Abstract
Peritraumatic dissociation (PD) and experiential avoidance (EA) have been implicated in the etiology of posttraumatic stress symptomatology (PTSS); however, the function of these two factors in the onset and maintenance of PTSS following a potentially traumatic event is unclear. The temporal relationships between EA, PD, and the four clusters of PTSS proposed by the Simms/Watson dysphoria model (Simms, Watson, & Doebbeling, 2002) were examined in a three-wave prospective investigation of 532 undergraduate women participating in an ongoing longitudinal study at the time of a campus shooting. Path analyses indicated that pre-shooting EA predicted greater PD, intrusions, and dysphoria symptoms approximately one month post-shooting. PD was associated with increased symptomatology across all four clusters one-month post-shooting, while one-month post-shooting EA was associated with higher dysphoria and hyperarousal symptoms eight months post-shooting. PD had a significant indirect effect on all four PTSS clusters eight months post-shooting via one-month post-shooting symptom reports. The results suggest that both EA and PD show unique influences as risk factors for PTSS following a potentially traumatic event.
Keywords: peritraumatic dissociation, experiential avoidance, posttraumatic stress, trauma
Avoidance of trauma-related stimuli is a core diagnostic feature of posttraumatic stress disorder (PTSD; American Psychiatric Association [APA], 2000). Avoidance symptoms can be conceptualized as attempts to avoid unpleasant emotions, sensations, thoughts, and memories in the aftermath of trauma, which function to initially decrease the frequency and severity of aversive experiences. Avoidance, however, interferes with the emotional processing necessary for the extinction of fear responses that result from a traumatic experience (Foa & Meadows, 1997) and that ultimately increases distressing private experiences, including symptoms of re-experiencing and hyperarousal (Hayes, Strosahl, & Wilson 1999; Hayes, Wilson, Gifford, Follette, & Strosahl, 1996; Marx & Sloan, 2002, 2005; Polusny & Follette, 1995). Despite a growing body of literature indicating that avoidance is influential in the development and maintenance of psychological symptoms among trauma survivors (Marx & Sloan, 2002, 2005; Tull & Roemer, 2003), the role of varied forms of avoidance in the etiology of PTSD is unclear. Moreover, a major limitation of the available literature is the lack of prospective studies examining pre-traumatic, peritraumatic, and posttraumatic avoidance reactions as risk factors for various aspects of PTSD symptomatology. To address these limitations, the present prospective study investigates the temporal influences of experiential avoidance and peritraumatic dissociation on the development and maintenance of posttraumatic stress symptoms within the four symptom clusters proposed by the Simms/Watson dysphoria model of PTSD (Simms, Watson, & Doebbeling, 2002).
Peritraumatic Dissociation
The relationship between experiencing a traumatic event and subsequent dissociative reactions (i.e., altered sense of time, out-of-body experiences, derealization, depersonalization, feeling disconnected from one’s body, and feeling confused or disoriented) is well-documented (e.g., Bremner et al., 1992; Briere, Scott, & Weathers, 2005; Wagner & Linehan, 1998). Dissociative experiences during a traumatic event or shortly thereafter are referred to as peritraumatic dissociation (PD; Marmar et al., 1994). PD is thought to occur in the context of intense traumatic distress (i.e., fear, helplessness, or horror; Bernat, Ronfeldt, Calhoun, & Arias, 1998; Friedman, 2000) and may function to regulate aversive peritraumatic affect as it is experienced (Wagner & Linehan, 1998).
PD is often identified as a significant risk factor for the development of posttraumatic stress symptomatology (e.g., Birmes et al., 2003; Bremner et al., 1992; Marmar et al., 1994); however, the extant literature suggests that the relationship between PD and PTSD symptoms is complex. Meta-analytic reviews support that PD contributes to PTSD symptomatology (Breh & Seidler, 2007; Lensvelt-Mulders et al., 2008), and PD has emerged as a stronger predictor of PTSD symptoms than factors such as prior trauma, prior adjustment, and perceived life-threat during the trauma (Ozer, Best, Lipsey, & Weiss, 2003). Conversely, a review of prospective studies examining the role of PD in predicting PTSD symptoms suggests that PD may have little independent influence in predicting PTSD symptoms beyond three months post-trauma (van der Velden & Wittmann, 2008). Marshall and Schell (2002) found significant cross-sectional associations between PD and PTSD symptoms; however, this association was not significant in later prospective analyses, which may indicate that PD has differential associations with symptoms across time. Consistent with this suggestion, numerous investigations have demonstrated that PD does not prospectively predict PTSD symptoms beyond mental health problems assessed soon after the traumatic event (e.g., van der Velden et al., 2006; Wittmann, Moergeli, & Schnyder, 2006).
Although methodological variability and heterogeneity of trauma types across studies make it difficult to reconcile inconsistencies regarding the role of PD in the development of PTSD (Lensvelt-Mulders et al., 2008), disparities in the timing of PD and PTSD assessments relative to one another and relative to the index trauma may contribute to the multitude of discrepant findings. In its entirety, existing research implies that PD may influence PTSD symptoms differentially at various points during the course of the disorder. Bryant (2007) suggests that PD may play an important role in the etiology of initial psychological problems in the aftermath of a traumatic experience, whereas van der Velden and Wittmann (2008) purport that PD has little influence on more distal symptomatology. Thus, one possible explanation is that PD may contribute to the onset of PTSD symptoms, while other variables may be responsible for the maintenance of symptoms across time.
Experiential Avoidance
Because PD may serve the function of avoiding or altering intense, aversive aspects of a traumatic event in order to allow an individual to cope with the experience, researchers have suggested that PD may be a form of experiential avoidance (EA; Hayes et al., 1996; Marx & Sloan, 2005; Polusny & Follette, 1995; Wagner & Linehan, 1998). EA is defined as the unwillingness to remain in contact with aversive private experiences (i.e., thoughts, memories, sensations, emotions), as well as steps taken to alter the form or frequency of those experiences (Hayes et al., 1996). EA has been implicated in a wide range of affective and behavioral difficulties (Hayes et al., 1996; Kashdan, Barrios, Forsyth, & Steger, 2006; Marx & Sloan, 2002). Further, EA has been implicated in the development of PTSD in general (e.g., Marx & Sloan, 2002, 2005; Tull & Roemer, 2003) and with avoidance, numbing, and hyperarousal symptoms in the King four-factor emotional numbing model of PTSD (e.g., King, Leskin, King, & Weathers, 1998).
In a concurrent examination of PD and EA as predictors of PTSD, Marx and Sloan (2005) found that both PD and EA significantly predicted symptom severity at baseline. Prospectively, EA, but not PD, predicted PTSD symptom severity over and above baseline PTSD symptoms. These findings support the notion that EA, more so than PD, may play a substantial role in the maintenance of PTSD symptoms following trauma exposure. However, a lack of pre-trauma assessments of EA and PTSD symptomatology precludes conclusions about temporal sequencing of these relationships. Additionally, 78% of the sample reported an index traumatic event that occurred six months to more than five years prior, increasing the likelihood of errors or bias in the recall of PD (Marshall & Schell, 2002). The extended time delay between the traumatic event and baseline assessments makes inferences regarding symptom onset impossible, while also weakening conclusions that can be drawn about the course of PTSD symptom severity.
The Present Study
Despite extant research and substantial theoretical support, questions remain regarding the associations between EA, PD, and posttraumatic stress symptomatology (PTSS). Examining these relationships is relevant for improving current understanding of the development of PTSD and evaluating to what extent pre-traumatic, peritraumatic, and post-traumatic factors influence the course of PTSD symptomatology. The present study aims to examine the influence of EA and PD on PTSS across time. Additionally, we sought to fill a gap in the literature by investigating whether PD and EA have differential effects on symptoms among the four clusters of PTSS (i.e., intrusions, avoidance, dysphoria, hyperarousal) proposed by the Simms/Watson dysphoria model of PTSD (Simms et al., 2002). This latter objective is important for advancing understanding of factors that contribute to PTSS as conceptualizations of the structure of PTSD evolve beyond the current DSM-IV criteria. In addition, an examination of PTSS clusters allows investigation of whether PD and EA are predictive of PTSS beyond the avoidance cluster. Although research on the structure of PTSS has shown support for two 4-factor models (i.e., the King emotional numbing [King et al., 1998] and Simms/Watson dysphoria models [Simms et al., 2002]), we chose to utilize the Simms/Watson model because of recent evidence supporting this model in a range of samples exposed to various types of potentially traumatic experiences (see Yufik & Simms, 2010, for a recent meta-analytic review).
In the present study, EA, PD, and PTSS were assessed in a prospective investigation among college women following a campus mass shooting. At 3:05 p.m. on February 14, 2008, a gunman opened fire in a classroom of over 120 students on the Northern Illinois University (NIU) campus, in DeKalb, Illinois, killing five and wounding 21 before taking his own life. It was the fourth-deadliest university shooting in U.S. history. At the time of the shooting, a sample of undergraduate women was enrolled in a longitudinal study of sexual revictimization. The trauma-focused nature of the pre-shooting longitudinal study provided the opportunity to examine the effects of EA and PD in the development of PTSS following a large-scale potentially traumatic event.
Data were collected at three time points. The initial assessment took place prior to the occurrence of the shooting, allowing for pre-trauma assessment of EA and PTSS related to previous exposure to potentially traumatic events. The second assessment was initiated 17 days after the shooting (M = 27 days), providing relatively fast measurement of PD and acute reactions to the campus shooting. The third assessment took place approximately eight months post-shooting, allowing for the measurement of symptoms across a considerable span of time. The prospective nature of the study provides a unique opportunity to understand the effects of EA and PD in the course of PTSS.
Consistent with prior research suggesting that PD may be a form of EA (Hayes et al., 1996; Marx & Sloan, 2005; Polusny & Follette, 1995; Wagner & Linehan, 1998), we hypothesized that higher levels of pre-shooting EA would increase the likelihood of PD at the time of the shooting. Secondly, we hypothesized that higher levels of PD would be associated with more severe PTSS in the weeks following the shooting but would not have a direct effect on symptoms eight months post-shooting. Finally, we posited that one-month post-shooting EA would contribute to the maintenance of PTSS at eight-months post-shooting.
Method
Procedure
Data were obtained from female participants who completed three waves of a longitudinal study; all waves received approval from the NIU Institutional Review Board. Participants who completed the first session (T1; N = 1,045) were Introductory Psychology students recruited from a mass testing pool to provide an initial assessment for a longitudinal investigation of risk factors for sexual revictimization. The only prerequisites for T1 participation were that participants be women over the age of 18 and fluent in English; participants were not selected based on victimization history. At T1, participants completed measures of lifetime exposure to potentially traumatic events, PTSS, and EA as part of a larger battery of measures. Measures included in the T1 assessment were computer administered and took approximately one hour to complete. Participants received partial course credit for their participation. Data for T1 were collected between September 2006 and prior to the shooting on February 14, 2008.
The sample for the present study was drawn from participants who consented to future contact at T1 and were enrolled at the university at the time of the shooting. Specifically, of the 1,045 female participants interviewed at T1, 812 (78%) were invited via e-mail to complete a battery of measures on-line. Of those invited, 691 (85%) completed the post-shooting assessment (T2). The T2 survey was brief; taking approximately 30 minutes to complete. Participants could opt to receive $40 compensation or partial course credit, for the subset enrolled in Introductory Psychology. During the T2 session, participants completed measures of PTSS, EA, PD related to the shooting, and level of exposure to the shooting. The time elapsed between T1 and the shooting ranged from a few hours to 74 weeks, with an average of 27 weeks (SD = 21). The T2 survey was launched 17 days post-shooting (March 2, 2008). The average time elapsed between the shooting and completion of the T2 assessment was 27 days (SD = 12), and a majority of the sample (80%) completed the T2 survey within 40 days.
Approximately seven months post-shooting (September 28, 2008), participants from the T2 sample (n = 691) were invited via e-mail to complete an additional follow-up survey online. Five hundred eighty-eight (85%) participants from the T2 sample completed the third session (T3). The T3 survey took approximately 30 minutes to complete and assessed EA and PTSS related to the shooting. Participants could opt to receive $40 compensation for participation. The average time elapsed between the shooting and the T3 assessment was 35 weeks (SD = 3.1). Fifty-six participants who completed the T3 survey reported that they were not on campus during the shooting and did not know anyone who was wounded or killed. These participants were excluded from the present study, resulting in a final sample of 532.
Participants
The average age of participants was 19.2 (SD = 1.95) at T1, 19.9 (SD = 2.01) at T2, and 20.4 (SD = 2.04) at T3. Among the final sample (n = 532), 71% self-identified their race as White, 17% as Black, and 3% as Asian, while 8% identified their race as belonging to another category and 1% refused. With regard to ethnicity, 7% of participants self-identified as Hispanic/Latino.
Measures
Potential covariates
Age and race/ethnicity were evaluated as potential covariates. Race and ethnicity were assessed according to the National Institute of Health policy on reporting race (six categories plus “other”) and ethnicity (Hispanic or Latino) data. In the present analyses, race and ethnicity were collapsed into a single dummy coded variable (coded as White and Non-Hispanic [n = 368, 69.2%] versus all others [n = 152, 28.6%]). To control for duration effects on the relationships between variables measured at T1 and T2, time elapsed between the T1 and T2 assessments was calculated in weeks. The resulting variable was non-normal and was Blom transformed and rank normalized, which resulted in nonsignificant skew and kurtosis levels.
Exposure to mass shooting
Participants completed a 12-item measure of exposure, modified from the Littleton, Grills-Taquechel, and Axsom (2009) Virginia Tech Shooting Exposure Measure. Participants were asked a series of yes/no questions about their personally-experienced exposure to aspects of the shooting (e.g., on campus, heard gunfire, saw individuals who had been wounded or killed, knew anyone wounded, in building placed on lockdown). A total score was calculated by summing across the 12 items.
Traumatic Life Events Questionnaire (TLEQ)
The TLEQ (Kubany, Haynes et al., 2000) assesses exposure to 22 potentially traumatic events as specified in Criterion A1 of the diagnostic criteria for PTSD in the DSM-IV-TR (APA, 2000). Additionally, the TLEQ assesses Criterion A2 of the diagnostic criteria for PTSD (i.e., the subjective experience of intense fear, helplessness, or horror). The TLEQ has demonstrated good short-term test-retest percent agreement (approximately 84% across several samples and time periods) as well as good content validity (Kubany, Haynes et al., 2000). In the present study, participants completed the TLEQ at T1 to report lifetime trauma history. Participants indicated the frequency with which they had experienced 22 potentially traumatic events on a scale of 0 to 6 (0 = Never, 1 = Once, 2 = Twice, 3 = 3 times, 4 = 4 times, 5 = 5 times, 6 = More than 5 times). A sum score was calculated across the 22 items; the resulting variable was non-normal and was Blom transformed and rank normalized, which resulted in nonsignificant skew and kurtosis levels.
Distressing Events Questionnaire (DEQ)
The DEQ (Kubany, Leisen, Kaplan, & Kelly, 2000) is a 17-item self-report measure which assesses the severity of the 17 symptoms of PTSD (APA, 2000) experienced in the previous 30 days, rated on a scale of 0 (Absent or did not occur) to 4 (Present to an extreme or severe degree). A total score of 18 or above is indicative of significant symptoms among women (Kubany, Leisen et al., 2000). The DEQ has demonstrated good short-term test-retest reliability, excellent internal consistency, and good convergent and discriminant validity (Kubany, Leisen et al., 2000). The DEQ was administered at all time points. For Time 2 and Time 3, participants were instructed to answer the DEQ based on the shooting event. Consistent with the four-factor Simms/Watson dysphoria model (Simms et al., 2002), mean subscale scores were calculated for the intrusions, avoidance, dysphoria, and hyperarousal clusters. Internal consistency within this sample for each cluster at each time point was acceptable (Intrusions; α = .85 to .86, Avoidance α = .79 to .83, Dysphoria; α = .86 to .88; Hyperarousal; α = .74 to .80).
Acceptance and Action Questionnaire – II (AAQ-II)
The AAQ-II (Bond et al., in press) is a 7-item self-report measure of experiential avoidance (e.g., I am afraid of my feelings, Emotions cause problems in my life). Items are rated on a scale from 1 (Never true) to 7 (Always true). Across six samples (N = 2,816), the AAQ-II demonstrated good convergent, discriminant, and incremental validity (Bond et al., in press). The 3- and 12-month test-retest reliability coefficients were .81 and .79, respectively. Further, the mean internal consistency estimate was .84 with a range of .78 to .88 across samples. Scores on the AAQ-II concurrently, prospectively and incrementally predict a range of relevant outcomes. The AAQ-II was administered at all time points. Internal consistency within this sample for each time point was good (T1; α = .84, T2; α = .91, T3; α = .91).
Peritraumatic Dissociative Experiences Questionnaire (PDEQ)
The PDEQ (Marmar et al., 1994; Marmar, Metzler, & Otte, 2004) is a self-report measure of PD. A recent examination of the latent structure of the PDEQ revealed that the measure is best characterized by two 4-item factors representing 1) altered awareness and 2) depersonalization/derealization. The first factor failed to predict post-trauma symptomatology, while the second factor was predictive of symptoms of depression, anxiety, and acute stress disorder post-trauma (Brooks et al., 2009). At T2, the internal consistency for the 4-items of the PDEQ corresponding to peritraumatic depersonalization/derealization was .79 (i.e., “My sense of time changed – things seemed to be happening in slow motion,” “What was happening seemed unreal to me, like I was in a dream or watching a movie or play,” “I felt as though I was a spectator watching what was happening to me,” “There were moments when my sense of my own body seemed distorted or changed”). Items are rated from 1 (Not at all true) to 5 (Extremely true). When completing the 4-items at T2, participants were asked to focus specifically on their experiences and reactions “during the mass shooting at NIU.”
Results
Descriptive Statistics and Preliminary Analyses
Means, standard deviations, and correlations among variables are presented in Table 1. At T1, 20.8% of participants eligible for T2 (n = 812), endorsed experiencing significant levels of pre-shooting PTSS in the 30 days prior to the T1 assessment (as indicated by a score of 18 or above on the DEQ; Kubany, Leisen et al., 2000). The average frequency of potentially traumatic events reported by participants at T1 was 7.57 (SD = 7.12). The most frequently endorsed potentially traumatic events were the unexpected death of a loved one, a loved one surviving a life threatening illness, natural disaster, witnessing family violence, stalking, and sexual abuse or assault.
Table 1.
Correlations, Means, and Standard Deviations
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1T2 WKSa | -- | ||||||||||||||||||
| 2. T1 TRMa | .01 | -- | |||||||||||||||||
| 3. T1 EA | .02* | .21** | -- | ||||||||||||||||
| 4. T1 INT | .01 | .45** | .43** | -- | |||||||||||||||
| 5. T1 AVO | −.02 | .40** | .33** | .76** | -- | ||||||||||||||
| 6. T1 DYS | .00 | .47** | .53** | .67** | .56** | -- | |||||||||||||
| 7. T1 HYP | .01 | .37** | .37** | .48** | .41** | .56** | -- | ||||||||||||
| 8. T2 EA | −.05 | .18** | .67** | .36** | .27** | .42** | .27** | -- | |||||||||||
| 9. T2 PD | .02 | .11* | .24** | .19** | .18** | .21** | .13** | .36** | -- | ||||||||||
| 10. T2 EXP | −.06 | .04 | .16** | .10* | .10* | .11* | .08^ | .24** | .23** | -- | |||||||||
| 11. T2 INT | −.06 | .18** | .24** | .21** | .19** | .19** | .17** | .40** | .49** | .28** | -- | ||||||||
| 12. T2 AVO | −.07^ | .22** | .24** | .26** | .27** | .22** | .19** | .37** | .40** | .20** | .69** | -- | |||||||
| 13. T2 DYS | −.03 | .26** | .37** | .27** | .23** | .31** | .17** | .59** | .57** | .29** | .65** | .56** | -- | ||||||
| 14. T2 HYP | −.05 | .12** | .20** | .23** | .19** | .22** | .20** | .32** | .47** | .28** | .54** | .44** | .57** | -- | |||||
| 15. T3 EA | −.03 | .15** | .60** | .27** | .19** | .37** | .26** | .62** | .26** | .16** | .26** | .25** | .42** | .24** | -- | ||||
| 16. T3 INT | −.07 | .17** | .28** | .25** | .24** | .26** | .22** | .32** | .32** | .31** | .40** | .33** | .39** | .30** | .36** | -- | |||
| 17. T3 AVO | −.03 | .16** | .22** | .25** | .28** | .25** | .19** | .28** | .29** | .24** | .35** | .44** | .37** | .30** | .29** | .65** | -- | ||
| 18. T3 DYS | −.04 | .15** | .36** | .25** | .22** | .35** | .24** | .45** | .24** | .25** | .27** | .27** | .45** | .22** | .60** | .56** | .47** | -- | |
| 19. T3 HYP | −.01 | .14** | .21** | .18** | .16** | .19** | .22** | .31** | .28** | .25** | .34** | .28** | .39** | .43** | .36** | .52** | .40** | .54** | -- |
| M | −.05 | .00 | 2.49 | .69 | .82 | .49 | .61 | 2.60 | 2.79 | 3.21 | .77 | .84 | 1.03 | 1.88 | 2.49 | .39 | .46 | .36 | 1.02 |
| SD | .97 | .98 | 1.07 | .78 | 1.09 | .68 | .88 | 1.15 | 1.06 | 1.45 | .81 | .98 | .83 | 1.30 | 1.21 | .59 | .80 | .58 | 1.10 |
| Minimum | −2.89 | −1.98 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Maximum | 2.62 | 3.07 | 6.29 | 4 | 4 | 3.5 | 4 | 6.14 | 5 | 10 | 4 | 4 | 3.88 | 4 | 7 | 3.2 | 4 | 3.63 | 4 |
| N | 532 | 529 | 530 | 496 | 491 | 492 | 492 | 532 | 531 | 532 | 532 | 530 | 526 | 520 | 528 | 526 | 526 | 525 | 525 |
Note. T1 = Time 1; T2 = Time 2; T3 = Time 3; WKS = weeks between T1 and T2; TRM = frequency of T1 trauma; EA = experiential avoidance; INT = posttraumatic stress symptom (PTSS) cluster of intrusions; AVO = PTSS cluster of avoidance; DYS = PTSS cluster of dysphoria; HYP =PTSS cluster of hyperarousal; PD = peritraumatic dissociation; EXP = exposure to mass shooting.
Underlined values designate temporal stability correlations.
Variable was transformed to reduce non-normality..
p < .01,
p < .05,
p < .10.
Of the T2 sample, 524 participants (76%) were on campus at the time of the shooting, 474 (69%) saw police or emergency responders, and 334 (48%) were in a campus building that was locked down. One-hundred-and-fifty-two (22%) participants saw people who had been killed or wounded, 44 (6%) heard gunfire, 24 (3%) were in the building in which the shooting occurred, 15 (2%) saw the gunman, 11 (2%) witnessed the gunman firing his weapon, and 3 (.4%) were wounded in the shooting. Two-hundred-and-thirty-five (34%) participants knew someone who was wounded in the shooting and 159 (23%) knew someone who died in the shooting.
At T2, 90% of the sample (n = 622/691) reported experiencing intense fear, helplessness, or horror (Criterion A2 of the diagnostic criteria for PTSD: DSM-IV-TR; APA, 2000) in response to the shooting. Additionally, 49.4% of T2 participants (n = 341/691), and 11.4% of T3 participants (n = 67/588) endorsed significant levels of PTSS associated with the shooting (a total score of 18 or above on the DEQ; Kubany, Leisen et al., 2000).
To assess differences due to attrition between T1 and T2, those responding at T2 (n = 691) were compared to eligible nonresponders (n = 121) on demographics and variables measured at T1. Non-Hispanic White participants were more likely to complete T2 than all other participants, χ2(1, N = 793) = 5.14, p < .05, and participants who completed the T2 assessment reported lower levels of EA at T1 compared to participants who did not complete T2, t(808) = 2.58, p < .01. To assess differences due to attrition between T2 and T3, those responding at T3 (n = 588) were compared with those who did not respond (n = 103) on demographics and T2 variables. Participants who identified as being of Non-Hispanic White race/ethnicity were more likely to complete T3 than participants from all other race/ethnicity categories, χ2(1, N = 674) = 12.4, p < .01. No other significant differences emerged. The 56 participants who were excluded because they were not on campus during the shooting and did not know anyone who was wounded or killed were also compared to the 532 participants included in the present analyses. Excluded participants had longer intervals between T1 and T2 assessments (t(586) = 3.70, p < .001), reported less PD (t(586) = −5.10, p < .001), and endorsed fewer intrusion (t(586) = −3.52, p < .001) and avoidance symptoms (t(586) = −3.14, p < .01) at T2.
Path Model
EA (measured at T1, T2, and T3) and PD (measured at T2) were examined as possible risk factors for each of the four PTSS clusters (i.e., intrusions, avoidance, hyperarousal, and dysphoria) at T2 and T3. Path analysis was conducted in Mplus (Version 5.21; Muthén & Muthén, 1998–2009) using maximum likelihood estimation. Parameters were estimated using all available data (incomplete data were assumed to be missing at random, and thus included in the parameter estimates).
Age and race/ethnicity were included in the model because they were significantly correlated with at least one of the key study variables. Specifically, age (r(529) = .10, p < .05) and race/ethnicity (r(529) = −.19, p < .001) were associated with frequency of potentially traumatic events reported at T1. Race/ethnicity was also correlated with PD (r(517) = .10, p < .05). Pre-shooting PTSS and frequency of trauma exposure were included in the model to control for effects of previous trauma experiences and symptomatology. Weeks elapsed between T1 and T2 was modeled to control for duration effects on the relationships between variables measured at T1 and T2. Level of exposure to the shooting was included as a predictor of PD and T2 and T3 PTSS. Within each time-point, each of the four PTSS clusters and EA were correlated. All paths estimated in the model and the resulting standardized path coefficients are shown in Table 2.
Table 2.
Standardized Path Coefficients for Path Analytic Model
| Variables | AGE | T1T2 WKS |
RACE | T1 TRM |
T1 EA |
T1 INT |
T1 AVO |
T1 DYS |
T1 HYP |
T2 EXP |
T2 PD |
T2 EA |
T2 INT | T2 AVO |
T2 DYS |
T2 HYP |
T3 EA |
T3 INT |
T3 AVO |
T3 DYS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 TRM | .10* | −.19*** | -- | |||||||||||||||||
| T1 EA | −.05 | .04 | .30*** | -- | ||||||||||||||||
| T1 INT | −.01 | −.02 | .49*** | .43*** | -- | |||||||||||||||
| T1 AVO | .04 | .00 | .43*** | .34*** | .76*** | -- | ||||||||||||||
| T1 DYS | .03 | −.03 | .50*** | .53*** | .68*** | .58*** | -- | |||||||||||||
| T1 HYP | .05 | −.05 | .39*** | .38*** | .50*** | .42*** | .56*** | -- | ||||||||||||
| T2 PD | .05 | .09* | .00 | .15** | .04 | .04 | .06 | −.00 | .19*** | -- | ||||||||||
| T2 EA | −.02 | −.06^ | .01 | .59*** | .07 | −.04 | .05 | −.03 | .20*** | -- | ||||||||||
| T2 INT | .01 | −.04 | −.03 | .07 | .09* | .08 | −.00 | −.09 | .05 | .14*** | .44*** | .22*** | -- | |||||||
| T2 AVO | −.01 | −.06^ | −.08* | .08^ | .09^ | .06 | .12^ | −.08 | .04 | .07^ | .34*** | .20*** | .59*** | -- | ||||||
| T2 DYS | .02 | −.03 | .02 | .11** | .19*** | .01 | .00 | .06 | −.06 | .10** | .47*** | .40*** | .49*** | .42*** | -- | |||||
| T2 HYP | .04 | −.03 | −.10** | −.05 | .03 | .10 | .00 | −.02 | .09^ | .17*** | .40*** | .12* | .38*** | .30*** | .41*** | -- | ||||
| T3 EA | −.02 | −.03 | .01 | .57*** | −.05 | .00 | .08 | .04 | -- | |||||||||||
| T3 INT | −.00 | .03 | .07^ | .20*** | .08 | .08^ | .16** | .06 | .07 | .01 | .23*** | -- | ||||||||
| T3 AVO | −.01 | .01 | .04 | .13** | .06 | .04 | −.01 | .32*** | .07 | .03 | .16*** | .57*** | -- | |||||||
| T3 DYS | −.02 | −.07^ | −.02 | .12** | .00 | .27*** | −.09 | .03 | .34*** | −.06 | .46*** | .48*** | .38*** | -- | ||||||
| T3 HYP | −.01 | .02 | .04 | .10* | .01 | .12** | .02 | −.00 | .09 | .30*** | .22*** | .41*** | .28*** | .47*** |
Note. T1= Time 1; T2 = Time 2; T3 = Time 3; AGE = age in weeks at T1; T1T2 WKS = weeks between T1 and T2; RACE = White and Non-Hispanic versus all others; TRM = frequency of T1trauma; EA = experiential avoidance; INT = posttraumatic stress symptom (PTSS) cluster of intrusions; AVO = PTSS cluster of avoidance; DYS = PTSS cluster of dysphoria; HYP = PTSS cluster of hyperarousal; PD = peritraumatic dissociation; EXP = exposure to mass shooting.
Correlations are italicized. Empty cells indicate non-modeled relationships. Directionality is by column, not row (i.e., variable in column header predicts non-italicized coefficients in the column).
p <.001,
p <.01,
p <.05,
p <.10
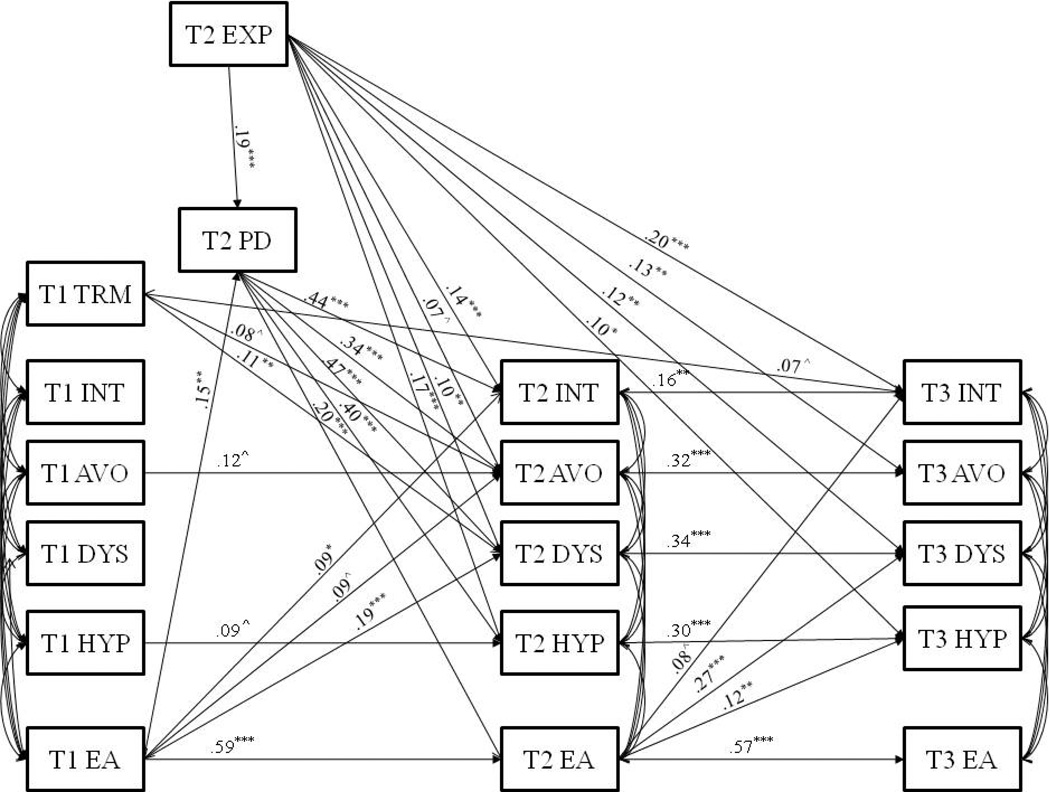
Significant paths among primary hypothesized relationships in the resulting model are shown in Figure 1. The model fit was good, χ2 (47) = 130.77, p < .001, RMSEA was .06 (90% confidence interval of .05 to .07), CFI = .98, and TLI = .92. The model accounted for a significant amount of variance in PTSS at T2 (Intrusions; R2 = .29, Avoidance; R2 = .22, Dysphoria; R2 = .38, Hyperarousal; R2 = .27) and T3 (Intrusions; R2 = .22, Avoidance; R2 = .22, Dysphoria; R2 = .26, Hyperarousal; R2 = .23).
Figure 1.
Results of path analytic model depicting experiential avoidance and peritraumatic dissociation as risk factors for posttraumatic stress symptom (PTSS) clusters with nonsignificant paths not depicted. Coefficients are standardized. N = 532. χ2 (47) = 133.77, p < .001, RMSEA = .06, CFI = .98, TLI = .92. T1 = Time 1; T2 = Time 2; T3 = Time 3; TRM = frequency of T1 trauma; EA = experiential avoidance; INT = PTSS cluster of intrusions; AVO = PTSS cluster of avoidance; DYS = PTSS cluster of dysphoria; HYP = PTSS cluster of hyperarousal; PD = peritraumatic dissociation; EXP = exposure to mass shooting. *** p < .001, **p < .01, *p < .05, ^p < .10.
Examination of covariates revealed that Non-Hispanic White participants reported higher levels of PD than participants in other racial/ethnic categories (β = .09, p < .05). Non-Hispanic White participants reported fewer potentially traumatic events at T1 (β = −.19, p < .001) and lower levels of avoidance (β = −.08, p < .05) and hyperarousal (β = −.10, p < .01) symptoms at T2. Higher levels of exposure to the shooting predicted increased ratings of PD (β = .19, p < .001), greater PTSS among three of the four clusters at T2 (Intrusions; β = .14, p < .001, Dysphoria; β = .10, p < .01, Hyperarousal; β = .17, p < .001; Avoidance; β = .07, p < .10), and all four clusters at T3 (Intrusions; β = .20, p < .001, Avoidance; β = .13, p < .01, Dysphoria; β = .12, p < .01, Hyperarousal; β = .10, p < .05).
As hypothesized, higher levels of pre-shooting EA predicted PD at the time of the shooting (β = .15, p < .01). PD did not have a significant direct effect on PTSS at T3 in our analyses, but did display strong relationships with all four PTSS clusters at T2 (Intrusions; β = .44, p < .001, Avoidance; β = .34, p < .001, Dysphoria; β = .47, p < .001, Hyperarousal; β = .40, p < .001). In addition, PD demonstrated a significant indirect effect on each of the T3 PTSS clusters via its relationship with T2 PTSS (Intrusions; β = .07, p < .01, Avoidance; β = .11, p < .001, Dysphoria; β = .16, p < .001, Hyperarousal; β = .12, p < .001). Results also support the hypothesis that EA would contribute to the maintenance of PTSS over time; however, EA had differential prospective effects on various PTSS clusters. As depicted in the model, T1 EA was predictive of intrusions (β = .09, p < .05) and dysphoria symptoms (β = .19, p < .001) at T2. T2 EA was predictive of dysphoria (β = .27, p < .001) and hyperarousal (β = .12, p < .01) symptoms at T3. EA was also relatively stable across time.
Discussion
The aim of the current study was to integrate research on EA and PD as risk factors for PTSS and to investigate EA and PD as predictors of the prospective course of the four clusters of PTSS proposed by the Simms/Watson dysphoria model (Simms et al., 2002). We utilized a three-wave prospective investigation with a sample of 532 undergraduate women who were involved in an ongoing longitudinal study at the time of a campus shooting. Among our sample, pre-shooting EA was found to predict reports of PD--specifically, depersonalization and derealization--which supports the argument that PD may aid in avoiding the experience of intense, aversive peritraumatic emotional responses (e.g., Bernat et al., 1998; Friedman, 2000; Marx & Sloan, 2005). Despite their association, PD and EA demonstrated differential effects on the course of PTSS.
PD was strongly related to all four clusters of PTSS approximately one month post-shooting, supporting our hypothesis that PD would contribute to PTSS after experiencing a potentially traumatic event. PD has been proposed as an important etiological factor in the development of PTSD symptomatology, as dissociative experiences during a trauma may interfere with the formation or organization of memories (Spiegel, 1991; van der Kolk & Fisler, 1995). In individuals with PTSD, traumatic memories are often fragmented and poorly organized, resulting in deficits in the ability to recall aspects of the trauma (Amir, Stafford, Freshman & Foa, 1998; Foa, Molnar & Cashman, 1995; Foa & Riggs, 1993; Koss, Figueredo, Bell, Tharan & Tromp, 1996; van der Kolk & Fisler, 1995). Thus, PD has been suggested as an explanation for the fragmentation of traumatic memories and a subsequent contributing factor to the development of PTSD symptoms (Spiegel, 1991; van der Kolk & Fisler, 1995). In support of this theory, Halligan, Michael, Clark, and Ehlers (2003) found that peritraumatic cognitive processing was associated with the development of disorganized memories and PTSD in a cross-sectional sample of assault victims.
PD most likely occurs in response to intense peritraumatic emotional reactions (i.e., high levels of fear, helplessness, or horror; Bernat et al., 1998; Friedman, 2000). Consistent with this conceptualization, Fikretoglu et al. (2007) reported that fear, helplessness, or horror, as well as symptoms of panic, predicted the occurrence of PD among individuals with a history of trauma exposure. Although there are growing questions about the validity of the inclusion of peritraumatic emotional responses in the diagnostic criteria for PTSD (e.g., Bedard-Gilligan & Zoellner, 2008; Bovin & Marx, in press; Kilpatrick, Resnick, & Acierno, 2009), the experience of intense fear, helpless, or horror currently constitutes PTSD Criterion A2 (APA, 2000). PD may function to limit awareness of threatening experiences and allow an individual to cope with intense emotions that would otherwise be overwhelming (e.g., Bryant, 2007; Horowitz, 1986; Moleman, van der Hart, & van der Kolk, 1992). Thus, PD is likely adaptive during and shortly after the experience of a trauma because of its ability to protect an individual from intense fear, helplessness and horror. PD’s adaptive function appears short-lived, however, as it has been associated with development of PTSD symptomatology (Bremner, 1997; Briere et al., 2005; Marmar, Weiss, & Metzler, 1998; van der Kolk, van der Hart, & Marmar, 1996). Although we conceptualize PD as a functional reaction to intense peritraumatic emotions, we do not assume that it is an intentional response. As suggested by the cognitive model of PTSD proposed by Ehlers and Clark (2000), dissociative reactions, including PD, likely include both strategic and automatic or reflexive responses.
Despite its initial deleterious effects, PD did not have a direct effect on reports of PTSS approximately eight months post-shooting in the present study. This finding corresponds with a number of studies that have failed to demonstrate a prospective link between PD and later symptomatology when early post-trauma symptoms are taken into account (e.g., van der Velden et al., 2006; Wittmann et al., 2006), suggesting that other factors, such as EA, may exert a stronger influence on the maintenance of symptoms across time. The current results suggest that EA functions both to promote and maintain the presence of various PTSS. In the present sample, pre-shooting EA was predictive of intrusions and dysphoria symptoms approximately one month post-shooting. In addition, post-shooting EA was predictive of dysphoria and hyperarousal symptoms approximately eight months later. Use of a pre-shooting assessment of EA, as well as the ability to take into account the effects of pre-shooting PTSS, allows for greater confidence in temporal precedence and strengthens conclusions that can be drawn about the effect of EA in increasing vulnerability to PTSD (Vogt, King, & King, 2007).
EA has been suggested as an important factor in the development and maintenance of PTSS because attempts to suppress, control, or avoid aversive private events are linked to psychological and behavioral difficulties (Hayes et al., 1996, Marx & Sloan, 2002). Continued attempts to avoid unwanted emotions, thoughts, memories, and sensations associated with a traumatic experience may initially decrease the frequency and severity of aversive experiences, serving to reinforce an individuals’ likelihood of engaging in experientially avoidant behavior. Ultimately, however, continued avoidance attempts result in an increased frequency of these aversive experiences (Hayes et al., 1996; Hayes et al., 1999; Polusny & Follette, 1995). EA may also serve to maintain PTSS by preventing extinction of the fear response associated with traumatic memories and emotions (Ehlers & Clark, 2000).
Although EA has previously been suggested to increase the occurrence of re-experiencing, avoidance, and hyperarousal symptoms associated with PTSD (Marx & Sloan, 2005), the current results suggest that EA does not prospectively predict all clusters of PTSS. Of particular note is that EA was only marginally predictive of subsequent avoidance symptoms. In contrast, EA had the strongest and most consistent influence on later dysphoria symptoms, which have been suggested to represent general distress rather than symptoms specific to PTSD (Simms et al., 2002). EA has been linked to a number of negative mental health outcomes in prior research (Hayes et al., 1996; Kashdan et al., 2006; Marx & Sloan, 2002), which in concert with the present findings, suggests that EA may underlie a range of psychopathology characterized by internalized distress, including depressive disorders, anxiety disorders, and PTSD.
The finding that EA and PD may have differential temporal effects on the development of different facets of PTSS has important implications for treatment and prevention. Specifically, screening individuals for PD experiences in the acute aftermath of potentially traumatic events may help identify those at risk for developing symptoms associated with posttraumatic stress, at which point appropriate interventions may be implemented. Additionally, interventions designed to promote the acceptance of emotional experiences and increase psychological flexibility, such as Acceptance and Commitment Therapy (ACT; Hayes et al., 1999), may prevent or mitigate symptom severity among individuals exposed to trauma.
Despite the pattern of clear and theoretically meaningful findings in the present study, several limitations should be acknowledged. A primary limitation involves restrictions in generalizing the present findings to symptoms consistent with a PTSD diagnosis. A portion of female participants in our sample likely did not experience a level of exposure to the shooting consistent with the current definition of a Criterion A stressor, which precludes the possibility of a PTSD diagnosis. Although level of exposure to the shooting was included in analyses and participants with the least exposure were excluded, the measure used to assess level of exposure is not reflective of PTSD Criterion A1. That being said, studies following mass traumas suggest that many individuals experience significant distress following these events, even among those not directly exposed (e.g., North, Smith, & Spitznagel, 1994; Schwarz & Kowalski, 1991). Additionally, Criterion A2 was endorsed by 90% of the sample, which, while diminishing the ability to utilize this measure in analyses, suggests that the shooting was highly impactful. There was also a relatively short latency between the occurrence of the shooting and the assessment of symptoms at T2, with a large portion of the sample completing the T2 assessment within 30 days. Although the immediacy of the post-shooting assessment is a strength of the study, the symptoms assessed at T2 are better viewed as acute reactions to the shooting rather than PTSD symptoms. Despite these limitations, an examination of PTSS is likely beneficial given evidence that PTSD appears to have a dimensional structure where differences in symptomatology reflect variations along a continuum of posttraumatic stress responses, rather than representing a qualitatively distinct syndrome (e.g., Broman-Fulks et al., 2006; Ruscio, Ruscio, & Keane, 2002).
Issues related to the measurement of PD also present important limitations. Despite the relatively short latency between the occurrence of the shooting and the T2 assessment, reports of PD were retrospective and may be subject to biases of both self-report and time. Furthermore, the concurrent assessment of PD and PTSS at T2 may confound the results of the present study, particularly because evidence suggests that recall of PD may be biased by an individual’s current psychological state (Bryant, 2007; Candel & Merckelbach, 2004; Harvey & Bryant, 1999; Marshall & Schell, 2002). Thus, at T2, the direction of the relationship between PD and PTSS is not definitive (Sterlini & Bryant, 2002). Additionally, the current study utilized four items to measure PD, based on recent findings identifying this cluster of items as predictive of symptoms post-trauma (Brooks et al., 2009). The majority of available studies incorporate the 10-item version of the PDEQ, which may reduce generalizability across studies using the 10-item measure. Further, dissociation was not assessed at T1, precluding examination of how PD may be influenced by pre-trauma dissociative tendencies.
Because the sample for the present study was comprised solely of undergraduate women enrolled in an introductory psychology course, the ability to generalize the current findings to other populations is limited. This is of particular concern given research suggesting differences between women and men in the prevalence and chronicity of PTSD symptoms (Norris, Foster, & Weisshaar, 2002; Tolin & Foa, 2006). There were also differences in sample characteristics due to attrition over the course of the study, which may have biased the present findings. Limits to generalizability may also be associated with the nature of the traumatic experience of focus in the current study. Because all participants reported PTSS related to the mass shooting, results are limited to reactions to that singular traumatic event. In addition, for some participants, the T1 PTSS assessment was fairly distal from the shooting. An added limitation is that EA, as measured with the AAQ-II, had lower temporal stability in the present sample than in previous research (Bond et al., in press). Finally, PTSS and PD measures were linked to the index event while EA was not; the impact of this difference is unknown.
Given the methodological issues raised, it will be important to replicate and extend the present results in other populations. Obtaining the samples necessary to test pre-traumatic, peritraumatic, and posttraumatic emotional and behavioral responses poses a considerable challenge to researchers. To date, existing prospective studies lack pre-trauma assessments of EA and PTSD symptomatology, limiting the ability to discriminate between pre-traumatic risk factors and posttraumatic reactions. In addition, it continues to be difficult to conduct rapid post-trauma assessments because of the unexpected nature of traumatic events.
Despite the limitations of the present study, the findings have the potential to contribute significantly to the literature examining PD and EA as risk factors for PTSS. Given the reliance on cross-sectional designs and the limitations of the available prospective studies in this area, the current prospective design, availability of pre-trauma assessments, and speed of the initial post-trauma assessment represent unique strengths of the study.
Acknowledgments
This research was funded by grants to the second author from the Joyce Foundation, the National Institute for Child and Human Development (1R15HD049907-01A1), and the National Institute of Mental Health (5R21MH085436-02).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: Author; 2000. text revision. [Google Scholar]
- Amir N, Stafford J, Freshman MS, Foa EB. Relationship between trauma narratives and trauma pathology. Journal of Traumatic Stress. 1998;11:385–392. doi: 10.1023/A:1024415523495. [DOI] [PubMed] [Google Scholar]
- Bedard-Gilligan M, Zoellner LA. The utility of the A1 and A2 criteria in the diagnosis of PTSD. Behaviour Research and Therapy. 2008;46:1062–1069. doi: 10.1016/j.brat.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernat JA, Ronfeldt HM, Calhoun KS, Arias I. Prevalence of traumatic events and peritraumatic predictors of posttraumatic stress symptoms in a nonclinical sample of college students. Journal of Traumatic Stress. 1998;11:645–664. doi: 10.1023/A:1024485130934. [DOI] [PubMed] [Google Scholar]
- Birmes P, Brunet A, Carreras D, Ducasse JL, Charlet JP, Lauque D, Schmitt L. The predictive power of peritraumatic dissociation and acute stress symptoms for posttraumatic stress symptoms: A three month prospective study. American Journal of Psychiatry. 2003;160:1337–1339. doi: 10.1176/appi.ajp.160.7.1337. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. doi: 10.1016/j.beth.2011.03.007. (in press) [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP. The importance of the peritraumatic experience in defining traumatic stress. Psychological Bulletin. doi: 10.1037/a0021353. (in press) [DOI] [PubMed] [Google Scholar]
- Breh DC, Seidler GH. Is peritraumatic dissociation a risk factor for PTSD? Journal of Trauma and Dissociation. 2007;8:53–69. doi: 10.1300/J229v08n01_04. [DOI] [PubMed] [Google Scholar]
- Bremner JD. Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10:37–49. doi: 10.1023/a:1024804312978. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick S, Brett E, Fontana A, Rosenheck R, Charney DS. Dissociation and posttraumatic stress disorder in Vietnam combat veterans. American Journal of Psychiatry. 1992;149:328–332. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- Briere J, Scott C, Weathers F. Peritraumatic and persistent dissociation in the presumed etiology of PTSD. American Journal of Psychiatry. 2005;162:2295–2301. doi: 10.1176/appi.ajp.162.12.2295. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, Saunders BE. Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Brooks R, Bryant RA, Silove D, Creamer M, O’Donnell M, McFarlane AC, Marmar CR. The latent structure of the peritraumatic dissociative experiences questionnaire. Journal of Traumatic Stress. 2009;22:153–157. doi: 10.1002/jts.20414. [DOI] [PubMed] [Google Scholar]
- Bryant RA. Does dissociation further our understanding of PTSD? Journal of Anxiety Disorders. 2007;21:183–191. doi: 10.1016/j.janxdis.2006.09.012. [DOI] [PubMed] [Google Scholar]
- Candel I, Merckelbach H. Peritraumatic dissociation as a predictor of post-traumatic stress disorder: A critical review. Comprehensive Psychiatry. 2004;45:44–50. doi: 10.1016/j.comppsych.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Fikretoglu D, Brunet A, Best SR, Metzler TJ, Delucchi K, Weiss DS, Marmar CR. Peritraumatic fear, helplessness and horror and peritraumatic dissociation: Do physical and cognitive symptoms of panic mediate the relationship between the two? Behaviour Research and Therapy. 2007;45:39–47. doi: 10.1016/j.brat.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: A critical review. Annual Review of Psychology. 1997;48:449–480. doi: 10.1146/annurev.psych.48.1.449. [DOI] [PubMed] [Google Scholar]
- Foa EB, Molnar C, Cashman L. Change in rape narratives during exposure therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 1995;8:675–690. doi: 10.1007/BF02102894. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS. Post-traumatic stress disorder in rape victims. In: Oldham J, Riba MB, Tasman A, editors. American Psychiatric Press review of psychiatry, Vol. 12. Washington, DC: American Psychiatric Association Press; 1993. pp. 273–303. [Google Scholar]
- Friedman M. What might the psychobiology of posttraumatic stress disorder teach us about future approaches to pharmacotherapy? Journal of Clinical Psychiatry. 2000;91:44–51. [PubMed] [Google Scholar]
- Halligan SL, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of Consulting and Clinical Psychology. 2003;71:419–431. doi: 10.1037/0022-006x.71.3.419. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Bryant RA. Dissociative symptoms in acute stress disorder. Journal of Traumatic Stress. 1999;12:673–680. doi: 10.1023/A:1024773202939. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Wilson KG, Gilford EV, Follette VM, Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ. Stress response syndromes. 2nd ed. Northvale, NJ: Jason Aronson; 1986. [Google Scholar]
- Kashdan TB, Barrios V, Forsyth JP, Steger MF. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behaviour Research and Therapy. 2006;44:1301–1320. doi: 10.1016/j.brat.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Acierno R. Should PTSD criterion A be retained? Journal of Traumatic Stress. 2009;22:374–383. doi: 10.1002/jts.20436. [DOI] [PubMed] [Google Scholar]
- King D, Leskin G, King L, Weathers F. Confirmatory factor analysis of the clinician administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Koss MP, Figueredo AJ, Bell I, Tharan M, Tromp S. Traumatic memory characteristics: A cross-validated mediational model of response to rape among employed women. Journal of Abnormal Psychology. 1996;105:421–432. doi: 10.1037//0021-843x.105.3.421. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Kelly MP. Validation of a brief measure of posttraumatic stress disorder: The Distressing Events Questionnaire (DEQ) Psychological Assessment. 2000;12:197–209. doi: 10.1037//1040-3590.12.2.197. [DOI] [PubMed] [Google Scholar]
- Lensvelt-Mulders G, van der Hart O, van Ochten JM, van Son MJM, Steele K, Breeman L. Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clinical Psychology Review. 2008;28:1138–1151. doi: 10.1016/j.cpr.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Littleton HL, Axsom D, Grills-Taquechel AE. Adjustment following the mass shooting at Virginia Tech: The roles of resource loss and gain. Psychological Trauma: Theory, Research, Practice, and Policy. 2009;1:206–219. doi: 10.1037/a0025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmar CR, Metzler TJ, Otte C. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. 2nd ed. New York: Guilford Press; 2004. pp. 144–167. [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. Peritraumatic dissociation and posttraumatic stress disorder. In: Bremner JD, Marmar CR, editors. Trauma, memory, and dissociation. Washington, DC: American Psychiatric Press; 1998. pp. 229–252. [Google Scholar]
- Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL. Peritraumatic dissociation and posttraumatic stress disorder in male Vietnam theater veterans. American Journal of Psychiatry. 1994;151:902–907. doi: 10.1176/ajp.151.6.902. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL. Reappraising the link between peritraumatic dissociation and PTSD symptom severity: Evidence from a longitudinal study of community violence survivors. Journal of Abnormal Psychology. 2002;111:626–636. doi: 10.1037//0021-843x.111.4.626. [DOI] [PubMed] [Google Scholar]
- Marx BP, Sloan DM. The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behavior Therapy. 2002;33:563–578. [Google Scholar]
- Marx BP, Sloan DM. Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy. 2005;43:569–583. doi: 10.1016/j.brat.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Moleman N, van der Hart O, van der Kolk BA. Dissociation and hypnotizability in posttraumatic stress disorder. Journal of Nervous and Mental Disease. 1992;180:271–272. doi: 10.1097/00005053-199204000-00010. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus User’s Guide. Fifth Edition. Los Angeles, CA: Muthen & Muthen; 1998–2009. [Google Scholar]
- Norris F, Foster J, Weisshaar D. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Oimette P, Wolfe J, editors. Gender and PTSD. New York: Guilford Press; 2002. pp. 3–42. [Google Scholar]
- North CS, Smith EM, Spitznagel EL. Posttraumatic stress disorder in survivors of a mass shooting. American Journal of Psychiatry. 1994;151:82–88. doi: 10.1176/ajp.151.1.82. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SS, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Follette VM. Long-term correlates of child sexual abuse: Theory and review of the empirical literature. Applied and Preventive Psychology. 1995;4:143–166. [Google Scholar]
- Ruscio AM, Ruscio J, Keane TM. The latent structure of posttraumatic stress disorder: A taxometric investigation of reactions to extreme stress. Journal of Abnormal Psychology. 2002;111:290–301. [PubMed] [Google Scholar]
- Schwarz ED, Kowalski JM. Posttraumatic stress disorder after a school shooting: Effects of symptom threshold selection and diagnosis by DSM-III, DSM-III-R, or proposed DSM-IV. American Journal of Psychiatry. 1991;148:592–597. doi: 10.1176/ajp.148.5.592. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf war. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Spiegel D. Dissociation and trauma. In: Tasman A, Goldfinger SM, editors. Annual review of psychiatry, Vol. 10. Washington, DC: American Psychiatric Press; 1991. pp. 261–275. [Google Scholar]
- Sterlini GL, Bryant RA. Hyperarousal and dissociation: A study of novice skydivers. Behavioral Research and Therapy. 2002;40:431–437. doi: 10.1016/s0005-7967(01)00021-3. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tull MT, Roemer L. Alternative explanations of emotional numbing of posttraumatic stress disorder: An examination of hyperarousal and experiential avoidance. Journal of Psychopathology and Behavioral Assessment. 2003;25:147–154. [Google Scholar]
- van der Kolk BA, Fisler R. Dissociation and the fragmentary nature of traumatic memories: Overview and exploratory study. Journal of Traumatic Stress. 1995;8:505–525. doi: 10.1007/BF02102887. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA, van der Hart O, Marmar CR. Dissociation and information processing in posttraumatic stress disorder. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic stress. New York: Guilford Press; 1996. pp. 303–330. [Google Scholar]
- van der Velden PG, Kleber RJ, Christiaanse B, Gersons BP, Marcelissen FG, Drogendijk AN, Meewisse ML. The independent predictive value of peritraumatic dissociation for postdisaster intrusions, avoidance reactions, and PTSD symptom severity: A 4-year prospective study. Journal of Traumatic Stress. 2006;19:493–506. doi: 10.1002/jts.20140. [DOI] [PubMed] [Google Scholar]
- van der Velden PG, Wittmann L. The independent predictive value of peritraumatic dissociation for PTSD symptomatology after type I trauma: A systematic review of prospective studies. Clinical Psychology Review. 2008;28:1009–1020. doi: 10.1016/j.cpr.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Vogt DS, King DW, King DW. Risk pathways for PTSD: Making sense of the literature. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 99–115. [Google Scholar]
- Wagner AW, Linehan MM. Dissociative behavior. In: Follette VM, Ruzek JI, Abueg FR, editors. Cognitive-behavioral therapies for trauma. New York: Guilford Press; 1998. pp. 191–225. [Google Scholar]
- Wittmann L, Moergeli H, Schnyder U. Low predictive power of peritraumatic dissociation for PTSD symptoms in accident survivors. Journal of Traumatic Stress. 2006;19:639–651. doi: 10.1002/jts.20154. [DOI] [PubMed] [Google Scholar]
- Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology. 2010;119:764–776. doi: 10.1037/a0020981. [DOI] [PMC free article] [PubMed] [Google Scholar]