Abstract
Background
Although constipation can be a chronic and severe problem, it is largely treated empirically. Evidence for the efficacy of some of the older laxatives from well-designed trials is limited. Patients often report high levels of dissatisfaction with their treatment, which is attributed to a lack of efficacy or unpleasant side-effects. Management guidelines and recommendations are limited and are not sufficiently current to include treatments that became available more recently, such as prokinetic agents in Europe.
Purpose
We present an overview of the pathophysiology, diagnosis, current management and available guidelines for the treatment of chronic constipation, and include recent data on the efficacy and potential clinical use of the more newly available therapeutic agents. Based on published algorithms and guidelines on the management of chronic constipation, secondary pathologies and causes are first excluded and then diet, lifestyle, and, if available, behavioral measures adopted. If these fail, bulk-forming, osmotic, and stimulant laxatives can be used. If symptoms are not satisfactorily resolved, a prokinetic agent such as prucalopride can be prescribed. Biofeedback is recommended as a treatment for chronic constipation in patients with disordered defecation. Surgery should only be considered once all other treatment options have been exhausted.
Keywords: algorithm, constipation, dissatisfaction, prokinetic, prucalopride
Introduction
Constipation is very common and many or most people are affected at some time in their life. However, for up to a quarter of the population it is more than a minor annoyance; for them, constipation can be chronic, sometimes severe, and has a significant, even debilitating, effect on their quality of life.1–3 Many patients suffer in silence and try to self-medicate, while for those who do seek medical help, treatments can be unsatisfactory.2,4 Nonetheless, in the authors’ experience, most patients can be helped with the right treatment approach. There are few detailed guidelines and recommendations available for the management of chronic constipation, and these do not always include more recently available treatments. Therefore, this article provides a summary of the condition from a European perspective, reviewing the pathophysiology, diagnosis and current management of constipation, including more recently available therapeutic agents.
It is estimated that constipation affects between 2% and 27% of the population, depending on the definition used,5,6 with 12% of people worldwide reporting self-defined constipation.7 However, the prevalence of constipation can be underestimated, as at least 65% of patients suffering from constipation do not seek immediate medical advice, but use over-the-counter (OTC) laxatives instead.2,5
Constipation may be severe and chronic; in a survey of over 10 000 individuals in the US, 14.7% met the criteria for constipation and 45% of these respondents reported having the condition for 5 years or more.6 Some experience weeks without a bowel movement and suffer from bloating, straining, defecation urge with an inability to evacuate, and painful evacuation.2,3 Daily activities and ability to work can be compromised, e.g., by discomfort, the need to be near a toilet, and by the length of time it takes to defecate. Measures of general health, social functioning, and mental health are significantly impaired compared with healthy individuals and levels are comparable with other conditions such as osteoarthritis, rheumatoid arthritis, chronic allergies and diabetes.1
In a web-based survey of approximately 4600 US respondents reporting one or more symptoms of constipation, only one in four reported seeking treatment from a doctor in the previous year.2 Those who do seek medical treatment are often not effectively treated, and only between one-quarter to two-thirds of patients with chronic constipation are satisfied with their laxative treatment.2,4 In a European survey of 744 patients with chronic constipation, almost half were using alternative treatments (homeopathy, massage and acupuncture) and one in three were not taking any medication.4 Nearly 90% of respondents expressed interest in new therapies.
Pathophysiology
Constipation may be primary (idiopathic) or secondary to other factors (Table 1).8
Table 1.
Causes of secondary constipation8
| Cause | Example |
|---|---|
| Organic | Colorectal cancer, extra-intestinal mass, postinflammatory, ischemic or surgical stenosis |
| Endocrine or metabolic | Diabetes mellitus, hypothyroidism, hypercalcemia, porphyria, chronic renal insufficiency, panhypopituitarism, pregnancy |
| Neurological | Spinal cord injury, Parkinson's disease, paraplegia, multiple sclerosis, autonomic neuropathy, Hirschsprung's disease, chronic intestinal pseudo-obstruction |
| Myogenic | Myotonic dystrophy, dermatomyositis, scleroderma, amyloidosis, chronic intestinal pseudo-obstruction |
| Anorectal | Anal fissure, anal strictures, inflammatory bowel disease, proctitis |
| Drugs | Opiates, antihypertensive agents, tricyclic antidepressants, iron preparations, anti-epileptic drugs, anti-Parkinsonian agents (anticholinergic or dopaminergic) |
| Diet or lifestyle | Low fiber diet, dehydration, inactive lifestyle |
Several sub-types of primary constipation are recognized, however, patients can display symptoms consistent with those from several sub-types. Constipation may be slow-transit (prolonged delay in passage of stool through the colon), or normal-transit. With slow and normal-transit times, there may be functional obstruction in the form of dysfunction of pelvic floor and anal sphincter muscles (anismus), leading to difficulty in expelling stools from the anorectum, or there can be no identifiable pathology with normal-transit constipation (Fig. 1).
Figure 1.
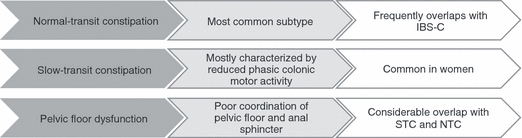
Types of constipation.Primary (idiopathic) constipation can be conceptually categorized into three main types: normal-transit, slow-transit and pelvic floor dysfunction. IBS-C, constipation predominant irritable bowel syndrome; STC, slow-transit constipation.8
Normal-transit constipation
Normal-transit constipation is probably the most common form of constipation seen by general clinicians, although this has not formally been studied.8,9 Stool traverses at a normal rate through the colon and stool frequency may be normal, but patients feel constipated.10 This group of patients report difficulty with evacuation, bloating, abdominal pain or discomfort and hard stools; however, reduced colonic transit cannot be confirmed.11 Constipation based on a patient's report of frequency of bowel movements may be underestimated without the use of a stool diary.10
On investigation, some patients in this group may have increased rectal compliance, reduced rectal sensation or both.12 A significant overlap exists between this subgroup of constipation and the irritable bowel syndrome (IBS) subgroup.
Slow-transit constipation
Approximately half of patients with symptoms refractory to supplementary fiber have a prolonged intestinal transit time.12 This group of patients has been found to have significant impairment of propulsive colonic motor activity,13 and significantly diminished colonic responses following a meal and on awakening in the morning;10 however, diurnal rhythm is usually preserved.14 In some patients, slow transit may be the result of an underlying defecation disorder, as colon transit times can become normalized following treatment (e.g., using biofeedback) for the underlying problem.15
The impaired motility in slow-transit constipation may be due to a number of factors. Propagating pressure waves in the colon, known as high amplitude propagated contractions (HAPCs), are strong contractions that begin at variable points in the colon and propagate towards the rectum. Several studies have shown that HAPCs are significantly decreased in constipated patients.14,16 A potential basis for these impairments are abnormalities of the myenteric plexus, characterized by a reduction in the number of argyrophilic neurons and axons, and an increase in the number of variably sized nuclei within ganglia.17 Interstitial cells of Cajal may also be important since their volume is significantly reduced in patients with slow-transit constipation.18 Interstitial cells of Cajal are required for generating the smooth muscle electrical slow wave, thus determining its contractile activity. In the absence of an electrical slow wave, contractile activity is reduced and irregular, resulting in decreased intestinal transit.18 Alternatively, the excitatory extrinsic nervous input to the bowel may be diminished, or extrinsic inhibitory activity to the bowel may be enhanced.
Acetylcholine is a neurotransmitter at neuro-neuronal and neuro-effector synaptic junctions within the enteric nervous system (ENS), and release of acetylcholine from enteric postsynaptic cholinergic neurons is the primary stimulant for spontaneous contractile activity of colonic smooth muscle.19 Compared with healthy subjects, constipated patients display an impaired colonic motor response to cholinergic stimulation in the descending colon.19 Serotonin [5-hydroxytryptamine (5-HT)], released from enterochromaffin cells in the gastrointestinal (GI) tract, stimulates neurons of the myenteric plexus to initiate peristaltic and secretory reflexes. While it is clear that 5-HT signaling is dysfunctional in intestinal motility disorders,20 it is not yet apparent whether this is underpinned by changes in the availability of 5-HT per se, or whether 5-HT re-uptake mechanisms, receptor density and/or function are diminished.21
It has been suggested, but not anatomically proven, that neuronal damage arising from neurodegeneration, or from damage during pelvic surgery or childbirth, reduces colonic motility and may underlie certain cases of idiopathic slow-transit constipation.22
Although the relationship between sex hormones and chronic constipation is not clear, a decreased level of ovarian and adrenal steroid hormones has been reported in association with constipation.23 Furthermore, one in vitro study proposed a mechanism for slow-transit constipation where the over-expression of progesterone receptors can down-regulate contractile G-proteins and up-regulate inhibitory G-proteins in colonic circular muscle cells.24
Defecation disorders
A number of patients with chronic constipation display a difficulty in expelling stools from the rectum. This failure may be due to impaired rectal contraction, paradoxical anal contraction, or inadequate anal relaxation.25 Lack of coordination, or dyssynergia, of the muscles involved in defecation is thought to be the most likely cause,26 but a high proportion of patients may also show impaired rectal sensation.25 Structural abnormalities are less common but include rectal prolapse and/or intussusceptions, rectocele (a herniation, usually of the anterior rectal wall towards the vagina), and excessive perineal descent. In many patients, pelvic floor dysfunction may contribute to constipation with or without delayed transit, and as a consequence, biofeedback therapy has been shown to be beneficial in recent controlled trials.27–29
Many constipated patients show reduced sensitivity to slow rectal distension, suggesting that there may be diminished sensory innervation to the rectum and sigmoid colon. In addition to a reduced urge to defecate, this may indicate an imbalance between sympathetic and parasympathetic influences in some constipated patients, associated with decreased propulsive motor activity and tone.12
Diagnosis of chronic constipation
The duration and characteristics of the patient's symptoms must be assessed to distinguish chronic from transient constipation. Transient constipation is easily recognized by history, indicating constipation started at a time of change in dietary habits, mobility or lifestyle. Secondary constipation, as a consequence of other factors (Table 1), should be identified and treated accordingly.
Diagnostic resources
Rome III criteria
The Rome III classification system is widely recognized as the only standardized symptom-based diagnostic criteria for functional GI disorders (FGIDs), including chronic constipation (Table 2).30 Other definitions of chronic constipation are consistent with the Rome III criteria but are less quantitative and more subjective.31,32 Although clinicians are aware of the Rome criteria, these are used principally for research purposes and are not widely applied in clinical practice, with the possible exception of IBS.33 However, the Rome Foundation diagnostic algorithm project has recently published a new set of clinical algorithms for FGIDs, including chronic constipation, which make active use of the Rome criteria for diagnostic and therapeutic management (discussed in section entitled Review of currently available guidelines, recommendations and algorithms).
Table 2.
Rome III criteria for chronic constipation30
| Criteria fulfilled for the last 3 months and symptom onset at least 6 months prior to diagnosis |
| Presence of ≥2 of the following symptoms: |
| • Lumpy or hard stools in ≥25% of defecations |
| • Straining during ≥25% of defecations |
| • Sensation of incomplete evacuation for ≥25% of defecations |
| • Sensation of anorectal obstruction/blockage for ≥25% of defecations |
| • Manual maneuvers to facilitate ≥25% of defecations (digital manipulations, pelvic floor support) |
| • <3 evacuations per week |
| Loose stools rarely present without the use of laxatives |
| Insufficient criteria for irritable bowel syndrome |
Bristol Stool Form Scale
The Bristol Stool Form Scale (BSFS) 34 is a useful visual aid that was designed to assist in the evaluation of patients with constipation. Using simple visual descriptors, it illustrates the common stool forms and consistency on a 7-point scale. It has been validated in a number of studies and has been found to be easily understood by patients, enabling them to recognize and thus classify the stool type that most closely represents their own experience. The form of the stool depends on the time that it spends in the colon; therefore, the BSFS is a quick and reliable indicator of transit time. It is particularly useful in patients with self-reported constipation who do not have infrequent bowel movements, to establish that hard or lumpy stools are, indeed, present.
Diagnostic evaluation
Routine extensive diagnostic and physiological testing is not recommended for chronic constipation.32,35 However, in those not responding to initial treatment, three main physiological tests can be used to assess anorectal disorders (e.g., dyssynergic defecation): anorectal manometry,25,26,36 the balloon expulsion test 36 and colon transit studies.36,37 If necessary, colonoscopy can be used to detect the presence of lesions such as rectal ulcers, inflammation or malignancy, and radiography of the abdomen can provide evidence for an excessive amount of stool in the colon. Barium enema plays a limited role today but can identify megacolon and megarectum. Anorectal manometry and histology of the nerve plexuses can be used to confirm Hirschsprung's disease.
As discussed earlier, constipation may arise secondary to a variety of factors (Table 1).8 Secondary causes of constipation are recognized by careful history taking and clinical examination, including a thorough rectal examination (e.g., the 10-step approach described by Talley).38 Colonoscopy is recommended in case of alarm symptoms and in those over 50 to screen for colorectal cancer.8,39 Alarm features suggestive of a serious GI disorder requiring further investigation include:40
Weight loss.
Blood in the stool.
Anemia.
Sudden change in bowel habit after the age of 50.
Significant abdominal pain.
Family history of colon cancer or inflammatory bowel disease.
Hence, routine diagnostic testing is generally not recommended for chronic constipation. However, if there is suspicion of metabolic causes, these can be investigated with a complete blood cell count, biochemical profile, serum calcium, glucose levels and thyroid function tests. If these give rise to suspicion, serum protein electrophoresis, urine porphyrins, serum parathyroid hormone and serum cortisol levels can be considered, but this will only rarely be indicated.10
Treatment options
Current treatment options
Current laxatives aid defecation by decreasing stool consistency (softening) and/or artificially or indirectly stimulating colon motility, via one or more of a number of mechanisms (Table 3).41,42
Table 3.
| Laxative type | Examples | Proposed mode of action | Potential limitations |
|---|---|---|---|
| Dietary fiber/bulking agents | Wheat bran Psyllium seed husk Methylcellulose | Luminal water binding increases stool bulk and reduces consistency | Flatulence and abdominal distension Stool impaction (rarely) Not recommended in frail, immobile, or palliative care patients |
| Osmotic laxatives | |||
| Undigestible disaccharides and sugar alcohols | Lactulose Sorbitol | Luminal water binding by creating an osmotic gradient | Bloating, flatulence |
| Synthetic macromolecules | PEG Polycarbophil | Luminal water binding | Bloating |
| Salinic laxatives | Magnesium hydroxide (e.g., milk of magnesia) Magnesium citrate Magnesium sulfate Sodium phosfate | Luminal water binding Increases fluid excretion | Electrolyte imbalance (must be used with caution in patients with compromised renal or cardiac function) |
| Stimulant laxatives | |||
| Diphenylmethane derivatives | Bisacodyl, sodium picosulfate | Act locally to stimulate colonic motility, decrease water absorption from large intestine | Abdominal discomfort and cramps |
| Anthraquinones | Senna, aloe, cascara | Act locally to stimulate colonic motility, decrease water absorption from large intestine | Abdominal discomfort and cramps |
Well-designed, placebo-controlled, blinded, clinical trials of older laxatives are sparse. Although many trials report improvements in the number of bowel movements per week and some report improvements of certain symptoms, many studies are small and lack comprehensive clinically relevant treatment endpoints. Similarly, there is a lack of head-to-head comparisons; hence, there is a lack of evidence to determine whether one laxative class is superior to another. It is also largely unknown if laxative treatments address the impaired quality of life observed in patients with chronic constipation, as most studies have failed to assess quality of life measures. Indeed, for some patients, laxatives can worsen certain symptoms, such as bloating and flatulence.43
Undigestible fibers attract water, which leads to a larger and softer fecal mass. Systematic reviews of older studies indicate that fiber increases the number of bowel movements, but the quality of these studies is inconsistent and the treatment duration was usually limited to 4 weeks or less.42 It has been shown that patients with slow transit and/or impaired defecation are unlikely to respond to fiber.44
Most comparative data suggest that lactulose and polyethylene glycol (PEG) have similar efficacy, but with lower incidence of vomiting and flatulence associated with the latter.45,46 PEG provides well-tolerated and effective relief in constipated patients.46,47 In a 6-month placebo-controlled study, 304 patients with chronic constipation received either 17 g PEG or placebo. Fifty-two percent of PEG-treated patients compared with 11% of placebo-treated patients (P< 0.001) were successfully relieved from constipation (according to modified Rome criteria) for more than 50% of their treatment weeks. No treatment-related safety differences were observed between the PEG and placebo groups during the study, with the exception of GI complaints (39.7% PEG-treated patients vs 25% placebo-treated patients; P= 0.015). This difference was observed due to abdominal distension, diarrhea, loose stools, flatulence and nausea, which are considered usual effects of laxative use.48 In addition, a retrospective study of institutional patients with chronic constipation reported good long-term results for up to 12 months,49 and for up to 5 months in a randomized prospective study in adult50 and pediatric constipated patients.51
Stimulant laxatives act via the lumen to alter electrolyte transport and increase intraluminal fluid secretion; when in contact with the mucosa they indirectly stimulate sensory nerve endings, thereby stimulating propulsion.41,42 Based on older literature, stimulant laxatives are more effective than placebo.52 A recent 4-week placebo-controlled trial with picosulfate 10 mg daily showed that this laxative was superior to placebo in increasing the number of (complete) spontaneous bowel movements, and in improving symptoms of straining and some aspects of quality of life. However, nearly 50% of the patients down-titrated the dose.53 Stimulant laxatives (especially bisacodyl) are traditionally used as rescue therapy in recent therapeutic trials in chronic constipation, suggesting that they are considered to have superior efficacy, although comparative trials with other agents are lacking.54,55 There is evidence that stimulant laxatives may cause abdominal pain.56 Early concerns of a possible link between chronic anthraquinone use, colonic inertia, and colon cancer have not been substantiated.37,57
In summary, a wide variety of laxatives are available, many of which are effective and well-tolerated in most constipated patients. However, they are not effective in all patients, and for some, the mode of action or dosage schedule is unacceptable and leads to patient dissatisfaction.2 In Table 4, we have summarized the available data on the use of dietary fiber, laxatives, and treatment of chronic constipation.40,55,58 Although the levels of evidence and grading of the recommendations varies between the meta-analyzes, in general:
Table 4.
Evidence-based review of treatments for constipation
| Recommendation | |||
|---|---|---|---|
| Agent/procedure | Ramkumar & Rao (2001)58 | ACG chronic constipation task Force (2005)55 | American Society of Colon and Rectal Surgeons (2007)40 |
| Dietary fiber/bulking agent | 1C | B (psyllium) | B (fiber/psyllium) |
| Osmotic laxatives | 1B | A (PEG and lactulose) | A (PEG) B (lactulose) |
| Diphenylmethanes†, anthraquinones | 2B | Insufficient evidence (Grade B) | C |
| Stool softeners | – | Insufficient evidence (Grade B) | C |
| Lubiprostone* | – | – | A |
| Biofeedback therapy‡ (selected cases) | 1B | Insufficient evidence (Grade C) | B |
| Surgery (severe colonic inertia) | 2B | – | B |
Grade A recommendations are supported by good evidence.
Grade B recommendations are supported by moderate evidence.
Grade C recommendations are only supported by poor evidence.
Grade 1 recommendations are supported by one or more randomized clinical trials.
Grade 2 recommendations are supported by one or more well-designed cohort or case-controlled studies.
Grade 3 recommendations are supported by expert opinion based on clinical experience.
Recent controlled studies have established the efficacy of biofeedback in the management of chronic constipation in those with defecatory disorders, but the efficacy seems less in those with slow-transit constipation.27–29 This establishes biofeedback as the treatment of choice for constipation with defecation disorders. However, recognizing and diagnosing defecatory disorders is beyond the scope of primary care practice, and is usually only done by gastroenterologists. Moreover, this therapy requires a patient who understands the concept and aim of the biofeedback process, and a skilled and motivated physiotherapist. Availability of experienced therapists and reimbursement of biofeedback is problematic in most parts of Europe.
New pharmacological treatments for constipation
Currently available treatments
Lubiprostone
Chloride channels play an important role in fluid transport and the maintenance of cell volume and pH in a variety of tissue and cell types, and in particular, in intestinal epithelial cells.59 Nine separate channels have been identified, of which the CIC-2 channel is of particular interest; when it is activated, the secretion of intestinal fluid is promoted.60 The secretion of fluids into the GI tract improves stool consistency and may contribute to normal transit.
Lubiprostone activates chloride channels to increase intestinal fluid secretion.61 However, its exact mechanism is unclear and may involve type-2 chloride channels, cystic fibrosis transmembrane conductance regulator chloride channels and/or G-protein-coupled prostaglandin receptors.62 It has been shown to significantly increase bowel movement frequency [5.89 spontaneous bowel movement (SBM)/week vs 3.99, P<0.0001] and relieve other constipation-related symptoms compared with placebo.61,63 It was approved by the FDA in 2006 for the treatment of chronic idiopathic constipation in adults, and subsequently for constipation-predominant IBS (IBS-C) in 2008, but, apart from Switzerland,64 it is not approved in Europe, as the Marketing Authorization Application was withdrawn in September 2009 as a result of a strategic decision by Sucampo Pharma Europe, Ltd.
5-HT4 agonists
As has already been discussed, serotonin is a critical component in the regulation of gut motility, visceral sensitivity, and intestinal secretion, acting via serotonin 5-HT4 receptors, which are expressed mainly by ENS interneurones. It is logical, therefore, to target 5-HT4 receptors in developing treatments for constipation. 5-HT4 receptor agonists stimulate 5-HT4 receptors on ENS interneurones to enhance the peristaltic reflex and have been shown to be effective in the treatment of chronic constipation.65 However, the poor selectivity of the early 5-HT4 receptor agonists, such as cisapride and tegaserod, has affected their risk : benefit profile and has ultimately restricted their clinical use. Cisapride, a member of the substituted benzamide family, is a partial 5-HT4 receptor agonist that was widely used for the treatment of gastro-esophageal reflux and dyspepsia before its withdrawal from the market in July 2000. It was associated with rare dose-dependent cardiac events, including lengthening of the QT interval, syncope, and ventricular arrhythmia in patients with predisposing conditions.66 This effect is now believed to be caused by its interaction with the cardiac hERG potassium channel.67 Tegaserod, an aminoguanidine indole, is a 5-HT4/5-HT1 receptor partial agonist, a 5-HT2 receptor antagonist, and has been shown to inhibit dopamine and noradrenaline transporters.68 It was previously approved in the USA (but not in Europe, apart from Switzerland), but was withdrawn in March 2009 because of a possible increased risk of cardiovascular adverse events (AEs) and is now only available for emergency use. Although the mechanisms underlying these adverse effects are not clear, they are unlikely to be related to 5-HT4 effects.69,70 More recently, a number of new 5-HT4 receptor agonists, with better selectivity profiles, have been developed.
Prucalopride
Prucalopride is highly selective for the 5-HT4 receptor, unlike cisapride, displaying at least 150-fold selectivity for its therapeutic target receptor.68,71 Early studies demonstrated that it decreased colonic transit time in normal and constipated subjects.72,73 Three large randomized Phase III controlled trials with a total of 1977 patients (1750 female and 227 male) with severe chronic constipation (defined as ≤2 SCBM/week for a minimum of 6 months with either very hard or hard stools, sensation of incomplete evacuation or straining during defecation for at least 25% of the time) confirmed that, averaged over 12 weeks, bowel function (measured as an increase of ≥1 SBM/week) was significantly improved in up to 69% of patients receiving the recommended dose of 2 mg prucalopride, with a median time of 2.5 h to first SBM.74–76 Transit studies showed that prucalopride was found to accelerate gastric emptying, small bowel transit, overall colon transit, and ascending colonic emptying in patients with functional constipation.73 Phase III trials have also confirmed that, in addition to improving bowel function, prucalopride significantly improves patient treatment satisfaction and quality of life, and alleviates a broad spectrum of constipation-related symptoms, including bloating, abdominal discomfort, and defecation urge with inability to evacuate.74–77 The most common adverse reactions (headache, nausea, diarrhea and abdominal pain) were mild and usually disappeared after the first day of treatment.78 Safety data from two randomized Phase I cross-over trials showed no clinically significant results from 24-h Holter monitoring. No difference was observed in the mean QT values corrected according to Fridericia's method (QTcF) when comparing prucalopride with placebo, and no QTcF values exceeded 500 ms or increased >60 ms during the treatment periods.79 These data indicate that there was no increased risk of drug-induced QT prolongation in this study.79 A randomized Phase II dose-escalating safety study conducted in 89 elderly patients aged ≥65 years old with constipation (87.7% of whom had a history of cardiovascular disease), also showed no clinically relevant differences in QT or QTcF time intervals between prucalopride and placebo, suggesting there is no specific cardiovascular safety concern in the elderly.80 Results from a long-term (24 months) open-label extension study show that treatment satisfaction is maintained with prolonged use; no safety signals were recorded in this study.81 Prucalopride has also been shown to be effective in the elderly 82 and patients with opioid-induced constipation.83
In October 2009, prucalopride received EU approval for the treatment of chronic constipation in women in whom laxatives fail to provide adequate relief, and now represents a new therapeutic option in the management of this condition. The therapeutic potential in hypomotile disorders of both the upper and lower GI tract, and the different pharmacological mode of action, might be the reason why the regulatory authorities have classified prucalopride in a separate class to laxatives (WHO ATC classification A03AE, drugs for functional bowel disorders – acting on serotonin receptors).
Experimental treatments
Opioid antagonists
Three mu-opioid antagonists (naloxone, methylnaltrexone and alvimopan) are currently under evaluation for the treatment of opiate-induced constipation 84,85 and postoperative ileus.86 Although endogenous opioids may play a role in modulating GI function,87 early reports suggested that opioid antagonists are not effective in idiopathic constipation.88
Linaclotide
Linaclotide is an agonist of guanylate cyclase-C receptors, which stimulates intestinal fluid secretion and transit. In early studies, it has been found to increase bowel movement frequency and loosen stool consistency.89 A recently published dose range-finding study and results from two Phase III trials in 1272 patients with chronic constipation, show that linaclotide significantly improved bowel function (measured as ≥3 complete SBMs (SCBM) per week, with an increase of ≥1 from baseline for ≥9 of 12 weeks) in up to approximately 20% of patients.90 The median time to first SBM was 21.9 h (150 μg).91 Furthermore, abdominal symptoms, global measures of constipation and quality of life were also significantly improved 91,92 and there was no evidence of rebound constipation upon treatment cessation.93 The most common AEs were GI-related, of which diarrhea had the highest incidence.91 Linaclotide is currently not licensed for use in the EU.
Other 5-HT4 agonists
Other enterokinetic agents in development include the 5-HT4 receptor agonists TD-5108 (Phase II),94 and ATI-7505 (Phase II).95 A number of other prokinetic 5-HT4 receptor agonists have been developed for GI disorders, which are of considerable therapeutic interest but are in the early stages of development.
Review of currently available guidelines, recommendations and algorithms
A number of groups have provided recommendations for the diagnosis and treatment of constipation;32,35,40,96,97 however, no standardized treatment guidelines have gained acceptance in general medical practice. Although the evidence for a number of interventions (including modifications to diet and lifestyle) is weak or contradictory, all the guidelines recommend that these be tried before pharmacological intervention. In general, where treatment pathways are recommended, the sequence is:
Exclude other pathologies and secondary causes.35,40,55,96,97
Begin treatment with dietary and lifestyle adjustments.35,40,55,96,97
Move to osmotic laxatives, stool softeners and bulk-forming agents – there is no consensus on the order in which these should be tried.35,96,97
Move to stimulant laxatives, suppositories and/or enemas96,97– some guidelines recommend medical supervision at this stage.97
Surgery should be used as a last resort or to treat identified disorders that require surgical correction.40,97
Although prokinetic agents feature in the two sets of US guidelines (Grade A recommendation),40,55 these are now out of date. Tegaserod has now been limited to emergency use in the US and has not received licensing approval in the EU. Prucalopride has recently received EU approval for the treatment of chronic constipation in women in whom laxatives fail to provide adequate relief; this is not mentioned in the guidelines.
Once organic disorders and obstructions have been excluded, a functional bowel disorder is the most likely explanation for the constipation. Most patients with chronic constipation report minimal abdominal bloating or discomfort associated with their other symptoms of chronic constipation; however, in some patients, as symptoms often overlap, it may be difficult to distinguish chronic constipation and IBS-C.55 The American College of Gastroenterology (ACG) Chronic Constipation Task Force defined IBS-C as clinically important abdominal discomfort associated with symptoms of constipation.61 National Institute for Clinical Excellence (NICE) guidelines for IBS indicate a positive diagnosis only if the person has abdominal pain/discomfort that is either relieved by defecation, or associated with altered bowel frequency or stool form, and at least two of the following: altered stool passage; abdominal bloating, distension, tension, or hardness, symptoms made worse by eating and passage of mucus.98
As previously mentioned, guidelines and algorithms for the management and treatment of chronic constipation have not taken into account more recent therapeutic developments. Although a new set of Rome Foundation diagnostic algorithms covering the diagnosis and management of FGIDs including chronic constipation35 and refractory constipation36 have been recently published, newer agents have not been included. According to these guidelines, patients with constipation that is refractory to a high-fiber diet and traditional laxatives should be referred for physiological testing, such as anorectal manometry, rectal balloon expulsion, and colon transit. Now, with the recent availability of prokinetic agents such as prucalopride, an additional therapeutic step can be added to these existing guidelines. Once idiopathic chronic constipation has been identified, and IBS and secondary constipation have been excluded, empirical treatment with osmotic and/or stimulant laxatives should be employed. Following this, if patients still experience continuous symptoms (e.g., bloating, abdominal discomfort and incomplete bowel movements), a prokinetic agent such as prucalopride could be considered (Fig. 2). If constipation symptoms are refractory to pharmacological treatment, patients should be referred for physiological testing as outlined in the published Rome algorithm for refractive constipation and difficult defecation (Fig. 3).36 Patients should only be referred for surgery following colon transit testing without, and then with, laxatives.
Figure 2.
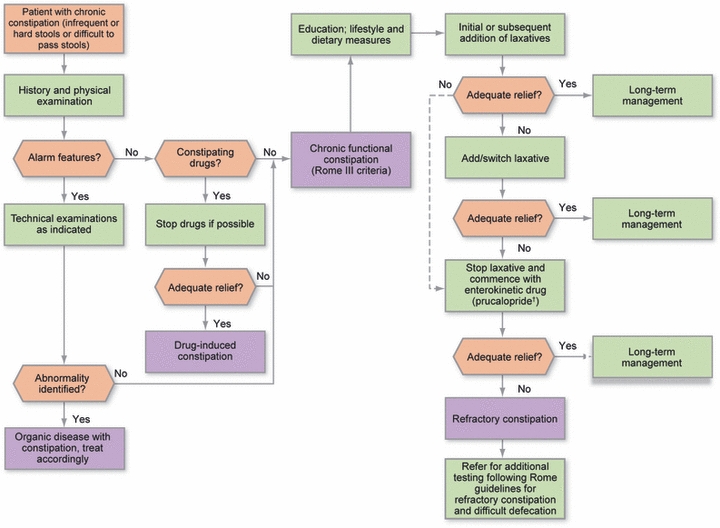
Enterokinetic treatment algorithm. Once idiopathic chronic constipation has been identified (Rome III); and education, lifestyle and dietary measures; and treatment with laxatives (response evaluable after 2–4 weeks) have failed to provide adequate relief, an enterokinetic agent can be commenced (response to prucalopride evaluable after 4–12 weeks). If constipation symptoms are still refractory to pharmacological treatment, patients should be referred for physiological testing as outlined in the published Rome algorithm for refractive constipation and difficult defecation. †2 or 1 mg day−1 if the patient is >65 years.
Figure 3.
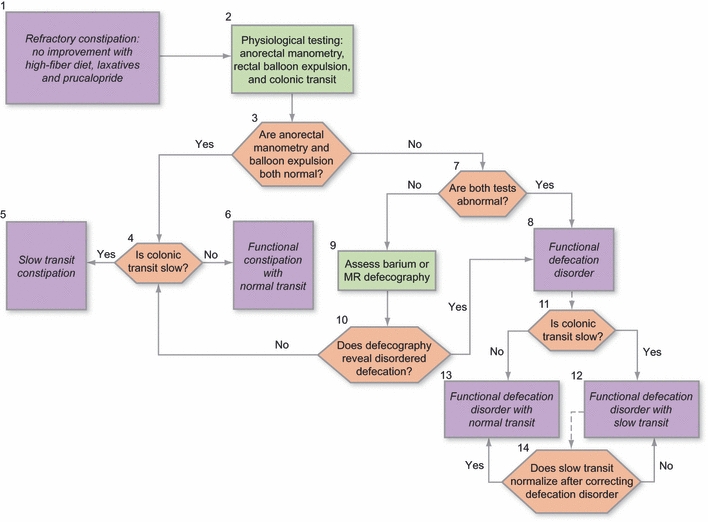
Refractory constipation and difficult defecation. (1) Patients who fulfill the criteria for functional constipation and those who have not improved with an increase in dietary fiber and the use of simple laxatives, and with no alarm features, often warrant further physiological assessment. (2) The three key physiological investigations are anorectal manometry, the balloon expulsion test, and a colonic transit study. (3, 4) If both anorectal manometry and balloon expulsion are normal, the results of colonic transit testing enable characterization of the disorder as functional constipation with slow (5) or normal transit (6). (7, 8) If both manometry and the rectal balloon expulsion test are abnormal, this is sufficient to diagnose a functional defecation disorder. (9) If only one of the anorectal manometry and balloon expulsion is abnormal, further testing using barium or magnetic resonance defecography may be used to confirm or exclude the diagnosis. (10) If defecography reveals features of disordered defecation, a diagnosis of a functional defecation disorder can be made. (8) If defecography is not abnormal, then the patient does not fulfill criteria for the diagnosis of a functional defecation disorder; further diagnosis then depends on the presence or absence of colonic transit delay (see above 4–6). (11–13) Treatment of choice for disordered defecation is biofeedback. If there is no adequate response to therapy, further investigation may be considered at this point. The presence of a functional defecation disorder does not exclude the diagnosis of slow colonic transit. Thus, depending on the results of the colonic transit study, the patient can be characterized as suffering from a functional defecation disorder with slow (12) or normal colonic transit. (13, 14) Slow colonic transit may result from a defecation disorder. If it is felt appropriate to distinguish between the two possibilities, the colonic transit evaluation may be repeated after correction of the defecation disorder. If transit normalizes, the presumption is that the delay was secondary to the defecation disorder; if not, the delayed colonic transit is presumed to be a comorbid condition, which may require therapy if there is no clinical improvement with the treatment of functional defecation disorder. This figure has been adapted by permission from Macmillan Publishers Ltd: The American Journal of Gastroenterology,36 copyright (2010).
Conclusions
Constipation is common and for some it can be chronic, where symptoms can be severe and can significantly affect a patient's quality of life. Although many laxative treatments are available, either OTC or by prescription, patients may often need additional treatment to achieve optimal symptom relief. As evidence for the effectiveness for many of the older laxatives is limited and there are relatively few guidelines on the management of this condition, treatment is often empirically-based. If diet, lifestyle measures, and traditional laxative therapies fail to provide adequate relief, the use of a motility agent offers a novel mechanism of action with therapeutic benefit. The 5-HT4 agonist prucalopride, approved in the EU, increases colonic motility and is a valuable clinical option for the patient who is dissatisfied or incompletely treated by laxatives.
Acknowledgments
JT, SML, VS, GB, MK, MS, JPG, and MF significantly contributed to the concept of the paper, discussion and design of the algorithm, and writing and review of the paper. Medical writing support in the development of this article was provided by Jude Douglass and Victoria Harvey, and was funded by Movetis.
Disclosures
Jan Tack is an advisor for Addex Pharma, AGI Therapeutics, Almirall, Aryx, AstraZeneca, Danone, Ipsen, Menarini, Movetis, Norgine, Novartis, Nycomed, Ocera, Rose Pharma, SK Life Sciences, Smartpill, Sucampo, Theravance, Tranzyme, Xenoport, and Zeria.
Stefan Müller-Lissner is an advisor for ARYx Therapeutics, AstraZeneca, Axcan, Boehringer Ingelheim, Movetis, and Mundipharma.
Vincenzo Stanghellini is an advisor for Axcan, Movetis, Norgine, Nycomed, and Pfizer.
Guy Boeckxstaens is an advisor for AstraZeneca, GSK, Movetis, and Xenoport. No financial interests.
Michael A Kamm is an advisor for Boehringer Ingelheim and Movetis.
Magnus Simren is an advisor for AstraZeneca, Albireo, Boehringer Ingelheim, Danone, Movetis and Novartis.
Jean-Paul Galmiche has served as a speaker, a consultant and an advisory board member for Addex Pharma SA, Xenoport, Movetis, Norgine, AstraZeneca, Janssen-Cilag, Renckitt Benckiser, Given Imaging and Mauna Kea Technologies, and has received research funding from AstraZeneca, Mauna Kea Technologies, Given Imaging, and Janssen-Cilag.
Michael Fried is an advisor for Movetis, Novartis, Nycomed, and AstraZeneca.
References
- 1.Belsey J, Greenfield S, Candy D, Geraint M. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31:938–49. doi: 10.1111/j.1365-2036.2010.04273.x. [DOI] [PubMed] [Google Scholar]
- 2.Johanson J, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther. 2007;25:599–608. doi: 10.1111/j.1365-2036.2006.03238.x. [DOI] [PubMed] [Google Scholar]
- 3.Wald A, Scarpignato C, Kamm MA, et al. The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther. 2007;26:227–36. doi: 10.1111/j.1365-2036.2007.03376.x. [DOI] [PubMed] [Google Scholar]
- 4.Tack J, Mueller-Lissner S, Dubois D, Schenck F. Only 27% of European patients with chronic constipation are satisfied with current treatment options. UEGW/WCOG: Gut. 2009;58(Suppl. II) [Google Scholar]
- 5.Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L. An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol. 2001;96:3130–7. doi: 10.1111/j.1572-0241.2001.05259.x. [DOI] [PubMed] [Google Scholar]
- 6.Stewart WF, Liberman JN, Sandler RS, et al. Epidemiology of constipation (EPOC) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol. 1999;94:3530–40. doi: 10.1111/j.1572-0241.1999.01642.x. [DOI] [PubMed] [Google Scholar]
- 7.Wald A, Scarpignato C, Mueller-Lissner S, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther. 2008;28:917–30. doi: 10.1111/j.1365-2036.2008.03806.x. [DOI] [PubMed] [Google Scholar]
- 8.Eoff JC. Optimal treatment of chronic constipation in managed care: review and roundtable discussion. J Manag Care Pharm. 2008;14:1–15. doi: 10.18553/jmcp.2008.14.S8-A.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mertz H, Naliboff B, Mayer E. Physiology of refractory chronic constipation. Am J Gastroenterol. 1999;94:609–15. doi: 10.1111/j.1572-0241.1999.922_a.x. [DOI] [PubMed] [Google Scholar]
- 10.Rao SSC. Constipation: evaluation and treatment. Gastroenterol Clin North Am. 2003;32:659–83. doi: 10.1016/s0889-8553(03)00026-8. [DOI] [PubMed] [Google Scholar]
- 11.Ashraf W, Park F, Lof J, Quigley EM. An examination of the reliability of reported stool frequency in the diagnosis of idiopathic constipation. Am J Gastroenterol. 1996;91:26–32. [PubMed] [Google Scholar]
- 12.Mertz H, Naliboff B, Mayer E. Physiology of refractory chronic constipation. Am J Gastroenterol. 1999;94:609–15. doi: 10.1111/j.1572-0241.1999.922_a.x. [DOI] [PubMed] [Google Scholar]
- 13.Bassotti G, Imbimbo BP, Betti C, Dozzini G, Morelli A. Impaired colonic motor response to eating in patients with slow-transit constipation. Am J Gastroenterol. 1992;87:504–8. [PubMed] [Google Scholar]
- 14.Bassotti G, Gaburri M, Imbimbo BP, et al. Colonic mass movements in idiopathic chronic constipation. Gut. 1988;29:1173–9. doi: 10.1136/gut.29.9.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emmanuel AV, Kamm MA. Response to a behavioral treatment, biofeedback, in constipated patients is associated with improved gut transit and autonomic innervation. Gut. 2001;49:214–9. doi: 10.1136/gut.49.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bazzocchi G, Ellis J, Villanueva-Meyer J, et al. Postprandial colonic transit and motor activity in chronic constipation. Gastroenterology. 1990;98:686–93. doi: 10.1016/0016-5085(90)90289-d. [DOI] [PubMed] [Google Scholar]
- 17.Krishnamurthy S, Schuffler MD, Rohrmann CA, Pope CE., 2nd Severe idiopathic constipation is associated with a distinctive abnormality of the colonic myenteric plexus. Gastroenterology. 1985;88:26–34. doi: 10.1016/s0016-5085(85)80128-1. [DOI] [PubMed] [Google Scholar]
- 18.He CL, Burgart L, Wang L, et al. Decreased interstitial cell of cajal volume in patients with slow-transit constipation. Gastroenterology. 2000;118:14–21. doi: 10.1016/s0016-5085(00)70409-4. [DOI] [PubMed] [Google Scholar]
- 19.Bassotti G, Chiarioni G, Imbimbo BP, et al. Impaired colonic motor response to cholinergic stimulation in patients with severe chronic idiopathic (slow transit type) constipation. Dig Dis Sci. 1993;38:1040–5. doi: 10.1007/BF01295719. [DOI] [PubMed] [Google Scholar]
- 20.Atkinson W, Lockhart S, Whorwell PJ, Keevil B, Houghton LA. Altered 5-hydroxytryptamine signaling in patients with constipation- and diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2006;130:34–43. doi: 10.1053/j.gastro.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 21.Costedio MM, Coates MD, Brooks EM, et al. Mucosal serotonin signaling is altered in chronic constipation but not in opiate-induced constipation. Am J Gastroenterol. 2010;105:1173–80. doi: 10.1038/ajg.2009.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knowles CH, Scott SM, Lunniss PJ. Slow transit constipation: a disorder of pelvic autonomic nerves? Dig Dis Sci. 2001;46:389–401. doi: 10.1023/a:1005665218647. [DOI] [PubMed] [Google Scholar]
- 23.Kamm MA, Farthing MJG, Lennard-Jones JE, Perry L, Chard T. Steroid hormone abnormalities in women with severe idiopathic constipation. Gut. 1991;32:80–4. doi: 10.1136/gut.32.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiao ZL, Pricolo V, Biancani P, Behar J. Role of progesterone signaling in the regulation of G-protein levels in female chronic constipation. Gastroenterology. 2005;128:667–75. doi: 10.1053/j.gastro.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol. 1998;93:1042–50. doi: 10.1111/j.1572-0241.1998.00326.x. [DOI] [PubMed] [Google Scholar]
- 26.Rao SSC. Dyssynergic defecation. Gastroenterol Clin North Am. 2001;31:97–114. doi: 10.1016/s0889-8553(05)70169-2. [DOI] [PubMed] [Google Scholar]
- 27.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–64. doi: 10.1053/j.gastro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Rao SS, Seaton K, Miller M, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007;5:331–8. doi: 10.1016/j.cgh.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 29.Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007;50:428–41. doi: 10.1007/s10350-006-0814-9. [DOI] [PubMed] [Google Scholar]
- 30.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 31.Locke G, III, Pemberton J, Phillips S. American Gastroenterological Association Medical Position Statement: guidelines on constipation. Gastroenterology. 2000;119:1761–6. doi: 10.1053/gast.2000.20390. [DOI] [PubMed] [Google Scholar]
- 32.American College of Gastroenterology Chronic Constipation Task Force. An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100:S1–4. doi: 10.1111/j.1572-0241.2005.50613_1.x. [DOI] [PubMed] [Google Scholar]
- 33.Kellow JE. Introduction: a practical evidence-based approach to the diagnosis of the functional gastrointestinal disorders. Am J Gastroenterol. 2010;105:743–6. doi: 10.1038/ajg.2010.64. [DOI] [PubMed] [Google Scholar]
- 34.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastoenterol. 1997;32:920–4. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 35.Spiller RC, Thompson WG. Bowel disorders. Am J Gastroenterol. 2010;105:775–85. doi: 10.1038/ajg.2010.69. [DOI] [PubMed] [Google Scholar]
- 36.Bharucha AE, Wald AM. Anorectal disorders. Am J Gastroenterol. 2010;105:786–94. doi: 10.1038/ajg.2010.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muller-Lissner S. The pathophysiology, diagnosis and treatment of constipation. Dtsch Arztebl Int. 2009;106:424–31. doi: 10.3238/arztebl.2009.0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Talley NJ. How to do and interpret a rectal examination in gastroenterology. Am J Gastroenterol. 2008;103:820–2. doi: 10.1111/j.1572-0241.2008.01832.x. [DOI] [PubMed] [Google Scholar]
- 39.Rao SS. Constipation: evaluation and treatment. Gastroenterol Clin North Am. 2003;32:659–83. doi: 10.1016/s0889-8553(03)00026-8. [DOI] [PubMed] [Google Scholar]
- 40.Ternent CA, Bastawrous AL, Morin NA, Ellis CN, Hyman NH, Buie WD. Practice parameters for the evaluation and management of constipation. Dis Colon Rectum. 2007;50:2013–22. doi: 10.1007/s10350-007-9000-y. [DOI] [PubMed] [Google Scholar]
- 41.Johnson D. Treating chronic constipation: how should we interpret the recommendations? Clin Drug Investig. 2006;26:547–57. doi: 10.2165/00044011-200626100-00001. [DOI] [PubMed] [Google Scholar]
- 42.Tack J, Muller-Lissner S. Treatment of chronic constipation: current pharmacologic approaches and future directions. Clin Gastroenterol Hepatol. 2009;7:502–8. doi: 10.1016/j.cgh.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 43.Jones M, Talley N, Nuyts G, Dubois D. Lack of objective evidence of efficacy of laxatives in chronic constipation. Dig Dis Sci. 2002;47:2222–30. doi: 10.1023/a:1020131126397. [DOI] [PubMed] [Google Scholar]
- 44.Voderholzer WA, Schatke W, Muhldorfer BE, Klauser AG, Birkner B, Muller-Lissner SA. Clinical response to dietary fiber treatment of chronic constipation. Am J Gastroenterol. 1997;92:95–8. [PubMed] [Google Scholar]
- 45.Petticrew M, Rodgers M, Booth A. Effectiveness of laxatives in adults. Qual Health Care. 2001;10:268–73. doi: 10.1136/qhc.0100268... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dupont C, Leluyer B, Maamri N, et al. Double-blind randomized evaluation of clinical and biological tolerance of polyethylene glycol 4000 versus lactulose in constipated children. J Pediatr Gastroenterol Nutr. 2005;41:625–33. doi: 10.1097/01.mpg.0000181188.01887.78. [DOI] [PubMed] [Google Scholar]
- 47.Di Palma JS, Cleveland MV, McGowan J, Herrera JL. A randomized, multicenter comparison of polyethylene glycol laxative and tegaserod in treatment of patients with chronic constipation. Am J Gastroenterol. 2007;102:1964–71. doi: 10.1111/j.1572-0241.2007.01365.x. [DOI] [PubMed] [Google Scholar]
- 48.Dipalma JA, Cleveland MV, McGowan J, Herrera JL. A randomized, multicenter, placebo-controlled trial of polyethylene glycol laxative for chronic treatment of chronic constipation. Am J Gastroenterol. 2007;102:1436–41. doi: 10.1111/j.1572-0241.2007.01199.x. [DOI] [PubMed] [Google Scholar]
- 49.Migeon-Duballet I, Chabin M, Gautier A, et al. Long-term efficacy and cost-effectiveness of polyethylene glycol 3350 plus electrolytes in chronic constipation: a retrospective study in a disabled population. Curr Med Res Opin. 2006;22:1227–35. doi: 10.1185/030079906X112543. [DOI] [PubMed] [Google Scholar]
- 50.Corazziari E, Badiali D, Bazzocchi G, et al. Long term efficacy, safety and tolerability of low daily doses of isosmotic polyethylene glycol electrolyte balanced solution (PMF-100) in the treatment of functional chronic constipation. Gut. 2000;46:522–6. doi: 10.1136/gut.46.4.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loening-Baucke V, Pashankar D. A randomized, prospective, comparison study of polyethylene glycol 3350 without electrolytes and milk of magnesia for children with constipation and fecal incontinence. Pediatrics. 2006;118:528–35. doi: 10.1542/peds.2006-0220. [DOI] [PubMed] [Google Scholar]
- 52.Bosshard W, Dreher R, Schnegg J, Bula C. The treatment of chronic constipation in elderly people: an update. Drugs Aging. 2004;21:911–30. doi: 10.2165/00002512-200421140-00002. [DOI] [PubMed] [Google Scholar]
- 53.Mueller-Lissner S, Kamm MA, Wald A, et al. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of sodium picosulfate in patients with chronic constipation. Am J Gastroenterol. 2010;105:897–903. doi: 10.1038/ajg.2010.41. [DOI] [PubMed] [Google Scholar]
- 54.Ramkumar D, Rao SS. Efficacy and safety of traditional medical therapies for chronic constipation: systematic review. Am J Gastroenterol. 2005;100:936–71. doi: 10.1111/j.1572-0241.2005.40925.x. [DOI] [PubMed] [Google Scholar]
- 55.Brandt LJ, Prather CM, Quigley EM, Schiller LR, Schoenfeld P, Talley NJ. Systematic review on the management of chronic constipation in North America. Am J Gastroenterol. 2005;100:S5–22. doi: 10.1111/j.1572-0241.2005.50613_2.x. [DOI] [PubMed] [Google Scholar]
- 56.Bengtsson M, Ohlsson B. Psychological well-being and symptoms in women with chronic constipation treated with sodium picosulphate. Gastroenterol Nurs. 2005;28:3–12. doi: 10.1097/00001610-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Morales MA, Hernandez D, Bustamante S, Bachiller I, Rojas A. Is senna laxative use associated to cathartic colon, genotoxicity, or carcinogenicity? J Toxicol. 2009;2009 doi: 10.1155/2009/287247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramkumar DP, Rao SSC. Functional anorectal disorders. In: Irvine EJ, Hunt RH, editors. Evidence-Based Gastroenterology. London: B C Decker; 2001. pp. 207–22. [Google Scholar]
- 59.Jentsch TJ. CLC chloride channels and transporters: from genes to protein structure, pathology and physiology. Crit Rev Biochem Mol Biol. 2008;43:3–36. doi: 10.1080/10409230701829110. [DOI] [PubMed] [Google Scholar]
- 60.Cuppoletti J, Malinowska DH, Tewari KP, et al. SPI-0211 activates T84 cell chloride transport and recombinant human ClC-2 chloride currents. Am J Physiol Cell Physiol. 2004;287:C1173–83. doi: 10.1152/ajpcell.00528.2003. [DOI] [PubMed] [Google Scholar]
- 61.Lacy BE, Levy LC. Lubiprostone: a novel treatment for chronic constipation. Clin Interv Aging. 2008;3:357–64. doi: 10.2147/cia.s2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wood JD. Enteric nervous system: sensory physiology, diarrhea and constipation. Curr Opin Gastroenterol. 2010;26:102–8. doi: 10.1097/MOG.0b013e328334df4f. [DOI] [PubMed] [Google Scholar]
- 63.Barish CF, Drossman D, Johanson JF, Ueno R. Efficacy and safety of lubiprostone in patients with chronic constipation. Dig Dis Sci. 2010;55:1090–7. doi: 10.1007/s10620-009-1068-x. [DOI] [PubMed] [Google Scholar]
- 64.Sucampo Pharma Europe Ltd. Sucampo receives marketing authorization for Amitiza® in Switzerland for treatment of chronic idiopathic constipation. 2009. Available at: http://www.sucampo.com (accessed on 7 June 2010)
- 65.Tonini M, Pace F. Drugs acting on serotonin receptors for the treatment of functional GI disorders. Dig Dis. 2006;24:59–69. doi: 10.1159/000090309. [DOI] [PubMed] [Google Scholar]
- 66.Tonini M, de Ponti F, Di Nucci A, Crema F. Review article: cardiac adverse effects of gastrointestinal prokinetics. Aliment Pharmacol Ther. 1999;13:1585–91. doi: 10.1046/j.1365-2036.1999.00655.x. [DOI] [PubMed] [Google Scholar]
- 67.Mohammad S, Zhou Z, Gong Q, January CT. Blockage of the HERG human cardiac K+ channel by the gastrointestinal prokinetic agent cisapride. Am J Physiol. 1997;273:H2534–8. doi: 10.1152/ajpheart.1997.273.5.H2534. [DOI] [PubMed] [Google Scholar]
- 68.de Maeyer J, Lefebvre R, Schuurkes J. 5-HT4 receptor agonists: similar but not the same. Neurogastroenterol Motil. 2008;20:99–112. doi: 10.1111/j.1365-2982.2007.01059.x. [DOI] [PubMed] [Google Scholar]
- 69.Busti AJ, Murillo JR, Jr, Cryer B. Tegaserod-induced myocardial infarction: case report and hypothesis. Pharmacotherapy. 2004;24:526–31. doi: 10.1592/phco.24.5.526.33351. [DOI] [PubMed] [Google Scholar]
- 70.Chan KY, de Vries R, Leijten FP, et al. Functional characterization of contractions to tegaserod in human isolated proximal and distal coronary arteries. Eur J Pharmacol. 2009;619:61–7. doi: 10.1016/j.ejphar.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 71.Briejer MR, Bosmans JP, Van Daele P, et al. The in vitro pharmacological profile of prucalopride, a novel enterokinetic compound. Eur J Pharmacol. 2001;423:71–83. doi: 10.1016/s0014-2999(01)01087-1. [DOI] [PubMed] [Google Scholar]
- 72.Bouras EP, Camilleri M, Burton DD, McKinzie S. Selective stimulation of colonic transit by the benzofuran 5HT4 agonist, prucalopride, in healthy humans. Gut. 1999;44:682–6. doi: 10.1136/gut.44.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bouras EP, Camilleri M, Burton DD, Thomforde G, McKinzie S, Zinsmeister AR. Prucalopride accelerates gastrointestinal and colonic transit in patients with constipation without a rectal evacuation disorder. Gastroenterology. 2001;120:354–60. doi: 10.1053/gast.2001.21166. [DOI] [PubMed] [Google Scholar]
- 74.Camilleri M, Kerstens R, Rykx A, Vandeplassche L. A placebo-controlled trial of prucalopride for severe chronic constipation. N Engl J Med. 2008;358:2344–54. doi: 10.1056/NEJMoa0800670. [DOI] [PubMed] [Google Scholar]
- 75.Quigley EM, Vandeplassche L, Kerstens R, Ausma J. Clinical trial: the efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation – a 12-week, randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2009;29:315–28. doi: 10.1111/j.1365-2036.2008.03884.x. [DOI] [PubMed] [Google Scholar]
- 76.Tack J, van Outryve M, Beyens G, Kerstens R, Vandeplassche L. Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Gut. 2009;58:357–65. doi: 10.1136/gut.2008.162404. [DOI] [PubMed] [Google Scholar]
- 77.Dubois D, Gilet H, Viala-Danten M, Tack J. Psychometric performance and clinical meaningfulness of the patient assessment of constipation – quality of life (PAC-QOL) questionnaire in prucalopride (RESOLOR) trials for chronic constipation. Neurogastroenterol Motil. 2009;22:e54–63. doi: 10.1111/j.1365-2982.2009.01408.x. [DOI] [PubMed] [Google Scholar]
- 78.Tack J, Ausma J, Kerstens R, Vanderplassche L. Safety and tolerability of prucalopride (Resolar) in patients with chronic constipation: pooled data from three pivotal phase III studies. Gastroenterology. 2008;134:A–530. [Google Scholar]
- 79.Boyce M, Kerstens R, Beyens G, Ausma J, Vandeplassche L. Cardiovascular safety of prucalopride in healthy subjects: results from two randomized, double-blind, placebo-controlled, cross-over trials. Gastroenterology. 2009;136(Suppl. 1):T1265. [Google Scholar]
- 80.Camilleri M, Beyens G, Kerstens R, Robinson P, Vandeplassche L. Safety assessment of prucalopride in elderly patients with constipation: a double-blind, placebo-controlled study. Neurogastroenterol Motil. 2009;21:1256–e117. doi: 10.1111/j.1365-2982.2009.01398.x. [DOI] [PubMed] [Google Scholar]
- 81.Camilleri M, Van Outryve MJ, Beyens G, Kerstens R, Robinson P, Vandeplassche L. Clinical trial: the efficacy of open-label prucalopride treatment in patients with chronic constipation – follow-up of patients from the pivotal studies. Aliment Pharmacol Ther. 2010;32:1113–23. doi: 10.1111/j.1365-2036.2010.04455.x. [DOI] [PubMed] [Google Scholar]
- 82.Mueller-Lissner S, Rykx A, Kerstens R, Vandeplassche L. A double-blind, placebo-controlled study of prucalopride in elderly patients with chronic constipation. Neurogastroenterol Motil. 2010;22:991–8. doi: 10.1111/j.1365-2982.2010.01533.x. [DOI] [PubMed] [Google Scholar]
- 83.Sloots CE, Rykx A, Cools M, Kerstens R, De Pauw M. Efficacy and safety of prucalopride in patients with chronic non-cancer pain suffering from opioid-induced constipation. Dig Dis Sci. 2010;55:2912–21. doi: 10.1007/s10620-010-1229-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Holzer P. Opioid antagonists for prevention and treatment of opioid-induced gastrointestinal effects. Curr Opin Anaesthesiol. 2010;23:616–22. doi: 10.1097/ACO.0b013e32833c3473. [DOI] [PubMed] [Google Scholar]
- 85.Meissner W, Leyendecker P, Mueller-Lissner S, et al. A randomised controlled trial with prolonged-release oral oxycodone and naloxone to prevent and reverse opioid-induced constipation. Eur J Pain. 2009;13:56–64. doi: 10.1016/j.ejpain.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 86.Tan EK, Cornish J, Darzi AW, Tekkis PP. Meta-analysis: alvimopan vs placebo in the treatment of postoperative ileus. Aliment Pharmacol Ther. 2007;25:47–57. doi: 10.1111/j.1365-2036.2006.03150.x. [DOI] [PubMed] [Google Scholar]
- 87.Greenwood-Van Meerveld B, Gardner CJ, Little PJ, Hicks GA, Dehaven-Hudkins DL. Preclinical studies of opioids and opioid antagonists on gastrointestinal function. Neurogastroenterol Motil. 2004;16(Suppl. 2):46–53. doi: 10.1111/j.1743-3150.2004.00555.x. [DOI] [PubMed] [Google Scholar]
- 88.Kelleher D, Johanson J, Pobiner B, Carter E, Dukes G. Alvimopan, a peripherally acting mu-opioid receptor (PAM-OR) antagonist- a study in patients with chronic idiopathic constipation (CIC) not taking opioid medications. Am J Gastroenterol. 2006;101 [Abstract 1239] [Google Scholar]
- 89.Johnston JM, Kurtz CB, Drossman DA, et al. Pilot study on the effects of linaclotide in patients with chronic constipation. Am J Gastroenterol. 2009;104:125–32. doi: 10.1038/ajg.2008.59. [DOI] [PubMed] [Google Scholar]
- 90.Lembo AJ, Schneier H, Lavins BJ, et al. Efficacy and safety of once daily linaclotide administered orally for 12 weeks in patients with chronic constipation: results from two randomized, double-blind, placebo-controlled phase 3 trials. Presented at DDW, May 1–5 2010. Abstract [286]
- 91.Lembo AJ, Kurtz CB, Macdougall JE, et al. Efficacy of linaclotide for patients with chronic constipation. Gastroenterology. 2010;138:886–95. doi: 10.1053/j.gastro.2009.12.050. e1. [DOI] [PubMed] [Google Scholar]
- 92.Carson RT, Tourkodimitris S, Macdougall JE, et al. Effect of linaclotide on quality of life in adults with chronic constipation: results from two randomized, double-blind, placebo-controlled phase 3 trials. Presented at DDW, May 1–5 2010. Abstract [847d]
- 93.Johnston JM, Schneier H, Lavins BJ, et al. Results from the randomized withdrawal period of a phase 3 clinical trial of linaclotide in chronic constipation. Presented at DDW, May 1–5 2010. Abstract [T1817]
- 94.Michael RG, Yu-Ping L, Kenneth P, John FJ, Allen WM, Michael MK. T1389 TD-5108, a selective 5-HT4 agonist, is consistently better than placebo regardless of response definition in patients with chronic constipation. Gastroenterology. 2008;134:A–545. [Google Scholar]
- 95.Camilleri M, Vazquez-Roque M, Burton D, et al. Pharmacodynamic effects of a novel prokinetic 5-HT4 receptor agonist, ATI-7505, in humans. Neurogastroenterol Motil. 2007;19:30–8. doi: 10.1111/j.1365-2982.2006.00865.x. [DOI] [PubMed] [Google Scholar]
- 96.World Gastroenterology Organisation. WGO-OMGE Practice Guideline: constipation. 2007 Available at: http://www.worldgastroenterology.org/assets/downloads/en/pdf/guidelines/05_constipation.pdf (accessed on 24 August 2010) [Google Scholar]
- 97.Piche T, Dapoigny M, Bouteloup C, et al. Recommandations pour la pratique clinique dans la prise en charge et le traitement de la constipation chronique de l'adulte. Gastroentérol Clin Biol. 2007;31:125–35. [PubMed] [Google Scholar]
- 98.NICE. Irritable bowel syndrome in adults: diagnosis and management of irritable bowel syndrome in primary care (CG61) 2008.


