Abstract
Background
Panic Disorder with/without Agoraphobia (PD/PDA) is a prevalent anxiety disorder, associated with impairment in quality of life and functionality, as well as increased healthcare utilization. Extant research shows a relationship between stressful life events (SLEs) and the onset of panic attacks in adults who ultimately develop PD/PDA. However, limited attention has been paid to how SLEs might affect the severity of panic symptoms in individuals with PD/PDA. In this study, we examined the relationship between SLEs and panic symptom severity in adults with PD/PDA.
Methods
Four hundred-eighteen adults with PD/PDA from the Harvard/Brown Anxiety Research Program (HARP), a long-term prospective longitudinal observational multicenter study of adults with a current or past history of anxiety disorders were included in this study. We examined occurrence of SLEs and their impact on panic symptom severity 12-weeks pre- and post-SLE.
Results
A time-slope effect showed that participants had worsened panic symptoms over the course of the 12-weeks after family/friends/household and work SLEs. That is, their symptoms worsened progressively after the event, rather than immediately thereafter (i.e., significant symptom change within the same week of the event).
Limitations
The sample may not be representative of the general population.
Conclusions
These findings provide new insights into how SLEs affect panic symptoms in adults with PD/PDA in that household-related SLEs, such as serious family arguments, and work-related SLEs, such as being fired, put some adults at risk for worsened panic symptoms within 12-weeks of the event.
Keywords: Panic Disorder, Panic Disorder with Agoraphobia, Stressful Life Events
Panic Disorder and Panic Disorder with Agoraphobia (PD/PDA) are common and debilitating conditions. Recent estimates suggest that 3.7% of people will meet criteria for PD and 1.1% for PDA in their lifetime (Kessler et al., 2006). PD/PDA is associated with significant impairment in quality of life and role functioning (Hollifield et al., 1997; Stein, et al., 2005). Moreover, PD/PDA is associated with increased healthcare utilization (Rief, Martin, Klaiberg, & Brähler, 2005), decreased productivity in the form of increased disability (Kouzis & Eaton, 1994), and missed work days (Stein et al., 2005). Given the prevalence and burden associated with these disorders, it is important to delineate factors that may influence the course and severity of PD/PDA.
Previous data supports the association between stressful life events (SLEs) and the onset of PD/PDA in adulthood, with SLEs being a precursor (in the prior year) to individuals’ first panic attack in 80–100% of cases (see Klauke et al., 2010 for a review). SLEs associated with PD/PDA onset include: threats to primary relationships, such as interpersonal conflict and separation or loss; as well as threats to health, including physical illness. Less is known about the temporal relationship between SLEs and PD/PDA course (e.g., do SLEs lead to worsened PD/PDA symptoms?). A better understanding of the role SLEs play in the course of PD/PDA could help clinicians anticipate factors that might put their patients at risk for worsening illness.
No study to date has examined the longitudinal relationship between SLEs and the symptomatic course of PD/PDA in adults. Thus, we examined the impact of SLEs on the course of PD/PDA in 418 adults participating in the Harvard/Brown Anxiety Research Program (HARP). We hypothesized that SLEs would be the antecedent to worsening severity of current PD/PDA, as measured by changes in panic symptoms. We investigated the immediate impact SLEs had on panic symptom severity (i.e., how do symptoms change within the week of the actual SLE?), whether or not SLEs impacted panic symptom severity in the 12 weeks prior to their occurrence (e.g., does the anticipation of an upcoming SLE (e.g., divorce) worsen panic symptoms even before the SLE actually occurs?), and whether or not SLEs had a residual effect on symptoms over the 12 weeks after their occurrence (i.e., does the SLE trigger a progressive worsening in symptoms over time?). Given the exploratory nature of this study, we did not make specific predictions regarding which SLEs would be associated with symptom change.
Methods
Participants
Participants were part of the Harvard/Brown Anxiety Research Program (HARP), a prospective, longitudinal, observational study of adults with a current or past history of anxiety disorders. In total, 711 participants were recruited from psychiatry clinics of 11 hospitals in Massachusetts and Rhode Island. HARP Inclusion criteria were a past or current diagnosis of PD or PDA, Agoraphobia without PD, Social Phobia (SP), or Generalized Anxiety Disorder (GAD). Participants were at least 18 years of age at intake and willing to complete informed consent for participation. Exclusion criteria were the presence of an organic brain syndrome, a history of Schizophrenia, or current psychosis. The study protocol was approved by the institutional review board at each study site. HARP methods are described in detail elsewhere (Keller et al., 1994). Analyses were limited to 418 participants who met criteria for PD (n=78)/PDA (n=340) at intake.
Procedures
An initial diagnostic interview assessed lifetime psychopathology and functional history using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R Non-Affective Disorders – Patient Version (SCID-P; Spitzer, Williams, Gibbon, & First, 1988) and the Research Diagnostic Criteria (RDC) Schedule for Affective Disorders – Lifetime (SADS-L; Endicott & Spitzer, 1978). Items on the SCID-P and SADS-L were combined to create the SCALUP, a structured interview used to assess diagnoses at intake. This instrument assessed both present and past RDC diagnoses for affective disorders and DSM-IIIR diagnoses for non-affective (including anxiety) disorders. Interviews were conducted by bachelor’s- and master’s-level clinical interviewers. Participants completed assessments at baseline and subsequent follow-ups were obtained at 6-month, 1-year, and annually thereafter. Data on SLEs were collected during years 9–15 of HARP; therefore, the data in this report were collected during those years.
Measures
Longitudinal Interval Follow-Up Evaluation
(LIFE; Keller, Lavori, Friedman, & Nielsen, 1987). The LIFE is an interviewer-administered assessment that collects detailed information on anxiety disorder symptoms, psychosocial functioning, and treatment status. The LIFE uses a 6-point psychiatric status rating (PSR) scale to indicate the severity of psychiatric pathology. For PD/PDA, PSR ratings focus on severity of panic symptoms. A PSR of 6 indicates one or more panic attack per day; PSR 5 indicates one panic attack per week; PSR 4 represents “persistent fear of panic attack,” without attacks actually occurring; PSR 3 indicates the presence of limited symptom attacks only; PSR 2 equals,” No attacks, though sometimes feels on verge of attack, but is able to control it;” and, PSR 1 means none of the above symptoms. Interrater reliability and long-term test-retest reliability for the LIFE diagnostic ratings has been found to be good to excellent for all anxiety disorders and MDD (Warshaw, Keller, & Stout, 1994).
The Short Life Events and Difficulties Scale
(SLEDS; Smith & Oatley, 1997) The SLEDS is a shortened version of the Life Events and Difficulties Scale (LEDS; Brown & Harris, 1978), a semi-structured life events interview typically used to collect information about stressful experiences. It distinguishes acute and ongoing stressors, and gathers contextual and subjective ratings of these experiences. The SLEDS has the same format as the original LEDS but was developed specifically to assess those events and difficulties thought to be of etiological significance for depression. The LEDS is a reliable and valid measure of life stress (Brown & Harris, 1989) and the SLEDS has been demonstrated to predict depression at a rate that is highly comparable to that of the original interview (Smith & Oatley, 1997). The SLEDS assesses for the occurrence of the following nine life event domains, with multiple events included in each domain: school event (e.g., dropped out of school or training program), work event (e.g., fired from work), love event (e.g., got a divorce), health event (e.g., hospitalization for a life-threatening physical illness), crime/legal event (e.g., arrested), family/friends/household event (e.g., serious family argument), residence event (e.g., lost a residence through fire), death event (e.g., spouse/mate died), and childbirth related (e.g., found out that you could not have children). Consistent with previous research (e.g., Pagano et al., 2004), we established which events would be labeled as stressful (i.e., negative) a priori. For example, some items in each event category were unequivocally positive (e.g., “changed jobs for a better one”); these items were not used in these analyses as we did not predict they would precipitate worsening PD/PDA symptoms.
Statistical analysis
Interrupted time series analyses (Box, Jenkins, & Reinsel, 1994; McDowall, McCleary, Meidinger, & Hay, 1980) were used to determine if SLEs were associated with reliable changes in severity of PSR ratings, thereby evidencing their influence on panic symptom severity, within 12 weeks before and/or after the SLE. We chose to examine the 12 weeks prior to the event in addition to 12 weeks after the event because we hypothesized participants had some expectation that a SLE was going to occur. For instance, getting divorced does not simply occur “out of the blue;” instead, multiple events take place before a couple is legally divorced. We examined the effect of SLEs on the slope of panic symptom severity over time (i.e., a gradual/progressive effect occurring 12 weeks pre- and/or post-event) and to determine if SLEs had a specific intercept effect on panic symptom severity (i.e., an immediate/proximal effect during the week of the event).
Results
Descriptive analyses
At baseline, a majority of participants were Caucasian (98.1%; n=410), female (67.7%; n=283), married (53.4%; n=223), and unemployed (56.7%; n=237). The mean age was 40.3 (SD=12.0) years old. The most common current comorbid baseline diagnoses were Major Depressive Disorder (26.1%; n=109), GAD (21.3%; n=89), SP (17.5%; n=73), and Posttraumatic Stress Disorder (6.9%; n=29). Over the course of the years examined, 15.9% to 28.1% of participants received psychiatric treatment (medication and/or psychotherapy).
The mean number of SLEs experienced each year ranged from 0.65 (SD=0.86) in year 9 to 1.26 (SD=1.4) in year 15. Common SLEs included loss of job, hospitalization for physical illness, mate or spouse had a major change in health status, and financial situation worsened.
Primary Analyses
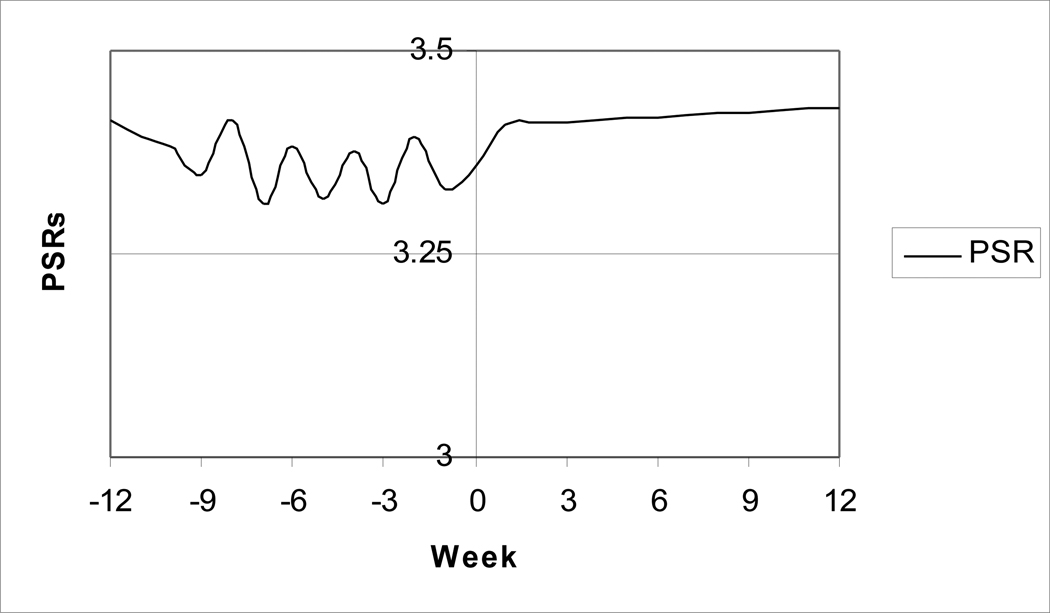
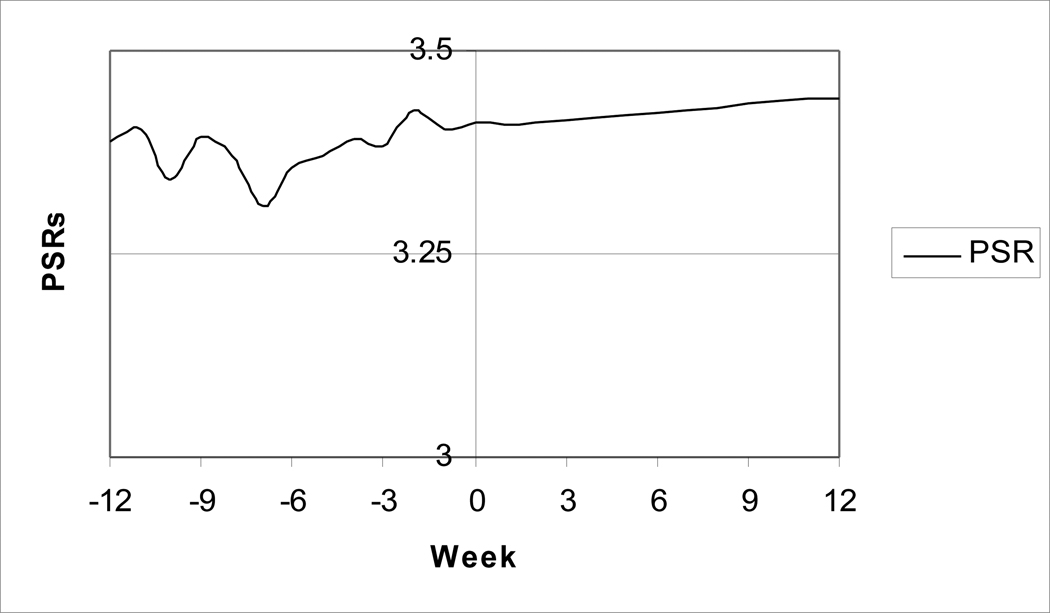
Results failed to show a significant pre-SLE effect or immediate SLE effect on PD/PDA panic symptom severity (ps>.05). Specifically, no significant change in panic symptom severity was observed during the course of the 12 weeks prior to the SLE or in the week in which the SLE occurred. However, results showed that when plotted as a function of the event (i.e., time-slope effect), both family/friends/household events and work events had residual effects on PD/PDA panic attack severity that occurred over the course of the 12 weeks after the event (tlin(5795)=10.8, p=.001; tlin(5499)=5.9, p=.015, respectively), meaning symptoms gradually worsened after the SLE (see Figures 1 and 2).
Figure 1.
Progressive impact of family/friend/household events (occurring at week 0) on panic symptom severity for adults with PD/PDA (n=418).
Note: PSR: Psychiatric Status Rating
Figure 2.
Progressive impact of work events (occurring at week 0) on panic symptom severity for adults with PD/PDA (n=418).
Note: PSR: Psychiatric Status Rating
Discussion
Results failed to show worsening PD/PDA panic symptoms in the 12 weeks leading up to an SLE or during the week in which the SLE occurred. However, results did show a residual effect caused by family/friend/household events and work events, meaning that within 12 weeks of these SLEs, participants’ panic symptoms had significantly worsened in severity. Examples of family/friend/household SLEs include: serious family argument, serious argument with close friend, stopped seeing a close family member; examples of work SLEs include: demoted at work, laid off, fired, changed jobs for a worse one. Results align with previous research that shows a relationship between threats to interpersonal relationships and financial stability and the onset of PD/PDA (Klauke et al., 2010) by showing that stresses associated with these events also put individuals at risk for worsened symptoms.
Results inform the temporal association between SLEs and worsened panic symptoms, but they do not necessarily confirm a causal relationship. A predominant biological theory of PD/PDA is that panic attacks develop due to individual differences in risk for hyperreactivity of the suffocation alarm system (Klein, 1993). These results might show that SLEs trigger an underlying biological diathesis. For instance, a serious family argument could lead to increased arousal of the autonomic nervous system, increasing risk for sensations of hyperventilation that ultimately lead to panic attacks. Alternatively, there might be an underlying mechanism that makes individuals with PD/PDA more likely to experience family/friendship- or work-related SLEs; for example, individuals with PD/PDA are more likely to be unable to work than individuals with other anxiety disorders (Moitra, Beard, Weisberg, & Keller, 2011), suggesting they experience significant occupational disruptions. These scenarios are not mutually exclusive; future research could inform this debate by comparing the likelihood of experiencing SLEs across anxiety disorders.
Strengths of the current study include the large sample size and the methodology that afforded us the ability to examine the temporal relationship of SLEs and worsening of symptoms week-to-week. However, the current study also had limitations. We used a sample of individuals who were seeking treatment at the time of recruitment, and may not generalize to the general population.
From a clinical standpoint, the study of SLEs has important implications for the primary prevention and treatment of anxiety disorders. The design of interventions for preventing or altering maladaptive stress and coping processes in adults begins with a basic knowledge of their differential response to stressors. Clinicians may then tailor risk assessments and treatments based on the individual’s vulnerability to the pernicious effects of SLEs.
Acknowledgements
HARP is supported by NIMH Grant 2R01MH051415-13A1.
Role of Funding Source
Funding for this study was provided by NIMH Grant 2R01MH051415-13A1; the NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this research were presented at the 44th annual convention of the Association for Behavioral and Cognitive Therapies (November 2010), San Francisco, CA.
Conflict of Interest
Disclosure for Andri S. Bjornsson, Ph.D., Honoraria: Dialogues in Clinical Neuroscience. Grants Research: None. Advisory Boards: None. Major Stockholder: None.
Disclosure for Risa B. Weisberg, Ph.D., Consultant Honoraria: Astra Zeneca, Eli Lilly and Company, Bristol Myers Squibb, and SciMed. Grants Research: Pfizer. Advisory Boards: None. Major Stockholder: None.
Disclosure for Martin B. Keller, MD., Consultant Honoraria: CENEREX, Forest Laboratories, Medtronic, Organon, Pfizer, Shire, Wyeth, Sierra Neuropharmaceuticals. Grants Research: Pfizer, Wyeth. Advisory Boards: CENEREX, Forest Laboratories, Organon. Major Stockholder: None.
All other authors declare that they have no conflicts of interest.
Contributors
Drs. Keller and Weisberg designed the study and wrote the protocol. Ms. Dyck and Drs. Moitra, Beard, Sibrava, and Bjornsson managed the literature searches and analyses. Ms. Dyck and Dr. Moitra undertook the statistical analysis. Dr. Moitra wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
References
- Box G, Jenkins GM, Reinsel G. Time Series Analysis: Forecasting & Control. 3rd ed. Upper Sadle River, NJ: Prentice Hall; 1994. [Google Scholar]
- Brown GW, Harris T. Social origins of depression: a reply. Psychol Med. 1978;8:577–588. doi: 10.1017/s0033291700018791. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. Life events and illness. New York: Guilford Press; 1989. [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia (SADS-L) Arch Gen Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Hollifield M, Katon W, Skipper B, Chapman T, Ballenger JC, Mannuzza S, Fyer AJ. Panic disorder and quality of life: variables predictive of functional impairment. Am J Psychiatry. 1997;154:766–772. doi: 10.1176/ajp.154.6.766. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, et al. Remission and relapse in subjects with panic disorder and panic with agoraphobia: A prospective short-interval naturalistic follow-up. J Nerv Ment Dis. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63:415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klauke B, Deckert J, Reif A, Pauli P, Domschke K. Life Events in Panic Disorder – An Update on “Candidate Stressors”. Depress Anxiety. 2010;27:716–730. doi: 10.1002/da.20667. [DOI] [PubMed] [Google Scholar]
- Klein DF. False suffocation alarms, spontaneous panics, and related conditions: an integrative hypothesis. Arch Gen Psychiatry. 1993;50:306–317. doi: 10.1001/archpsyc.1993.01820160076009. [DOI] [PubMed] [Google Scholar]
- Kouzis AC, Eaton WW. Psychopathology and the initiation of disability payments. Psychiatr Serv. 2000;51:908–913. doi: 10.1176/appi.ps.51.7.908. [DOI] [PubMed] [Google Scholar]
- McDowall D, McCleary R, Meidinger EE, Hay RA. Interrupted time series analysis. Quantitative applications in the social sciences volume 21. Thousand Oaks, CA: Sage; 1980. [Google Scholar]
- Moitra E, Beard C, Weisberg RB, Keller MB. Occupational impairment and Social Anxiety Disorder in a sample of primary care patients. J Affect Disord. 2011;130:209–212. doi: 10.1016/j.jad.2010.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, et al. Stressful life events as predictors of functioning: findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatr Scand. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rief W, Rief W, Martin A, Klaiberg A, Brähler E. Specific effects of depression, panic, and somatic symptoms on illness behavior. Psychosom Med. 2005;67:596–601. doi: 10.1097/01.psy.0000171158.59706.e7. [DOI] [PubMed] [Google Scholar]
- Smith TA, Oatley K. Validation of a brief life stress interview — The Short Life Events and Difficulties Schedule (SLEDS): a measure designed to assess severe life stress in major depression. Toronto, Canada: Poster presented at the annual Canadian Psychological Association Convention; 1997. Jun, [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R – Patient Version (SCID-P) New York: New York State Psychiatric Institute; 1988. [Google Scholar]
- Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, et al. Functional Impact and Health Utility of Anxiety Disorders in Primary Care Patients. Med Care. 2005;43:1164–1170. doi: 10.1097/01.mlr.0000185750.18119.fd. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]