Abstract
This paper has two aims. First, we provide an overview of the potential of technology in the area of brief interventions for substance use, and describe recent projects from our lab that are illustrative of that potential. Second, we present data from a study of during-session predictors of brief intervention response. In a sample of post-partum women (N = 39), several variables showed promise as predictors of later drug use, and a brief index derived from them predicted abstinence with a sensitivity of .7 and a specificity of .89. This promising approach and initial study findings support the importance of future research in this area.
Keywords: Pregnancy, substance abuse, motivational interviewing, technology, prediction
Computer-delivered interventions for substance use have a range of potential advantages over more traditional approaches. These advantages include greater ease of dissemination and replication, cost-effectiveness, anonymity, accessibility, and personalization (Copeland & Martin, 2004; Hester & Miller, 2006; Kypri, Sitharthan, Cunningham, Kavanagh, & Dean, 2005; Ondersma, Chase, Svikis, & Schuster, 2005). Interactive technology for promotion of behavior change has been supported by clinical trials of its use for alcohol abuse (Hester, Squires, & Delaney, 2005; Kypri, et al., 2004; Neighbors, Larimer, & Lewis, 2004), drug abuse (Gilbert, et al., 2008; Ondersma, Svikis, & Schuster, 2007), and sexual risk-taking (Kiene & Barta, 2006).
Current uses of intervention technology in substance abuse
Such data suggest that this technology may have utility in a number of areas. In recent years, a number of computer-delivered interventions have been made available online. Examples includewww.alcoholscreening.org and www.drugscreening.org, both of which are part of “Join Together,” a program of the Boston University School of Public Health with major funding from the Robert Wood Johnson Foundation; e-chug and e-toke (www.e-chug.com, www.e-toke.com), which can be purchased by schools or colleges interested in making online feedback-based interventions available to their students; and www.drinkerscheckup.com, which provides an interactive brief motivational intervention for interested adults. The efficacy of both e-chug (Walters, Vader, & Harris, 2007) and www.drinkerscheckup.com (Hester, et al., 2005)have been supported in early trials of this technology.
Brief computer-delivered interventions in primary care
Many other current applications are employed in primary care settings, where the tremendous potential reach of computer-delivered approaches can be leveraged(e.g., Kypri et al., 2005). This is true of our own work, which has focused primarily on brief motivational interventions with low-income urban women who report use of drugs or alcohol in the post-partum period (Ondersma, et al., 2005; Ondersma, et al., 2007). This population was selected for three reasons. First, nearly all of this particular population is theoretically accessible via primary care, since only .9% of women in the United States give birth outside of a hospital (Martin, et al., 2007). Second, interventions at this juncture may make optimal use of the “teachable moment” that often accompanies new parenthood (McBride, Emmons, & Lipkus, 2003). Finally, reducing substance abuse among parenting women is likely to benefit both new mothers and their infants.
In this approach, women are recruited during their post-delivery hospital stay, prior to discharge. Participants are given a touch-screen enabled Tablet PC, accessing web-based software that is extremely easy to use regardless of reading or computer literacy; it features a clean appearance, a limited number of colors, large font, and a three-dimensional, talking, animated narrator. The software presents questions one at a time during the assessment section, and uses information gathered during this phase to provide personalized and normed feedback regarding how each participant’s drug use compares to national averages. In addition to receiving personalized/normed feedback, participants are asked to complete a decisional balance exercise which assesses the pros and cons of drug use, and an optional goal-setting exercise which explores interest in quitting, cutting down, etc. The most recent version of this software also includes components addressing low self-efficacy, relapse prevention, the negative effects of parental substance use on child outcomes, as well as preparation for change. All components are presented via branching logic and/or participant expression of interest in that topic.
Acceptability and efficacy are key issues with any new intervention approach. Regarding acceptability, participants in the development phase of this research (Ondersma, et al., 2005) gave the software high marks for ease of use (N = 47; mean of 5.0 on a 1–5 scale), respectfulness (mean of 4.8), and overall liking (mean of 4.7). Subjective responses were also positive, particularly regarding the animated narrator and the blending of humor with the central intervention components. Approximately 16% of women approached for a larger, later study declined to be screened for eligibility (Ondersma et al., 2007), and an additional small proportion expressed concern about their ability to work with a computer; but the concerns of the hesitant women were easily allayed through a demonstration of the simple software and touch-screen interface. Most importantly, no prospective participants indicated that they were unwilling to use the computer as part of study participation.
Regarding efficacy, the National Institute on Drug Abuse (NIDA; part of the U. S. National Institutes of Health) is currently funding a confirmatory randomized clinical trial of this computer-delivered intervention, with a proposed N of 350. An earlier trial designed to determine feasibility, acceptability, and an estimate of effect size yielded encouraging results: we found a significant effect on overall drug use at 4-month follow-up (d = .46 vs. an assessment-only condition, which is considered a small to moderate effect). Although preliminary, this effect size is comparable to those for substance use interventions generally(e.g., Burke, Arkowitz, & Menchola, 2003; Moyer, Finney, Swearingen, & Vergun, 2002; Prendergast, Podus, Chang, & Urada, 2002).
Extending brief intervention to non-disclosers
A second approach being used with post-partum women attempts to address an important shortcoming of traditional screening and brief intervention programs. That is, they are all reliant on self-report of substance abuse, which limits their applicability to only those persons who are willing to report substance abuse. Disclosure of drug use is an issue in nearly every setting, but particularly with women in the perinatal period, who fear a number of negative consequences should their drug use become known (Markovic, et al., 2000). These fears are justified in many parts of the country, where evidence of prenatal substance abuse can lead to loss of child custody or even criminal prosecution (Ondersma, Malcoe, & Simpson, 2001; Ondersma, Simpson, Brestan, & Ward, 2000).
We are attempting to address this problem in two ways. First, we are validating a brief, indirect measure of drug use risk by administering to post-partum women a large checklist of risk factors known to be associated with drug use (smoking, history of trauma, risk-taking, etc.), and subsequently obtaining urine and hair samples to be tested for various drugs (since hair sample scan detect drug use over an approximate 90-day window). Items that predict positive urine/hair tests will be cross-validated in a new sample. The resulting measure will be given a low cutoff score in order to maximize sensitivity over specificity. It is hoped that this procedure will allow practitioners to identify a large number of true drug-using persons, while also ruling out at least half of all persons screened.
Second, we are exploring ways to utilize information gained from indirect screening. Clearly, this approach will result in identification of many persons who cannot be engaged in a direct conversation about their drug use, for two reasons: (a) they have not disclosed drug use, and (b) drug use may not be present. We are thus developing an indirect intervention that engages participants in discussion of change at a more macro level, without presuming drug use or giving offense in any way. This indirect intervention will raise the issue of “parenting strengths” at a more general level, and will encourage participants to interactively discuss their status in several areas, including safety from violence, emotional well-being, and a healthy lifestyle. In this way, issues related to drug use can be raised in a non-threatening manner, as part of a larger discussion that is strengths-based, often in the context of other factors that may co-occur with substance use in the target individual or their significant other (violence exposure/trauma and mental illness). We are currently examining the feasibility and acceptability of this approach under an exploratory/developmental award from NIDA.
Augmenting early home visitation
We are also using computer-delivered intervention technology as a supplement for early home visitation with mothers who have recently given birth. Early home visitation programs are many and varied; most involve frequent in-home sessions with a paraprofessional or nurse, and focus on prevention of child maltreatment among at-risk parents who have not yet been in contact with Child Welfare Services. Although popular (a 2005 report by Gomby suggested that approximately 350,000 families were enrolled in early home visitation annually), evidence for the effectiveness of such programs has been inconsistent at best (Chaffin, 2004; Duggan, et al., 2007; Duggan, McFarlane, et al., 2004). Process examinations have suggested that risk factors for maltreatment such as substance abuse, parental mental health disorders, and intimate partner violence often go unrecognized and unaddressed in such programs (Duggan, Fuddy, et al., 2004).
Our current work in this area involves the provision of Tablet PC’s to home visitors. The PC’s use aircards (which access the internet via cell phone towers), and are used by the parent directly for the first 20 minutes of the first 8 regularly scheduled home visitation sessions. This approach allows for direct screening and brief intervention for the key child maltreatment risk factors of intimate partner violence, depression and other mental illness, and substance abuse. It also allows for direct introduction of other evidence-based strategies that are difficult for home visitors to replicate because of (a) the intensive training needed to provide treatments such as Motivational Interviewing or Cognitive Therapy, (b) discomfort with such topics, and (c) fear of alienating parents who do not wish to discuss these topics. This ongoing Centers for Disease Control and Prevention (CDC)-funded randomized clinical trial will randomly assign 420 women into (a) home visitation as usual, (b) software-supplemented home visitation, or (c) community referral conditions, in order to evaluate the ability of the brief computer-delivered sessions to augment the efficacy of traditional early home visitation.
Predicting intervention outcome via dynamic, during-session responses
The above all represent specific applications of interactive technology to brief substance use interventions with women in the perinatal period, and are potentially fruitful directions for research. The consistency, interactivity, and modularity of such technology also opens up a number of additional, less frequently discussed avenues for research.
One such avenue involves the possibility of leveraging the exacting, moment-by-moment nature of technology to examine how it exerts its effects, and with whom. For example, computer-delivered interventions have a unique ability to repeatedly evaluate participants’ during-session responses (such as current intention to change, interest, or self-efficacy), and to analyze those responses in order to (a) forecast later behavioral responses, and (b) further tailor intervention content within a particular intervention session. The first of these possibilities--forecasting intervention response--would enable developmental clinical trials to use in-session response as a proxy for longer-term behavioral change. Under such a scenario, large numbers of developmental trial participants could facilitate intervention optimization, without the substantial added cost and delay inherent in longitudinal follow-up. These developmental trials could then be followed by more expensive but more rigorous traditional trials. Such a process could work much like animal studies for medication development, in which earlier, less expensive developmental work paves the way for further research. However, achieving modest or better associations between in-session responses and subsequent behavior—particularly if the responses are measured only during a single, brief intervention session—may be a challenge. Such variables by definition have low reliability, which in turn puts a cap on validity.
The second of the above possibilities--dynamic tailoring of intervention content--would allow the computer to actively seek and respond to predefined in-session responses and attitude changes. For example, if a 20% increase in self-reported willingness to quit using drugs is shown to be a key criterion, the computer could be programmed to present intervention components in a pre-determined order until that standard is met. Such data could also allow leveraging of artificial intelligence (AI) techniques into the field of computer-delivered behavioral interventions. AI is a complex multidisciplinary field in which, broadly speaking, software is developed that can reason, learn, plan, and communicate in intelligent ways. In the present example, AI technology could allow the computer to teach itself the best strategies for obtaining responses that are correlated with a positive behavioral response at follow-up (Miller, 2001). Either of the above approaches would allow a move from interventions that pre-determine length and content, to those that dynamically alter length and content based on actual response.
Dynamic in-session predictors: Considerations
Regarding what to measure, potential constructs should be related to actual behavior change, and should be state variables with some possibility of changing in the course of a single session. State variables are rarely of primary interest in behavioral science. Studies overwhelmingly focus on stable traits with the potential to predict key outcomes such as disease risk, treatment response, morbidity and mortality, etc. In the present project, however, state variables are necessary in order to capture the moment-to-moment changes being sought. Ideal dynamic predictor variables are also briefly measured, given their intended use one or more times during individual intervention sessions; and clearly associated with key outcomes.
A wide range of constructs may fit the above criteria. For example, intention to change can be measured quickly and can theoretically fluctuate rapidly. A recent meta-analysis suggested that treatment-related effects on intention to change are related to actual behavior change (Webb & Sheeran, 2006). Recognition that one’s behavior is causing problems has also been supported as a correlate of change (Demmel, Beck, Richter, & Reker, 2004; Zhang, Harmon, Werkner, & McCormick, 2004). Openness to treatment, through the clear association between treatment and outcomes, may also be a good candidate for such an approach. Finally, subjective satisfaction with a given intervention approach may also be related to later response (Long, Williams, Midgley, & Hollin, 2000). But although such variables meet the above criteria in terms of candidacy for in-session prediction of follow-up outcomes, the extent to which they actually do so is unknown.
Further, such variables must be summed or scored in order to yield a prediction, but there is no guidance available regarding the specific type of algorithm to be used. For example, regarding self-efficacy, is it best to measure average during-session feelings of self-efficacy, increase in self-efficacy from pre-session to post-session, self-efficacy at the end of the treatment session, or the slope of during-session change in self-efficacy? It is not clear which of these would be most likely to predict outcomes.
Current study
The present analysis is a preliminary examination of (a) the extent to which state variables, measured during a single-session computer-delivered motivational intervention, can predict behavior change 4 months later; and (b) the extent to which various methods of scoring in-session dynamic indicators (i.e., mean value, ending value, and magnitude of change) predict behavior change. Evidence that such variables can explain even modest amounts of variance in subsequent behavior will suggest that in-session indicators merit further consideration.
Method
Participants
Participants were 39 post-partum women who were randomized into the intervention condition in a previously reported trial (Ondersma, et al., 2007). Participants were included if they reported any illicit drug use in the month prior to pregnancy, and were excluded if they were younger than 18 years of age, had not slept since giving birth (in order to reduce the influence of fatigue), had an infant in the Neonatal In-session prediction 12 Intensive Care Unit (in order to avoid seeking informed consent from distressed or grieving mothers), or had been administered narcotic pain medication in the past 4 hours. The sample for this study was restricted to participants who returned for follow-up evaluation. The present sample of 39 women represents 70.9% of 55 participants randomized into the intervention condition. Participants were all African-American and primarily of low socioeconomic status (Table 1).
Table 1.
Sample characteristics (N = 39)
| Characteristic | N(%) |
|---|---|
| African-American | 39 (100) |
| Less than high school education | 16 (41) |
| Public assistance in past year | 37 (94.9) |
| Married | 3 (7.7) |
| Age | 25.6 (5.9) |
| Any drug use 3 months prior to pregnancy | 32 (82.1) |
| Any drug use 3 months prior to follow up | 27 (69.2) |
Note. “Public assistance” refers to receipt of food stamps, Women, Infants, and Children food supplements (WIC), or Temporary Assistance for Needy Families (TANF).
Procedure
Research assistants approached women in their private hospital rooms and provided a brief description of the study. Women expressing interest were asked to provide verbal consent (using an information sheet) for a brief, anonymous, computer-based screening to determine eligibility. Those who were eligible on the computer-based screening were asked to provide written informed consent. All those providing consent were randomly assigned to either assessment only or assessment plus 20-minute computer-delivered intervention conditions. All participants worked with the Tablet PC (a laptop with integrated touch screen, eliminating the need to use a keyboard or mouse) while in their hospital bed, using headphones for privacy. Participants were given a $30 gift certificate to Target stores, as compensation for their time and effort. All procedures were approved by the Wayne State University Institutional Review Board (IRB).
The single-session intervention itself consisted of three components based on motivational interviewing and brief intervention principles (Miller & Rollnick, 2002): (a) feedback regarding the negative consequences of drug use that the participant reported, as well as self-reported readiness to change, and drug use as compared to that of all adult women; (b) pros and cons of drug use and related change, in which the participant chooses from lists of positive and negative aspects of drug use from their perspective; and (c) a summary and query regarding the participant’s interest in change, followed by optional goal-setting regarding drug use. These three components were presented to each participant in counterbalanced order. Measures tapping drug use likelihood and recognition of the need for change (see below) were administered at baseline and following each intervention component; satisfaction-related items (see below) were administered following each component.
Follow-up evaluations took place in the investigators’ offices at approximately 4 months post-baseline, and were conducted by a research assistant blind to experimental group as well as drug use status of the participant. Participants were contacted repeatedly by mail and later by phone following published tracking guidelines (Scott, 2004). Participants completing the follow-up evaluation received a $60 gift certificate and assistance with transportation (either a $10 gas card or a taxi). In addition, participants who completed follow-up assessment were eligible for a lottery-style drawing for an additional prize (ranging from hand lotion to a single $100 gift card).
Measures
As noted above, a very brief assessment battery was adopted in order to account for repeated measurements in a brief time frame. First, respondents answered a series of visual analogue scale items via the computer, in which “marks” on an on-screen scale were coded from 1 to 100. The first such item tapped drug use likelihood (“How likely are you to use drugs, even a little, ever again?”, scored negatively to represent predicted drug avoidance), and two additional visual analogue scale items tapped perceptions of the seriousness of the drug use (“How big of a problem is your drug use?”), and treatment motivation (“How interested are you in treatment right now?”). Internal consistency of these two items was good, particularly for a 2-item scale (Cronbach’s alpha = .79 as rated pre-session, and .78 as rated during the computer-delivered intervention session).
Visual analogue scale items measuring satisfaction tapped general approval (“How much did you like the … component?), ease of use (“Was it easy to use?), and perceived respect (“Was it respectful of you?). As above, respondents answered each item via the computer, in which “marks” on the scale were coded from 1 to 100. Internal consistency of these 3 items ranged from .82 to .92 (Cronbach’s alpha). The questions assessing drug use likelihood, need for change, treatment readiness, and satisfaction were asked at the end of each intervention component (feedback, pros and cons, and goal setting).
At both baseline and follow-up, all participants completed the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), a well-validated brief measure developed by the World Health Organization, that evaluates frequency of use as well as consequences of use for all categories of substances separately (Newcombe, Humeniuk, Hallet, & Ali, 2003; Newcombe, Humeniuk, & Ali, 2005; WHO ASSIST Working Group, 2002). The ASSIST has previously shown an internal consistency estimate of .80 and strong evidence of concurrent, predictive, construct, and discriminative validity (e.g., sensitivity of .80 to .97, and specificity of .71 to .96, in predicting structured interview-based determinations of drug abuse) (Humeniuk & Ali, 2006). Given the unreliability of self-report of drug use prior to pregnancy, the need for participant protection, and the tendency for women to eliminate or reduce drug use during pregnancy, the baseline ASSIST was completed with respect to the 3 months preceding pregnancy; at follow-up the ASSIST tapped drug use during the past 3 months. At follow-up qualitative urinalysis testing was conducted for methamphetamines, cocaine, marijuana, opiates, and benzodiazepines using the Redwood Biotech Redi Cup.™ All urinalysis results, which are displayed on the Redi Cup™ as bars indicating that drug use is either present or not present, were read by a research assistant blind to participant experimental condition. Participants were considered positive for drug use at follow-up if (a) urine testing indicated the presence of metabolites of any illicit drug; or (b) their completed ASSIST protocol indicated marijuana use at least weekly, or any other illicit drug use at any point in the past 3 months.
Data analysis
Participants’ responses were scored in five ways: (a) mean value--a simple mean of all three during-intervention responses; (b) first value—the response provided following the first of the three counterbalanced intervention components; (c) ending value--the value present at the end of the last of the three components; (d) change—the extent to which the mean response represents a change (increase or decrease) from the baseline (pre-session) rating (note that this scoring method was only available for the motivation-related items), and (e) slope--the change in value (increase or decrease) from the first intervention component to the last. Each scoring method was utilized for each of the three state variable domains.
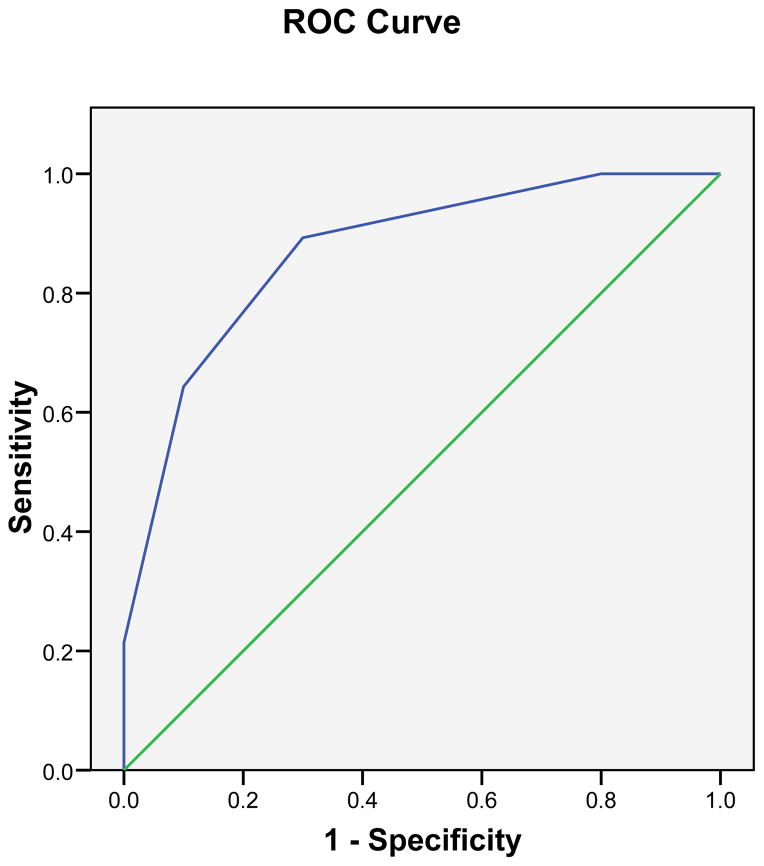
Primary analyses were of two types. First, each item or group of items was correlated with drug use at follow-up using rank biserial correlations (using the SAS Biserial macro), for ease of evaluating the strength of associations. Since significance values are not available with the SAS Biserial macro, the significance of these associations was evaluating using Mann-Whitney U tests. Second, higher-performing predictors were combined into a single scale, the characteristics and ideal cutoff of which was evaluated via a Receiver Operating Characteristics (ROC) curve.
Results
Participants
All 38 participants were African-American women, with a mean age of 25.9 (σ = 5.7). Overall SES was low: 36 (94.7%) reported receiving some form of public assistance in the past year, 35 (92.1%) were unmarried, 15 (40%) had less than a high-school education, and 25 (65.8%) had not worked full-time in the prior 6 months. Most were regular marijuana users, with 28 (73.7%) reporting using marijuana at least weekly. N = 4(10.5%) reported using cocaine in the month prior to pregnancy, and ten participants (26.3%) were drug-free at follow-up.
Correlations
Table 2 presents the results of rank biserial correlations between the three within-session predictors (rows) and drug use at follow-up, arranged under the five scoring methods (columns). The first section of Table 2 presents the above for predictor-measurement combinations that collapse across the three counterbalanced intervention components (pros and cons, feedback, and optional goal-setting) in favor of focusing on ordering of components. The second section of Table 2 focuses on ratings taken after presentation of the pros and cons component (collapsing across order), and therefore lacks values for scoring methods that are dependent on order. The same is true for the next two sections, representing ratings taken after presentation of the feedback and goal-setting components.
Table 2.
Rank biserial correlations between predictors and 4-month drug use outcome, by scoring method
| Variable | Scoring method | ||||
|---|---|---|---|---|---|
| Mean | Change from baseline | First | Ending | Slope | |
| Collapsing across components | |||||
| Likelihood | −.11 | −.11 | −.31† | .14 | .26 |
| Seriousness | .00 | .01 | .06 | −.06 | .12 |
| Satisfaction | −.31† | -- | −.10 | −.08 | −.14 |
| Pros and cons only | |||||
| Likelihood | −.04 | −.15 | -- | -- | -- |
| Seriousness | −.09 | −.46*† | -- | -- | -- |
| Satisfaction | −.13 | -- | -- | -- | -- |
| Feedback only | -- | -- | -- | ||
| Likelihood | −.32*† | −.10 | -- | -- | -- |
| Seriousness | .05 | −.26 | -- | -- | -- |
| Satisfaction | −.50*† | -- | -- | -- | -- |
| Goal setting only | |||||
| Likelihood | −.07 | −.09 | -- | -- | -- |
| Seriousness | .15 | −.03 | -- | -- | -- |
| Satisfaction | −.11 | -- | -- | -- | -- |
Note. N = 39. “Mean” refers to mean of ratings from each of the three intervention components; “Change from baseline” refers to the difference between the baseline and during-treatment session mean. The five cells noted with a dagger symbol (†) are those utilized for the summed prediction scale.
p < .05 (evaluated via Mann-Whitney U tests)
Although many variables were only weakly associated with drug use at follow-up, several showed moderate associations with drug use at follow-up. Higher self-reported satisfaction following the feedback component was associated with decreased likelihood of drug use (rrb = −.50, p = .014). During-treatment increases in problem recognition/treatment readiness were moderately associated with decreased likelihood of drug use (rrb = −.46, p = .022). Higher mean satisfaction with the three intervention components, and lower self-reported likelihood of future drug use (following either the feedback component, and/or the first component presented) were also associated with decreased likelihood of drug use (rrb = approximately −.31).
Overall, and as expected, scoring methods based on mean ratings were negatively associated with drug use at follow-up—such that higher ratings of likelihood of avoiding drug use and satisfaction with the intervention were related to less drug use. This was less true of mean ratings of the seriousness of drug use, which were at times positively associated with later use. Also as expected, changes in ratings from baseline to during-session were negatively associated with later drug use, such that increases in expected avoidance of drug use or of the seriousness of one’s drug use were both associated with less drug use at follow-up. In contrast, 7 of the 29 variables predicted drug use at follow-up in the opposite direction expected (positive correlations in Table 2); of these, 5 involved self-rated seriousness of drug use (from the item, “How big a problem is your drug use?”).
Multivariate prediction of drug use
The potential for several such variables in combination to predict outcome was evaluated by converting the five items most strongly associated with outcome (with correlations of ≥ .3, noted with a ‘†’ on Table 2) into dichotomous variables, which in all cases was based on a median split. The resulting scale was then evaluated for its ability to predict drug use outcome using an ROC curve. As seen in Figure 1, the resulting curve had an area under the curve of .87; at a cutoff of 3, this scale had a sensitivity of .70 and a specificity of .89. At a score of 2 or less on this scale (which had a range of 0 to 5), 92% of participants were positive at for drug use at follow up; at a score of 4 or more, only 37.5% of participants were positive for drug use at follow-up; none of the participants with a score of 5 were positive for drug use at follow up.
Figure 1.
ROC curve for scale made from five top items (dichotomized), predicting 4-month drug-use outcome (N = 39; AUC = .87)
Discussion
Behavioral science is just beginning to tap all the possibilities of technology. Utilizing changes in state motivation, intention, efficacy, satisfaction, etc. to predict behavioral response is one such possibility. Pilot work examining the ability of such variables to predict outcomes is an important step in evaluating the feasibility of this approach. Evidence of prediction, even under ideal circumstances, would strongly suggest that this approach has merit.
In this sample of 39 post-partum women with histories of drug use, five potential dynamic during-session predictors were associated with drug use at 4-month follow-up at rrb ≥ .3. A scale that included all five significant predictors was clearly associated with later drug use, with an AUC of .87; at a cutoff of 2, this scale had a sensitivity of .89 and a specificity of .7. Clearly, this procedure capitalizes on chance by selecting the top predictors from a larger set, in a sample with a relatively small N. As this was an exploratory study, our goal was not to confirm the significance of any particular predictor or set of predictors. Rather, our interest was in the conceptual question of whether during-session changes in state variables could potentially be used to predict later behavior.
The fact that during-session changes in state variables were able to predict later behavior in this sample is rather remarkable given the transitory nature of state variables, and the length of time between measurement of predictors and follow-up behavior. In the present analysis, all participants scoring 5 or higher on the brief index(5% of participants) were negative for drug use at follow up, and 92% of participants scoring 2 or less(50% of participants) were positive at follow-up; all participants scoring 1 or lower(16% of participants) were positive at follow-up. Should predictive ability even approximating this be demonstrated in future studies, it will be a noteworthy development. For example, developmental clinical trials could seek to maximize the number of participants showing a high likelihood of having responded (and to minimize the number showing high likelihood of not having responded). Further, the software could be programmed to provide an entirely different approach with those showing indications of not having responded well to the previous approach. Such efforts are also likely to shed important light on the mechanisms through which brief interventions result in long-term behavior change.
In examining the pattern of results, it is noteworthy that state responses to the feedback component were particularly likely to predict later drug use. Self-rated likelihood of future drug use following the feedback component, subjective satisfaction with the feedback component, and baseline to post-feedback increase in the seriousness of drug use all emerged as significant predictors of drug use. It appears that reaction to feedback may function as useful litmus test for overall brief intervention response.
Also regarding specific predictors, 5 of the 7 contrasts showing associations in the opposite of the expected direction were based on self-rated seriousness of drug use. In contrast, as noted above, increases in self-reported seriousness from baseline to during-session were significantly related to decreases in drug use at follow-up. It appears that this variable—when scored in a non-time dependent way—may function primarily as a marker for the severity of drug use. Also notable is the failure of 2 of 3 slope variables to predict later drug use in the expected direction. The pattern of results for self-reported avoidance likelihood following the first component presented (rrb = −.31) and the last component presented (rrb = .14) suggests that response following the first component presented may be more relevant than during-session increases or decreases on these variables. Regarding the utility of various scoring methods, then, it appears that average scores, changes as measured against baseline, and early reaction to the intervention may all predict later drug use. Predictions based on slope of change from early in the intervention session to the end did not fare as well in this preliminary analysis.
These findings have interesting parallels with those from counselor-delivered interventions, the efficacy of which are often strongly related to personal characteristics of the counselor(e.g., Keijsers, Schaap, & Hoogduin, 2000; Luborsky, et al., 1986)and to client ratings of therapeutic alliance(e.g., Keijsers, et al., 2000). In the present study, satisfaction with the computer-delivered brief intervention—particularly following the somewhat challenging feedback component—was negatively associated with drug use at follow-up, such that higher satisfaction ratings were associated with lower levels of drug use. For obvious reasons, constructs such as therapeutic alliance may not apply to computer-delivered interventions; but software can vary greatly in the extent to which it communicates empathy, judgment, collaborativeness, optimism, and other key characteristics. These variables may well prove to be associated with intervention efficacy.
From a theoretical perspective, there is clear interest in understanding how, when, why, and in whom a sudden critical change—leading to changes in behavior—might take place. Resnicow (Resnicow & Page, 2008; Resnicow & Vaughan, 2006)makes a compelling case that such change is often more quantum than linear, and that sudden decisions to initiate change may be the result of highly idiosyncratic and complex confluences of factors such as state characteristics, individual characteristics, cumulative experiences, values, and external influences. As such, Resnicow places human behavior change alongside what are often considered “chaotic” systems, such as epidemics, tornadoes, or recessions—none of which are easily predictable, all of which represent a sudden change that only occurs if a great number of conditions combine in a certain way, and all of which are highly sensitive to initial conditions. Applying Chaos Theory (e.g., Stewart, 2002)in this manner suggests that it may be nearly impossible to predict in whom and when a sudden determination to change will arise. However, Resnicow suggests that this theory would support (a) periodic exposure to potentially motivational stimuli, and (b) use of stimuli that are maximally tailored and relevant to that individual (Resnicow & Vaughan, 2006).
Ethical issues must also be considered. Notably, technology has yet to be proposed as a replacement for counselor contact. Rather, its use has been focused on situations in which individual counseling is neither sought nor likely to be forthcoming (e.g., medical settings), or as an adjunct to care in treatment settings (rather than as a replacement for counselor contact altogether; for example, see the work of Bickel, Marsch, Buchhalter, & Badger, 2008). Certainly, technology-based interventions face the same ethical issues as more traditional interventions and should be held to the same standards. Potential concerns with issues such as recognition of suicide risk, disclosure, and efficacy should be examined empirically, and findings from such research should be interpreted in light of the context in which the technology-based intervention is used. With respect to brief interventions, for example, context is crucial to consider; approximately 85% of all persons needing treatment for substance use have neither received any form of treatment in the past year, nor believe that they need it(Substance Abuse and Mental Health Services Administration, 2008). A range of attempts to reach this at-risk group appears to be warranted, and technology may be a well-justified part of that larger response.
In summary, there is a nearly infinite range of potential uses of technology in understanding and addressing substance use. Several of those are described above, and a particular theoretical use of technology is investigated in more detail. This exploratory investigation is limited in many ways, including sample size, generalizability, number of comparisons, and lack of cross-validation. It would be inappropriate to draw conclusions from these data regarding the predictive ability of specific variables, or the accuracy with which later behavior can be predicted by state variables as measured during single computer-delivered sessions. In spite of this, it does seem appropriate to conclude that prediction of later drug use by dynamic in-session ratings merits significant additional study.
Acknowledgments
Funding for this study was provided by grants DA00516 and DA14621 from the National Institute on Drug Abuse.
This research was supported by grants DA00516 and DA14621 from the National Institute on Drug Abuse. Preliminary results from this study were presented at the 70th Annual Scientific Meeting of the College of Problems on Drug Dependence, San Juan, Puerto Rico, June 14–19, 2008. The authors gratefully acknowledge the assistance of Mr. Wassim Tarraf in data analysis.
Glossary
- Mann-Whitney U test
A non-parametric equivalent to the t-test, appropriate for examining independence of two groups on an ordinal variable
- Perinatal period
The period surrounding childbirth
- Rank-biserial correlation
A measure of the strength of association of two variables, when one is dichotomous and the other is ordinal
- State variable
A variable that reflects current emotional, intentional, or attitudinal functioning, and that is capable of fluctuating rapidly (as opposed to the more commonly measure trait variables, which are seen as stable characteristics)
- Tablet PC
Alaptop computer with an integrated touch-screen; many are convertible, meaning that the screen can fold over the keyboard, thus allowing the user to interact only with the touch-screen
Footnotes
Conflict of Interest Notification:
No conflict of interest to report for any authors.
Contributor Information
Steven J. Ondersma, Wayne State University.
Emily R. Grekin, Wayne State University.
Dace Svikis, Virginia Commonwealth University.
References
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Exp Clin Psychopharmacol. 2008;16(2):132–143. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Chaffin M. Is it time to rethink Healthy Start/healthy families? Child Abuse & Neglect. 2004;28(6):589–595. doi: 10.1016/j.chiabu.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Copeland J, Martin G. Web-based interventions for substance use disorders; A qualitative review. J Subst Abuse Treat. 2004;26(2):109–116. doi: 10.1016/S0740-5472(03)00165-X. [DOI] [PubMed] [Google Scholar]
- Demmel R, Beck B, Richter D, Reker T. Readiness to change in a clinical sample of problem drinkers: relation to alcohol use, self-efficacy, and treatment outcome. Eur Addict Res. 2004;10(3):133–138. doi: 10.1159/000077702. [DOI] [PubMed] [Google Scholar]
- Duggan A, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse Negl. 2007;31(8):801–827. doi: 10.1016/j.chiabu.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Duggan A, Fuddy L, Burrell L, Higman SM, McFarlane E, Windham A, et al. Randomized trial of a statewide home visiting program to prevent child abuse: impact in reducing parental risk factors. Child Abuse Negl. 2004;28(6):623–643. doi: 10.1016/j.chiabu.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Duggan A, McFarlane E, Fuddy L, Burrell L, Higman SM, Windham A, et al. Randomized trial of a statewide home visiting program: impact in preventing child abuse and neglect. Child Abuse Negl. 2004;28(6):597–622. doi: 10.1016/j.chiabu.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Ciccarone D, Gansky SA, Bangsberg DR, Clanon K, McPhee SJ, et al. Interactive “Video Doctor” counseling reduces drug and sexual risk behaviors among HIV-positive patients in diverse outpatient settings. PLoS ONE. 2008;3(4):e1988. doi: 10.1371/journal.pone.0001988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomby DS. Home visitation in 2005: Outcomes for children and parents. Sunnyvale, CA: 2005. [Google Scholar]
- Hester RK, Miller JH. Computer-based tools for diagnosis and treatment of alcohol problems. Alcohol Res Health. 2006;29(1):36–40. [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. The Drinker’s Check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. J Subst Abuse Treat. 2005;28(2):159–169. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R. Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and pilot brief intervention: A technical report of phase II findings of the WHO ASSIST Project. 2006 Available from http://www.who.int/substance_abuse/activities/assist/en/index.html.
- Keijsers GP, Schaap CP, Hoogduin CA. The impact of interpersonal patient and therapist behavior on outcome in cognitive-behavior therapy. A review of empirical studies. Behav Modif. 2000;24(2):264–297. doi: 10.1177/0145445500242006. [DOI] [PubMed] [Google Scholar]
- Kiene SM, Barta WD. A brief individualized computer-delivered sexual risk reduction intervention increases HIV/AIDS preventive behavior. J Adolesc Health. 2006;39(3):404–410. doi: 10.1016/j.jadohealth.2005.12.029. [DOI] [PubMed] [Google Scholar]
- Kypri K, Saunders JB, Williams SM, McGee RO, Langley JD, Cashell-Smith ML, et al. Web-based screening and brief intervention for hazardous drinking: a double-blind randomized controlled trial. Addiction. 2004;99(11):1410–1417. doi: 10.1111/j.1360-0443.2004.00847.x. [DOI] [PubMed] [Google Scholar]
- Kypri K, Sitharthan T, Cunningham JA, Kavanagh DJ, Dean JI. Innovative approaches to intervention for problem drinking. Curr Opin Psychiatry. 2005;18(3):229–234. doi: 10.1097/01.yco.0000165591.75681.ab. [DOI] [PubMed] [Google Scholar]
- Long CG, Williams M, Midgley M, Hollin CR. Within-program factors as predictors of drinking outcome following cognitive-behavioral treatment. Addict Behav. 2000;25(4):573–578. doi: 10.1016/s0306-4603(99)00018-0. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Crits-Christoph P, McLellan AT, Woody G, Piper W, Liberman B, et al. Do therapists vary much in their success? Findings from four outcome studies. Am J Orthopsychiatry. 1986;56(4):501–512. doi: 10.1111/j.1939-0025.1986.tb03483.x. [DOI] [PubMed] [Google Scholar]
- Markovic N, Ness RB, Cefilli D, Grisso JA, Stahmer S, Shaw LM. Substance use measures among women in early pregnancy. American Journal of Obstetrics and Gynecology. 2000;183(3):627–632. doi: 10.1067/mob.2000.106450. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: Final Data for 2005. National Vital Statistics Reports. 2007;56(6) [PubMed] [Google Scholar]
- McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- Miller WR. John Henry and Motivational Interviewing: Can a computer do it? Motivational Interviewing Newsletter: Updates, Education, and Training. 2001;8(2):1–3. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York: Guilford; 2002. [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: efficacy of a computer-delivered personalized normative feedback intervention. J Consult Clin Psychol. 2004;72(3):434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Newcombe DA, Humeniuk RE, Hallet C, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and Pilot Brief Intervention. Parkside, Australia: Drug & Alcohol Services Council of Australia; 2003. [DOI] [PubMed] [Google Scholar]
- Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005;24(3):217–226. doi: 10.1080/09595230500170266. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Chase SK, Svikis DS, Schuster CR. Computer-based brief motivational intervention for perinatal drug use. J Subst Abuse Treat. 2005;28(4):305–312. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Malcoe LH, Simpson SM. Child protective services’ response to prenatal drug exposure: Results from a nationwide survey. Child Abuse & Neglect. 2001;25(5):657–668. doi: 10.1016/s0145-2134(01)00235-6. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Simpson SJ, Brestan EV, Ward M. Prenatal drug exposure and social policy: The search for an appropriate response. Child Maltreatment. 2000;5:93–108. doi: 10.1177/1077559500005002002. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Svikis DS, Schuster CR. Computer-based brief intervention a randomized trial with postpartum women. Am J Prev Med. 2007;32(3):231–238. doi: 10.1016/j.amepre.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast ML, Podus D, Chang E, Urada D. The effectiveness of drug abuse treatment: a meta-analysis of comparison group studies. Drug Alcohol Depend. 2002;67(1):53–72. doi: 10.1016/s0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Page SE. Embracing chaos and complexity: a quantum change for public health. American Journal of Public Health. 2008;98(8):1382–1389. doi: 10.2105/AJPH.2007.129460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Vaughan R. A chaotic view of behavior change: a quantum leap for health promotion. Int J Behav Nutr Phys Act. 2006;3:25. doi: 10.1186/1479-5868-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug Alcohol Depend. 2004;74(1):21–36. doi: 10.1016/j.drugalcdep.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart I. Does God Play Dice? The New Mathematics of Chaos. 2. New York: Wiley-Blackwell; 2002. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings (Vol. NSDUH Series H-34, DHHS Publication No. SMA 08–4343) Rockville, MD: 2008. [Google Scholar]
- Walters ST, Vader AM, Harris TR. A controlled trial of web-based feedback for heavy drinking college students. Prev Sci. 2007;8(1):83–88. doi: 10.1007/s11121-006-0059-9. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Zhang AY, Harmon JA, Werkner J, McCormick RA. Impacts of motivation for change on the severity of alcohol use by patients with severe and persistent mental illness. J Stud Alcohol. 2004;65(3):392–397. doi: 10.15288/jsa.2004.65.392. [DOI] [PubMed] [Google Scholar]