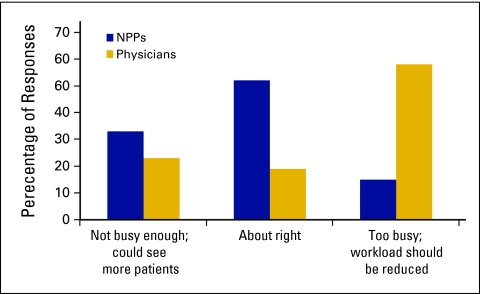
Perception of Workload
In addition to measuring satisfaction, we also asked physicians and NPPs in the study group to indicate their perception of their own workload (Figure 3). The majority (58%) of physicians responded that their workload was too busy. Conversely, slightly more than 50% of NPPs said that their workload was about right, and another 33% felt they were not busy enough and could see more patients.
Figure 3.
Perception of workload among physicians and nonphysician practitioners (NPPs).
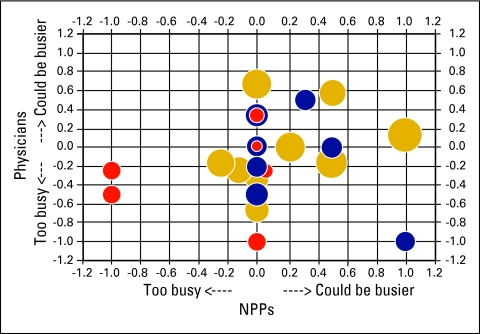
Productivity
Another goal of the SCPA was to document the impact of collaborative practice models on practice productivity and efficiency. Study group practices reported the number of patient encounters for selected evaluation and management codes for a 6-month reporting period. The total number of patient encounters was divided by the total number of full-time equivalent (FTE) providers, defined as physicians and NPPs. Productivity was reported at the provider level for each practice. We then looked at the correlation between perception of workload and productivity as measured by the number of patient encounters per FTE provider (Figure 4).
Figure 4.
Perception of workload and patient encounters per full-time equivalent (FTE) provider. Each circle represents a practice; their size and color indicate practice productivity based on the number of patient encounters per FTE provider in the reporting period. The smaller red circles indicate below average productivity; blue is average; and the larger gold circles indicate greater than average productivity. The horizontal axis reflects the nonphysician provider (NPP) perception of workload and the vertical axis the physician perception. Circles in the upper right quadrant represent sites where both physicians and NPPs think they could see more patients. Circles in the lower left quadrant represent sites where both the physicians and the NPPs think they are seeing too many patients.
As shown in Figure 4, there is no correlation between the subjective perception and objective measurement of workload. Larger gold circles, indicating higher productivity per FTE provider, appear in the upper right quadrant (could be busier); smaller red circles, indicating lower productivity, appear in the lower left quadrant (too busy). It appears that being busy reinforces the idea that more patients could be seen; five of the nine practices that produced higher than average patient encounters per FTE provider felt they could be even busier. Conversely, being less busy is associated with the subjective perception of being able to see fewer patients, as demonstrated by three of the eight practices with lower than average productivity.
Collaborative Style and Productivity
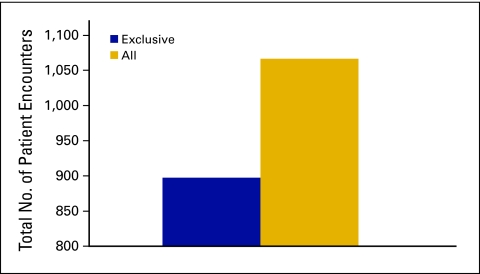
We also analyzed the correlation between collaborative style and productivity. The average number of patient encounters per FTE provider for the group in which the collaborative style was “exclusive” (NPPs work exclusively with specific physician(s) and see only their patients) was 897 ± 146 in the 6-month observation period, with 95% confidence. The average number of patient encounters per FTE provider for the group in which the collaborative style was “all” (NPPs work with all practice physicians and see a wide variety of patients) was 1,066 ± 146 in the observation period, with 95% confidence. The difference represents a productivity increase of 19% in favor of the sites where NPPs work with all physicians (Figure 5).
Figure 5.
Collaborative style and total patient encounters per full-time equivalent provider.
Conclusion
Although there are many interesting observations to be made from the data collected in this study, there are five important conclusions. First, oncology patients are aware when care is provided by an NPP and are very satisfied with the care they receive in a collaborative practice model. This is evidence that such collaborative practice arrangements are well accepted by patients, and we believe there should be no lingering concerns that patients will react negatively to oncology care provided by nonphysician practitioners in a collaborative practice model.
Second, practices in which the NPPs work with all practice physicians and see a wide variety of patients demonstrate a 19% increase in productivity as measured by patient encounters per FTE provider compared with practices in which NPPs work exclusively with one or more physicians in the practice.
Next, in both the survey group and the study group, reimbursement economics appear to drive the selection and development of the collaborative practice. This is evidenced by the prevalence of the incident-to practice model in this study.
Another important conclusion is that there is little observed correlation between the subjective perception of workload and the objective measure of work production. Five of the nine practices that produced higher than average patient encounters per FTE provider indicated that they could be even busier. Conversely, three of the eight practices with lower than average productivity reported that they were too busy.
Finally, physician and NPP satisfaction with their collaborative practice model is high, indicating a positive professional experience. Taken together, these findings provide strong support for the inclusion of NPPs in oncology practices.
Acknowledgment
This study was funded by Susan G. Komen for the Cure and conducted for ASCO. Analysis was conducted by Oncology Metrics, a division of Altos Solutions, under the guidance of the ASCO Workforce Advisory Group. We thank members of the ASCO Workforce Advisory Group for their participation in this project, including Michael A. Goldstein, MD, Co-Chair, Beth Israel Deaconess Medical Center, Boston, MA; Dean Bajorin, MD, Co-Chair, Memorial Sloan-Kettering Cancer Center, New York, NY; Michael P. Kosty, MD, Scipps Clinic, La Jolla, CA; R. Steven Paulson, MD, Baylor Charles A. Sammons Cancer Center, Dallas, TX; Kathleen W. Beekman, MD, Ypsilanti, MI; Patrick A. Grusenmeyer, ScD, Helen F. Graham Cancer Center, Newark, DE; Gladys I. Rodriguez, MD, South Texas Oncology Hematology, San Antonio, TX; Stephanie F. Williams, MD, Hematology-Oncology Associates of Illinois, Chicago, IL. We also thank Suanna Bruinooge and M. Kelsey Mace for their contributions to the study.
Appendix
Table A1.
Collaborative Practice Models
| Model | Survey Group | Study Group |
|---|---|---|
| Incident-to practice | 101 | 26 |
| Shared practice | 17 | 2 |
| Independent practice | 11 | 2 |
| Blend | 3 | 0 |
Footnotes
See article in Journal of Clinical Oncology 29:3599–3600, 2011
Authors' Disclosures of Potential Conflicts of Interest
Although all authors completed the disclosure declaration, the following authors indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Elaine L. Towle, Oncology Metrics, a division of Altos Solutions (C); Thomas R. Barr, Oncology Metrics, a division of Altos Solutions (C) Consultant or Advisory Role: None Stock Ownership: None Honoraria: None Research Funding: None Expert Testimony: None Other Remuneration: None
Author Contributions
Conception and design: Elaine L. Towle, Thomas R. Barr, Amy Hanley, Michael Kosty, Stephanie Williams, Michael A. Goldstein
Administrative support: Elaine L. Towle, Thomas R. Barr, Amy Hanley
Provision of study materials or patients: Elaine L. Towle, Thomas R. Barr
Collection and assembly of data: Elaine L. Towle, Thomas R. Barr
Data analysis and interpretation: Elaine L. Towle, Thomas R. Barr, Michael Kosty, Michael A. Goldstein
Manuscript writing: Elaine L. Towle, Thomas R. Barr, Amy Hanley, Michael Kosty, Stephanie Williams, Michael A. Goldstein
Final approval of manuscript: Elaine L. Towle, Thomas R. Barr, Amy Hanley, Michael Kosty, Stephanie Williams, Michael A. Goldstein
References
- 1.Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buswell LA, Ponte PR, Shulman LN. Provider practice models in ambulatory oncology practice: Analysis of productivity, revenue, and provider and patient satisfaction. J Oncol Pract. 2009;5:188–192. doi: 10.1200/JOP.0942006. [DOI] [PMC free article] [PubMed] [Google Scholar]