Abstract
Background
Physicians often do not provide adequate medication counseling.
Purpose
To develop and evaluate an educational program to improve physicians’ assessment of adherence and their medication counseling skills, with attention to health literacy.
Methods
We compared internal medicine residents’ confidence and counseling behaviors, measured by self-report at baseline and one month after participation in a two-hour interactive workshop.
Results
Fifty-four residents participated; 35 (65%) completed the follow-up survey. One month after training, residents reported improved confidence in assessing and counseling patients (p<0.001), including those with low health literacy (p<0.001). Residents also reported more frequent use of desirable behaviors, such as assessing patients’ medication understanding and adherence barriers (p<0.05 for each), addressing costs when prescribing (p<0.01), suggesting adherence aids (p<0.01), and confirming patient understanding with teach-back (p<0.05).
Conclusion
A medication counseling workshop significantly improved residents’ self-reported confidence and behaviors regarding medication counseling one month later.
Keywords: medication adherence, health literacy, health communication
Approximately 50% of patients do not take medications as prescribed (1, 2). This can lead to poor control of chronic diseases and worse health outcomes, including higher mortality (3, 4). Patients with low health literacy are at particular risk of misunderstanding medication instructions (5, 6), and this lack of understanding may be associated with worse medication adherence (7, 8).
Physicians often are not fully aware of patients’ non-adherence, in part because they do not adequately assess patients’ medication use during routine office visits (9, 10). Physicians also commonly fail to provide appropriate counseling about prescription medications (11–14). For example, when prescribing a new medication, physicians often do not discuss the medication's name (missing 26% of the time), purpose (13%), dosing instructions (42–45%), potential adverse effects (65%), or cost (88%) (15, 16). In both inpatient and outpatient settings, patients rate physicians’ consideration of their desire and ability to comply with treatment recommendations lower than other aspects of physician-patient communication (17, 18).
Educational programs are needed to improve physicians’ assessment of medication use and their patient counseling skills (9). Such programs should address the intersection of health literacy and medication use, especially in clinical settings where low health literacy is prevalent (6, 19). Here we describe the development and evaluation of a workshop for physicians to improve skills in medication counseling, with an emphasis on the needs of patients with low health literacy. The objective of the present evaluation is to assess the effect of this focused educational intervention on physicians’ confidence and behaviors with regard to counseling patients about prescription medications.
Methods
Setting and participants
The study was conducted among internal medicine residents at Emory University School of Medicine. The residents’ continuity clinics are located in the Primary Care Center of Grady Memorial Hospital, where inadequate health literacy affects more than one-third of all patients and 80% of those over age 60 (19). In previous research, 47% of clinic patients were unable to understand directions for taking medicine on an empty stomach, and 44% could not understand how to take a medication every six hours (20). A patient education needs assessment indicated that medication adherence was the most important educational issue for patients in the clinics (21).
All residents (postgraduate years (PGY) 1, 2, and 3) assigned to their ambulatory medicine rotation from March to December 2007 were eligible. During this rotation, residents have one half-day per week blocked for educational workshops. The medication counseling workshop was part of this required series. Attendance at educational conferences was expected of all residents who did not have a schedule conflict (e.g., vacation or having just taken overnight call). Participation in the research study was voluntary and did not affect residents’ standing in the program. Participants provided informed consent. The study was reviewed and approved by the Institutional Review Boards of Emory and Vanderbilt Universities.
Intervention
We followed an established six-step method for curriculum development: problem identification and general needs assessment; needs assessment of targeted learners; goals and objectives; educational strategies; implementation; and evaluation and feedback (22). The workshop content was devised from a literature review and other educational materials on clear health communication, medication adherence, and patient counseling (23–28). An overview of workshop content is shown in Table 1. A version of the workshop slides, adapted for clinical pharmacists, is available online (29).
Table 1.
Medication counseling workshop content
| 1 | Background |
| Definition of adherence and persistence | |
| Forms of non-adherence (e.g., not filling a prescription, gaps between refills, discontinuation of medication, ‘drug holiday’) | |
| Prevalence of non-adherence | |
| 2. | Health effects of non-adherence |
| Chronic disease control | |
| Healthcare utilization | |
| Costs | |
| Mortality | |
| 3. | Factors contributing to non-adherence |
| Patient characteristics (e.g., forgetfulness, lack of belief in treatment effect) | |
| Disease characteristics (e.g., asymptomatic conditions, psychiatric co-morbidity) | |
| Regimen characteristics (e.g., cost, complexity, side-effects) | |
| External barriers (e.g., transportation, access to care) | |
| Provider or interpersonal factors (e.g., patient-provider relationship, counseling skills) | |
| 4. | The role of health literacy in medication use |
| Understanding of prescription drug information | |
| Adherence | |
| 5. | Techniques to improve counseling of patients, especially those with low health literacy |
| Ask about adherence at every visit. Ask in an open-ended way that normalizes non-adherence and encourages an honest response. Examples: ‘Many people have trouble getting their refills on time or taking their medications correctly every day. What difficulties have you been having?’ ‘Tell me more about one or two of the main problems that you are having with your medicines.’ ‘A lot of my patients tell me they miss their medications from time to time. In the last week, how many days have you missed a dose of one of your medicines?’ ‘A lot of people say the instructions on medication bottles can be hard to follow, especially when they're taking a lot of medicines. How hard is it for you to follow the instructions on your medication bottles?’ | |
| Quickly address one or two identified problems. Engage the patient in problem-solving and shared goal setting. | |
| Refer patients to a pharmacist for additional counseling when needed | |
| Prescribe in a way that promotes adherence | |
| Simplify regimen (number of medications as well as times of administration) | |
| Tailor regimen to patient's lifestyle | |
| Consider out-of-pocket costs | |
| Provide the drug indication | |
| Confirm patient understanding | |
| When doing a teach-back, normalize the process, put the burden on your shoulders, and be specific. Example: ‘I always ask my patients to repeat things back to me so I can be sure I explained them clearly. If you were trying to tell your husband how you should take this new medicine, what would you say?’, then ‘What two possible side-effects do you need to watch out for?’, then ‘What should you do if you feel dizzy in the morning?’ | |
| Demonstrate new skills (e.g., inhaler technique) | |
| 6. | Other aids or programs to improve adherence (e.g., pill boxes, blister packaging, medication management services) |
The two-hour workshop was taught by the lead author, using didactic but primarily interactive techniques to engage participants fully, meet their individual needs, and maximize behavior change (30, 31). Participants discussed their perceptions of and previous experiences with non-adherent patients, including communication difficulties related to low health literacy. Small group breakout sessions allowed participants to practice the teach-back technique and adherence-building strategies, using scripted scenarios and role play (32). In these breakout sessions, participants worked in groups of three, with one serving as the patient, one as the physician, and the third as an observer who provided feedback.
Data collection
The instruments for this study were developed from existing questionnaires located through a literature review (11, 33, 34). New items of a comparable format were added. Variables assessed in the baseline and follow-up questionnaires included demographics (age, gender, race, year of training); previous training in medication counseling (baseline only); knowledge, beliefs, and attitudes about physician medication counseling; confidence in performing medication counseling; and self-reported medication counseling behaviors. The knowledge, beliefs, and attitudes scale had poor internal consistency reliability at baseline (Cronbach's α=0.002), and its results are not reported here.
The confidence scale comprised seven items with Likert response choices ranging from 1 (‘not confident’) to 4 (‘very confident’). Specifically, participants were asked to rate their confidence in their ability to describe effectively the scope of medication non-adherence, discuss its health effects, describe factors that may contribute to non-adherence, discuss the role of health literacy in medication use, assess patients’ medication adherence, counsel patients about medication use, and counsel low-literacy patients about medication use. The items demonstrated good internal consistency reliability at baseline (Cronbach's α=0.77).
To assess self-reported medication counseling behaviors, participants indicated the frequency with which they performed 24 behaviors on a Likert scale that ranged from 1 (‘never’) to 5 (‘all of the time’). Examples of desirable counseling behaviors included assessing patients’ adherence and their understanding of how to take their medications, asking patients about their barriers to adherence, helping patients develop a plan to overcome their own barriers, asking patients about the cost of their medications, considering cost when prescribing, discussing potential side-effects and their management, demonstrating how to perform skills (e.g., inhaler use), avoiding jargon, and using teach-back. The behavioral items demonstrated good internal consistency reliability at baseline (Cronbach's α=0.80).
The initial questionnaire was administered in person during the workshop. Follow-up questionnaires were administered through an internet-based application approximately one month later. Each questionnaire took about five to eight minutes to complete. Responses to both questionnaires were confidential. Upon completion of the second survey, subjects were asked to e-mail or call an administrative assistant, who was not a member of the research team, to receive a $10 gift card. This allowed us to distinguish who had participated without associating responses with individual participants or being able to link pre-test and post-test responses.
Statistical analysis
The sample size was determined by the number of available residents, rather than by statistical calculations. The primary outcome was self-reported medication counseling behaviors. The secondary outcome was self-reported confidence in the ability to provide medication counseling. Scores on each of these scales were computed by adding individual item scores and dividing by the number of valid responses, so the confidence scale score ranged from 1 to 4 and behavioral scale score ranged from1 to 5. Higher scores indicated greater confidence in medication counseling and more frequent use of recommended medication counseling behaviors, respectively.
We first established pre-test and post-test group equivalence on each demographic characteristic using chi-square tests for categorical variables and t-tests for continuous variables. A single chi-square test examined prior medication counseling training (none/a little bit=1 and a moderate amount/a lot=2) by year in residency (PGY1=1, PGY2=2, PGY3=3).
We used independent samples t-tests to assess change in the scales for confidence and medication counseling behaviors, comparing pre-test and post-test responses. We examined the magnitude of the pre- to post-test group mean difference in confidence and behavior by calculating Cohen's d. This effect size classification that has since become convention exhibits the following values: small effect d=0.20, medium effect d=0.50, and large effect d=0.80 (35).
A series of Mann Whitney U tests was also performed to examine pre/post change on individual items pertaining to confidence and behaviors. One-way ANOVAs examined residency year differences in confidence and behaviors at pre-test and post-test. We used a Bonferroni correction to adjust for multiple comparisons. All analyses were performed in SPSS version 19.0 for Windows. A two-sided p-value <0.05 was considered statistically significant.
Results
Out of approximately 60 residents who attended one of the medication counseling workshops, 54 enrolled in the study and completed the baseline pre-survey. Thirty-five residents (65%) also completed the post-survey. At pre-test, approximately 46% of the participants were female, 57% were white, and most were in their first year of residency (69%; see Table 2). The pre-test and post-test groups did not differ significantly in demographic characteristics (Table 2). According to a single chi-square test, at pre-test PGY1 participants were more likely than PGY2 and PGY3 participants to report they had none/a little bit of prior training in medication counseling, χ2 (2)=2.7, p=0.03.
Table 2.
Characteristics of resident physicians at pre-test (n=54) and post-test (n=35)
| Characteristic | Pre-test | Post-test | p-value |
|---|---|---|---|
| Age in years, mean±SD | 28±2.9 | 27.6±2.3 | .446 |
| 23–25 | 6 (11.2) | 3 (8.8) | .688 |
| 26–28 | 28 (51.9) | 21 (61.8) | .468 |
| 29–31 | 12 (22.3) | 7 (20 | .786 |
| 32–36 | 6 (11.2) | 3 (8.8) | .688 |
| Gender | |||
| Female | 25 (46.3) | 16 (51.4) | .457 |
| Race | |||
| Asian | 13 (24.1) | 8 (22.9) | .953 |
| Black or African American | 6 (11.1) | 1 (2.9) | .168 |
| White | 31 (57.4) | 24 (68.6) | .214 |
| Other | 4 (7.4) | 2 (5.8) | .378 |
| Hispanic ethnicity | |||
| No | 52 (96.3) | 33 (94.3) | .450 |
| Year in residency | |||
| 1st | 37 (68.5) | 22 (62.9) | .711 |
| 2nd | 9 (16.7) | 5 (14.3) | .807 |
| 3rd | 8 (14.8) | 8 (22.9) | .483 |
Note: Unless noted otherwise, values are presented as N (%). Pre/post-test group equivalence was established with chi-square tests for categorical variables and t-tests for continuous variables (age).
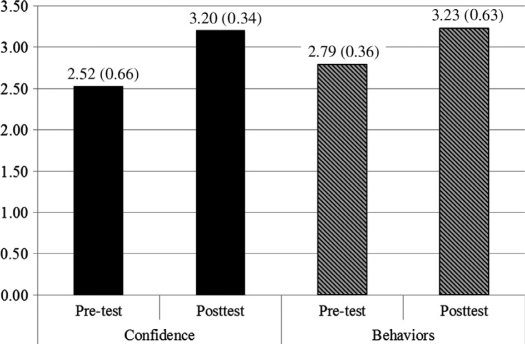
At baseline, participants’ confidence in performing medication adherence counseling was relatively poor, with a mean (SD) of 2.52 (0.66) out of a possible 4.00 on the confidence scale. After training, confidence increased significantly (post-test mean=3.20, SD=0.34), p<0.001 (Fig. 1). The effect size was large (Cohen's d=−1.38). Responses on each item from the confidence scale improved significantly from pre-test to post-test (p<0.001 for each), including participants’ confidence in counseling low-literacy patients.
Fig. 1.
Mean change in medication counseling confidence and behaviors.
Values represent mean (SD).
Residents’ self-reported medication counseling behaviors also improved, though less consistently across items. Overall, the mean (SD) for the behaviors scale rose from 2.79 (0.36) at pre-test to 3.23 (0.63) at post-test, out of a possible 5.00, p<0.001 (Fig. 1). Again, the effect size was large (Cohen's d=−0.90).
Participants reported using a number of desirable behaviors after attending the workshop. They more frequently reported assessing patients’ understanding of how to take their medications, as well as barriers to adherence (p<0.05 for each). After the workshop, participants were more likely to ask patients about medication costs (p<0.01), look up prices (p<0.05), and consider patients’ out-of-pocket costs when prescribing (p<0.01). They were also more likely to tailor the regimen to the patient's lifestyle to enhance adherence (p<0.01). Residents more frequently reported engaging patients about medication use (e.g., eliciting their feelings about following the treatment plan and encouraging the use of reminders, p<0.01 for each). After the training, residents also reported greater use of recall-promoting strategies, such as having patients teach-back key instructions, p<0.05.
Participants’ self-reported behaviors did not change in several other areas, including trying to be non-judgmental when a patient admits non-adherence; asking patients whether they are experiencing side-effects from their medications; discussing potential side-effects; enlisting the support of a patient's friend or family to help with adherence; or use of simple, non-medical language when discussing medications. Participants reported high scores on the latter at pre- and post-test, suggesting a ceiling effect.
One-way ANOVA models revealed no significant differences on the confidence and behavior scales by residency year at pre-test and post-test.
Discussion
Physician-patient counseling about medications has the potential to improve patients’ understanding of and adherence to their medication regimen (9, 26). This study evaluated the effect of an educational training program designed to improve resident physicians’ assessment of medication use and their adherence counseling skills. We found that a medication counseling workshop significantly improved residents’ confidence to perform adherence counseling, awareness of medication costs, and self-reported counseling behaviors at one month.
At baseline, physicians’ confidence to counsel patients about medication use was relatively low. This finding is congruent with the results of an investigation by Russell and colleagues (12), which found relatively low medication assessment and counseling skills (compared to other patient-provider communication skills) among a multidisciplinary group of physicians and clinic staff. Interestingly, Golin and colleagues found that physicians’ perceived skill in medication counseling correlated with their likelihood of providing such counseling (11).
Tarn and others have examined how often physicians counsel patients about various aspects of medication use (11–16). Such discussions occur infrequently overall, though they appear more common for newly prescribed or changed therapies (11, 13). We are encouraged by the results of this study, which showed that a single medication counseling workshop significantly increased the self-reported performance of numerous medication counseling behaviors. Importantly, many of these behaviors addressed aspects of health literacy, such as assessing patients’ understanding of how to take their medications, suggesting reminder strategies (e.g., pill boxes, medication calendars), demonstrating use (e.g., inhaler technique), and employing teach-back to confirm patient comprehension. Increasingly, low health literacy is recognized as a barrier to safe and effective medication use (36, 37). Others have shown that physicians feel ill-equipped to address the health-literacy-related needs of their patients (38). Thus an increase in these specific medication counseling behaviors, along with a significant increase in residents’ confidence to counsel low-literacy patients about medication use, is particularly encouraging and important.
Another noteworthy area of improvement relates to addressing the cost of medications. Concerns about the high cost of prescription medications and the effect of costs on adherence have garnered much attention (39–44). Alexander and colleagues noted that research is needed to assess the effect of communication about costs on patient satisfaction, utilization, and outcomes (40). While it was outside the scope of this study to assess patient outcomes, we did observe an increase in awareness of medication costs, as well as an increase in residents asking patients about costs and considering patients’ out-of-pocket costs when prescribing. Subsequent studies could assess the effect of increased awareness and discussion of costs on patients’ expenses and adherence.
In addition to improvements in counseling related to health literacy and cost, we observed an increase in counseling behaviors pertinent to providing patient-centered care. These included asking patients about barriers to adherence and tailoring the regimen to the patient's daily lifestyle. Residents also more often reported eliciting patients’ feelings about their ability to follow the treatment regimen, an area which in prior research has been rated by patients as lacking (17, 18).
Before the workshop, PGY1 residents were more likely to report that they had received no or little prior training in medication counseling. However, we observed no consistent differences in residents’ confidence and behaviors at pre-test or post-test, suggesting that an educational model such as this could be valuable for residents in all years of training.
This study has several limitations which should be acknowledged. First, it took place at a single institution, which may limit its generalizability. Second, due to the nature of the consent and data collection processes, which were designed to protect the confidentiality of the participating residents, the comparisons presented here are at the group level (pre versus post), rather than paired at the individual level. Third, while the majority of workshop participants completed a follow-up survey, others did not. Non-responders may have had less interest in the subject matter or perceived less of a change in their confidence or behaviors. Fourth, because of the resources available, we relied on residents’ self-assessments, rather than direct observation of their counseling behaviors. The measures utilized are subject to social desirability bias, and their validity and reliability are still being established. Fifth, we did not assess whether the benefits of this intervention persisted beyond one month; this should be the subject of future research.
Conclusion
Through a relatively brief training intervention, it is feasible to improve residents’ confidence in counseling patients about medication adherence, including those with low health literacy. Residents who attended this program also reported a significant increase in their use of desirable counseling behaviors one month after the intervention.
Educational initiatives to improve physicians’ medication counseling skills should be disseminated more widely. Indeed, the program described here was adapted to train pharmacists on how better to counsel patients with low health literacy (29), and it has been incorporated into the training of pharmacists who provided medication counseling in two controlled trials (45, 46). In doing so, we have tailored the program's scope and length according to the audience and available teaching time. Additional studies are needed to assess the effect of such training on patient medication adherence and clinical outcomes.
Disclosures
Supported by award numbers K23HL077597 from the National Heart, Lung, and Blood Institute (Kripalani) and K01DK087894 from the National Institute of Diabetes and Digestive Kidney Diseases (Osborn). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute; National Institute of Diabetes and Digestive Kidney Diseases; or the National Institutes of Health.
Dr Kripalani serves as a consultant to and holds equity in PictureRx, LLC. Dr Kripalani has received investigator-initiated grant funding from Pfizer, Inc. and has served as a consultant to Pfizer, Inc. and Bristol-Myers Squibb/Sanofi. These companies did not provide support, materials, or funding for the present work.
References
- 1.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 2.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2003;26:331–42. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 3.McDermott MM, Schmitt B, Wallner E. Impact of medication nonadherence on coronary disease outcomes: a critical review. Arch Intern Med. 1997;157:1921–9. [PubMed] [Google Scholar]
- 4.Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15. doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 6.Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. 2006;21:852–6. doi: 10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gazmararian J, Kripalani S, Miller MJ, Echt KV, Ren J, Rask KJ. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–21. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalichman S, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14:267–73. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stevenson FA, Cox K, Britten N, Dundar Y. A systematic review of the research on communication between patients and health care professionals about medicines: the consequences for concordance. Health Expect. 2004;7:235–45. doi: 10.1111/j.1369-7625.2004.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson IB, Schoen C, Neuman P, Kitchman Strollo M, Rogers WH, Chang H, et al. Physician-patient communication about prescription medication nonadherence: a 50-state study of America's seniors. J Gen Intern Med. 2007;22:6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golin CE, Smith SR, Reif S. Adherence counseling practices of generalist and specialist physicians caring for people living with HIV/AIDS in North Carolina. J Gen Intern Med. 2004;19:16–27. doi: 10.1111/j.1525-1497.2004.21151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russell ML, Insull W, Jr, Probstfield JL. Examination of medical professions for counseling on medication adherence. Am J Med. 1985;78:277–82. doi: 10.1016/0002-9343(85)90438-3. [DOI] [PubMed] [Google Scholar]
- 13.Scherwitz L, Hennrikus D, Yusim S, Lester J, Vallbona C. Physician communication to patients regarding medications. Patient Educ Couns. 1985;7:121–36. doi: 10.1016/0738-3991(85)90003-5. [DOI] [PubMed] [Google Scholar]
- 14.Morris LA, Tabak ER, Gondek K. Counseling patients about prescribed medication: 12-year trends. Med Care. 1997;35:996–1007. doi: 10.1097/00005650-199710000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. American Journal of Managed Care. 2006;12:657–64. [PubMed] [Google Scholar]
- 16.Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. Physician communication when prescribing new medications. Arch Intern Med. 2006;166:1855–62. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 17.Kripalani S, Jacobson TA, Mugalla CI, Cawthon RC, Niesner KJ, Vaccarino V. Health literacy and the quality of physician-patient communication during hospitalization. J Hosp Med. 2010;5:269–75. doi: 10.1002/jhm.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schillinger D, Bindman AB, Wang F, Stewart AL, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52:315–23. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 19.Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–82. [PubMed] [Google Scholar]
- 20.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss JR. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 21.Bobrow E, Evans M, Franco E, McClain S. Patient education needs of Grady health system's ambulatory care clinics. Rollins School of Public Health of Emory University, Community Needs Assessment. 1997 [Google Scholar]
- 22.Kern D, Thomas P, Howard D, Bass E. Curriculum development for medical education. Baltimore, MD: Johns Hopkins University Press; 1998. [Google Scholar]
- 23.Miller NH, Hill M, Kottke T, Ockene IS. The multilevel compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation. 1997;95:1085–90. doi: 10.1161/01.cir.95.4.1085. for the Expert Panel on Compliance. [DOI] [PubMed] [Google Scholar]
- 24.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 25.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21:888–90. doi: 10.1111/j.1525-1497.2006.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540–50. doi: 10.1001/archinte.167.6.540. [DOI] [PubMed] [Google Scholar]
- 27.Kripalani S, Jacobson KL, Brown S, Manning K, Rask KJ, Jacobson TA. Development and implementation of a health literacy training program for medical residents. Medical Education Online. 2006;11:1–8. doi: 10.3402/meo.v11i.4612. [DOI] [PubMed] [Google Scholar]
- 28.American Society of Health-System Pharmacists. ASHP guidelines on pharmacist-conducted patient education and counseling. Am J Health-Syst Pharm. 1997;54:431–4. doi: 10.1093/ajhp/54.4.431. [DOI] [PubMed] [Google Scholar]
- 29.Kripalani S, Jacobson KL. A training program for pharmacy staff. Rockville, MD: Agency for Healthcare Research and Quality; 2007. Strategies to improve communication between pharmacy staff and patients. Available from www.ahrq.gov/qual/pharmlit/pharmtrain.htm Accessed August 5, 2011. [Google Scholar]
- 30.Davis DA, Thompson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effects of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 31.Knowles M. The adult learner: a neglected species. Houston, TX: Gulf Publishing; 1973. [Google Scholar]
- 32.Schweickert EA, Heeren AB. Scripted role play: a technique for teaching sexual history taking. J Amer Osteopathic Assoc. 1999;99:275–6. doi: 10.7556/jaoa.1999.99.5.275. [DOI] [PubMed] [Google Scholar]
- 33.Jenkins L, Britten N, Stevenson F, Barber N, Bradley C. Developing and using quantitative instruments for measuring doctor-patient communication about drugs. Patient Educ Couns. 2003;50:273–8. doi: 10.1016/s0738-3991(03)00049-1. [DOI] [PubMed] [Google Scholar]
- 34.Reif S, Smith SR, Golin CE. Medication adherence practices of HIV/AIDS case managers: a statewide survey in North Carolina. AIDS Patient Care & Stds. 2003;17:471–81. doi: 10.1089/108729103322395500. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. Statistical power analysis for the behavioral sciences. 2nd edn. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 36.Institute of Medicine. Health literacy. A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 37.Institute of Medicine. Standardizing medication labels: confusing patients less, workshop summary. Washington, DC: National Academies Press; 2008. [Google Scholar]
- 38.Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, et al. Physician notification of their diabetes patients’ limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20:1001–7. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shrank WH, Hoang T, Ettner SL, Glassman PA, Nair K, DeLapp D, et al. The implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med. 2006;166:332–7. doi: 10.1001/archinte.166.3.332. [DOI] [PubMed] [Google Scholar]
- 40.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290:953–8. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 41.Masoudi FA, Baillie CA, Wang Y, Yongfei BW, David S, John FH, Edward P, et al. The complexity and cost of drug regimens of older patients hospitalized with heart failure in the United States, 1998–2001. Arch Intern Med. 2005;165:2069–76. doi: 10.1001/archinte.165.18.2069. [DOI] [PubMed] [Google Scholar]
- 42.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164:1749–55. doi: 10.1001/archinte.164.16.1749. [DOI] [PubMed] [Google Scholar]
- 43.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 44.Reichert S, Simon T, Halm EA. Physicians’ attitudes about prescribing and knowledge of the costs of common medications. Arch Intern Med. 2000;160:2799–803. doi: 10.1001/archinte.160.18.2799. [DOI] [PubMed] [Google Scholar]
- 45.Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy-based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Ann Pharmacother. 2010;44:80–7. doi: 10.1345/aph.1M328. [DOI] [PubMed] [Google Scholar]
- 46.Schnipper JL, Roumie CL, Cawthon C, Businger A, Dalal AK, Mugalla I, et al. The rationale and design of the Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study. Circulation: Cardiovascular Quality & Outcomes. 2010;3:212–9. doi: 10.1161/CIRCOUTCOMES.109.921833. [DOI] [PMC free article] [PubMed] [Google Scholar]