Abstract
A patient with anaplastic meningioma and lung metastases resistant to conventional treatment underwent radiopeptide therapy with 177Lu- DOTA-octreotate in our institute. The treatment resulted in significant improvement in patient's quality of life and inhibition of tumor progression. This case may eventually help to establish the value of radiopeptide therapy in patients with this rare condition.
Keywords: 18F-FDG-PET/CT, anaplastic meningioma, 111In-DTPA-octreotide, radio receptor therapy
Background
Meningiomas are generally slow-growing lesions that arise from intracranial and spinal meninges. They are usually perceived as benign tumours for which radical surgery is the treatment of choice [1]. However, they may occasionally behave aggressively in atypical or malignant meningiomas, invading the brain and/or metastasising outside the CNS, which occurs in only 0.01% of all cases [2]. The most common extracranial location of metastasis is the lung followed by liver, lymph nodes and bones [3,4]. Meningiomas present ideal targets for somatostatin receptor scintigraphy (SRS) with 111In-DTPA-octreotide. However, the value of the radioreceptor therapy using radiolabeled somatostatin analog 177Lu-DOTA-octreotate is not yet well established in patients with metastasized or inoperable meningiomas [5,6]. Here, we present a patient with metastatic anaplastic meningioma who benefited from radiopeptide targeting.
Case presentation
A 62 year old female with intracranial anaplastic meningioma was referred to our department for a restaging with 18F-fluorodeoxyglucose (FDG)-PET/CT. The patient suffered from a protrusio bulbi of the left eye and progressive facial pain. No conventional treatment option could be offered to the patient, who had undergone multiple surgical resections and percutaneous radiation before.
The fused PET/CT images (Biograph; Siemens Medical Solutions Inc) manifested multifocal accumulation in the left temporal region with local bone infiltration. Furthermore, they demonstrated multiple pulmonary metastases in the upper lobe of the left lung (Figure 1). In view of these findings, including the diagnosis of pulmonary metastases, the patient was referred for SRS to evaluate the option of a palliative radiopeptide therapy with 177Lu- DOTA-octreotate. SRS images showed strong uptake in the left temporal region as well as in the upper lobe of the left lung, consistent with the PET/CT findings (Figure 2). Due to the abundance and high affinity of somatostatin receptors (sstr), we performed radiopeptide therapy with 177Lu- DOTA-octreotate consisting of 3 cycles (cumulative dose: 691 mCi) without any serious side effects (Figure 3). The patient experienced a dramatic reduction of facial pain assessed by visual analogue scale (VAS) as well as a significant improvement in quality of life with a 30% increase in her performance status using karnofsky scoring 6 weeks after commencement of the treatment. Disease stabilization could also be achieved, according to functional MD Anderson criteria, evaluated 3 months after termination of radiopeptide therapy [7]
Figure 1.

Maximal intensity projection visualisation of PET/CT demonstrating the intracranial meningioma and its pulmonary metastases.
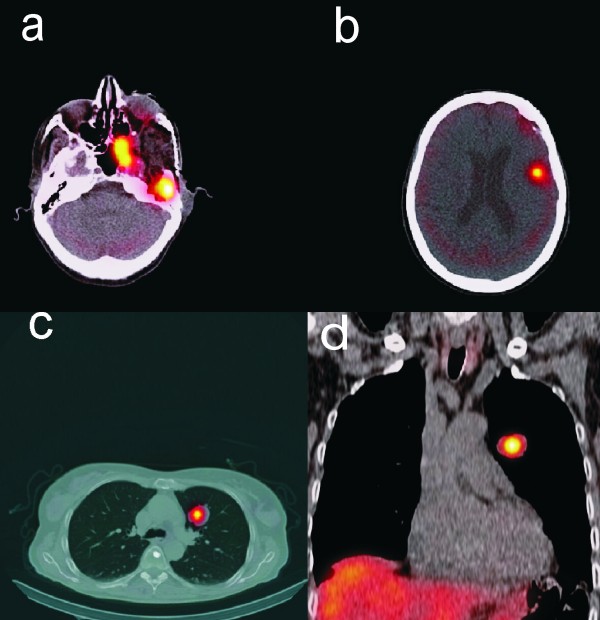
Figure 2.
SPECT/CT images of somatostatin receptor scintigraphy display avid uptake in the intracranial meningioma (2a and b) as well as in the pulmonary metastases (2c and d).
Figure 3.
Post-therapeutic 177Lu- DOTA-octreotate images show radiopeptide accumulation in the tumors (A: anterior view, B: posterior view).
Discussion
The local recurrence rate of meningioma is determined by the extent of the resection, histopathological grade and biological aggressiveness of the tumor [8,9]. Once a meningioma recurs, it is more likely to recur again later, resulting in a poor prognosis of the patient [10]. 18F-FDG-PET/CT has been commonly used in patients with primary tumours of central nervous system including meningioma for tumor grading, determination of the prognosis and discrimination of tumor recurrence from radiation necrosis [11,12]. With their high sstr density and location outside the blood-brain barrier, meningiomas also present ideal targets for SRS with 111In-DTPA-octreotide which is the main imaging technique for neuro endocrine tuomors (NETs) but may be also used in other tumors expressing somatostatin receptors such as neuroblastoma, pheochromocytoma and paraganglioma [13-15]. This procedure is used apart from staging and monitoring the effect of treatment for selecting patients for peptide receptor radionuclide therapy (PRRT), primarily used in gastroenteropancreatic NETs with very encouraging results. The value of PRRT is not yet well established in patients with meningiomas [5]. Our patient experienced a dramatic symptomatic relief as well as a significant improvement in quality of life following the PRRT along with inhibition of tumor progression.
Conclusions
The presented case may help to establish the value of PRRT in patients with the rare condition of anaplastic meningioma.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Conception of the case report: A.S., S.E., HJ.B.; Collection and assembly of data: H.A., W.W., U.H.; Literature review and interpretation of data: A.S. S.E., H.A.; Drafting of the article: A.S., HJ.B., S.E.; Critical revision of the article for important intellectual content: U.H., H.A. W.W. All authors have read and approved the final manuscript.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Contributor Information
Amir Sabet, Email: amir.sabet@ukb.uni-bonn.de.
Hojjat Ahmadzadehfar, Email: hojjat.ahmadzadehfar@ukb.uni-bonn.de.
Ulrich Herrlinger, Email: ulrich.herrlinger@ukb.uni-bonn.de.
Winfried Wilinek, Email: winfried.wilinek@ukb.uni-bonn.de.
Hans-Jürgen Biersack, Email: hans-juergen.biersack@ukb.uni-bonn.de.
Samer Ezziddin, Email: samer.ezziddin@ukb.uni-bonn.de.
References
- Alvarez F, Roda JM, Perez Romero M, Morales C, Sarmiento MA, Blazquez MG. Malignant and atypical meningiomas: a reappraisal of clinical, histological, and computed tomographic features. Neurosurgery. 1987;20(5):688–694. doi: 10.1227/00006123-198705000-00003. [DOI] [PubMed] [Google Scholar]
- Figueroa BE, Quint DJ, McKeever PE, Chandler WF. Extracranial metastatic meningioma. Br J Radiol. 1999;72(857):513–516. doi: 10.1259/bjr.72.857.10505022. [DOI] [PubMed] [Google Scholar]
- Karasick JL, Mullan SF. A survey of metastatic meningiomas. J Neurosurg. 1974;40(2):206–212. doi: 10.3171/jns.1974.40.2.0206. [DOI] [PubMed] [Google Scholar]
- Kodama K, Doi O, Higashiyama M, Horai T, Tateishi R, Nakagawa H. Primary and metastatic pulmonary meningioma. Cancer. 1991;67(5):1412–1417. doi: 10.1002/1097-0142(19910301)67:5<1412::AID-CNCR2820670523>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- van Essen M, Krenning EP, Kooij PP. et al. Effects of therapy with [177Lu-DOTA0, Tyr3]octreotate in patients with paraganglioma, meningioma, small cell lung carcinoma, and melanoma. J Nucl Med. 2006;47(10):1599–1606. [PubMed] [Google Scholar]
- Bartolomei M, Bodei L, De Cicco C. et al. Peptide receptor radionuclide therapy with (90)Y-DOTATOC in recurrent meningioma. Eur J Nucl Med Mol Imaging. 2009;36(9):1407–1416. doi: 10.1007/s00259-009-1115-z. [DOI] [PubMed] [Google Scholar]
- Costelloe CM, Chuang HH, Madewell JE, Ueno NT. Cancer Response Criteria and Bone Metastases: RECIST 1.1, MDA and PERCIST. J Cancer. 2010;1:80–92. doi: 10.7150/jca.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marosi C, Hassler M, Roessler K. et al. Meningioma. Crit Rev Oncol Hematol. 2008;67(2):153–171. doi: 10.1016/j.critrevonc.2008.01.010. [DOI] [PubMed] [Google Scholar]
- Takahashi JA, Ueba T, Hashimoto N, Nakashima Y, Katsuki N. The combination of mitotic and Ki-67 indices as a useful method for predicting short-term recurrence of meningiomas. Surg Neurol. 2004;61(2):149–155. doi: 10.1016/S0090-3019(03)00575-5. discussion 155-146. [DOI] [PubMed] [Google Scholar]
- Commins DL, Atkinson RD, Burnett ME. Review of meningioma histopathology. Neurosurg Focus. 2007;23(4):E3. doi: 10.3171/FOC-07/10/E3. [DOI] [PubMed] [Google Scholar]
- Delbeke D, Meyerowitz C, Lapidus RL. et al. Optimal cutoff levels of F-18 fluorodeoxyglucose uptake in the differentiation of low-grade from high-grade brain tumors with PET. Radiology. 1995;195(1):47–52. doi: 10.1148/radiology.195.1.7892494. [DOI] [PubMed] [Google Scholar]
- Hustinx R, Pourdehnad M, Kaschten B, Alavi A. PET imaging for differentiating recurrent brain tumor from radiation necrosis. Radiol Clin North Am. 2005;43(1):35–47. doi: 10.1016/j.rcl.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Sisson JC, Shulkin BL. Nuclear medicine imaging of pheochromocytoma and neuroblastoma. Q J Nucl Med. 1999;43(3):217–223. [PubMed] [Google Scholar]
- Schmidt M, Scheidhauer K, Luyken C. et al. Somatostatin receptor imaging in intracranial tumours. Eur J Nucl Med. 1998;25(7):675–686. doi: 10.1007/s002590050269. [DOI] [PubMed] [Google Scholar]
- Nathoo N, Ugokwe K, Chang AS. et al. The role of 111indium-octreotide brain scintigraphy in the diagnosis of cranial, dural-based meningiomas. J Neurooncol. 2007;81(2):167–174. doi: 10.1007/s11060-006-9210-5. [DOI] [PubMed] [Google Scholar]