Abstract
Background. People with stroke are not maintaining adequate engagement in physical activity (PA) for health and functional benefit. This paper sought to describe any psychological and social factors that may influence physical activity engagement after stroke. Methods. A structured literature review of studies indexed in MEDLINE, CinAHL, P&BSC, and PsycINFO using search terms relevant to stroke, physical disabilities, and PA. Publications reporting empirical findings (quantitative or qualitative) regarding psychological and/or social factors were included. Results. Twenty studies from 19 publications (9 surveys, 1 RCT, and 10 qualitative studies) were included. Seventeen studies reported findings pertinent to psychological factors and fourteen findings pertinent to social factors. Conclusion. Self-efficacy, physical activity beliefs, and social support appear particularly relevant to physical activity behaviour after stroke and should be included in theoretically based physical interventions. The Transtheoretical Model and the Theory of Planned Behaviour are candidate behavioural models that may support intervention development.
1. Introduction
Long-term engagement in physical activity (PA) after stroke is increasingly being recognised as important for maintaining functional gains after rehabilitation and for general health benefits such as prevention of stroke recurrence and obesity, diabetes, and coronary heart disease. There is now a substantial body of work to demonstrate the effectiveness of regular PA on fitness and health parameters in this population [1]. However, it is also vitally important that clinicians, health promotion professionals, exercise instructors, and others involved in stroke care after rehabilitation understand the determinants of PA in this often elderly and frequently disabled population. Understanding these factors will allow development of appropriately targeted effective interventions that are contextually appropriate for increasing the uptake and maintenance of PA in this typically sedentary population.
A number of recent randomised controlled trials and systematic reviews [1–9] have demonstrated significant benefits of PA on a range of physical and functional parameters including muscle strength, gait, balance, function, and general fitness. Engaging in PA has also been shown to positively influence psychosocial outcomes such as quality of life and confidence [10]. This evidence is recognised by clinical guidelines which recommend long-term participation in PA after stroke because of its potential impact in reducing risk of cardiac events, diabetes depression, obesity, and recurrent stroke [11, 12]. Thus there is an evidence-based consensus that after stroke people should engage in long-term PA behaviour as part of, and as followup to, rehabilitation.
Despite the robust evidence regarding the many benefits of PA, people with stroke are not maintaining adequate long-term levels of engagement in PA for health and functional benefit. Many survivors adopt or return to sedentary lifestyles after rehabilitation [13] with between 58% and 68% of individuals with stroke undertaking minimal postrehabilitation PA [14, 15]. Furthermore, studies show that even where physical and functional improvements from organised programmes are significant, benefits are typically lost at followup [5, 16]. This suggests that survivors are either choosing not to undertake self-directed PA or are encountering barriers that prevent them from engaging in activity. In order to support people with stroke to start or return to be physically active and to maintain engagement in PA, it is important that factors influencing uptake and long-term maintenance in PA in this population are fully understood. However, the determinants of PA behaviour are complex, and are known to be influenced by interlinked psychosocial, personal, and environmental factors [17, 18]. A starting point to understand and explain the role of these interlinked concepts is therefore to examine the psychosocial factors that might influence uptake and maintenance PA after stroke.
One approach to understanding the role of factors that may influence PA is the application of health behaviour models to explain the importance and relationship of such factors. Social cognition models of health behaviour and their component theoretical constructs, for example, have been applied at the level of the individual, to explain PA behaviour [17–19]. Theories such as Social Cognitive Theory [20] the Transtheoretical Model [21], Self-Determination Theory [22], and the Theory of Planned Behaviour [23] are models that currently dominate the PA behaviour change literature [17]. These models incorporate a range of potentially modifiable cognitive constructs believed to influence behaviour [17, 24, 25]. Some of the most important of these for PA behaviour in general appear to be attitudinal beliefs which evaluate the positive and negative aspects of the behaviour. Expected outcome and self-efficacy beliefs, and perceived competence, as well as perceived behavioural control relate to confidence in one's ability to perform the behaviour and are important determinants of PA behaviour [17, 18, 24, 25]. Other important constructs involve intention to undertake the behaviour, which incorporates setting goals and committing to the behaviour through use of self-regulatory skills [17, 18, 21, 24]. Prestroke exercise history may influence these beliefs and cognitions and should also be examined as a determinant of PA after stroke [26].
Understanding the role of psychological constructs in relation to PA behaviour after stroke is clearly important if effective interventions are to be developed to support long-term engagement in PA in this population.
The psychological literature from the general population also suggests that social constructs are important in determining PA, and these factors may apply after stroke [18]. Social normative beliefs relate to beliefs of others about one's engagement in PA, vicarious beliefs about others who are engaging in the behaviour [20]. More pragmatically, and moving away from an individualistic to a social model of behaviour, socioenvironmental factors may influence PA behaviour. Support from family and friends appears important in influencing motivation for PA in adults, and group exercise is known to be important in influencing motivation [18, 26]. Furthermore, sociodemographic factors such as ethnicity, gender, education, income, and age may also be influential in determining likely engagement in PA [26, 27]. Given the evidence from the general population that social environment may influence uptake and maintenance of PA, it is clearly important to also examine what is known about these factors in relation to stroke if interventions to address the psychosocial complexities of PA behaviour are to be appropriately developed and applied.
The purpose of this structured review of the existing empirical data was to find and describe the role of psychological and social factors in influencing uptake and maintenance of PA engagement after stroke. Given the potential for health behaviour models to account for and explain the relative role of such factors, it was important to consider if data existed within the literature concerning these models. We used three clinically relevant questions to guide and structure our review. (1) What is the role of psychological factors in influencing the uptake and/or maintenance of PA after stroke? (2) What is the role of social factors in influencing the uptake and/or maintenance of PA after stroke? (3) Within the literature that explores the role of psychosocial factors in the uptake and/or maintenance of PA after stroke, which health behaviour models have been investigated?
2. Methods
We conducted a structured review of the literature. Relevant primary and secondary literature was identified by searching four online electronic databases via the EBSCO Host platform (Medline, CinAHL, Psychology and Behavioural Sciences Collection (P&BSC), and PsycINFO).
Search terms included relevant subject headings related to physical disabilities with mobility impairment or stroke (the presence of the word stroke in the title and abstract of a publication were also searched for). This search string was combined, using the Boolean operator “AND” with subject headings relevant to PA or exercise (see Table 1).
Table 1.
Search terms used and databases searched.
| Search architecture | |
|---|---|
| (1) | (MH “Stroke”) or (MH “Arthritis+”) or (MH “Cerebral Palsy”) or (MH “Multiple Sclerosis”) or (MH “Muscular Dystrophy+”) or (MH “Muscular Dystrophies+”) or (MH “Parkinson Disease”) |
| (2) | TI stroke or AB stroke |
| (3) | 1 or 2 |
| (4) | (MH “PA”) or (MH “Exercise+”) or (MH “Physical Mobility”) or (MM “PA”) OR (MM “Exercise”) |
| (5) | 3 and 4 |
Databases searched: Medline; Cumulative Index to Nursing and Allied Health Literature (CinAHL); Psychology and Behavioural Sciences Collection (PBSC); PsycINFO.
Publications were limited to the English language only. No other limits or filters were applied. Identified publications were scrutinised independently by two members of the study team, and a decision made as to whether or not publications should be included or excluded was made according to criteria reported in Table 2.
Table 2.
Criteria for including and excluding publications in the review.
| Criteria | |
|---|---|
| Include if publication | (i) included participants with diagnosed stroke |
| (ii) focuses on psychological or social factors | |
| (iii) focuses on issues pertinent to the uptake of or maintenance of PA/exercise after stroke | |
| (iv) reports empirical data whether quantitative (e.g., RCT, survey, cohort, case-control, interrupted time series) or qualitative (e.g., in-depth interview, focus group, and ethnography) | |
| (v) reports primary or secondary derived data | |
| Exclude if publication | (i) does not include a sufficient focus on people with stroke |
| (ii) is not primarily focused on PA or exercise after stroke | |
| (iii) does not report data pertinent to understanding psychological or social factors | |
| (iv) is not empirical | |
Publications assessed as meeting all inclusion criteria were retrieved in full. Two members of the research team independently examined full-text copies of all selected papers. Consensus was reached by consultation with the rest of the team. All publications included in the review were then categorised based on methodology. Data were extracted regarding (1) the methods used; (2) the primary study aims; (3) key findings specifically related to the review research questions.
The included studies were assessed for methodological quality according to individual elements of quality rather than a summary scale approach. For the assessment of quantitative studies (e.g., randomized controlled trials) the use of such summary scales is not supported by empirical evidence [28] and is actively discouraged [29]. Methodological components assessed for RCTs were randomisation, blinding, allocation concealment, and whether or not there had been an intention to treat analysis. Components for surveys were sampling strategy, response rate, use of validated instruments, and appropriate statistical testing.
Assessing the methodological quality of qualitative studies using composite scales has also been hotly debated and contested [30]. We therefore performed a global assessment of study quality, dichotomised according to whether it appears to be strong or weak. Strong studies are likely to include triangulation of data, respondent validation, clear exposition of methods of data collection and analysis, and reflexivity. We also considered the nature of the evidence reported in the qualitative studies and assessed these in terms of the “typologies” of their findings as described by Sandelowski and Barroso [31]. According to Sandelowski, the findings of qualitative studies in the health domain can be classified on a continuum of data transformation from findings that are not qualitative (no finding, topical survey), to ones that are exploratory (thematic survey), descriptive (conceptual/thematic description), or explanatory (interpretive explanation).
3. Results
Of the 1,470 publications returned from the search strategy, 1,426 were excluded following screening of the title and abstract (see Figure 1). 46 publications were retrieved and reviewed in full. A further 27 were excluded (see Table 3 for reasons) leaving 19 publications, which met inclusion criteria (see Table 4). Two publications [32, 33] reported a qualitative and a quantitative study. The quantitative study reported in Maher et al. [32] was quasiexperimental and did not report outcome data so was excluded. The studies reported in the paper by Galvin et al. [33] did meet inclusion criteria thus were both included. Thus from 19 publications included, 20 studies met all inclusion. 1 study was a randomized controlled trial (RCT), 9 were surveys, and 1 was qualitative (see Table 4).
Figure 1.
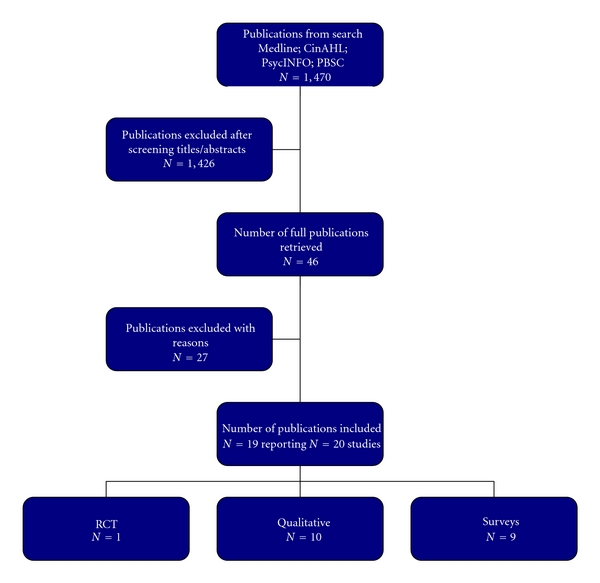
Flow diagram of publications found and included or excluded.
Table 3.
Excluded publications with reasons for exclusion by publication/study type.
| Publication | Reason for exclusion | |||
|---|---|---|---|---|
| No stroke population focus | No focus on psychosocial factors | No focus on maintenance or uptake of exercise | Not empirical | |
| Surveys | ||||
| Bohannon 2004 | — | √ | √ | — |
| Cliodhna 2007 | — | — | √ | — |
| Junker 2011 | √ | — | — | — |
| Michael 2006 | — | — | √ | — |
| Bonetti 2008 | — | — | √ | — |
| Cohort | ||||
| Molloy 2008 | — | — | √ | — |
| CT/RCTs | ||||
| Boysen 2009a | — | √ | √ | — |
| Coyle 1995 | √ | — | √ | — |
| Gillham 2010 | — | √ | — | — |
| Harrington 2010 | — | √ | — | — |
| Huijbregts 2008 | — | — | √ | — |
| Langhammer 2008 | — | √ | √ | — |
| Marsden 2010 | — | √ | √ | — |
| McLellan 2004 | — | √ | √ | — |
| Michael 2009 | — | √ | √ | — |
| Patterson 2010 | — | √ | √ | — |
| Stuart 2009 | — | √ | √ | — |
| van der Ploeg 2006 | — | √ | √ | — |
| Qualitative | ||||
| Pound 1999 | — | — | √ | — |
| Commentaries/reviews/ recommendations/letters |
||||
| Ada 2006 | — | √ | — | √ |
| Blennerhassett 2008 | — | √ | — | √ |
| Boysen 2009b | — | √ | √ | √ |
| Gordon 2004 | — | — | √ | √ |
| Lawrence 2009 | — | √ | √ | √ |
| Mead 2009 | — | √ | — | √ |
| Morris 2009 | — | √ | — | √ |
| Shaughnessy 2009 | — | — | — | √ |
CT: controlled trial; RCT: randomized controlled trial.
Table 4.
Summary of included studies.
| Study (first author) | Year | Country of study | Study type |
Participants (time since stroke) |
Ethnicity | Reports data pertinent to | |
|---|---|---|---|---|---|---|---|
| psychological factors | social factors | ||||||
| Kinne | 1999 | USA | Survey | Not reported | 91% Caucasian; 3% African American; 3% Asian American; 1% Hispanic |
√ | — |
| Johnston | 1999 | UK | Survey | 10 days–6 months | Not reported | √ | — |
| Cardinal | 2004 | USA | Survey | Not reported | 91.9% Caucasian | √ | — |
| Shaughnessy | 2006 | USA | Survey | 60.2 months | 70% Caucasian; 22% African American; 7% other |
√ | √ |
| Nosek | 2006 | USA | Survey | Not reported | 80.8% Caucasian; 9.6% African American; 6.0% Hispanic |
√ | √ |
| Resnick | 2007 | USA | Survey | Not reported | 57% Caucasian | √ | — |
| Barker | 2007 | Australia | Survey | 4.9 years | 98% nonindigenous; 2% indigenous |
√ | — |
| Rimmer | 2008 | USA | Survey | Not reported | 9% Caucasian; 80% African American; 10% Hispanic |
√ | √ |
| Galvin | 2009 | Ireland | Survey | Not reported | Not reported | — | √ |
| Boysen | 2009 | Denmark/Poland/ China/Estonia |
RCT | <90 days | Not reported | — | √ |
| Maher | 1999 | USA | Qualitative | Not reported | Not reported | √ | √ |
| Barker | 2005 | Australia | Qualitative | Mean 4.9 yrs | Not reported | √ | √ |
| Damush | 2007 | USA | Qualitative | <12 months | 85% African American, 15% white |
√ | √ |
| Wiles | 2008 | UK | Qualitative | Not reported | Not reported | √ | √ |
| Resnick | 2008 | USA | Qualitative | 6 months+ | 47% black, 48% white, 5% mixed, Hispanic or Asian-Pacific |
√ | √ |
| Graham | 2008 | Canada/N. Ireland | Qualitative | Not reported | Not reported | √ | √ |
| Reed | 2009 | UK | Qualitative | 15–40 months | Not reported | √ | √ |
| Carin-Levy | 2009 | UK | Qualitative | Not reported | Not reported | √ | √ |
| Galvin | 2009 | Ireland | Qualitative | Not reported | Not reported | — | √ |
| Patterson | 2009 | Australia | Qualitative | Not reported | Not reported | √ | √ |
4. Overview of the Studies
The overview contains design, setting, participants, interventions, measures, types and reported levels of PA reported, and methodological quality.
5. Design
5.1. Quantitative Studies
There were eight cross-sectional surveys [14, 33–39] and one longitudinal survey [40]. The only RCT was an international multicentre trial [41].
5.2. Qualitative Studies
Two qualitative studies involved focus groups only [33, 42], three conducted face-to-face or telephone interviews [10, 32, 43], and three conducted focus groups an interviews [44–46]. One study [47] produced longitudinal case studies.
6. Setting
Study setting is reported in Table 4.
7. Participants
Details of participant age, time since stroke, and proportion of participants with stroke in quantitative and qualitative studies are reported in Table 4.
7.1. Quantitative Studies
Most participants were community dwelling, however, two studies [33, 40] recruited hospital inpatients. One study [40], had followup at one and six months after hospital discharge. The RCT recruited participants 90 days after stroke onset with followup at 3 monthly intervals then at 18 and 24 months [41].
Most surveys included only people with stroke, however, three involved mixed disabled populations (Table 4). Mean reported age ranged from 47.1 years [36] to 69.4 years [40]. Time since stroke onset ranged from 10 days [40] to 5.2 years [14] most studies did not report this [33–38].
7.2. Qualitative Studies
Most participants were community dwelling. One study [33] involved inpatients receiving physiotherapy. Seven studies included only people with stroke; however, two [32, 47] interviewed mixed disabled populations (Table 4).
8. Interventions
The RCT included an intervention to increase PA [41] which involved repeated encouragement and verbal instruction about PA from a physiotherapist.
9. Measures
Several surveys used measures developed by the researchers to assess family involvement in exercise [33] self-efficacy, social support for PA [36], and exercise coping [40]. Other surveys used standardised tests to assess barriers to PA [34], barriers to health activities among disabled populations [38, 39], self-efficacy and outcome expectancy [14, 35, 37, 38], and locus of control [39, 40].
Where they were assessed, PA levels were measured using self-report. For the RCT, the primary outcome measure was the PA Scale for the Elderly [41], the Yale PA Survey was also used [35], and another study used measures developed by study researchers [36]. No study measured PA levels using pedometers or accelerometers.
10. Types of PA
10.1. Quantitative Studies
Types of PA ranged from passive exercise to aerobic exercise [36]; any type of PA aimed at improving a particular skill or ability [33]; type of PA defined by the Yale PA Survey [35]; walking, jogging, swimming, biking, rowing, wheelchair racing, off-road pushing arm-cranking, and so forth [37]; PA of at least 20 minutes duration that caused sweating or increases in respiratory of heart rate [14] and items included in the Physical Activities Scale for the Elderly [41]. Barker examined exercise for the upper limb [39]. Some surveys did not define the type of PA [34, 38, 40].
10.2. Qualitative Studies
Qualitative studies examined views and perceptions of people with stroke in relation to engagement in various physical activities including a seated exercise class [47], treadmill walking [45] exercise on prescription [46], and a conditioning class [32]. Engagement in upper limb exercise [44], exercise and physiotherapy [33], PA in general [42], and exercise versus relaxation classes [10] were also examined. One study did not define type of PA [43].
11. Reported Levels of PA
11.1. Quantitative Studies
The proportion of participants undertaking regular PA varied between 31% reporting regular PA for six months or more [38] to 68% of participants undertaking an unspecified amount of PA since their stroke [34]. One study [34] reported that 32% of participants had stopped PA since their stroke whilst another [14] reported that 27% undertook no PA since the stroke—an increase of 12% from Prestroke levels.
11.2. Qualitative Studies
No qualitative studies reported level of PA undertaken by participants.
12. Methodological Quality
Survey quality was good overall (Tables 5 and 6); however, four [33–35, 38] demonstrated sampling strategies with low likelihood of generalisability, due to convenience sampling. All but one study [33] used previously validated measures. Qualitative studies were more varied in quality. All except one [46] were either topical surveys or thematic analyses without sufficient analytical depth to develop conceptual themes or interpretive explanation. Therefore whilst the studies reflected emerging themes, their interpretive contribution towards development of theories that might facilitate new understandings about PA engagement after stroke was limited.
Table 5.
Methodological quality assessment of the 10 quantitative studies included.
| Study | Methodological element | |||
|---|---|---|---|---|
| Surveys | Sampling strategy indicates likelihood of generalizability | Reported good response rate (60%+) | Use of validated instruments | Appropriate statistical testing |
| Barker et al. [39] | √ | Not stated | √ | √ |
| Cardinal et al. [37] | √ | √ | √ | √ |
| Galvin et al. [33] | × | √ | × | × |
| Johnston et al. [40] | √ | √ | √ | √ |
| Kinne et al. [38] | × | √ | √ | √ |
| Nosek et al. [36] | √ | √ | √ | √ |
| Resnick et al. [35] | × | √ | √ | √ |
| Rimmer et al. [34] | × | × | √ | √ |
| Shaughnessy et al. [14] | √ | × | √ | √ |
| RCT | Adequate allocation concealment | Adequate randomisation | Adequate blinding | Intention to treat analysis |
| Boysen et al. [41] | √ | √ | √ | √ |
Table 6.
Global assessment of study quality and typologies of study findings of the 10 qualitative studies included.
| Study | Typology of study findings | |||||
|---|---|---|---|---|---|---|
| Qualitative studies | Global assessment of study quality | No findings | Topical survey | Thematic survey | Conceptual thematic description | Interpretive explanation |
| Barker and Brauer [44] | Strong | — | — | √ | — | — |
| Carin-Levy et al. [10] | Strong | — | — | √ | — | — |
| Maher et al. [32] | Strong | — | — | √ | — | — |
| Reed et al. [43] | Strong | — | — | — | √ | — |
| Wiles et al. [46] | Strong | — | — | √ | — | — |
| Damush et al. [42] | Weak | — | — | √ | — | — |
| Galvin et al. [33] | Weak | — | √ | — | — | — |
| Graham et al. [47] | Weak | — | — | √ | — | — |
| Patterson and Ross-Edwards [48] | Weak | — | — | √ | — | — |
| Resnick et al. [45] | Weak | — | — | √ | — | — |
13. Findings from the Included Studies
Detailed information of findings from the quantitative and qualitative studies is provided in the appendix.
Seventeen studies (8 surveys and 9 qualitative studies) reported findings pertinent to the role of psychological factors. Fourteen studies (all qualitative studies, the RCT and 3 surveys) reported findings pertinent to the role of social factors. Table 7 lists the range of psychological and social factors.
Table 7.
Psychological and social factors for which findings exist.
| Psychological factors | Social factors |
|---|---|
| Self-efficacy | The role of family and friends in supporting PA after stroke |
| Locus of control | The role of health professionals |
| Competence to be physically active | The role of exercise professionals |
| Beliefs about the nature of PA | The role of other people with stroke and disability |
| Motivational barriers to becoming or remaining physically active | Group exercise |
| Self-determination as a facilitator to becoming and remaining physically active | |
| Beliefs about positive and negative outcomes of being physically active |
Findings from included studies are tabulated in the appendix and summarized in the following section, starting with the psychological factors.
14. The Importance and Role of Psychological Factors
Eight surveys reported data pertinent to understanding the role of psychological factors in the uptake and maintenance of exercise after stroke.
14.1. Self-Efficacy
Four surveys found that self-efficacy for PA, which can be described as appraisal of confidence or capability to perform PA, predicted greater involvement in PA [14, 36] or maintenance of exercise behaviour [37, 38]. Another study [39] demonstrated that confidence to do what needs to be done and helpful information from own efforts were important for self-directed physical activity. Self-efficacy beliefs also varied with activity type [36], with perceived efficacy higher for gentle flexibility than for aerobic exercise. Only one study found that self-efficacy and self-reported exercise levels were not associated [35].
In the qualitative studies, physical impairments after stroke reduced confidence to engage in PA [42, 43]. Stroke led to loss of role and purpose, and unwillingness to participate outside a perceived safe environment [43]. Feeling vulnerable caused anxiety about attending an exercise class [10]. For participants overcoming that barrier, worries about difficulty with speech and social interaction [10] and negative attitudes from others created desire to give up [44].
14.2. Locus of Control
Related to the construct of self-efficacy, greater perceived locus of control for recovery was predictive of recovery in two surveys [39, 40]. However in one study [40] frequency of exercise at one month after hospital discharge was not correlated significantly with perceived control, suggesting that engagement in exercise was not the coping mechanism by which perceived control improved disability. Furthermore, the relationship between perceived control and disability existed only at one month after hospital discharge, and was not apparent at six months. No study directly examined the role of perceived control on exercise behaviour.
14.3. Competence to Be Physically Active
Beliefs about competence to exercise influenced behaviour. Not knowing how or where to exercise, and beliefs that exercise was too difficult were barriers to PA [34, 38].
In the qualitative literature, focusing on physical limitations, making unfavourable comparisons with previous health and function, coupled with negative comparison to others affected perceived competence to engage in PA [47]. Feeling ill-equipped to engage in PA owing to physical impairments and associated cognitive impairments led to difficulty understanding and remembering information on how to competently engage in PA [42–44]. Furthermore, previous negative experiences leading to repeated failures and frustrations were overwhelming and limited trying [44].
14.4. Beliefs about the Nature of PA
One survey [34] found that lack of interest in exercise and beliefs that it was boring were barriers to PA engagement.
In the qualitative studies, PA was viewed as a meaningful activity and a way to fill time. Having someplace to go and something to do created a sense of purpose [42]. Engaging in regular PA brought structure and routine, all of which encouraged adherence [10, 45]. In contrast, negative attitudes towards PA were also evident. Age limited the amount and type of PA deemed appropriate [42]. PA was considered formal and planned, and not something that could be incorporated into daily life. Leisure time PA such as walking and gardening were not classed as PA [42]. Furthermore, gains from engaging in organised PA were not maintained at home because individuals felt that they had learnt all there was to learn [10].
14.5. Motivational Barriers to Becoming or Remaining Physically Active
Higher perceived motivational barriers were associated with lower levels of PA [37, 38]. Lack of motivation, perceptions of being too lazy, and being tired were barriers to uptake or maintenance of PA [34, 38]. A study of the transtheoretical model [37], also known as the stage of change model, reported different behavioural processes at different stages of behaviour change. Behavioural processes to support the behaviour, such as laying out exercise clothes and sharing intention to be active with others for support were apparent when people were beginning to be active, but were less prevalent in people who maintained PA over a long period. Similarly, cognitive processes such as evaluating and monitoring progress and making oneself consciously aware of the commitment to be active were less prevalent in people who maintained PA over a long period.
Similar motivational barriers were evident in the qualitative studies. Lack of energy and fatigue limited motivation to be physically active [42], and low mood and feelings of depression led to no hope of recovery and reduced motivation to engage [44].
14.6. Self-Determination as a Facilitator to Becoming and Remaining Physically Active
Self-determination, a feeling of “having to do it oneself” was examined in the qualitative studies. It resulted in a “can do” attitude and pushed individuals to engage in PA [32, 42, 44, 45]. Negative attitudes from others acted as a motivator to “prove them wrong” and to push the boundaries of what is achievable, despite physical impairments [44, 47].
14.7. Beliefs about Positive and Negative Outcomes of Being Physically Active
Two surveys demonstrated that belief in positive outcomes of PA predicted increased engagement in PA. In one study [14], advice from a physician enhanced outcome expectations, and positively influenced PA behaviour. Similarly, one study examining the decisions that people made about being active demonstrated that perceived benefits about exercise became greater and perceived disadvantages became lower as people became more active and maintained PA behaviour over a long period [37].
Conversely, beliefs in negative outcomes of PA also potentially influenced engagement. One study showed that health concerns prevented 28% of participants from engaging in PA and also that 36% of participants believed that exercise would not improve their condition [34].
Beliefs around the outcomes of PA were also evident in the qualitative studies. Feeling physically stronger, walking better, improved balance, and less falling were recognised as benefits of PA and acted as motivators to continue [45]. Stroke survivors saw being physically active as essential for recovery and a way to improve fitness and health [43, 44, 46, 47]. Being physically active was seen as an alternative to physiotherapy, although more physiotherapy was the preferred option [43, 44].
With regards to affective outcome expectations [17], fear of falling, pain, failure, stroke recurrence, and worries about doing the wrong thing or being embarrassed were seen as negative outcomes of PA and acted as barriers to engaging [10, 32, 44]. However, PA was also seen as being fun and enjoyable, and as a way to help ease feelings of depression, and increase energy levels [10, 43, 47]. Being physically active eased anxiety, built confidence, increased self-esteem, and offered a sense of achievement and pride [10, 32, 43]. This had a cumulative effect as improved confidence and higher self-esteem negated fears [43] and motivated individuals to engage in new activities both within the exercise setting, but also in achieving goals within the wider context of their life [32, 47, 48].
15. The Importance and Role of Social Factors
15.1. The Role of Family and Friends in Supporting PA after Stroke
The study by Galvin et al. [33] focused on the role of the family in exercise after stroke. The study was methodologically weak but demonstrated that 91% of participants with stroke agreed that a family member or friend had a role in their exercises after stroke. 91% of family or friends reported willingness to assist in physiotherapy and 85% to assist in more complex exercises involving walking and transfers. A small proportion of the participants with stroke indicated that they felt that this was not the role of their family or friends, and they did not feel confident in their capacity to assist or felt that family or friends would put them under too much pressure.
Differing views regarding the role of family and friends in supporting PA were also evident in the qualitative studies. For some stroke survivors, family and friends were central to recovery, and their support and encouragement motivated engagement in PA [44, 45]. Others, who lived on their own, felt being alone forced them to be more independent and to do more for themselves [44].
15.2. The Role of Health Professionals
Barker reported that lack of help from health professionals was negatively associated with uptake or maintenance of activity. Shaughnessy et al. [14] concurred with that finding, demonstrating that recommendations to exercise predicted higher levels of activity. In contrast, in the RCT, repeated instructions from a physiotherapist to be physically active did not increasing PA levels more than information about possible benefits of PA [41]. One survey reported that having a personal assistant was important for PA [36]. Cardinal et al. [37] also reported that helping relationships were predictive of stage of change for PA.
In the qualitative studies, physiotherapists were perceived as central to recovery after stroke, and therapy was considered essential to improving physical function and maintaining progress. Physiotherapy exercises were seen as a way to maintain PA levels, within rehabilitation and community settings [42, 44, 46, 48]. Physiotherapists were also seen as important for emotional support. Stroke survivors sought continued access to physiotherapists when engaging in PA in community settings, for guidance and reassurance [46, 48]. However, although support from physiotherapists was highly valued, it was acknowledged that they offered little information on self-directed exercise, and that they should place more emphasis on teaching stroke survivors how to exercise independently [44].
Stroke survivors in one study [44] felt supported by physicians, and followed their advice to engage in PA. In contrast, stroke survivors in another [42] experienced negative attitudes from health professionals regarding their physical recovery. This acted as a motivator to engage in PA to “prove them wrong.”
15.3. The Role of Exercise Professionals
In the qualitative studies, exercise professionals were seen to play an important role in teaching stroke survivors how to exercise independently [43]. Their presence increased feelings of safety, and their verbal encouragement and support led to improved confidence and increased self-efficacy [45]. Some concerns emerged about the level of support they could offer. Survivors were concerned about lack of monitoring and being “left to their own devices” too much [46]. The level of stroke expertise of exercise professionals concerned stroke survivors, carers, and physiotherapists [46]. This led stroke survivors to seek physiotherapist attendance during community exercise programs.
15.4. The Role of Other People with Stroke and Disability
The qualitative studies discussed the role of other people with stroke and disability. In one study [47], exercising with others with disability was viewed as a negative experience by one individual who felt that exercising with “no hopers” did not encourage progress. Otherwise, exercising with other stroke survivors and people with disabilities was viewed positively, offering opportunities to interact with individuals who had insight into the physical consequences of stroke [32, 43]. The sense of shared experience reduced feelings of loneliness and social isolation [10, 42, 43]. Being with “others in the same boat” invoked a sense of camaraderie and was seen as an opportunity to give and receive information and support [43, 44]. It was also seen as an opportunity for comparison. Facing disabilities of others acted as a reference point for one's own physical ability, and challenged self-perceived limitations [32, 47]. Observing other stroke survivors with a greater degree of disability engaging in PA and progressing, also offered hope for recovery [48]. Further, seeing others achieving acted as a motivator for continued engagement in PA to achieve personal goals [47, 48].
15.5. Group Exercise
Group exercise was seen as enjoyable and fun in the qualitative studies [10, 43]. It offered opportunities to connect socially and cultivate friendships [32, 47]. However, social involvement depended on the type of activity undertaken. Group exercise in a gym was seen as offering limited potential to meet other people [46].
Group exercise acted as a motivator to engage in PA. Perceiving oneself as being part of social group, resulted in implicit pressure to maintain attendance, as group members were reluctant to let both the instructor and other members down [42, 45]. Group exercise also increased levels of participation in PA. Social support from other group members offered encouragement to attempt new exercises and challenged negative perception of ability [43, 48].
16. Discussion
Studies of the general population indicate that psychological and some social influences on PA behaviour may be modifiable through intervention [17, 19]. In this structured review we considered the extent to which psychosocial factors influencing uptake and maintenance of PA after stroke is understood. Beliefs and attitudes about the activity, self-efficacy beliefs, or perceived control over behaviour, in addition to social support did in fact appear to be important for exercise behaviour after stroke.
It is clear from the nature and focus of the 20 studies included in this review, whilst relevant data exists to understand the role of psychosocial factors in exercise uptake and maintenance, this field of enquiry in stroke is in its infancy. The majority of included studies were exploratory qualitative studies examining experiences of participants with stroke, or cross-sectional surveys involving correlation-based theory testing. Only one trial, examining the effects of an intervention on reported PA levels, provided data regarding psychosocial factors. Furthermore, only two quantitative studies [40, 41] involved longitudinal assessment. Thus little is known about factors influencing patterns of uptake and maintenance of activity over time in this population.
Nevertheless, this review demonstrates the emerging evidence base examining PA behaviour after stroke that is mostly methodologically sound. However, studies have been predominantly conducted in the USA, often with minority ethnic populations [34, 42], therefore generalisation of findings internationally is not yet possible.
16.1. The State of the Evidence Base
Despite limitations of the field, and the necessary limits on our search strategies, one of the strengths of this evidence base is that it includes both qualitative and quantitative studies. Whilst the quantitative studies examined researcher derived theoretical constructs, the qualitative studies explored and described experiences and views of people with stroke, identifying what factors were important to stroke survivors. Consideration of qualitative and quantitative findings may enable us to identify and develop strategies to address gaps in the quantitative literature that are highly relevant to peoples' experiences and perceptions.
Most studies were conducted with community-dwelling participants, with only two recruiting in-patient participants [33, 40]. Strategies to support self-management of long-term engagement in PA necessarily occur in community settings after rehabilitation is complete, therefore the target population for these studies was appropriate. However, the time of transition between the end of rehabilitation and living in the community may present an opportunity for targeted interventions in which to shape long-term self-directed PA behaviour therefore understanding factors that might influence behaviour at this time is vitally important. Only one study was undertaken during this period [40].
Of the ten survey studies, only seven exclusively examined a stroke population. Similarly, two qualitative studies included participants with other disabling conditions. We included these mixed studies since all involved some participants with stroke, whilst acknowledging that differences in psychological, cognitive, and physical differences between conditions may make generalising findings to a purely stroke population difficult.
Definitions of PA varied across studies, from passive exercise to [36] undefined exercise that caused sweating and increased heart rate [14] to PA in general [42]. Participants in the qualitative studies referred to a greater range of activities, and activities for leisure and enjoyment such as walking and fishing were not classified as PA [42]. The lack of clear definition of what is meant by PA after stroke, presents a challenge to researchers, since their definition of PA may vary from that of participants. Participant definitions of PA may also be diverse, depending on previous experiences and opportunities available after the stroke. For progress in terms of understanding engagement in PA to occur in this field, clarity in terms of exertion involved, types of PA should be clearly defined, as well as mode of engagement, such as dose frequency and intensity, since these parameters may influence enjoyment, perceived confidence to participate, and likely uptake. Of those studies that did measure PA levels, measurement was undertaken using subjective self-report rating scales. None of the studies conducted objective measurement of PA level using pedometers or accelerometers, therefore assessment of impact of psychosocial factors on actual PA levels may not be accurate. Future studies should include more accurate assessment of PA.
16.2. Psychological Factors
The use of health behaviour models in the reviewed literature was limited, with few studies explicitly using any theoretical models in their entirety. Generally models were applied to investigate a single mediating construct such as self-efficacy or outcome expectations, outside a complete theoretical framework [14, 35, 36, 38]. Whilst it is clearly of importance to understand the correlations between individual variables and exercise behaviour, for theoretically based intervention development it is necessary to understand all the constructs likely to determine behaviour change. The qualitative studies rarely analysed findings in relation to health behaviour models or developed new theoretical models to explain the findings. The studies including participants with disability and not just stroke applied constructs from theoretical models of behaviour more consistently [36–38], a finding that may reflect the greater maturity of that field of study. The limited use of application of theoretical models to explain or change PA in the stroke studies may be an indication of immaturity of this field of study, and possibly reflects the fact that it falls at the intersection between therapy and physical outcomes research and behavioural psychology. If the field is to mature and optimal interventions are to be developed, tested and applied in practice, it is vitally important for multidisciplinary research to emerge that evaluates the behavioural as well as the physical aspects of PA.
Although there was no evidence of evaluation or application of theoretical models to develop interventions to support PA, the reviewed literature hints at some approaches that might be taken to progress the body of knowledge and practice. Of the psychological constructs examined in the extracted survey research, the mediating variable self-efficacy was the most common and most reliable predictor of exercise behaviour in the quantitative literature. It was also evident in the qualitative studies as loss of confidence for getting to places in which supported exercise occurs and for interacting with people there as well as for the PA itself, reflecting a range of specific self-efficacy beliefs that impact on the likelihood of a person with stroke becoming physically active. The observation of the importance of self-efficacy beliefs in determining PA behaviour is in line with many studies of the general population [17, 26], the elderly [49], clinical populations such as cardiac patients in rehabilitation [50], and people with multiple sclerosis [51].
Two studies showed that internal locus of control influenced physical outcome [39, 40] as opposed to PA behaviour. Possibly because it appears to apply to general perceptions of health construct than self-efficacy which is behaviour specific, there is limited evidence that locus of control is predictive of exercise behaviour from other populations [18, 49]. However, given the findings reported in our included studies that it may influence physical outcomes, perceived locus of control requires more investigation with stroke populations.
Beliefs about positive or negative effects of PA emerged from many of the studies [10, 14, 32, 34, 37, 39, 43–47]. These beliefs are considered theoretically to be important determinants of attitude and intention to be active and have been shown to be associated with exercise behaviour in many studies with clinical populations [17, 26, 49, 51].
Affective responses appear important in influencing PA after stroke. Feelings of depression, fatigue, and lack of motivation led to decreased desire to be physically active [42, 44]. These barriers are known to influence engagement in PA in clinical and general populations [26, 51–53]. Dwelling on previous health and functioning and drawing unfavourable comparisons with others led to a lack of confidence and trust in ability to negotiate barriers to PA [44, 47]. In addition, loss of purpose and the perceived attitudes of others towards disability after stroke led to reluctance to try new things, and instead stay in a safe environment [43]. The negative influence of the perceptions and attitudes of others is well documented in studies with disabled and clinical populations [54–56]. Clearly, feeling uncomfortable, self-conscious, and socially anxious undoubtedly limits the likelihood of a person with stroke engaging in PA.
However, some findings point to links between positive affect and PA. An inner drive and self-determination pushed individuals to engage in PA and facilitated goal-setting. Goal achievement was viewed as a step towards recovery and acted as motivator for continued PA [32, 42, 44, 45]. The importance of self-determination in physical activity behaviour is congruent with studies of the general population, where engaging in PA is most likely to occur when the person has internal motivation to do so [57, 58].
Competence in knowing what to do and how to do it was associated with better recovery [44] whilst perceiving that exercise was too difficult was reported as a barrier to PA [34]. The qualitative literature supported this finding, showing that negative experiences in which success did not occur influenced perceptions of competence and motivation for PA [44, 47]. Clearly, perceptions of skillfulness are important in influencing motivation for PA after stroke. Several theoretical models include perception of competence, suggesting that where achievement can be demonstrated, motivation is likely [54].
16.3. Social Factors
Social factors received comparatively less attention from researchers than psychological factors. Furthermore, the discussion of social factors was far less embedded in theoretical frameworks than the identified psychological factors.
Help from health professionals appears important in determining recovery [42, 44], and advice and helping relationships appear important in determining PA levels [14, 37]. However, the only included trial shows that an atheoretical intervention delivering advice and information from health professionals was not effective in increasing PA [41]. This finding is in line with many studies which demonstrate that information provision is not enough to change behaviour [59].
Many benefits were perceived from exercising in a group with other stroke survivors [10, 32, 42, 43, 47, 48]. Group exercise was seen as being fun and providing social opportunities and motivation through group pressure and hope for recovery. These findings concur with quantitative research in general populations which show that social support is a consistently important correlate of PA [26].
Opportunities to exercise together are clearly important to consider when developing intervention strategies to support PA after stroke given that being with others appears to enhance adherence and activity levels and to challenge perceptions of self as a disabled individual. Clearly strategies to encourage people to attend organised activities will be critical to achieving these benefits.
Family were seen on the whole as being helpful [33, 44, 45]; however, some studies also reported that they could be too critical or emotional [33], or not sufficiently confident to help [33]. The over protective or critical role of family when someone is recovering from stroke has been previously reported [60] and suggests that interventions to support PA need to involve the entire family. Interventions need to address attitudes and beliefs about their role and raising self-efficacy beliefs for supporting their family member with stroke.
16.4. Candidate Theoretical Models for Intervention Development
The psychological and social factors identified in this review point to candidate theoretical frameworks that may be useful in development of behavioural interventions that support uptake and maintenance of physical activity. One such model is the Transtheoretical Model [21] which is also known as the Stages of Change Model. This model evaluates and individual's readiness to change their behaviour. It suggests that people change behaviour in stages, from not being interested in the behaviour (precontemplation stage) to thinking about it (contemplation) to adopting (action stage) and to engaging in it long-term (maintenance). The model provides strategies to guide the individual through five stages to long term maintenance and includes self-efficacy as a key construct. Movement through the stages is underpinned by a number of social and psychological processes of change [21].
One of the disability studies in this review [37] found that the social and psychological factors did predict stage of change suggesting that the model is applicable to disabled populations. The model has been used in a number of clinical populations to improve PA behaviour and outcomes [61]; however, its effectiveness in supporting long-term adoption of PA has been challenged [59, 60]. Other stroke research has shown that the stages of change apply to stroke populations [61]. The fit of the social and psychological factors at each stage and through stage progression, however, requires replication in a stroke population before it is possible to be certain of this model as a candidate for behaviour change interventions in this population.
Another candidate theoretical model commonly used in PA research [59] is the Theory of Planned Behaviour (TPB) [23], which specifically targets intention to change behaviour, and has been used successfully in PA research [60]. Our findings show that friends and family are very important in supporting PA behaviour after stroke. With its emphasis on beliefs as a precursor to intention and its consideration of subjective normative beliefs, or beliefs about what others think about the behaviour, this model may be of particular use in encouraging adoption of PA in stroke. The evidence suggested that self-efficacy was also important for physical activity after stroke. The TPB includes perceived behavioural control as a construct that is allied to self-efficacy and suggests that strategies to enhance control over the behaviour may be effective in enhancing PA [59]. These might include experience of successfully enacting the behaviour, vicarious experience, that is, observing others perform the behaviour, and physiological feedback compatible with successful performance [59].
Strategies to apply these models to behaviour change may include individualised and tailored information provision and persuasion, approaches to increase skills through rehearsal and modelling, planning of behaviour, and setting goals as well as provision of social support, such as stroke specific group exercise or buddying support [59]. Self-monitoring and other self-regulatory skills, including setting and reviewing behavioural goals and obtaining feedback on performance are considered key to the effectiveness of behaviour change interventions [61]. With the exception of the study examining the Transtheoretical Model in which self-regulatory processes are incorporated [37]; these skills were not discussed or included in the stroke review. Clearly in developing new theoretically based interventions to support PA behaviour after stroke, it is of critical importance to evaluate how best to incorporate such strategies into interventions.
Another challenge is that individuals with stroke probably experience activity limitations due to more than only one condition, especially with increased age. The cumulative impairment may be modulated differently through psychosocial factors, compared to people who only have single diagnosis. Moreover, stroke is a complex condition, which may not only affect mobility but also communication, cognition, affective expression, and opportunities for social engagement. The literature so far has not sufficiently addressed the diversity of this population. For example, it is not clear whether psychological constructs hold true for people with altered cognitive functioning. Similarly, the social barriers and facilitators to exercise for people who experience aphasia after stroke are not well understood. Finally, as pointed out in the introduction, psychosocial factors are only one piece of the puzzle in the understanding of exercise activity after stroke. They interact with demographic, environmental, value, and societal factors, which have not been considered as part of this review. However, not acknowledging these factors would unjustly locate issues around nonadherence to exercise recommendations exclusively in the individual, while failing to acknowledge the physical environment and socioeconomic context in which people live.
17. Conclusion
This review demonstrated that there is an evidence base that begins to help us understand the role and importance of psychosocial factors in the uptake and maintenance of PA after stroke. Self-efficacy and PA beliefs appear particularly relevant constructs and should be taken cognisance of enhancing the development of theoretically based physical interventions. Theoretical frameworks such as the Transtheoretical Model and the Theory of Planned Behaviour are candidate models that may support intervention development. However, whilst our review shows that psychological constructs have been examined in relation to PA after stroke, it is clear that behavioural change theories are often not discussed in empirical publications on physical activities after stroke, and this is an area for future investigation. Social factors such as family support and opportunities to participate in group exercise are likely also to be important in PA engagement. However, the psychosocial factors are only part of a very complex picture of determinants of PA and further evaluation of health, sociodemographic, and environmental factors must be also evaluated.
Appendix
Table 8.
Details of the qualitative studies included in the review regarding method, participants, setting, summary of findings pertinent to psychological and social factors, and notes regarding theoretical models.
| Study | Method | Participants | Setting | Summary of findings | Notes |
|---|---|---|---|---|---|
| Damush et al. [42] | Qualitative: focus groups N = 13 |
Age: mean = 59 Gender: M = 8, F = 5 Time since stroke = < 12 months 85% AA, 15% white |
Country: USA Service: Academic researchers, recruited from health service—local hospital |
Barriers and facilitators to engage in PA. Barriers: Psychological: low mood, lack of motivation, and fear (pain, damage, and recurrence) Facilitators: intrinsic motivation, PA as meaningful activity Social: support from family, GP, physio, and other stroke survivors |
No theoretical model used to underpin findings |
| Maher et al. [32] | Mixed methods Qualitative: interview N = 16 (4 with stroke) |
Age: mean for whole sample (n = 16) = 47.5 years Gender: whole sample (n = 16) M=40%, F=60% Time since stroke: not reported |
Country: USA Service: local government researchers—recruited from local authority run conditioning classes |
Psychological: PA increased personal control, self-esteem, and feeling of autonomy Social: increased self-esteem and independence lessens burden on carers and relationships. PA reduces social isolation, offers chance to meet others with disability—shared experience. Exercise in group acts as motivator to participate and adhere |
No theoretical model used to underpin findings |
| Reed et al. [43] | Qualitative: interviews N = 12 | Age: >60–73+ Gender: M = 5, F = 7 Time since stroke: 15–40 months, mean 26 months |
Country: UK Service: university researchers—recruited from community stroke scheme |
Psychological: loss of confidence, loss of role/purpose and doubts over competence limit engagement in PA PA increased self-esteem, confidence, and gave sense of achievement—negated fear of falling PA seen as substitute to physio and central to recovery Social: ex-instructors important for support and recovery Shared experience—PA offers learning from others, helped reestablish role in life and positive view of social self Group PA fun, increased self-esteem, and encouraged progress |
Developed own theoretical model to underpin findings |
| Barker and Brauer [44] | Qualitative: focus groups and interviews N = 19 | Age: mean = 64 Gender: M = 12, F = 7 Time since stroke: 4.9 years |
Country: Australia Service: physiotherapy researchers—recruited from stroke support groups |
Psychological: fear of pain and harm, frustration, previous failure, low mood, feelings of incompetence (physical/cognitive), negative attitude from others, lack of self-determination, lack of access all limit engagement in PABut, negative attitudes from others also act as a motivator, and PA seen as important for recovery and progress Social: family often supportive but conversely also seen to encourage dependence Therapist important for support and recovery—but need to encourage self-management.Group PA offers camaraderie, humour, and information exchange |
Developed own theoretical model to underpin findings |
| Carin-Levy et al. [10] | Qualitative: interviews N = 14 | Age: range 45–85 Gender: M = 8, F = 6 Time since stroke: not reported |
Country: Scotland Service: academic researchers, recruited from RCT |
Psychological: vulnerability, anxiety, fear of falling, and concerns about communication act as barriers to PA Once engaged in PA: increased confidence and reduced anxiety PA offered feeling of empowerment—increased feelings of control PA class either acted as motivator to exercise at home or conversely PA not maintained as had learned all there was to learn Social: shared experience important—not feeling alone PA in group important for social self, valued social interaction, and group exercise fun |
Locus of control discussed in part explanation of results |
| Resnick et al. [45] | Qualitative: focus groups or telephone interviews N = 29 |
Age: over 45 Gender: M = 55, F = 45 Time since stroke: at least 6 months after stroke |
Country: USA Service: academic researchers, recruited from community, attended university medical centre |
Psychological: intrinsic self-determination, sense of routine, monitoring of health, and feeling physically better all motivators to engage in PA Offered increased sense of independence, offered something to do, helped keep active, and was enjoyable Social: support from family, health professionals, ex instructors encouraged adherence Not group based, but social interaction during transportation also encouraged adherence |
Aspects of SCT self-efficacy used to underpin findings |
| Galvin et al. [33] | Mixed methods Qualitative: focus groups (10 physios) stroke 40 male, 35 female |
Age: not reported Gender: not reported Time since stroke: not reported |
Country: Ireland Service: physio researchers |
Social: physios see family/friends play important role in rehab—continue work of physio Eases transition from acute to community family members often motivated to help with rehab although also acknowledged that family can be too critical, too intense, or too emotional |
No theoretical model used to underpin findings |
| Graham et al. [47] | Qualitative: interviews N = 11 (5 stroke) Interviewed initially, 3 months, and 6 months |
Age: not reported Gender: M = 5, F = 0 Time since stroke: not reported |
Country: Northern Ireland/Canada Service: clinical psych researcher (NHS), recruited from community day centre |
Psychological: focusing on disability and comparison with premorbid function and others = low self-confidence = barrier to PA. Conversely, PA seen as way to improve mood and offers encouragement to try other things and improve health PA offers way to replace loss of identity/role—competent and athletic versus disabled PA seen as way to push boundaries of society's idea of disability PA retained role of active person and continued engagement in competitive sport—change perceptions of disablement Social: PA with others provides reference point for one's own physical ability—either offers encouragement or conversely not conducive to progress—“no hopers” group PA fun and important opportunity for interaction and way to connect socially and regain degree of independence |
Aspects of SCT self-efficacy used to underpin psychological factors Self-determination theory—increased autonomy and competence and social interaction increases intrinsic motivation to engage in PA |
| Wiles et al. [46] | Qualitative interviews with stroke survivors (N = 9) and ex-professionals (N = 6) and focus groups and interviews physios (N = 15) | Age: mean = 18–78 Gender: M = 8, F = 1 Time since stroke: not specified 1993–2003 |
Country: UK Service: community EoP |
Psychological: stroke survivors motivated to engage to maintain health and fitness and as alternative to physio after rehab, but ultimately just want more physio Physio see EoP as a bridge, ex professional see it as way to control own ex-regime Social: physios role seen as very important—stroke survivor seeks presence of physio throughout EoP—want more interaction between physio and ex professional. Physio uncomfortable as could encroach on ex professional domain Ex professional role—stroke survivors “left to own devices” and concerns reexpertise from stroke survivors, carers and physio. Ex professional confident in own ability but open to specialised training Group exercise: limited interaction with other stroke survivors. Physio see opportunity for learning but acknowledge limited interaction based on own experience. Ex professional think EoP social |
No theoretical model used to underpin results |
| Patterson and Ross-Edwards [48] | Qualitative interviews with stroke survivors (N = 10) |
Age: mean = 59.8 Gender: M = 6, F = 4 Time since stroke: not reported |
Country: Australia Service: community Stroke maintenance exercise class |
Psychological: PA improved confidence and increased motivation, within group exercise class setting, but also in achieving goals within the community Offered hope for recovery when see others with greater disability engaging and progressing in PA, which motivated to continue Self-efficacy: exercise class offered practical, emotional, and social support. PA increased feelings of confidence, motivation, and associated improved self-efficacy, leading to minimisation of physical symptoms and perceived improved functioning in daily activities Social: presence of health professionals important role in guiding exercises to do, but also in accessing ongoing support not accessible in community Observing other stroke survivors achieving personal goals/making progress motivator to continue with PA and achieve own goals. Social support from other group members offered encouragement to attempt new exercises and challenge self-perceived limitations Social benefits of exercising in a group setting important as they allow for exchange of experiences, support, and information with other stroke survivors. Created feeling of belonging and sense of community |
Aspects of SCT self-efficacy |
Table 9.
Details of the quantitative studies included in the review regarding: method, participants, setting, summary of findings pertinent to psychological and social factors, and notes regarding theoretical models.
| Study | Methods | Participants | Setting | Findings | Notes |
|---|---|---|---|---|---|
| Rimmer et al. [34] | Survey: barriers to physical activity and disability survey |
N = 83 54.2 (8.2) 30 M, 70 F not reported |
USA Health promotion programme |
Psychological: competence: not knowing how and where to exercise main personal barriers to exercise, reported by 46% and 44% of participants. Motivation: lack of motivation ranked 4th personal barrier by (37%) of participants. Too lazy to exercise ranked 6th personal barrier by 33% of participants. Beliefs: 36% reported belief that exercise will not improve condition Social: importance of exercise professionals: personal trainer or exercise instructor unable to help reported by 36% of participants |
No theoretical model used to underpin questionnaire or findings |
| Galvin et al. [33] | Survey: family-mediated exercise survey |
N = 73 people with stroke 40 F, 35 M Age not reported N = 100 family members/friends 71 F, 29 M |
Ireland Hospital physiotherapy services |
Social: 91% of respondents with stroke believed that family member/friend had a role in assisting them with exercise after rehabilitation. 99% of family members/friends reported they would be willing to help with exercise after rehabilitation | No theoretical model used to underpin questionnaire or findings Not clear how questionnaire was developed. Validity and reliability not reported |
| Shaughnessy et al. [14] | Survey using the Short Self-Efficacy for Exercise Scale and the Short Outcome Expectations for Exercise Scale |
N = 321 Age 62.9 (11.7) F 177, M 127 60.2 months after stroke |
USA Mailed survey distributed via the National Stroke Association |
Psychological: self-efficacy, outcome expectations, exercise behaviour before stroke, and physician advice to exercise significantly associated with exercise behaviour. These variables predicted 33% of variance in exercise behaviour. Older participants and those experiencing fatigue had lower self-efficacy for exercise. Exercise history also significantly predicted exercise behaviour | Low response rate from national survey, attended stroke support groups therefore likely to be motivated |
| Johnston et al. [40] | Longitudinal survey assessing outcomes at 10–20 days, one month after discharge, and six months after discharge Measures: (i) the recovery locus of control scale (ii) Exercise coping self-rating for frequency and duration (iii) HADS (iv) Barthel Index (v) Observer assessed disability |
N = 71 Age 69.4 years 35 F, 36 M 10–20 days after stroke to 6 months after stroke |
Scotland Acute inpatients followed up after discharge |
Psychological: perceived control predicts recovery from disability after stroke. Frequency of exercise not correlated with one month recovery locus of control (P > 0.05), nor with observer assessed recovery at 6 months (P > 0.05), suggests that exercise not a coping response that medicates between control cognitions and recovery | Amount of explained variance is small Some measures designed for the study—validity and reliability not tested fully |
| Cardinal et al. [37] | Survey National cross-sectional survey of individuals with disability Stage of change algorithm to assess stage, process of change measure, self-efficacy scale, decisional balance scale, and exercise barriers scale |
N = 322 52.5 (13.9) years 62% F Disabled population Stroke: n = 18 |
USA Recruitment by targeting voluntary organisations and hospitals |
Psychological: transtheoretical model used to examine what constructs associated with stages. All major constructs associated with the stages of change. Largest portion of variance derived from behavioural processes of change and self-efficacy. Cognitive processes decrease and behavioural processes increase with stage progression. Cons decrease and pros increase with stage progression, self-efficacy increases with stage progression Social: helping relationships significantly associated with stage |
Stroke participants formed only small proportion of sample therefore generalisation difficult Unable to extract specific data about behavioural processes and cognitive processes used |
| Nosek et al. [36] | Survey Physical activity Social support Environmental factors Impairment and functioning (SF-36 physical functioning and role limitations) Psychological factors (SF36 mental health, role functioning emotional, self-efficacy) Social factors CHART short form and MOS social support survey |
N = 386 47.1 (10.1) years 386 F Stroke n = 25 (6.5%) |
USA National survey recruitment via disability service organisations and print and broadcast media |
Psychological: self-efficacy highest for gentle flexibility, lowest for aerobic exercise 3 × per week. Physical activity significantly correlated with self-efficacy (r = 0.50, P < 0.0001) Model predicted 33.5% of variance. Self-efficacy predicts greater involvement in physical activity, pain and duration of disability predictive of less physical activity (F(7,268) = 19.27; P < 0.0001) Social: physical activity significantly correlated with level of personal assistance (F(6,269) = 2.23, P < 0.05) |
Physically active population with 73% engaging in physical activity once a week. Self-report of physical activity Disabled sample, self-selected, and few people with stroke |
| Kinne et al. [38] | Survey Sickness Impact Scale Stage of change Self-rated abilities for health: self-efficacy and outcome expectancy Barriers to health Activities for disabled persons |
N = 83 Age 47 (1.4 ) years Stroke 7% of sample |
USA Community dwelling, recruited via disability support groups |
Psychological: self-efficacy significantly higher for participants maintaining exercise (P < 0.0001) Motivational barriers scores significantly lower for exercise maintainers (P = 0.0006) People with higher motivational barriers less likely to maintain exercise (P = 0.01). Those with higher maintenance self-efficacy higher probability of maintenance Information about what to do a barrier to exercise behaviour ranked 4th behind impairment, money, and accessible facilities |
Small proportion of sample are people with stroke Although some participants indicated that they were less active in previous year, reasons for this not explored External factors, access to facilities, transportation, money, social support, and physical and functional status not predictive of maintenance |
| Boysen et al. [41] | RCT primary outcome: Physical Activity Scale for the Elderly |
N = 314 people with stroke able to walk unassisted Intervention group n = 157 Control group N = 157 Age 69.6 years (59.6–77.7) <90 days after onset |
Centres in Denmark, China, Poland, and Estonia stroke units | No significant difference between the groups on PASE at 3,6,9,12, 18 or 24 month followup | Self-reported levels of physical activity—not assessed by accelerometer, pedometer, and so forth, or by other fitness measures. No qualitative evaluation of involvement in PA made |
References
- 1.Saunders DH, Greig CA, Mead GE, Young A. Physical fitness training for stroke patients. Cochrane Database of Systematic Reviews. 2009;(4, article CD003316) doi: 10.1002/14651858.CD003316.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Silver KHC, Macko RF, Forrester LW, Goldberg AP, Smith GV. Effects of aerobic treadmill training on gait velocity, cadence, and gait symmetry in chronic hemiparetic stroke: a preliminary report. Neurorehabilitation and Neural Repair. 2000;14(1):65–71. doi: 10.1177/154596830001400108. [DOI] [PubMed] [Google Scholar]
- 3.Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke: a randomized, controlled trial. Stroke. 2005;36(10):2206–2211. doi: 10.1161/01.STR.0000181076.91805.89. [DOI] [PubMed] [Google Scholar]
- 4.Dean CM, Richards CL, Malouin F. Task-related circuit training improves performance of locomotor tasks in chronic stroke: a randomized, controlled pilot trial. Archives of Physical Medicine and Rehabilitation. 2000;81(4):409–417. doi: 10.1053/mr.2000.3839. [DOI] [PubMed] [Google Scholar]
- 5.Mead GE, Greig CA, Cunningham I, et al. Stroke: A randomized trial of exercise or relaxation. Journal of the American Geriatrics Society. 2007;55(6):892–899. doi: 10.1111/j.1532-5415.2007.01185.x. [DOI] [PubMed] [Google Scholar]
- 6.Cramp MC, Greenwood RJ, Gill M, Lehmann A, Rothwell JC, Scott OM. Effectiveness of a community-based low intensity exercise programme for ambulatory stroke survivors. Disability and Rehabilitation. 2010;32(3):239–247. doi: 10.3109/09638280903095916. [DOI] [PubMed] [Google Scholar]
- 7.Cramp MC, Greenwood RJ, Gill M, Rothwell JC, Scott OM. Low intensity strength training for ambulatory stroke patients. Disability and Rehabilitation. 2006;28(13-14):883–889. doi: 10.1080/09638280500535157. [DOI] [PubMed] [Google Scholar]
- 8.Wevers L, Van De Port I, Vermue M, Mead G, Kwakkel G. Effects of task-oriented circuit class training on walking competency after stroke: a systematic review. Stroke. 2009;40(7):2450–2459. doi: 10.1161/STROKEAHA.108.541946. [DOI] [PubMed] [Google Scholar]
- 9.Stuart M, Benvenuti F, MacKo R, et al. Community-based adaptive physical activity program for chronic stroke: feasibility, safety, and efficacy of the empoli model. Neurorehabilitation and Neural Repair. 2009;23(7):726–734. doi: 10.1177/1545968309332734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carin-Levy G, Kendall M, Young A, Mead G. The psychosocial effects of exercise and relaxation classes for persons surviving a stroke. Canadian Journal of Occupational Therapy. 2009;76(2):73–80. doi: 10.1177/000841740907600204. [DOI] [PubMed] [Google Scholar]
- 11.Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors: an American heart association scientific statement from the council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention. Stroke. 2004;35(5):1230–1240. doi: 10.1161/01.STR.0000127303.19261.19. [DOI] [PubMed] [Google Scholar]
- 12.Scottish Intercollegiate Guidelines Network (SIGN) Management of Patients with Stroke: Rehabilitation, Prevention and Management of Complications, and Discharge Planning: a National Clinical Guideline. Edinburgh, UK: Scottish Intercollegiate Guidelines Network; 2010. [Google Scholar]
- 13.Löfgren B, Nyberg L, Mattsson M, Gustafson Y. Three years after in-patient stroke rehabilitation: a follow-up study. Cerebrovascular Diseases. 1999;9(3):163–170. doi: 10.1159/000015948. [DOI] [PubMed] [Google Scholar]
- 14.Shaughnessy M, Resnick BM, Macko RF. Testing a model of post-stroke exercise behavior. Rehabilitation Nursing. 2006;31(1):15–21. doi: 10.1002/j.2048-7940.2006.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 15.Rand D, Eng JJ, Tang PF, Jeng JS, Hung C. How active are people with stroke?: use of accelerometers to assess physical activity. Stroke. 2009;40(1):163–168. doi: 10.1161/STROKEAHA.108.523621. [DOI] [PubMed] [Google Scholar]
- 16.Touillet A, Guesdon H, Bosser G, Beis JM, Paysant J. Assessment of compliance with prescribed activity by hemiplegic stroke patients after an exercise programme and physical activity education. Annals of Physical and Rehabilitation Medicine. 2010;53(4):250–265. doi: 10.1016/j.rehab.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Rhodes RE, Pfaeffli LA. Mediators of physical activity behaviour change among adult non-clinical populations: a review update. International Journal of Behavioral Nutrition and Physical Activity. 2010;7(11, article 37) doi: 10.1186/1479-5868-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biddle SJH, Mutrie N. Psychology of Physical Activity: Determinants, Well -Being, and Interventions. 2nd edition. London, UK: Routledge; 2008. [Google Scholar]
- 19.Plotnikoff RC, Karunamuni N. Steps towards permanently increasing physical activity in the population. Current Opinion in Psychiatry. 2011;24(2):162–167. doi: 10.1097/YCO.0b013e3283438107. [DOI] [PubMed] [Google Scholar]
- 20.Bandura A. Health promotion from the perspective of social cognitive theory. In: Norman P, Abraham C, Conner M, Norman P, Abraham C, Conner M, editors. Understanding and Changing Health Behaviour. Amsterdam,The Netherlands: Harwood Academic Publishers; 2000. pp. 299–339. [Google Scholar]
- 21.Prochaska JO, Di Clemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy. 1982;19(3):276–288. [Google Scholar]
- 22.Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Canadian Psychology. 2008;49(3):182–185. [Google Scholar]
- 23.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- 24.Noar SM, Zimmerman RS. Health behavior theory and cumulative knowledge regarding health behaviors: are we moving in the right direction? Health Education Research. 2005;20(3):275–290. doi: 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- 25.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions: how are we doing? How might we do better? American Journal of Preventive Medicine. 1998;15(4):266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 26.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Medicine and Science in Sports and Exercise. 2002;34(12):1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 27.Boslaugh SE, Andresen EM. Correlates of physical activity for adults with disability. Preventing Chronic Disease. 2006;3(3):p. A78. [PMC free article] [PubMed] [Google Scholar]
- 28.Emerson JD, Burdick E, Hoaglin DC, Mosteller F, Chalmers TC. An empirical study of the possible relation of treatment differences to quality scores in controlled randomized clinical trials. Controlled Clinical Trials. 1990;11(5):339–352. doi: 10.1016/0197-2456(90)90175-2. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JPT, Altman DG. Assessing risk of bias in included studies. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. chapter 8. The Cochrane Collaboration; 2011. [Google Scholar]
- 30.Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Quality and Safety in Health Care. 2004;13(3):223–225. doi: 10.1136/qshc.2003.008714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qualitative Health Research. 2003;13(7):905–923. doi: 10.1177/1049732303253488. [DOI] [PubMed] [Google Scholar]
- 32.Maher EJ, Kinne S, Patrick DL. “Finding a good thing”: the use of quantitative and qualitative methods to evaluate an exercise class and promote exercise for adults with mobility impairments. Disability and Rehabilitation. 1999;21(9):438–447. doi: 10.1080/096382899297422. [DOI] [PubMed] [Google Scholar]
- 33.Galvin R, Cusack T, Stokes E. To what extent are family members and friends involved in physiotherapy and the delivery of exercises to people with stroke. Disability and Rehabilitation. 2009;31(11):898–905. doi: 10.1080/09638280802356369. [DOI] [PubMed] [Google Scholar]
- 34.Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. Journal of Rehabilitation Research and Development. 2008;45(2):315–322. doi: 10.1682/jrrd.2007.02.0042. [DOI] [PubMed] [Google Scholar]
- 35.Resnick B, Shaughnessy M, Macko RF, et al. Testing of the short self-efficacy and outcome expectations for exercise scales in the USA. International Journal of Therapy and Rehabilitation. 2007;14(3):110–117. [Google Scholar]
- 36.Nosek MA, Hughes RB, Robinson-Whelen S, Taylor HB, Howland CA. Physical activity and nutritional behaviors of women with physical disabilities: physical, psychological, social, and environmental influences. Women’s Health Issues. 2006;16(6):323–333. doi: 10.1016/j.whi.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 37.Cardinal BJ, Kosma M, McCubbin JA. Factors influencing the exercise behavior of adults with physical disabilities. Medicine and Science in Sports and Exercise. 2004;36(5):868–875. doi: 10.1249/01.mss.0000126568.63402.22. [DOI] [PubMed] [Google Scholar]
- 38.Kinne S, Patrick DL, Maher EJ. Correlates of exercise maintenance among people with mobility impairments. Disability and Rehabilitation. 1999;21(1):15–22. doi: 10.1080/096382899298052. [DOI] [PubMed] [Google Scholar]
- 39.Barker RN, Gill TJ, Brauer SG. Factors contributing to upper limb recovery after stroke: a survey of stroke survivors in Queensland Australia. Disability and Rehabilitation. 2007;29(13):981–989. doi: 10.1080/09638280500243570. [DOI] [PubMed] [Google Scholar]
- 40.Johnston M, Morrison V, Macwalter R, Partridge C. Perceived control, coping and recovery from disability following stroke. Psychology and Health. 1999;14(2):181–192. [Google Scholar]
- 41.Boysen G, Krarup LH, Zeng X, et al. ExStroke Pilot Trial of the effect of repeated instructions to improve physical activity after ischaemic stroke: a multinational randomised controlled clinical trial. British Medical JournalBritish Medical Journal. 2009;339(7715):273–275. doi: 10.1136/bmj.b2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Damush TM, Plue L, Bakas T, Schmid A, Williams LS. Barriers and facilitators to exercise among stroke survivors. Rehabilitation Nursing. 2007;32(6):253–262. doi: 10.1002/j.2048-7940.2007.tb00183.x. [DOI] [PubMed] [Google Scholar]
- 43.Reed M, Harrington R, Duggan A, Wood VA. Meeting stroke survivors perceived needs: a qualitative study of a community-based exercise and education scheme. Clinical Rehabilitation. 2010;24(1):16–25. doi: 10.1177/0269215509347433. [DOI] [PubMed] [Google Scholar]
- 44.Barker RN, Brauer SG. Upper limb recovery after stroke: the stroke survivors’ perspective. Disability and Rehabilitation. 2005;27(20):1213–1223. doi: 10.1080/09638280500075717. [DOI] [PubMed] [Google Scholar]
- 45.Resnick B, Michael K, Shaughnessy M, Kopunek S, Nahm ES, Macko RF. Motivators for treadmill exercise after stroke. Topics in Stroke Rehabilitation. 2008;15(5):494–502. doi: 10.1310/tsr1505-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wiles R, Demain S, Robison J, Kileff J, Ellis-Hill C, McPherson K. Exercise on prescription schemes for stroke. Disability and Rehabilitation. 2008;30(26):1966–1975. doi: 10.1080/09638280701772997. [DOI] [PubMed] [Google Scholar]
- 47.Graham R, Kremer J, Wheeler G. Physical exercise and psychological well-being among people with chronic illness and disability: a grounded approach. Journal of Health Psychology. 2008;13(4):447–458. doi: 10.1177/1359105308088515. [DOI] [PubMed] [Google Scholar]
- 48.Patterson S, Ross-Edwards B. Long-term stroke survivors' needs and perceptions of an exercise maintenance model of care. International Journal of Therapy and Rehabilitation. 2009;16(12):659–669. [Google Scholar]
- 49.Rhodes RE, Martin AD, Taunton JE, Rhodes EC, Donnelly M, Elliot J. Factors associated with exercise adherence among older adults. An individual perspective. Sports Medicine. 1999;28(6):397–411. doi: 10.2165/00007256-199928060-00003. [DOI] [PubMed] [Google Scholar]
- 50.Sniehotta FF, Schwarzer R, Scholz U, Schüz B. Action planning and coping planning for long-term lifestyle change: theory and assessment. European Journal of Social Psychology. 2005;35(4):565–576. [Google Scholar]
- 51.Kayes NM, McPherson KM, Schluter P, Taylor D, Leete M, Kolt GS. Exploring the facilitators and barriers to engagement in physical activity for people with multiple sclerosis. Disability and Rehabilitation. 2011;33(12):1043–1053. doi: 10.3109/09638288.2010.520801. [DOI] [PubMed] [Google Scholar]
- 52.Cerin E, Leslie E, Sugiyama T, Owen N. Perceived barriers to leisure-time physical activity in adults: an ecological perspective. Journal of Physical Activity and Health. 2010;7(4):451–459. doi: 10.1123/jpah.7.4.451. [DOI] [PubMed] [Google Scholar]
- 53.Crombie IK, Irvine L, Williams B, et al. Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age and Ageing. 2004;33(3):287–292. doi: 10.1093/ageing/afh089. [DOI] [PubMed] [Google Scholar]
- 54.Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. American Journal of Preventive Medicine. 2004;26(5):419–425. doi: 10.1016/j.amepre.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 55.Buffart LM, Westendorp T, Van Den Berg-Emons RJ, Stam HJ, Roebroeck ME. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. Journal of Rehabilitation Medicine. 2009;41(11):881–885. doi: 10.2340/16501977-0420. [DOI] [PubMed] [Google Scholar]
- 56.Poder K, Ghatavi K, Fisk JD, et al. Social anxiety in a multiple sclerosis clinic population. Multiple Sclerosis. 2009;15(3):393–398. doi: 10.1177/1352458508099143. [DOI] [PubMed] [Google Scholar]
- 57.Standage M, Sebire SJ, Loney T. Does exercise motivation predict engagement in objectively assessed bouts of moderate-intensity exercise?: a self-determination theory perspective. Journal of Sport and Exercise Psychology. 2008;30(4):337–352. doi: 10.1123/jsep.30.4.337. [DOI] [PubMed] [Google Scholar]
- 58.Hagger MS, Chatzisarantis NLD. Intrinsic Motivation and Self-Determination in Exercise & Sport. Ill, USA: Human Kinetics; 2007. [Google Scholar]
- 59.Hardeman W, Johnston M, Johnston D, Bonetti D, Wareham N, Kinmonth AL. Application of the theory of planned behaviour in behaviour change interventions: a systematic review. Psychology and Health. 2002;17(2):123–158. [Google Scholar]
- 60.Darker CD, French DP, Eves FF, Sniehotta FF. An intervention to promote walking amongst the general population based on an ’extended’ theory of planned behaviour: a waiting list randomised controlled trial. Psychology and Health. 2010;25(1):71–88. doi: 10.1080/08870440902893716. [DOI] [PubMed] [Google Scholar]
- 61.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychology. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]


