Abstract
Objective
There is a need for natural history chronic fatigue syndrome (CFS) studies from random, community-based, multi-ethnic populations. Design: The present study examined the course of CFS from Wave 1 to Wave 2, which spanned over a ten year period of time, and, assessed whether socio-environmental and symptomatology factors were associated with CFS status over the ten year period.
Results
There was relative stability over time on critical measures of disability, fatigue, support, optimism and coping over time. One cardinal symptoms of CFS, post-exertional malaise, best differentiated the CFS group from the others. By Wave 2, of the original group of 32 individuals diagnosed with CFS, 4 had died, and 24 were found and agreed to be re-evaluated, and of this group, 16 continued to have CFS, 5 developed exclusionary illnesses, 2 were classified as Idiopathic chronic fatigue, and one had remitted. Conclusions: The current study found that over time in a community-based sample, unbiased by help seeking behavior the CFS group remained rather ill with a variety of different conditions over time.
Keywords: Chronic fatigue syndrome, natural history, epidemiology
There is a clear need to better understand the course of CFS over time. White (2007) summarized findings from five cohort studies involving postinfectious illness. These studies indicate that a postinfectious fatigue syndrome does exist, and that it is not a mood disorder. It appears that there are two postinfectious fatigue syndromes, one characterized by excessive sleep and the other by insomnia associated with muscle and joint pain. However, many of the natural history studies that are available have either not included a physician examination and psychiatric interview (Harvey, Wadsworth, Wessely, & Hotopf, 2008), were not based on a representative sample (Friedberg, Dechene, McKenzie, & Fontanetta, 2000), or were based on relatively short follow-up periods (Hickie et al., 2006). As an example, Ciccone, Chandler, and Natelson (2010) employed a two and half year follow up with participants seen at a tertiary clinic, and they found that those with CFS and co-occurring Fibromyalgia were 3.2 times more likely to be non-improvers than those with CFS alone. There is a clear need for research on the course of CFS in ethnically and socioeconomically diverse community populations.
Epidemiologic work on CFS began with attempts to determine the prevalence of CFS. While initial studies were limited to treatment-based samples along with their methodological biases (Richman, Flaherty & Rospenda, 1994), subsequent studies addressed the prevalence of CFS in community-based samples (Jason, Richman et al. 1999; Njoku, Jason, & Torres-Harding, 2007; Reeves et al., 2007; Reyes et al. 2003). While we now have varying estimates of the prevalence of CFS, and controversies about case definitions used in such studies (Jason, Najar, Porter, & Reh, 2008), an important next epidemiologic step involves the clear need for longitudinal cohort studies with representative samples that identify risk factors for both recovery/improvement and relapse. Below we review some of the more prominent risk factors that have been associated with either CFS onset or maintenance over time.
There is a steady increase of fatigue from middle to old age (Hammond, 1964). In an influential review article, Joyce, Hotopf, and Wessely (1997) concluded that older age was a risk factor for poor prognosis among individuals with CFS. For example, Clark and associates (1995) found that being over 38 years old predicted persistent illness in participants with chronic fatigue. Tiersky et al. (2001) also found the prognosis for CFS to be poor, with age being a significant predictor of outcome. Furthermore, Schmaling, Fiedelak, Katon, Bader, and Buchwald (2003) found that older age predicted a decline in physical functioning among individuals with unexplained chronic fatigue. Finally, in the Chicago community-based sample, Jason, Taylor, Kennedy, Jordan et al. (2000) found that those participants with CFS who were older had higher frequencies of symptoms and were more severely disabled. Conceivably, those who are older are less physically fit and/or have had more time to experience other physical illnesses or stressors that can cause fatigue.
CFS is more prevalent among women than men (Jason, Richman et al., 1999; Reyes et al., 2003). In the Chicago community-based sample, gender predicted fatigue severity, with women exhibiting higher fatigue scores than men (Torres-Harding, Jason, & Taylor, 2002). Also, within this sample, women had significantly poorer physical functioning, more bodily pain, poorer emotional role functioning, significantly more severe muscle pain, and significantly greater impairment in work activities (Jason, Taylor, Kennedy, Jordan et al., 2000).
Greater numbers of minorities than expected have been found in community-based studies (Dinos et al., 2009). In a Chicago community-based study, the prevalence of CFS was higher for Latinos and African-Americans than for Caucasians (Jason, Richman et al., 1999). Symptom severity outcome measures revealed that when compared to Caucasians, minorities had more severe sore throat pain, fatigue following exercise, headaches, unrefreshing sleep, and poorer general health (Jason, Taylor, Kennedy, Jordan, et al., 2000). In addition, Latinas who were older reported the highest relative severity of fatigue (Song, Jason, & Taylor, 1999).
While CFS has frequently been referred to as the “Yuppie Disease” because it was thought to primarily affect middle to upper class women, it should be noted that these findings were obtained from tertiary care clinics (Friedberg & Jason, 1998). Bierl et al. (2004) reported on a national US study that involved 2,728 households and found that lower income and education were associated with higher levels of chronic fatigue. Moreover, Jason, Jordan et al. (1999) found that individuals in a Chicago community-based sample with lower educational and occupational status reported higher levels of fatigue than those with higher educational and occupational status. Those from the lowest SES group had significantly higher disability ratings than those from the highest SES group.
Fatigue severity is strongly implicated in a poor prognosis for CFS. This is understandable given that fatigue severity is associated with more severe Fukuda et al. (1994) somatic symptoms and functional limitations (Taylor, Jason, & Torres, 2000). In Joyce et al.'s (1997) review article of prognostic studies, fatigue severity was one of the most consistent and important predictors of a more severe illness and poorer outcome. In the Chicago community-based study, Taylor, Jason, and Curie (2002) discovered that higher baseline fatigue scores predicted higher fatigue severity at a follow-up assessment. Those who are more fatigued experience a greater number of somatic symptoms and an increase in functional limitations. These factors might likely make it more difficult to recover from CFS.
Psychological distress has been found to play a significant role in relation to the onset and/or course of many health conditions. Prospective studies have examined the relationship between chronic fatigue and psychological distress (Joyce et al., 1997). In one study, predictors of post-infectious fatigue six months following infectious illness included fatigue before infection and psychological distress before and at the time of infection (Wessely, Chalder, Hirsch, Wallace, & Wright, 1997). Bombardier and Buchwald (1995) also found the coexistence of dysthymia predicted poorer outcomes. In contrast, Hickie et al. (2006) followed up with people who had cases of mononucleosis (glandular fever), Q fever, and Ross River virus, who later met the criteria for CFS, and they found CFS was predicted largely by the severity of the acute illness rather than by psychological or demographic factors.
Stressful life events have also been implicated as a risk factor for CFS. Buchwald, Rea, Katon, Russo, and Ashley (2000) found that a greater number of stressful life events predicted a worse functional and fatigue symptom profile at six months. Lim et al. (2003) found those who recovered from CFS over one year reported lower levels of life stress than those who did not recover. Jason, Taylor, Kennedy, Song, et al. (2000) indicated that half of the individuals with CFS in their community based sample were able to identify a stressful event occurring at the time of onset.
Jason, Porter, Hunnell, Rademaker, and Richman (in press) recently examined a group of individuals in a community-based sample with risk factor data collected from 1995-1997 (Wave 1) to their diagnostic status (CFS, Idiopathic chronic fatigue (ICF) which indicates the person has 6 months of fatigue but insufficient symptoms to meet the case definition of CFS, Medical reasons for the chronic fatigue, or controls) approximately 10 years (Wave 2). The CFS group at Wave 2 had significantly more impairment than the Controls only for Wave 1 Physical Composite Score, fatigue, and several somatic symptoms but not for any of the other measures of stress, support or coping. These findings suggest that physical measures of disability and fatigue, along with measures of specific somatic symptoms, better differentiate individuals who are later diagnosed with CFS than more psychosocial measures such as stress and coping. In addition, they found those in the group whose CFS had remitted over time were significantly younger than the group that developed CFS.
There is a dearth of studies that have followed representative samples of participants with CFS over time. Jason et al. (in press) examined risk factors gathered 10 years earlier and used this information to predict differences in diagnostic outcomes (CFS, ICF, Exclusionary, controls) a decade later. In contrast, the present study examined individuals who had been diagnosed with CFS, ICF, Exclusionary, or controls between 1995 to 1997 and followed them up over the next decade. In other words, the present study examined the course of CFS and other chronic fatiguing conditions over approximately a ten year period of time, with a random, community-based, multi-ethnic population. We examined a number of factors including life stressors, female gender, older age, minority status, lower SES, and higher fatigue severity and other types of symptomatology. We therefore assessed whether these socio-environmental and the course of illness symptomatology factors might be associated with CFS status over a ten year period of time.
Method
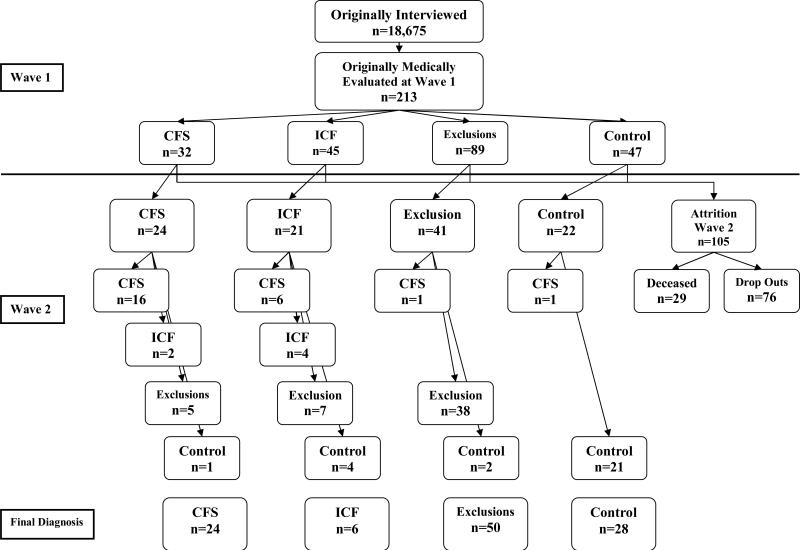
Wave 1 refers to a group of 213 individuals who were medically and psychiatrically evaluated from 1995-1997 (See Figure 1). These adults were previously evaluated in our original CFS epidemiology project (Jason, Jordan et al., 1999). The original Wave 1 sample is a stratified random sample of several neighborhoods in Chicago specifically selected to contain individuals from different ethnic and socioeconomic profiles. As a whole, Chicago, Illinois is an ethnically and socioeconomically diverse city. We sampled in eight Chicago community locations, including low socioeconomic areas such as West Garfield Park, middle-socioeconomic areas such as Bridgeport and Armour Park, gentrifying areas such as the near West Side, and high socioeconomic areas such as the Loop and the near North Side. The telephone numbers comprising the stratified random sample were obtained from Survey Sampling, Incorporated. This company generated random telephone numbers using valid Chicago exchanges, resulting in a sample of both listed and unlisted numbers (as well as business and non-working numbers). In the first stage of data collection in the original Wave 1 study, procedures developed by Kish (1965) were used to select one adult from each household for subsequent screening for CFS-like illness. Birth dates for each adult were gathered and the person with the most recent birthday was selected to be interviewed. The final sample of respondents consisted of 18,675 households. Racial data indicate that the sample consisted of 20.0% African-Americans, 52.6% Caucasians, 18.7% Latinos, 0.5% Native Americans, 5.5% Asian Americans, 1.4% multiracial individuals, and 1.3% individuals of other races (Jason, Jordan et al., 1999).
Figure 1.
Participant Group Movement from Wave 1 to Wave 2
For Wave 1, after a medical and psychiatric evaluation, we had physician consensus diagnoses for the following conditions: 32 with CFS, 45 with ICF, 89 with Exclusionary for CFS due to medically/psychiatrically explained chronic fatigue, and 47 Controls. We found that .42% of the overall sample was determined to have CFS, with rates being higher among Latino and African-American respondents compared to White respondents (Jason, Richman et al. 1999). The results of this epidemiological study suggested that this illness may affect approximately 800,000 people in the United States. Women, Latinos, middle-aged individuals, and persons of middle to lower socioeconomic status were found to be at higher risk for this illness. The findings directly contradicted the perception that middle to upper-class Caucasian women were most at risk for this illness. Moreover, about 90% of people identified as having CFS in this sample had not been previously diagnosed by a physician prior to participation in the study.
Wave 2 refers to a follow-up of this sample collected approximately 10 years later. The Wave 2 follow-up was carried out in two stages. In Stage 1, we attempted to re-contact the 213 adults who had been previously medically and psychiatrically evaluated. Stage 2 of the study encompassed a structured psychiatric assessment and a complete physical examination and a structured medical history.
Stage 1
The CFS Screening Questionnaire consists of two parts and was administered to all participants during Wave 2. It assesses participants’ sociodemographic characteristics and fatigue characteristics to determine whether any changes have occurred since the first wave of data collection in the original study. Basic demographic data included age, ethnicity, socioeconomic status, work status, marital status, parental status (including number of children) and gender. The revised scoring rules for Hollingshead's (1975) scale, developed and validated by Wasser (1991), were used to determine socioeconomic status. These scoring rules encompass explicit definitions of occupation and education. Socioeconomic status was estimated from data on occupation and education for the primary financial caretaker, resulting in the following five categories: (1) low, (2) low-middle, (3) middle, (4) middle-high, and (5) high.
Part 2 of the Stage 1 CFS Screening Questionnaire contains questions measuring more specific aspects of fatigue and health status. The questionnaire also included questions assessing the degree to which participants are experiencing each of the eight CFS symptoms as defined by the Fukuda et al. (1994) criteria. In addition, questions assessed the level of impairment that fatigue and illness cause to daily activities, as well as the frequency and duration of the fatigue. Respondents were also asked if they have ever been diagnosed with any other medical or psychiatric conditions associated with chronic fatigue and what current treatments they were receiving. A version of the screening scale used in the present study was evaluated by Jason, Ropacki et al. (1997). They recruited four groups of participants (i.e., those diagnosed with CFS, Lupus, and Multiple Sclerosis, and a healthy control group). All participants were interviewed with a screening instrument twice over a two-week period of time. The screening scale exhibited high discriminant validity and excellent test-retest and inter-rater reliability. Hawk, Jason, and Torres-Harding (2006) revised this CFS Screening Questionnaire, and administered the questionnaire to three groups (those with CFS, Major Depressive Disorder, and healthy controls). The revised instrument, which was used in the present study, evidences good test-retest reliability and has good sensitivity and specificity.
The Fatigue Scale (Chalder et al., 1993), was administered in the original Wave 1 study (Jason, Jordan, et al., 1999), and was contained within Part 1 of the Wave 2 CFS Screening Questionnaire. This scale was originally used in a hospital-based case control study (Wessely & Powell, 1989). The Fatigue Scale produces a score reflecting mental fatigue, a score reflecting physical fatigue, and an overall total score. The Fatigue Scale was further refined by Chalder et al. Despite its brevity, the scale has been found to be reliable and valid, possessing good face validity and reasonable discriminant validity. The 11-item scale is commonly scored in a continuous format. Continuous scoring codes responses according to a four-option continuum, with codes ranging from 0 to 3 and total scores ranging from 0-33 (with higher scores signifying greater fatigue). The Fatigue Scale is commonly used in community-based studies of fatigue, chronic fatigue, and CFS (Loge, Ekeberg, & Kaasa, 1998).
Stage 2
In Stage 2, the Structured Clinical Interview for the DSM-IV (SCID) (Spitzer, Williams, Gibbon, & First, 1995) was administered to assess current psychiatric diagnoses as defined on Axis I of the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM-IV) (American Psychiatric Association, 1994). The SCID was administered in both Waves 1 and 2. The SCID is a valid and reliable semi-structured interview guide that approximates a traditional psychiatric interview (First, Spitzer, Gibbon, & Williams, 1995). It has been successfully used to assess psychiatric disorders in samples of people with CFS (Taylor & Jason, 1998). For data analysis, we did not examine each specific disorder separately, but we grouped specific disorders into a more global category. While we assessed both current and lifetime psychiatric diagnoses, we only used the occurrence of one or more current psychiatric diagnoses for our hypotheses.
Following the structured psychiatric interview, participants were provided a medical history interview and complete medical examination. These procedures were followed for both Waves 1 and 2. Prior to the physical examination, the interviewer who accompanied participants and provided transportation to the medical examination administered the Medical Questionnaire at the physician's office to assess current and past medical history. The Medical Questionnaire is a modified version of The Chronic Fatigue Questionnaire, a structured instrument developed by Komaroff and Buchwald (1991) that was used in a study by Komaroff et al. (1996). This comprehensive instrument assesses symptoms related to CFS and chronic fatigue, as well as other medical and psychiatric symptoms, in order to help rule out exclusionary conditions such as HIV/AIDS, active malignancies, iatrogenic conditions resulting from the side effects of medication, unresolved cases of hepatitis, and active substance use. In addition, the Medical Questionnaire measures fatigue severity, fatigue-related social role impairment, psychosocial stressors, job satisfaction, toxic exposures prior to CFS onset, chemical sensitivities, presence of CFS or chronic fatigue in other network members, and family medical history.
Because sleep disturbances are often reported by individuals with CFS and chronic fatigue, the Sleep Disturbance Questionnaire, which has been validated experimentally in a sleep laboratory (Buchwald, Pascualy, Bombardier, & Kith, 1994), has been incorporated into the medical questionnaire to help identify participants with sleep disorders. We also used the Perceived Stress Scale (PSS), which is a reliable four-item revised version of a measure of global perceived stress. The time period that this instrument measured was the previous month (Cohen, Kamarck, & Mermelstein, 1983). We also administered the Coping Orientation to Problems Experienced Scale (COPE), which consists of five conceptually distinct scales of problem-focused coping and five conceptually distinct scales of emotion-focused coping (Carver, Scheier, & Weintraub, 1989). Respondents were asked to rate these items based upon what they think about when they are under a lot of stress. For this study, mean scores for each coping strategy were used, and higher scores indicate more use of that particular coping strategy. We also administered the revised version of the Life Orientation Test (LOT), which provided an overall score of optimism (Scheier & Carver, 1985). This measure is a well-validated scale and has a total score that ranges from 0-24, with higher scores indicating more optimism. We also administered the Social Support Questionnaire (SSQ6) (Sarason, Sarason, Shearin, & Pierce, 1987), which assesses the number of available others whom the individual feels he or she can turn to in times of need in a variety of situations (Number or Perceived Availability). The second part of each item measures the individual's degree of satisfaction (Satisfaction score) with the perceived support available in that particular situation. The internal reliabilities of the SSQ6 are .90 and .93 for Number and Satisfaction, respectively.
In addition, the Medical Outcomes Study 36-item Short-Form Survey (Ware & Sherbourne, 1992), a reliable and valid measure, was administered in Stage 2 to discriminate between gradations of disability. This instrument encompasses multi-item scales to assess Physical Functioning, Social Functioning, Role-Physical, Role-Emotional, Vitality, Bodily Pain, General Health, and Mental Health. A physical composite score was used to assess the four physical functioning scales, and a mental composite score was used to assess the four mental functioning scales. These composite scores have demonstrated adequate validity and reliability, as well as sensitivity and specificity in discriminating the gradations of health status among groups. Back-translated, Spanish language versions of all measures were administered to individuals choosing to respond in Spanish.
Following the medical history interview, the physician conducted a detailed medical examination. This examination was carried out in order to rule out exclusionary medical conditions and detect evidence of diffuse adenopathy, hepatosplenomegaly, synovitis, neuropathy, myopathy, cardiac or pulmonary dysfunction, or any other medical disorder. An 18-tender-point examination was used to test for Fibromyalgia (Goodnick & Sandoval, 1993). Laboratory tests administered to all participants included a chemistry screen (glucose, calcium, electrolytes, uric acid, liver function tests, and renal function tests), complete blood count with differential and platelet count, T4 and TSH, erythrocyte sedimentation rate, arthritic profile (which includes rheumatoid factor and antinuclear antibody), hepatitis B surface antigen, CPK, HIV screen, and urinalysis. An intra-dermal, intermediate-strength PPD skin test was applied, and a posterior-anterior chest x-ray was completed, if it was not already obtained by the participant within eight months of entering the study. At the time of evaluation, the examining physician was blinded to participants’ status with respect to initial classification based upon the Stage 1 screen. Participants were reimbursed $100.00 for the time and effort involved in participation. Participants also signed the Human Participant Consent Form.
Diagnosing CFS
At the end of Stage 2, a team of physicians was responsible for making final diagnoses. Two physicians independently rated each file according to the current U.S. definition of CFS, ICF, Exclusionary for CFS due to medically/psychiatrically explained chronic fatigue (Fukuda et al., 1994), or Control (participants with no exclusionary illness and less than 6 months of fatigue). Those with ICF had at least six months duration of fatigue, but with insufficient symptoms to meet the case definition of CFS. The Exclusionary group had chronic fatigue for at least six months duration, but with medical explanations of the fatigue including active medical conditions that explain chronic fatigue (e.g., untreated hypothyroidism), previously diagnosed medical disorders whose resolution has not been documented beyond reasonable clinical doubt, and whose continued activity may explain the chronic fatiguing illness (e.g., unresolved cases of hepatitis C). The Exclusionary group also included those with chronic fatigue for at least six months duration, but with psychiatric explanations of the fatigue (e.g., delusional disorders, schizophrenia, etc). Controls had less than 6 months of fatigue. Reviewing physicians had access to all information gathered on each participant during each of the phases of the study. Physicians who were not blind to Wave 1 status because they needed to be fully appraised of the medical history. The review panel was also provided with all results from the physical exam. If a disagreement occurred regarding whether a participant should receive a diagnosis of CFS, Idiopathic Chronic Fatigue, Exclusionary due to medically/psychiatrically explained chronic fatigue, or Controls during the physician review process, the participant's file was rated by a third physician reviewer, and the diagnosis was determined by majority rule. We used refinements of the Fukuda et al. criteria as recommended by an International Research group and the CDC (Reeves et al., 2003).
For Wave 1, we had physician consensus diagnoses for the following conditions: 32 with CFS, 45 with ICF, 89 with Exclusionary conditions, and 47 Controls. Figure 1 provides the flow of participants from Wave 1 to Wave 2. By Wave 2, of the original group of 32 individuals with CFS, 4 had died, and 24 were found and agreed to be re-evaluated (completion rate of 24/28=86%). By Wave 2, among the 45 ICF individuals at Wave 1, 4 had died, and we were able to re-evaluate 21 (completion rate of 51%). By Wave 2 among those 89 with an Exclusionary illnesses at Wave 1, 16 had died and we were able to re-evaluate 41 (completion rate of 56%). Finally, by Wave 2, among the 47 Controls at Wave 1, 5 had died, and we were able to re-evaluate 22 (completion rate of 53%).
Statistical Analyses
For continuous measures (e.g., fatigue and disability measures), we used repeated measures ANOVAs to test for whether significant overall effects occurred across the CFS, ICF, Exclusionary or Control groups and over the two time points, Waves 1 and 2. We used chi-squares for dichotomous measures (e.g., occurrence of somatic symptoms). Our particular interest was in the CFS condition versus the other three conditions. If an overall test was significant, for continuous measures, we used post-hoc Tukey tests to determine differences among conditions. We used a Bonferroni correction for dichotomous variables (with 4 groups means and 6 pair wise chi-square comparisons, we used .05/6=.0083 as our criterion for significance).
Results
Sociodemographic Characteristics
We examined Wave 1 differences between those we were able (N = 108) versus those were not able to re-evaluate at Wave 2 (N = 105), and we did not find any significant sociodemographic differences (i.e., age, SES, gender, race, marital status, education, work status). Given the high attrition rate (49%), this finding suggests that our final Wave 2 sample did not have any systematic bias.
Risk Factors associated with CFS at Wave 1 and Wave 2
We examined sociodemographic characteristics of the four Wave 1 diagnosed groups (i.e., 24 with CFS, 21 with ICF, 41 Exclusionary, and 22 Controls). In Table 1, the sociodemographic characteristics were from Wave 1. The Exclusionary group had significantly more psychiatric co-morbidity than the CFS group, whereas a significantly higher percent of the CFS group had psychiatric co-morbidity than did the Control group. The Exclusionary group in comparison to Controls had significantly lower SES scores, a significantly higher percent of women, significantly lower educational levels, and significantly more psychiatric co-morbidity. Those in the ICF group had significantly fewer men and significantly more psychiatric co-morbidity than the Controls.
Table 1.
Wave 1 Sociodemographics for Wave 1 Categorization (N=108)
| CFS (n=24) | ICF (n=21) | Exclusion (n=41) | Controls (n=22) | p | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age | 36.83 (11.95) | 39.67 (10.88) | 42.93 (10.09) | 41.41 (12.07) | |
| SES (Hollingshead) | 40.67 (16.95) | 41.95 (15.25) | 34.68 (14.18)c | 48.95 (12.11)c | ** |
| N (%) | N (%) | N (%) | N (%) | ||
| Genderbc | |||||
| Male | 8 (33.3) | 3 (14.3) | 10 (24.4) | 14 (63.6) | ** |
| Female | 16 (66.7) | 18 (85.7) | 31 (75.6) | 8 (36.4) | |
| Race | |||||
| Black | 3 (12.5) | 5 (23.8) | 9 (22) | 5 (22.7) | |
| White | 12 (50.0) | 8 (38.1) | 16.0 (39.0) | 14 (63.6) | |
| Hispanic/Latino | 8 (33.3) | 6 (28.6) | 13 (31.7) | 1 (4.5) | |
| Other | 1 (4.2) | 2 (9.5) | 3 (7.3) | 2 (9.1) | |
| Marital Status | |||||
| Married | 9 (37.5) | 10 (47.6) | 7 (17.1) | 6 (27.3) | |
| Separated/Widowed/Divorced | 6 (25.0) | 5 (23.8) | 12 (29.3) | 5 (22.7) | |
| Never Married | 9 (37.5) | 6 (28.6) | 22 (53.7) | 11 (50.0) | |
| Children | |||||
| Yes | 13 (54.2) | 14 (66.7) | 22 (53.7) | 7 (31.8) | |
| No | 11 (45.8) | 7 (33.3) | 19 (46.3) | 15 (68.2) | |
| Educationc | |||||
| H/S Degree/GED or Less | 9 (37.5) | 10 (47.6) | 19 (46.3) | 4 (18.2) | * |
| Some College/Spec. Training | 3 (12.5) | 2 (9.5) | 13 (31.7) | 3 (13.6) | |
| College/Grad Degree | 12 (50.0) | 9 (42.9) | 9 (22.0) | 15 (68.2) | |
| Work Status | |||||
| Disability/ Unemployed/Retired | 5 (20.8) | 3 (14.3) | 16 (39.0) | 2 (9.1) | |
| Student/Homemaker | 8 (33.3) | 3 (14.3) | 5 (12.2) | 2 (9.1) | |
| Part-time | 2 (8.3) | 2 (9.5) | 4 (9.8) | 3 (13.6) | |
| Full-time | 9 (37.5) | 13 (61.9) | 16 (39.0) | 15 (68.2) | |
| Psychiatric Comorbidityabcd | |||||
| Yes | 13 (54.2) | 14 (66.7) | 36 (87.8) | 5 (22.7) | *** |
| No | 11 (45.8) | 7 (33.3) | 5 (12.2) | 17 (77.3) | |
Statistically significant difference at the p < .05 level.
Statistically significant difference at the p<.01 level.
Statistically significant difference at the p<.001 level.
Statistically significant difference between CFS and Control
Statistically significant difference between ICF and Control
Statistically significant difference between Exclusion and Control
Statistically significant difference between CFS and Exclusion
Table 2 presents other risk factors from Wave 1 and Wave 2 for the four participant groups. As there were no significant group by time interaction effects for continuous measures, we examined group effects. When examining the measures of disability at Wave 1, the CFS, ICF and Exclusionary groups had significantly lower physical and mental composite scores. However, by Wave 2, only the CFS and Exclusionary groups had significantly lower scores on the physical composite, and there were no significant differences across groups for the mental composite scores. For fatigue scores at Wave 1, the CFS, ICF and Exclusionary groups again had significantly more fatigue than the controls, but by Wave 2, only the CFS and ICF group was significantly lower than the Controls (and the Exclusionary group had significantly lower fatigue than the CFS group). The ICF and Exclusionary group had higher stress at Wave 1, but there were no significantly differences by Wave 2. For social support, significant differences only emerged for Wave 1, with the CFS group having more numbers and satisfaction than the Exclusionary group, and the Exclusionary group had less satisfaction than Controls. The ICF and Exclusionary group had significantly less optimism than the Controls at Wave 1, but by Wave 2, only the Exclusionary group had less optimism. In regard to coping, at Wave 1, the ICF and Exclusionary group vented significantly more than Controls, but by Wave 2 there were no significant differences. For denial, there were no significant differences at Wave 1, but the Exclusionary group used more denial at Wave 2. Finally, for behavioral disengagement, the Exclusionary group had significantly higher scores at Wave 1 and 2 compared to Controls, and the CFS group had significantly higher scores than Controls just for Wave 2.
Table 2.
Wave l and Wave 2 Risk Factors at Wave 1 Categorization (N=108)
| CFS (n=24) | ICF (n=21) | Exclusion (n=41) | Controls (n=22) | p | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Wave 1 MOS | |||||
| Physical Composite | 34.54 (8.75)a | 40.51 (9.97)b | 38.44 (9.90)c | 49.72 (11.50)abc | *** |
| Mental Composite | 38.08 (10.19)a | 38.38 (11.17)b | 34.38 (9.60)c | 48.16 (11.98)abc | *** |
| Wave 2 MOS | |||||
| Physical Composite | 35.95 (11.19)a | 43.39 (9.68) | 38.49 (9.68)c | 38.39 (9.68)ac | *** |
| Mental Composite | 40.90 (12.29) | 44.74 (12.60) | 40.45 (11.25) | 47.40 (10.50) | |
| Wave 1 Fatigue | 20.38 (5.16)a | 20.86 (6.28)b | 19.98 (4.81)c | 13.73 (3.93)abc | *** |
| Wave 2 Fatigue | 20.56 (5.44)ad | 18.58 (7.33)b | 16.35 (5.35)d | 12.91 (3.07)ab | *** |
| Wave 1 Perceived Stress | 7.36 (3.53) | 8.95 (3.47)b | 8.67 (2.99)c | 4.86 (3.30)bc | *** |
| Wave 2 Perceived Stress | 6.39 (3.16) | 6.50 (3.86) | 7.00 (2.82) | 5.18 (3.20) | |
| Wave 1 Social Support | |||||
| Number of Social Supports | 3.27 (1.79)d | 2.24 (1.54) | 1.97 (1.47)d | 2.97 (2.03) | * |
| Satisfaction with Social Supports | 5.54 (.79)d | 5.32 (.70) | 4.59 (1.27)cd | 5.62 (.87)c | *** |
| Wave 2 Social Support | |||||
| Number of Social Supports | 3.54 (2.56) | 3.72 (3.31) | 2.91 (2.08) | 3.67 (2.36) | |
| Satisfaction with Social Supports | 4.86 (1.56) | 5.32 (.99) | 5.03 (1.10) | 5.53 (.48) | |
| Wave 1 Optimism | |||||
| Life Orientation Test | 15.86 (4.60) | 14.75 (4.40)b | 13.36 (4.50)c | 18.64 (3.49)bc | *** |
| Wave 2 Optimism | |||||
| Life Orientation Test Score | 15.12 (3.59) | 15.13 (5.14) | 13.86 (4.21)c | 18.59 (3.81)c | *** |
| Wave 1 Cope | |||||
| Seeking Social Support | 2.26 (.94) | 2.54 (.91) | 2.45 (.86) | 2.85 (.82) | |
| Positive Reinterpretation And Growth | 2.92 (.67) | 2.98 (.79) | 2.87 (.74) | 3.21 (.80) | |
| Acceptance | 2.99 (.61) | 2.89 (.56) | 2.99 (.72) | 2.89 (.71) | |
| Turning to Religion | 2.69 (1.13) | 2.76 (1.20) | 3.09 (1.03) | 2.97 (1.19) | |
| Venting | 2.56 (.55) | 2.93 (.79)b | 2.76 (.75)c | 2.26 (.62)bc | * |
| Denial | 2.03 (.95) | 1.91 (.78) | 1.91 (.80) | 1.64 (.61) | |
| Behavioral Disengagement | 1.86 (.88) | 1.88 (.60) | 2.21 (.79)c | 1.38 (.40)c | ** |
| Wave 2 Cope | |||||
| Seeking Social Support | 2.43 (1.07) | 2.27 (1.03) | 2.53 (.83) | 2.57 (.74) | |
| Positive Reinterpretation And Growth | 3.01 (.90) | 2.85 (.90) | 2.92 (.68) | 2.97 (.62) | |
| Acceptance | 2.93 (.73) | 2.61 (.70) | 3.08 (.59) | 2.81 (.67) | |
| Turning to Religion | 2.35 (1.13) | 2.52 (1.12) | 2.97 (.99) | 2.19 (1.27) | |
| Venting | 2.28 (.80) | 2.55 (.88) | 2.51 (.64) | 2.16 (.77) | |
| Denial | 1.78 (.71) | 1.67 (.75) | 1.86 (.79)c | 1.30 (.63)c | * |
| Behavioral Disengagement | 2.04 (.70)a | 1.80 (.76) | 2.03 (.70)c | 1.28 (.35)ac | *** |
Statistically significant difference at the p < .05 level.
Statistically significant difference at the p<.01 level.
Statistically significant difference at the p<.001 level.
Statistically significant difference between CFS and Control
Statistically significant difference between ICF and Control
Statistically significant difference between Exclusion and Control
Statistically significant difference between CFS and Exclusion
For Other Diagnoses, Table 3 indicates that there were significant differences for muscle weakness; with the CFS and Exclusionary group having significantly higher percentages than controls (these data were analyzed using 4 × 4 cross-tabulations with chi-squared statistics). There were significant group differences for the multiple chemical sensitivities category, with the CFS, ICF, and Exclusionary group having significantly higher percentages than Controls. Finally, there were significant differences for the insomnia condition, with the CFS and Exclusionary group being significantly different than controls.
Table 3.
Difference Scores of Dichotomous Variables for Wave 1 Categorization
| CFS (n=24) % | ICF (n=21) % | Exclusion (n=41) % | Controls (n=22) % | p | |
|---|---|---|---|---|---|
| Other Diagnoses | |||||
| Muscle Weaknessab | |||||
| No to Yes | 0.0 | 15.4 | 20.0 | 4.8 | *** |
| Yes to No | 12.5 | 38.5 | 22.9 | 14.3 | |
| No to No | 12.5 | 15.4 | 17.1 | 66.7 | |
| Yes to Yes | 75.0 | 30.8 | 40.0 | 14.3 | |
| Multiple Chemical Sensitivitiesabc | |||||
| No to Yes | 17.6 | 11.8 | 10.0 | 13.6 | ** |
| Yes to No | 17.6 | 23.5 | 5.0 | 0.0 | |
| No to No | 29.4 | 17.6 | 37.5 | 77.3 | |
| Yes to Yes | 35.3 | 47.1 | 47.5 | 9.1 | |
| Insomniaac | |||||
| No to Yes | 19.0 | 22.2 | 22.5 | 27.3 | ** |
| Yes to No | 23.8 | 27.8 | 17.5 | 4.5 | |
| No to No | 14.3 | 33.3 | 20.0 | 63.6 | |
| Yes to Yes | 42.9 | 16.7 | 40.0 | 4.5 | |
| Irritable Bladder | |||||
| No to Yes | 5.6 | 5.9 | 10.0 | 13.6 | |
| Yes to No | 16.7 | 17.6 | 17.5 | 0.0 | |
| No to No | 61.1 | 76.5 | 62.5 | 86.4 | |
| Yes to Yes | 16.7 | 0.0 | 10.0 | 0.0 | |
| Hypersomnia | |||||
| No to Yes | 9.5 | 5.6 | 15.0 | 4.5 | |
| Yes to No | 19.0 | 11.1 | 27.5 | 18.2 | |
| No to No | 52.4 | 66.7 | 40.0 | 72.2 | |
| Yes to Yes | 19.0 | 16.7 | 17.5 | 4.5 | |
| Irritable Bowel Syndrome | |||||
| No to Yes | 11.1 | 23.5 | 7.5 | 9.1 | |
| Yes to No | 0.0 | 0.0 | 2.5 | 4.5 | |
| No to No | 72.0 | 52.9 | 75.0 | 86.4 | |
| Yes to Yes | 16.7 | 23.5 | 15.0 | 0.0 | |
| Fibromyalgia | |||||
| No to Yes | 5.6 | 5.6 | 0.0 | 0.0 | |
| Yes to No | 11.1 | 16.7 | 8.6 | 0.0 | |
| No to No | 77.8 | 72.2 | 91.4 | 100.0 | |
| Yes to Yes | 5.6 | 5.6 | 0.0 | 0.0 | |
| Mononucleosis | |||||
| No to Yes | 0.0 | 0.0 | 2.5 | 4.5 | |
| Yes to No | 0.0 | 0.0 | 5.0 | 0.0 | |
| No to No | 72.8 | 94.1 | 87.5 | 95.5 | |
| Yes to Yes | 22.2 | 5.9 | 5.0 | 0.0 | |
| Hepatitis | |||||
| No to Yes | 0.0 | 0.0 | 0.0 | 0.0 | |
| Yes to No | 5.6 | 0.0 | 0.0 | 4.5 | |
| No to No | 88.9 | 100.0 | 92.5 | 95.5 | |
| Yes to Yes | 5.6 | 0.0 | 7.5 | 0.0 | |
| Blood Transfusion | |||||
| No to Yes | 11.8 | 0.0 | 10.5 | 0.0 | |
| Yes to No | 0.0 | 0.0 | 0.0 | 4.8 | |
| No to No | 70.6 | 88.2 | 81.6 | 81.0 | |
| Yes to Yes | 17.6 | 11.8 | 7.9 | 14.3 | |
| Fukuda Symptoms | |||||
| Unrefreshing Sleepabc | |||||
| No to Yes | 10.0 | 12.5 | 8.1 | 17.6 | *** |
| Yes to No | 5.0 | 12.5 | 21.6 | 0.0 | |
| No to No | 0.0 | 12.5 | 0.0 | 64.7 | |
| Yes to Yes | 85.0 | 62.5 | 70.3 | 17.6 | |
| Impaired Memory or Concentrationabce | |||||
| No to Yes | 5.0 | 11.8 | 14.3 | 25.0 | *** |
| Yes to No | 0.0 | 41.2 | 17.1 | 5.0 | |
| No to No | 0.0 | 17.6 | 14.3 | 65.0 | |
| Yes to Yes | 95.0 | 29.4 | 54.3 | 5.0 | |
| Muscle Pain | |||||
| No to Yes | 0.0 | 13.3 | 23.1 | 10.5 | |
| Yes to No | 11.1 | 20.0 | 20.5 | 15.8 | |
| No to No | 5.6 | 20.0 | 5.1 | 57.9 | |
| Yes to Yes | 83.3 | 46.7 | 51.3 | 15.8 | |
| Headachesac | |||||
| No to Yes | 11.1 | 0.0 | 3.0 | 11.1 | ** |
| Yes to No | 38.9 | 17.6 | 33.3 | 5.6 | |
| No to No | 11.1 | 29.4 | 15.2 | 61.1 | |
| Yes to Yes | 38.9 | 52.9 | 48.5 | 22.2 | |
| Joint Painc | |||||
| No to Yes | 11.1 | 18.8 | 18.9 | 23.8 | * |
| Yes to No | 11.1 | 12.5 | 10.8 | 14.3 | |
| No to No | 16.7 | 18.8 | 10.8 | 47.6 | |
| Yes to Yes | 61.1 | 50.0 | 59.5 | 14.3 | |
| Post Exertional Malaiseade | |||||
| No to Yes | 23.5 | 18.8 | 13.2 | 5.3 | *** |
| Yes to No | 29.4 | 25.0 | 18.4 | 10.5 | |
| No to No | 0.0 | 50.0 | 44.7 | 78.9 | |
| Yes to Yes | 47.1 | 6.3 | 23.7 | 5.3 | |
| Sore Throat | |||||
| No to Yes | 20.0 | 12.5 | 22.9 | 19.0 | |
| Yes to No | 26.7 | 25.0 | 28.6 | 14.3 | |
| No to No | 26.7 | 37.5 | 34.3 | 52.4 | |
| Yes to Yes | 26.7 | 25.0 | 14.3 | 14.3 | |
| Lymph Node Painad | |||||
| No to Yes | 26.3 | 8.3 | 0.0 | 0.0 | ** |
| Yes to No | 10.5 | 16.7 | 15.2 | 0.0 | |
| No to No | 36.8 | 66.7 | 75.8 | 88.9 | |
| Yes to Yes | 26.3 | 8.3 | 9.1 | 11.1 |
Statistically significant difference at the p < .05 level.
Statistically significant difference at the p<.01 level.
Statistically significant difference at the p<.001 level.
Statistically significant difference between CFS and Control
Statistically significant difference between ICF and Control
Statistically significant difference between Exclusion and Control
Statistically significant difference between CFS and Exclusion
Statistically significant difference between CFS and ICF
Finally, there were significant differences for 6 of the eight core CFS symptoms as defined by the Fukuda et al. (1994) criteria (See Table 3). For unrefreshing sleep, and impaired memory and concentration; the CFS, ICF and Exclusionary groups were significantly different from the Controls (also for impaired memory and concentration, the CFS group was significantly different from the ICF group). For headaches, and joint pain, the Exclusionary group was significantly different from the Controls and the CFS group significantly differed from the Control group for headaches. For post exertional malaise, the CFS group was significantly different than Controls, ICF and the Exclusionary groups (this was the only variable where the CFS group was significantly different from the other three conditions). Finally, for lymph node pain, the CFS group differed from the Control and Exclusionary groups.
Discussion
The failure to find significant group by time interaction effects suggests that there was little differential movement among the four groups over time. What this suggests is that there is relative stability, at least among the basic standings, on these critical measures of disability, fatigue, support, optimism and coping over time. However, there was considerable movement in the categories over time. For example by Wave 2, of the original group of 32 individuals diagnosed with CFS, 4 had died, and 24 were found and agreed to be re-evaluated, and of this group, only 16 continued to have CFS (5 developed exclusionary illnesses, 2 were classified as ICF, and one had remitted). What this suggests is that the CFS group for the most part remained rather ill, with a variety of different conditions over time.
Still, there were important differences among the conditions both at Waves 1 and 2. There were clearly more significant differences among the groups at Wave 1 than Wave 2. For example, the CFS, ICF and Exclusionary groups had significantly worse physical composite, mental composite, and fatigue scores at Wave 1, but by Wave 2, only the CFS and Exclusionary groups had significantly worse scores on the physical composite, and there were no significant differences across groups for the mental composite scores. For fatigue scores by Wave 2, only the CFS and ICF groups were significantly worse than the Controls. For stress, support and optimism, several significant Wave 1 differences emerged, but by Wave 2, the CFS group was no longer significantly different from any of the other groups. For coping, there were few significant differences among the groups at Wave 1 and Wave 2 and the CFS group only differed from the Controls at Wave 2 for behavioral disengagement.
Regarding sociodemographic findings, the ICF group a decade earlier had significantly more women and psychiatric co-morbidity than in the Control group. Our findings also indicated that when compared to the Control group, the Exclusionary group had significantly more women, lower SES and education level, but higher psychiatric co-morbidity. In general, the Exclusionary group appeared to be at the highest risk on these sociodemographic variables. The CFS group was only significantly different than the Exclusionary group on psychiatric comorbidity, which was expected. Because race was not significantly different, it is important to note that this was a diverse population, with only the control group having more than 50% of participants reporting themselves as white (50% of CFS, 38.1% of ICF, and 39% of Exclusions).
Our study found significant differences for 6 of the 8 core Fukuda et al. (1994) symptoms. However, among all the variables in this study, only for post-exertional malaise did the CFS group significantly differ from the other three conditions. This reaffirms the importance of this being a cardinal and critical symptom for CFS, and all of the individuals in the CFS group had this symptom either at Waves 1 or 2. For unrefreshing sleep and impaired memory and concentration, 100% of the CFS group had these symptoms at Wave 1 or Wave 2. Similar to post-exertional malaise, these results support the idea that unrefreshing sleep and impaired memory and concentration are core symptoms of CFS. It is of interest that these two symptoms are also considered core symptoms of the Canadian ME/CFS Clinical Case definition (Carruthers et al., 2003). For unrefreshing sleep and impaired memory and concentration, it is important to note that the CFS, ICF and Exclusionary groups were significantly different from the Control, so these symptoms might not be as unique in differentiating CFS from other conditions as it post-exertional malaise. For headaches and lymph node pain, the Exclusionary group was significantly different from the Controls, and the CFS group was significantly different than the Controls on headaches. Of particular interest is that the CFS and ICF groups were only significantly different on post-exertional malaise and impaired memory and concentration, and the CFS group had more participants exhibiting the symptoms than in the ICF group. This suggests that these two central features may distinguish CFS and ICF participants.
For Other Diagnoses, significant differences only emerged for muscle weakness, multiple chemical sensitivities and insomnia. For muscle weakness and multiple chemical sensitivities, the CFS and ICF groups had significantly higher percentages than controls (the Exclusionary group also was higher than Controls for multiple chemical sensitivities). For the insomnia condition, the CFS and Exclusionary groups were significantly different from controls. It was of interest that from 19% to 27.3% of individuals within groups went on to develop insomnia over time. Moreover, the controls had the highest percentage of participants developing insomnia, but still the highest percentage without insomnia (only 14.3% of the CFS group did not have insomnia at Wave 1 or Wave 2). Although there were no significant differences for blood transfusions, those in the CFS group had 29.4% which was the highest percentage among the groups. Also, though not significant, 22.2% of those in the CFS group had mononucleosis, which was also the highest percentage. Although the percentage of those with fibromyalgia was highest in the CFS and ICF groups, in general these percentages are relatively low compared to findings from other tertiary care settings.
There is a dearth of studies that have followed representative samples of participants with CFS over time, and the present study adds to the literature on the natural history of CFS over time. This study supports other findings when risk factors at Wave 1 were used to predict status 10 years later, and in that study, the CFS group only had significantly more impairment than the Controls for the physical composite index and the fatigue scores, but for none of the measures of stress, support or coping. Moreover, after examining the difference scores from Wave 1 to Wave 2, it is clear that there are many differences between the CFS and Control groups regarding illness progression and recovery. Also of interest, the symptom post-exertional malaise appears to be unique in differentiating CFS from the other groups, and this symptom is required for a diagnosis of ME/CFS based on the Canadian ME/CFS criteria (Carruthers et al., 2003). However, post-exertional malaise is not required for the Fukuda et al. (1994) case definition, as with this CFS criteria, individuals only need to meet 4 out of 8 symptoms for a diagnosis, of which only one of these 8 symptoms is post-exertional malaise. Limitations in this study include the small sample sizes, and the focus on psychological and self-report measures. Future papers will incorporate findings from more biological measures.
Acknowledgments
The authors appreciate the financial assistance provided by the National Institute of Allergy and Infectious Diseases (grant number AI055735).
Footnotes
Jason, L.A., Porter, N., Hunnell, J., Brown, A., Rademaker, A., & Richman, J.A. (2011). A natural history study of chronic fatigue syndrome. Rehabilitation Psychology, 56, 32-42. PMID: 21401284
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: 1994. [Google Scholar]
- Bierl C, Nisenbaum R, Hoaglin DC, Randall B, Jones AB, Unger ER, Reeves WC. Regional distribution of fatiguing illnesses in the United States: A pilot study. Population Health Metrics. 2004;2:1. doi: 10.1186/1478-7954-2-1. ( http://www.pophealthmetrics.com/content/2/1/1) [DOI] [PMC free article] [PubMed]
- Bombardier CH, Buchwald D. Outcome and prognosis of patients with chronic fatigue versus chronic fatigue syndrome. Archives of Internal Medicine. 1995;155:2105–2110. [PubMed] [Google Scholar]
- Buchwald D, Pascualy R, Bombardier C, Kith P. Sleep disorders in patients with chronic fatigue syndrome. Clinical Infectious Disease. 1994;18:S68–S72. doi: 10.1093/clinids/18.supplement_1.s68. [DOI] [PubMed] [Google Scholar]
- Buchwald DS, Rea TD, Katon WJ, Russo JE, Ashley RL. Acute infectious mononucleosis: Characteristics of patients who report failure to recover. The American Journal of Medicine. 2000;109(7):531–537. doi: 10.1016/s0002-9343(00)00560-x. [DOI] [PubMed] [Google Scholar]
- Carruthers BM, Jain AK, DeMeirleir KL, Peterson DL, Klimas NG, Lerner AM, et al. Myalgic Encephalomyelitis/chronic fatigue syndrome: Clinical working case definition, diagnostic and treatments protocols. Journal of Chronic Fatigue Syndrome. 2003;11:7–115. [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP. Development of a fatigue scale. Journal of Psychosomatic Medicine. 1993;37(2):147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- Ciccone DS, Chandler HK, Natelson BH. Illness trajectories in the chronic fatigue syndrome: a longitudinal study of improvers versus non-improvers. Journal of Nervous and Mental Disease. 2010;198:486–493. doi: 10.1097/NMD.0b013e3181e4ce0b. [DOI] [PubMed] [Google Scholar]
- Clark MR, Katon W, Russo J, Kith P, Sintay M, Buchwald D. Chronic fatigue: Risk factors for symptom persistence in a two and a half year follow-up study. American Journal of Medicine. 1995;98:187–195. doi: 10.1016/S0002-9343(99)80403-3. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamark T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;37(2):147–153. [PubMed] [Google Scholar]
- Dinos S, Khoshaba B, Ashby D, White PD, Nazroo J, Wessely S, Bhui KS. A systematic review of chronic fatigue, its syndromes and ethnicity: Prevalence, severity, comorbidity and coping. International Journal of Epidemiology. 2009;38:1554–70. doi: 10.1093/ije/dyp147. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient edition. Biometrics Research Department; New York: 1995. [Google Scholar]
- Friedberg F, Dechene L, McKenzie MJ, II, Fontanetta R. Symptom patterns in long-duration chronic fatigue syndrome. Journal of Psychosomatic Research. 2000;48:59–68. doi: 10.1016/s0022-3999(99)00077-x. [DOI] [PubMed] [Google Scholar]
- Friedberg F, Jason LA. Understanding chronic fatigue syndrome: An empirical guide to assessment and treatment. American Psychological Association; Washington, D.C.: 1998. [Google Scholar]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- Goodnick PJ, Sandoval R. Psychotropic treatment of chronic fatigue syndrome and related disorders. The Journal of Clinical Psychiatry. 1993;54(1):13–20. [PubMed] [Google Scholar]
- Hammond E. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. American Journal of Public Health. 1964;54:11–23. doi: 10.2105/ajph.54.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey SB, Wadsworth M, Wessely S, Hotopf M. Etiology of chronic fatigue syndrome: Testing popular hypotheses using a national birth cohort study. Psychosomatic Medicine. 2008;70:488–495. doi: 10.1097/PSY.0b013e31816a8dbc. [DOI] [PubMed] [Google Scholar]
- Hawk C, Jason LA, Torres-Harding S. Differential diagnosis of chronic fatigue syndrome and major depressive disorder. International Journal of Behavioral Medicine. 2006;13:244–251. doi: 10.1207/s15327558ijbm1303_8. [DOI] [PubMed] [Google Scholar]
- Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Lloyd A. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Medical Journal. 2006 doi: 10.1136/bmj.38933.585764.AE. doi:10.1136/bmj.38933.585764.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. 1975. (Unpublished manuscript, available from Department of Sociology, Yale University, New Haven, CT).
- Jason LA, Jordan KM, Richman JA, Rademaker AW, Huang C, McCready W, Frankenberry EL. A community-based study of prolonged and chronic fatigue. Journal of Health Psychology. 1999;4:9–26. doi: 10.1177/135910539900400103. [DOI] [PubMed] [Google Scholar]
- Jason LA, Najar N, Porter N, Reh C. Evaluating the Centers for Disease Control's empirical chronic fatigue syndrome case definition. Journal of Disability Policy Studies. 2008 doi:10.1177/1044207308325995. [Google Scholar]
- Jason LA, Porter N, Hunnell J, Rademaker AW, Richman JA. CFS prevalence and risk factors over time. Journal of Health Psychology. doi: 10.1177/1359105310383603. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Richman JA, Rademaker AW, Jordan KM, Plioplys AV, Taylor R, Plioplys S. A community-based study of chronic fatigue syndrome. Archives of Internal Medicine. 1999;159:2129–2137. doi: 10.1001/archinte.159.18.2129. [DOI] [PubMed] [Google Scholar]
- Jason LA, Ropacki MT, Santoro NB, Richman JA, Heatherly W, Taylor R, Plioplys S. A screening scale for chronic fatigue syndrome: Reliability and validity. Journal of Chronic Fatigue Syndrome. 1997;3:39–59. [Google Scholar]
- Jason LA, Taylor RR, Kennedy CL, Song S, Johnson D, Torres S. Chronic fatigue syndrome: Occupation, medical utilization, and subtypes in a community based sample. The Journal of Nervous and Mental Disease. 2000;188:568–576. doi: 10.1097/00005053-200009000-00002. [DOI] [PubMed] [Google Scholar]
- Jason LA, Taylor RR, Kennedy CL, Jordan K, Song S, Johnson D, Torres S. Chronic fatigue syndrome: Sociodemographic subtypes in a community-based sample. Evaluation and the Health Professions. 2000;23:243–263. doi: 10.1177/01632780022034598. [DOI] [PubMed] [Google Scholar]
- Joyce J, Hotopf M, Wessely S. The prognosis of chronic fatigue and chronic fatigue syndrome: A systematic review. Quarterly Journal of Medicine. 1997;90:223–233. doi: 10.1093/qjmed/90.3.223. [DOI] [PubMed] [Google Scholar]
- Kish L. Survey Sampling. Wiley; N.Y.: 1965. [Google Scholar]
- Komaroff AL, Buchwald D. Symptoms and signs of chronic fatigue syndrome. Review of Infectious Diseases. 1991;13:S8–S11. doi: 10.1093/clinids/13.supplement_1.s8. [DOI] [PubMed] [Google Scholar]
- Komaroff AL, Fagioli LR, Geiger AM, Doolittle TH, Lee J, Kornish J, Guerriero RT. An examination of the working case definition of chronic fatigue syndrome. American Journal of Medicine. 1996;100:56–64. doi: 10.1016/s0002-9343(96)90012-1. [DOI] [PubMed] [Google Scholar]
- Lim BR, Tan SY, Zheng YP, Lin KM, Park BC, Turk AA. Psychosocial factors in chronic fatigue syndrome among Chinese Americans: A longitudinal community-based study. Transcultural Psychiatry. 2003;40:429–441. doi: 10.1177/13634615030403006. [DOI] [PubMed] [Google Scholar]
- Loge JH, Ekeberg O, Kaasa S. Fatigue in the general population: Normative data and associations. Journal of Psychosomatic Research. 1998;45:53–65. doi: 10.1016/s0022-3999(97)00291-2. [DOI] [PubMed] [Google Scholar]
- Njoku MGC, Jason LA, Torres-Harding SR. The prevalence of chronic fatigue syndrome in Nigeria. Journal of Health Psychology. 2007;12:461–474. doi: 10.1177/1359105307076233. [DOI] [PubMed] [Google Scholar]
- Nisenbaum R, Jones JF, Unger ER, Reyes M, Reeves WC. A population-based study of the clinical course of chronic fatigue syndrome. Health and Quality of Life Outcomes. 2003;1:49. doi: 10.1186/1477-7525-1-49. (Available at http://www.hqlo.com/content/1/1/49) [DOI] [PMC free article] [PubMed]
- Reeves WC, Lloyd A, Vernon SD, Klimas N, Jason L, Bleijenberg G, Unger ER. Identification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution. BMC Health Services Research. 2003;3:25. doi: 10.1186/1472-6963-3-25. ( http://www.biomedcentral.com/content/pdf/1472-6963-3-25.pdf) [DOI] [PMC free article] [PubMed]
- Reeves WC, Jones JJ, Maloney E, Heim C, Hoaglin DC, Boneva R, Devlin R. New study on the prevalence of CFS in metro, urban and rural Georgia populations. Population Health Metrics. 2007;5:5. doi: 10.1186/1478-7954-5-5. 2007. doi:10.1186/1478-7954-5-5: (available at: http://www.pophealthmetrics.com/content/5/1/5) [DOI] [PMC free article] [PubMed]
- Reyes M, Nisenbaum R, Hoaglin DC, Unger ER, Emmons C, Randall B, Reeves WC. Prevalence and incidence of chronic fatigue syndrome in Wichita, Kansas. Archives of Internal Medicine. 2003;163:1530–1536. doi: 10.1001/archinte.163.13.1530. [DOI] [PubMed] [Google Scholar]
- Richman JA, Flaherty JA, Rospenda KM. Chronic Fatigue Syndrome: Have flawed assumptions been derived from treatment-based studies? American Journal of Public Health. 1994;84:282–284. doi: 10.2105/ajph.84.2.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4:497–510. [Google Scholar]
- Scheier M, Carver C. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Schmaling KB, Fiedelak BA, Katon WJ, Bader JO, Buchwald DS. Prospective study of the prognosis of unexplained chronic fatigue in a clinic-based cohort. Psychosomatic Medicine. 2003;65:1047–1054. doi: 10.1097/01.psy.0000088587.29901.69. [DOI] [PubMed] [Google Scholar]
- Song S, Jason LA, Taylor RR. The relationship between ethnicity and fatigue in a community-based sample. Journal of Gender, Culture, and Health. 1999;4:255–268. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-IV – Non-Patient Edition (SCID-NP, Version 2.0) American Psychiatric Press; Washington DC: 1995. [Google Scholar]
- Taylor R, Jason LA. Comparing the DIS with the SCID: Chronic fatigue syndrome and psychiatric comorbidity. Psychology and Health: The International Review of Health Psychology. 1998;13:1087–1104. [Google Scholar]
- Taylor RR, Jason LA, Curie CJ. The prognosis of chronic fatigue in a community-based sample. Psychosomatic Medicine. 2002;64:319–327. doi: 10.1097/00006842-200203000-00016. [DOI] [PubMed] [Google Scholar]
- Taylor RR, Jason LA, Torres A. Fatigue rating scales: An empirical comparison. Psychological Medicine. 2000;30:849–856. doi: 10.1017/s0033291799002500. [DOI] [PubMed] [Google Scholar]
- Tiersky LA, DeLuca J, Hill N, Dhar SK, Johnson SK, Lange G, Natelson BH. Longitudinal assessment of neuropsychological functioning, psychiatric status, functional disability and employment status in chronic fatigue syndrome. Applied Neuropsychology. 2001;8:41–50. doi: 10.1207/S15324826AN0801_6. [DOI] [PubMed] [Google Scholar]
- Torres-Harding S, Jason LA, Taylor RR. Fatigue severity, attributions, medical utilization, and symptoms in persons with chronic fatigue. Journal of Behavioral Medicine. 2002;25:99–113. doi: 10.1023/a:1014850819995. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): Conceptual framework and item selection. Medical Care. 1992:473–483. June. [PubMed] [Google Scholar]
- Wasser TE. Statistical correction of Hollingshead's four factor index of social status.. Paper presented at the American Psychological Association; San Francisco, CA. 1991, August. [Google Scholar]
- Wessely S, Chalder T, Hirsch S, Wallace P, Wright D. The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: A prospective primary care study. American Journal of Public Health. 1997;87:1449–1455. doi: 10.2105/ajph.87.9.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessely S, Powell R. Fatigue syndromes: A comparison of chronic ‘postviral’ fatigue with neuromuscular and affective disorders. Journal of Neurology, Neurosurgery and Psychiatry. 1989;52:940–948. doi: 10.1136/jnnp.52.8.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White PD. What causes prolonged fatigue after infectious mononucleosis—and does it tell us anything about chronic fatigue syndrome. Journal of Infectious Diseases. 2007;196:4–5. doi: 10.1086/518615. [DOI] [PubMed] [Google Scholar]