Abstract
Background
Adherence with inhaled controller medications for asthma is known to be highly variable with many patients taking fewer doses than recommended for consistent control of lung inflammation. Adherence also worsens as children become teenagers, although the exact causes are not well established.
Objective
To use focus group methodology to examine beliefs, feelings, and behaviors about inhaled asthma controller medication in adolescents and young adults who had previously participated in a longitudinal study of asthma treatment adherence and outcome in order to develop more effective management strategies.
Methods
Twenty-six subjects participated in 6 focus groups comprised of 3-5 young adults (age range 12-20 years). Verbatim transcripts of these groups were analyzed using the long-table method of content analysis to identify key themes raised by participants.
Results
A variety of beliefs, feelings and behaviors influence the adolescent’s decision about how to use their asthma medication. Some of the adolescents understood the importance of daily medication and were committed to the treatment plan prescribed by their provider. Poorer adherence was the product of misinformation, incorrect assumptions about their asthma, and current life situations.
Conclusions
These results, by highlighting potential mechanisms underlying both better and worse adherence inform the development of strategies to improve adherence behavior in adolescents and young adults with asthma. Knowledge of the specific beliefs, feelings and behaviors that underlie adolescents’ use of inhaled asthma controller medication will help providers maximize treatment adherence in this notoriously difficult patient population.
Keywords: asthma, adherence, adolescence, beliefs, behaviors, controller, decision-making
INTRODUCTION
Children and adults with asthma take an average of 50% or less of their prescribed inhaled anti-inflammatory medications (1-4). Additionally, adherence across individuals is not normally distributed but instead appears flat, with essentially equal percentages of patients taking >75%, 50-75%, 25-50%, and <25% of their prescribed medication (5). Although partial adherence may provide some anti-inflammatory benefit, it is unlikely that individuals taking <25% of prescribed medication are adequately protected (4). Conversely, some patterns, such as taking one set of twice-daily prescribed puffs almost every day, totaling 50% of prescribed dose, likely provides significant anti-inflammatory benefit. Other patterns, such as using 50% or more of prescribed medication by taking one’s prescribed dose on consecutive days for half a month, then no medication for the remainder of the month, are less clearly beneficial. Other observed patterns, including taking infrequent puffs with long gaps between uses, are clearly inconsistent with current practice guidelines (6, 7).
Lower socioeconomic resources, poorer education, minority racial/ethnic status, family dysfunction, and beliefs about asthma are factors associated with poorer medication adherence (8-13). Furthermore, teenagers typically have been found to have poorer adherence than younger children and adults (11, 12). However, mechanisms are not well understood, and interventions to improve adherence have had small and poorly sustained effects (14).
The manner in which adolescents make decisions about their health and health-related behavior shares some common ground with adults, yet adolescent decision-making may also differ from adults in significant ways. By midteens, cognitive ability and performance is similar between adolescents and adults. Still, some patterns can be identified which separate adolescent decision-making from that of adults: 1) Adolescents may react more slowly than adults to health threats; 2) Adolescents are prone to discount future health outcomes; and 3) Adolescents tend to be more impulsive when making choices (15). Consequently, the manner in which teens use information available to them to make health decisions may lead to a different conclusions and behaviors than might be typical in adults. Finally, all people draw from their own experiences and an acquired body of knowledge when making health decisions; consequently, with less life experience, adolescents may be less able to completely weigh the implications of specific health choices (16). Understanding the perceptions, motives, and beliefs of adolescents with asthma, therefore, can be quite useful to helping understand how they make adherence decisions, and can provide insight into how to guide adolescents toward better illness self management.
To further examine the motivations and beliefs associated with the level and pattern of medication use, we designed and conducted focus groups with adolescents and young adults who had previously participated in a longitudinal research study. Focus group methodology is particularly well suited to clarifying the roles of beliefs, attitudes, feelings, and behaviors on dynamic, multifactor phenomenon like medication adherence. Indeed, focus groups have revealed descriptions of the many and varied barriers to adherence, and provide arguments for the importance of strong partnerships among patients, families, and providers, for optimal asthma management (17-23). This report expands on the prior literature in two key ways. First, we focused on identifying factors underlying specific patterns of controller adherence previously identified in our prior research. Second, because focus group participants had participated in a prior study, we purposefully sampled across a broad range of known adherence behavior in designing the focus groups, as well as across age, gender and race/ethnicity, thereby allowing participants to explain patterns of adherence reflecting their own observed behavior.
METHODS
Participants and Recruitment
Focus group members were recruited via mailings and follow-up phone calls targeting participants in a previous longitudinal study of asthma treatment adherence and outcomes (10, 24). In that prior study, children between 7 and 16 years of age with physician diagnosis of persistent asthma who were currently prescribed an inhaled corticosteroid controlled medication were recruited from one of two sources: a public school sample chosen to be reflective of the “average” level of asthma care in metro Denver; and a Health Maintenance sample to reflect a population receiving a comprehensive system-level plan for treating asthma. Both the prior and this current study were reviewed and approved by the local Institutional Review Board.
Ninety-six participants of the original study were mailed letters addressed to the young adult (if participant was currently aged 18 years or older) or to the adolescent and parent (if aged less than 18 years). The letter to the younger participants explained the nature of the current study as follows:
“Based on what we learned from you (your child) and the others in this prior study, we now are conducting a new study with the purpose of learning how and when teenagers use their inhaled controller medication to treat their asthma. If you and your child are willing, we would like your child to participate in a discussion group with other teenagers with asthma. During this discussion group, we will ask the group questions about their views of asthma and how they decide when to take asthma medicine.”
This letter also included an informed consent/assent form, a gift certificate to a local video/music store, and a self-addressed stamped return envelope. All potential participants were informed that a member of the research team would be telephoning them in the next few weeks to discuss the study. They also were given a number to call to opt-out of the study and receive no further phone calls from research staff. During the telephone call, questions about the study and the informed consent document were reviewed with the potential participants (and where applicable with their parent). Those who agreed to participate returned the signed informed consent form and were scheduled to attend of the focus groups.
Of the 96 mailings sent out, 33 were returned due to an incorrect current address, 15 declined participating, and 22 never responded to follow-up attempts. Twenty-six individuals participated in the study; their characteristics are detailed in Table 1. Focus group participants had higher estimated full-scale IQ and maximal parental education than those we were not able to recruit; with no other significant differences (Table 1).
Table 1. Characteristics of Focus Group Recruitment Categories.
| Variable | Participants | Decliners | Unreachable | Sig |
|---|---|---|---|---|
| N | 26 | 37 | 33 | |
| Study Sample, % school sample | 46.2% | 29.7% | 60.6% | p<.05 |
| Gender, % male | 65.4% | 54.1% | 54.6% | N/S |
| Mean age at focus group, y (SD) | 15.3 (1.9) | N/A | N/A | |
| Mean age at first study visit, y (SD) | 10.0 (1.9) | 10.6 (2.5) | 10.3 (2.8) | N/S |
| Race | N/S | |||
| Asian | 0.0% | 2.7% | 3.0% | |
| African American | 7.7% | 8.1% | 18.2% | |
| Hispanic | 7.7% | 8.1% | 27.3% | |
| White | 84.6% | 81.1% | 14.6% | |
| Mean Child Est. Full Scale IQ, (SD)1 | 110.5 (16.8) | 110.3 (16.7) | 97.5 (15.9) | p<.05 |
| Household Socioeconomic Status2 | N/S | |||
| Class I | 19.2% | 13.5% | 6.1% | |
| Class II | 38.5% | 43.2% | 27.3% | |
| Class III | 38.5% | 27.0% | 39.4% | |
| Class IV | 0.0% | 10.8% | 18.2% | |
| Class V | 3.9% | 5.4% | 9.1% | |
| Maximum Parental Education, y (SD) | 15.7 (2.3) | 14.8 (2.1) | 14.2 (2.3) | p<.05 |
| Age of Asthma Onset, y | 3.5 (2.6) | 2.7 (2.0) | 3.0 (2.4) | N/S |
| Asthma Severity3 | N/S | |||
| Minimal | 38.5% | 27.0% | 24.2% | |
| Mild | 23.1% | 37.8% | 42.4% | |
| Moderate | 26.9% | 27.0% | 21.2% | |
| Severe | 11.5% | 8.1% | 12.1% | |
| Mean Child Asthma QoL, (SD) 4 | 5.7 (1.0) | 5.8 (1.0) | 5.6 (1.2) | N/S |
| Mean Impact of Illness Scale, (SD) 5 | 33.4 (9.1) | 32.6 (10.4) | 37.4 (8.4) | N/S |
| Inhaled Controller Adherence 6 | N/S | |||
| >75% of prescribed doses taken | 36.0% | 25.7% | 18.2% | |
| 35-75% of prescribed doses taken | 32.0% | 42.9% | 40.9% | |
| <35% of prescribed doses taken | 32.0% | 31.4% | 40.9% |
Estimated Full Scale Intelligence Quotient calculated by using the block design and vocabulary portions of the Wechsler Intelligence Scale for Children (38)
Hollingshead’s 4-factor index of Household Socioeconomic Status (39)
Functional Severity of Asthma Scale (40)
Pediatric Asthma Quality of Life Questionnaire (41)
Impact on Family Scale (42)
Mean score across ≥12 months of monitoring using Doser CT (10)
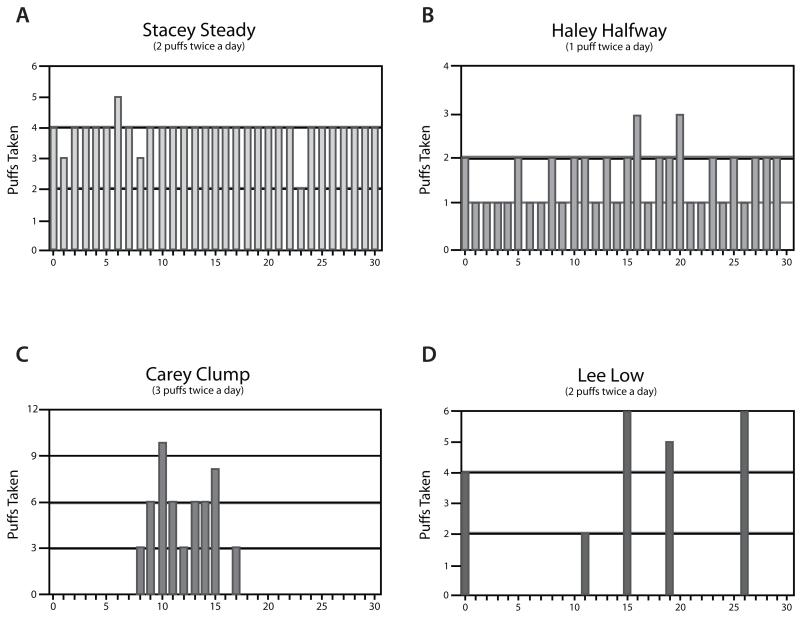
Procedure
Six focus groups were conducted, each lasting approximately 1.5 hours. All groups included both boys and girls, although groups were organized such that older and younger participants were in different groups. Furthermore, since we had prior knowledge of these adolescent’s adherence behavior from the prior study, all groups were purposively designed to include participants across a broad range of prior adherence (range <30% to > 80%) except one that by design had only poor adherers (range 9% to 58%). Adherence with inhaled asthma controller medications was monitored across the prior study using the Doser CT (Meditrack, Hudson, MA) in blinded mode for at least 12 months and summarized as the average across this time as previously described (10). The mean time from the onset of adherence measurement to participation in the focus groups was 4.8 ± 0.4 years (range = 4.1 to 5.6). Since adherence was tracked for a minimum of 12 months, at the time of participation, the adherence data were, at most, about 3.5 years “old.” Groups were lead by two senior faculty with extensive clinical and research experience with adolescents with asthma (FSW & BGB). After a brief set of introductions and “ice-breaking” activity, the group leaders explained the purpose of the groups, “We are very interested in learning how teenagers can best deal with asthma. We don’t understand some of the results from our last study, in which all of you participated, and we hope you can help us get a clearer idea of what people like you really think about using asthma medications.” We also made it clear that there were no “right answers” and that participants may have differing opinions. The participants were then shown 4 composite patterns of controller inhaler adherence derived from our prior results (5), and attributed to: 1) “Stacey Steady” - regular, consistent, daily use; 2) “Haley Halfway” - regular, consistent use of at least one of the days multiple doses; 3) “Carrie Clump” - sporadic but clustered use; and 4) “Lee Low” - sporadic, occasional use (see Figure 1). Each pattern was used to prompt discussion and elicit participant’s ideas about “the thoughts, words, and feelings of a teenager who would use their inhalers” like one of the composite teens. Multiple efforts were made to encourage participants to freely express their views, such as stating “We don’t really know how teens make their decisions how and when to take their inhalers. There are some ideas out there, however all of these explanations are from ‘old folks.’ No one has ever asked teens what they think. That’s what we want to do today. We do expect that by listening to you, we will learn something new.” In the second half of the group, participants were shown a set of explanatory statements regarding teen’s use of inhaled controller medications gathered from the published literature, again soliciting their thoughts and discussion (see Table 2 for a list of these statements). Again to facilitate discussion, participants were given the following instructions, “Now we are going to switch gears and get your ideas in a different way. We are going to look at some of the things that doctors say about how teenagers use their asthma medications, and get your ideas about the ‘old folks’ ideas.”
Figure 1. Monthly Composite Patterns of Inhaled Controller Adherence used as Focus Group Stimuli.
A. “Stacey Steady” - regular, consistent, daily use; B. “Haley Halfway” - regular, consistent use of at least one dose/day; C. “Carrie Clump” - sporadic but clustered use; and D. “Lee Low” - sporadic, occasional use.
Table 2. Statements about Inhaled Controller Adherence used as Focus Group Stimuli.
| My day is so full with other activities that I don’t think about taking my asthma medications. |
| My asthma is the last of my family’s worries and problems. |
| I am embarrassed about taking asthma medications when others can see me. |
| It’s easy to talk to my doctor. |
| My parents don’t agree about how I should take care of my asthma. |
| Since I have asthma, I expect that I’ll have trouble breathing at least once a week. |
| I have control over my asthma. |
| I take asthma inhalers only when I need them. |
| Asthma medications become less powerful after you have taken them for a long time. |
| Someday I will outgrow my asthma. |
| It is easy for me to take my medications because my schedule is about the same every day. |
| There are things I can’t do because I have asthma. |
| My asthma is different from “Real” asthma. |
| Asthma inhalers have serious, long-term side effects. |
| My doctor is only concerned about medications. |
| My doctor thinks that asthma medications are more important than they really are. |
Focus groups were audio- and videotaped and verbatim transcripts produced for each. Transcripts were analyzed for key themes using the “long table” method in which exact statements from the transcripts are sorted into thematic categories and sub-categories independently by a team of four coders, the two focus group leaders, and two graduate students, who worked as recruiters, support staff, and videographers for the focus groups. The coders met weekly to present their coding efforts, discuss discrepancies to consensus, and then recursively resort and discuss their coding efforts until a final parsimonious, stable, and meaningful categorization was reached (25, 26).
This report is focused on those thematic statements that were recorded across groups, discussion prompts (i.e., prototypic adherence charts or explanatory statements), ages, genders, and race. For the primary results, unless otherwise noted below, there were no major dissenting opinions expressed. Trends are also reported with variation by age, gender, or race. Finally, several statements that were heard only once but reflect potentially important content worthy of further study and reflection are noted.
RESULTS
Focus group participants described beliefs, feelings, and behaviors concerning asthma and prescribed medications, as well as perceptions and feelings about how parents and health care providers influence their adherence.
Beliefs and Feelings
Participants reported that adolescents know how to control their asthma; indeed all 4 prototypic adherence patterns were seen to reflect “control”:
(20 y.o. boy): “Well I know my doctor would disagree, but I think I have control over my asthma, as long as I have my albuterol inhaler with me. My doctor’s obviously gonna say that I don’t because I’m not taking my steroid inhaler … but I think I have control over my asthma.”
(17 y.o. girl): “I think all four of those people up there would probably say they have control over their asthma.”
Participants debated whether one could ever “outgrow” asthma. Some clearly stated that not only could they outgrow their asthma, but also that taking their medications regularly would help them do so:
(13 y.o. girl): “It looks like she [Stacey Steady] thinks if she does her medicine correctly, most of the time, she’ll outgrow it because she’ll get better and stronger.”
(13 y.o. girl): “Maybe Stacey feels like that because she feels like if she really takes a lot of medicine now, in the future she won’t [need it anymore], she’ll be like cured.”
Others suggested that being less adherent with medications was a way to “test” whether or not they had outgrown their asthma:
(16 y.o. boy): “Lee Low may think he outgrew it, but did not completely outgrow it, it does lessen as you get older. He may have reached the point where he believes this and does not take his medication.”
Some believed that one never completely outgrows asthma, emphasizing the need to regularly take anti-inflammatory medications:
(15 y.o. girl): I don’t think you outgrow your asthma. I just think, you know, it kind of goes away slowly, but it can always come back.
Another important set of beliefs reflected the degree to which participants saw their asthma as “serious” or “real,” with better adherence being needed for more serious asthma:
(17 y.o. girl): “I said that she [Stacey Steady] may have a more serious case of asthma and may have to remember to take her medicine or else she starts wheezing all over the place and she may want to be a very active person and in order to do that, she has to remember to take her inhaler.”
(17 y.o. girl): “I think Lee Low probably thought, I don’t think I have asthma, not real asthma.”
Some compared their asthma with peers to determine how “serious” their asthma was:
(15 y.o. boy): “Well I think that some people think that since their asthma is less than everybody else’s because like they might have friends that have nebulizers, that since theirs isn’t as bad as their friend’s then they don’t have to take it as often.”
Others stated how their adherence improved after an asthma crisis proved to them that they had severe asthma, a pattern labeled as being “Scared Steady”:
(14 y.o. boy): “She could be seriously sick. She might be like hospitalized, and she knows that is she doesn’t take it, she’s gonna get really sick.”
(20 y.o. boy): “Right, I mean, that’s so (laughs), I mean that summer after I was in the hospital three times, I took it, I took my inhaler just about everyday, everyday!”
Some participants viewed their medication as a tool that provided aid and strength, while others as a sign of weakness. Adolescents linked the first attribution with better adherence:
(13 y.o. girl): “Well I also play soccer every night and I exercise, so if she plays soccer on a competitive team that practices almost everyday, she’s gonna do it because she wants to be able to run. That’s like what it is for me.”
(17 y.o. boy): “One of my brothers was like that. He just didn’t, he decided to take it [only] when he needed it because he’s very athletic and just refused to admit [that he needed] it.”
A number of boys stated that their parents, especially their fathers, promoted the belief that “real men” don’t take medications:
(16 y.o. boy): “My dad used to have asthma so he believes in the whole, you can just sit there and wait and don’t worry about it, where my mom thinks that you should constantly react on it. That happened once and my dad ended up saying, ‘don’t worry about, just drink some hot water.’ And I started to turn blue, and I had to get an IV on the fire station floor and all that.”
(16 y.o. boy): “I know my dad is kind of the same, he’s like ‘oh just tough it out, you‘ll be fine.’ And my mom starts panicking and she’s like, ‘oh my God!’
Many believed one should take medication only when it was needed, i.e., when one is “sick.” For them asymptomatic asthma was not an illness. This belief was related to two differing patterns of medication use depending on how they defined being “sick.” For some being “sick” was entering an episode of illness, in which case medications would be taken regularly for the duration of the episode, possibly as a medication “burst”:
(17 y.o. girl): “At the beginning of the month or something she [Carey Clump], you know, she’s just basically that she’s feeling okay and then she starts getting sick, allergies start to act up. Then she takes it and then the, then she feels like it’s getting better and she stops taking it.”
At times the direct connection between medication gaps and increased lung inflammation was explicitly recognized:
(14 y.o. boy): “No, like he’ll, he’ll feel fine so he doesn’t take it. Then the absence of it in his lungs will make his lungs, like flame up or flare up.”
For others being “sick” was signaled by recent asthma symptoms, e.g., awakening last night, or anticipating symptoms with upcoming exertion, which lead to taking medication until symptoms disappeared, sometimes blurring the distinction between rescue and controller medication:
(14 y.o. boy): “Well on the days she [Haley Halfway] only takes one she might like not feel like she needs it. Like she’ll take it in the morning, maybe she’ll be tight, like her lungs will be tight in the morning or something. And then at night she’ll be fine. She won’t really need it.”
(18 y.o. boy): “Again, I think she’s like kind of like deciding on what you’re, like kind of knowing what you’re gonna be doing that day, so you’re like, oh I think I’ll take it this morning, then I’ll see if I need it later.”
Finally, some overtly denied or minimized the role of asthma and medications in their life: (16 y.o. girl): “It’s like, trying to escape from it. Like, maybe if I don’t have to take the medicine it’ll go away, or like if I take the medicine then I’m like accepting the fact that I have this.”
This dislike of having asthma and using medications at times was heightened, especially in younger adolescents, by “embarrassment” arising from social comparisons with non-asthmatic peers:
(13 y.o. girl): “Well I know that when I have a sleepover or whatever and I’m taking my inhalers, my friends are like, ‘Oh my God, what does it taste like? Does that hurt? Do you like having asthma? Do you like having inhalers?’ It’s so annoying. It’s so normal for me. I don’t, I’d rather just do it when I’m alone so that no one’s like staring at me with amazement that I’m taking an inhaler.”
(13 y.o. girl): “I think for me, like when I first told my friends in middle school that I had asthma, they thought it was a disease that they could catch from me. And that was something I went through trying to get them to believe that they’re not going to get asthma from me. It’s not something that I can pass on to people.”
Conversely, some expressed a clear acceptance that taking their medications as prescribed was easy to do and beneficial:
(13 y.o. girl): “Well I think it’s kind of like, you know, how are you gonna do those activities if you don’t take your medicines? I mean, put two puffs in your mouth and run. It’s not a big deal. It’s not like you sit down for hours, breathing into oxygen or something.”
Positive traits were related to such acceptance, most consistently “being responsible”:
(15 y.o. girl): “She’s [Stacey Steady] a good student.” (13 y.o. girl): “Good grades.” (15 y.o. girl): “Gets all her homework in on time.” (15 y.o. boy): “Good attendance at school.” (15 y.o. girl): “Maybe a leader in student [government], in power. She does what she’s supposed to do. She’s real responsible.”
Older age was associated with acceptance and being responsible:
(16 y.o. boy): “When you are really, really little your parents have more influence, then you are on your own and you have not gotten your responsibility. You get back to Stacey Steady when you are more mature.”
Behaviors
Participants reported that regular routines facilitated medication taking:
(16 y.o. boy): “I said that she [Stacey Steady] may have a scheduled routine. Like after she goes to school she directly does her homework, then eats, and sleeps even, and that might be part of her routine.”
(15 y.o. girl): “Well the first thing I do every morning, drag my butt into the bathroom, and it’s always there on the counter.”
Many emphasized, however, that the lives of adolescents, particularly older ones, are busy, hectic and even sometimes chaotic, making routines difficult:
(13 y.o. girl): “I think it gets harder as you get older because you cram more into your day. As you get older, you got out to clubs or something with friends and you get home at different times in the night and you’re like, ‘I’m going to bed’.”
Regular routines can be disrupted by the cycles of the school year, vacations, and athletic seasons, or by family crises:
(15 y.o. boy): “In the past, with sports and things, if I forget one day, I’ll forget the whole week.”
(15 b y.o. boy): “Someone could have died in the family, they have to have a funeral, or everything.”
Other stated difficulty maintaining a routine due to being disorganized or forgetful:
(15 y.o boy): “I was thinking maybe like she [Lee Low] just forgot about it, that they forgot about it and they’re just walking around their house one day, and [seeing an inhaler] they’re like, ‘Oh crap, I’m supposed to be taking this.’ So they start taking it and then they forget about it again.”
Certain strategies might help with forgetfulness or lack of a routines, such as having multiple inhalers scattered in different locations to facilitate being cued to take medication, or taking “extra puffs” when one does remember:
(17 y.o. girl): “Me, I lose stuff a lot. So, and if I give I to like my Mom, she’ll lose it. So, I’ll just like maybe have one in drawer, which I still have, and then I have one in my Mom’s car, in the glove compartment of my Mom’s car.”
Although only raised by one participant, one worrisome strategy to minimize need for medication, particular given the concerns of links between asthma and obesity, was to reduce one’s level of exercise:
(17 y.o. girl): “When I was little I had to go to the doctor a lot to take, get breathing treatments, and I found as I got older I didn’t need them as much because I wasn’t running around as much as I used to when I was little.” … “Like for me, I don’t take my asthma [medications] as much as I should, but I, let’s just say I haven’t taken it this week you know, so I feel that I have control over my asthma [by] not doing things that are too [strenuous], that will make me start wheezing or start breathing too hard.”
Roles of parents and providers
Parents and health care providers both were seen as having important roles in promoting or discouraging medication adherence. In general, participants said health care providers have a much more limited role than parents for a variety of reasons, including limited availability, or because their providers were not very facile at communicating with adolescents:
(14 y.o. boy): “Well you can never like get a hold of him. Can’t like call him up and ask him a question.”
(15 y.o. boy): “I’ve seen that happen before where the doctor just comes in and doesn’t really ask you what the problem is. He just starts prescribing medicine and then you’re like, ‘How do I even know if this is really going to help me?’”
Adolescents reported contributing to communication difficulties by withholding information as a way to avoid confrontation or the amount of time spent at the office visit:
(18 y.o. boy): “I think like Carey, like, she has a real hard time talking to her doctor, so like, maybe before she goes to her doctor’s appointment, like just before she goes to her doctor’s appointment about her asthma she starts taking it [controller medication]. That way she can, she feels a little bit better about saying, ‘Yeah I take it, I take it normally.’”
(18 y.o. boy): Regarding Carey Clump: “So that you don’t have to spend as much time in his office because if you aren’t taking your medicine, he’s gonna sit there and just reel off about how you’re not taking your medicine, da-da-da. But if you start taking it and everything, that way you can’t just be in and out, no problems. You don’t have to be around him.”
Adolescents reporting good relationships with their health care providers often had been long term patients or found their provider particularly helpful:
(17 y.o. boy): “I find it pretty easy, I have known my doctor probably for about 11 years so I can’t get away with anything with him anyway.”
Some reported resolving differences in goals over time in the context of a good relationship:
(14 y.o. boy): “I was sick and allergic to dogs and then I got better and I asked my doctor if I could have a dog, and he said no. Finally it took him three years to not be too protective and let me have a dog and sometimes we know that we can have a dog, because I have been in places where I have had dogs, so we know that we can get away with stuff, because we know ourselves better. … If you look at it from a doctor’s perspective he doesn’t really care because if I have a dog or not, it really doesn’t make him any more happy, but it would make me more happy. So like he doesn’t really, he just doesn’t want me to get sick. He just wants to keep his patients healthy. That is his main concern … He is thinking of keeping everything controlled.”
Similarly, some stressed the importance of having their doctors repeat key educational messages over time:
(14 y.o. boy): “Well I think that Lee and Carey might be younger and need more reminding. Like they don’t really know why they’re taking this inhaler and stuff. Kind of like they don’t really care because they don’t really know how to, they don’t really know why they’re doing it.”
Parents, in part because of greater daily contact, were seen as having much greater influence. One key role was day-to-day monitoring of asthma symptoms and medication use:
(16 y.o. girl): “My mom doesn’t really care if I take it day-to-day but when I start getting sick then she kinda pressures me about it.” … “Yeah, she’s worried then and she’s kinda, ‘You need to start taking your medicine now.’”
More parental monitoring was viewed as needed for younger children:
(15 y.o. girl): “She [Stacey Steady] seems to take it pretty regularly like she’s supposed to. She might also be younger because then usually parents work more with a child, so she could be younger. … It also seems like when you’re younger you don’t have to care, it’s like your parents, or older people, kind of do more of it than yourself.”
However, parental monitoring can become a source of parent-child tension or conflict, due to such factors as more limited parental influence or because the parent is construed as being “too anxious” about the adolescent’s asthma:
(20 y.o. boy): “Well I was recently out of town, and I didn’t bring my [BrandName], well because I don’t take it that often, but so and then when my mom realized, ‘Oh my gosh, you aren’t on your [BrandName]!’ And like kind of freaked out because she doesn’t know I don’t take it very often, and if she did know, she’d really be pissed.”
Despite some discomfort in being monitored by one’s parents, participants associated very poor adherence with “bad” parents who “don’t care:”
(15 y.o. girl): “He [Lee Low] could have bad parents that don’t really care, that don’t help him out with it, encourage him.”
Participants also discussed how parental monitoring could be disrupted during larger family difficulties, such as parental disagreement or divorce:
(14 y.o. boy): “Maybe Haley. Because like she might be, her parents might be divorced or something and she might be like with one or the other and one might say, ‘Just use one,’ and the other might say, ‘Just use two.’”
A final, important factor was the distressing reminder that many families cannot afford to controller medications:
(16 y.o. boy): “And also like if she [Haley Halfway] didn’t have medical insurance and her family was running low on money, it might have been trying to conserve and if she didn’t need it twice a day, just take it once a day and make it last.”
(20 y.o. boy): “She [my sister] didn’t have any health insurance, so she had to like, … Steroid inhalers are like really expensive, and she basically decided she wasn’t gonna bother because she couldn’t afford it.”
DISCUSSION
Focus group participants portrayed adherence as a complex, multi-dimensional phenomenon influenced by beliefs, feelings, and habits and the interpersonal context in which they occur. Despite the common perception that adolescents are reluctant to assume responsibility for chronic illness, most participants were strikingly insightful about factors underlying adherence. Some understood the importance of daily medication, appeared committed to the treatment plan prescribed by their provider, and saw positive adherence as aligned with other responsible behaviors. Although adolescent decision-making may be impeded by lack of experience with or concern about health outcomes, by mid adolescence most are cognitively capable of performing adult level cognitive tasks. More informed adolescents are capable of more logical decision-making (15). Adolescent adherence in this study was strengthened by acceptance of one’s asthma as a serious condition; understanding asthma and it’s treatment; adoption of daily routines consistent with regular medication use; oversight and support from parents and physician; and an expressed desire to achieve optimal health. Poorer adherence was a product of misinformation, incorrect assumptions about asthma, and more chaotic current life situations. Some were confused about the differences between controller and rescue medications. Adolescents who dislike taking daily medication and/or see it as a sign of weakness often interpreted the episodic nature of asthma as evidence that they had outgrown their asthma. A belief to take the least amount of medication necessary was frequently reported and similar to views of adults with asthma (8, 17). Busy schedules and family crises interfered with adherence and increased the probability of controller use only when symptoms become intrusive.
A number of clinical implications arise from these results. First, these results underscore the utility of employing the questions Kleinman proposed to elicit a patient’s “explanatory model” regarding their illness (27), including whether the patient agrees with the provider on diagnosis, need for any treatment, and need for the recommended treatment. Adolescents indicated that adherence would be poorer if they believed that their asthma was not “real” or “serious.” Similarly, many reported that decreased regular or even intermittent use of controller medication could adequately control their asthma. Also, some found asthma controllers helpful, but nonetheless, chose not to take them so as to not admit personal “weakness.” Perhaps most important, adolescents viewed all patterns of controller use consistent with “control” of their asthma. Hence, “asthma control” did not mean the same thing to all participants, and in many cases was at odds with current guidelines (e.g., gaining control during an episodes or in response to current symptoms, rather than a lack of episodes and/or symptoms). Since most office visits are conducted with the implicit assumption that patient and provider have the same “explanatory model” (e.g., agreement regarding working diagnosis and treatment), it is important for clinicians to know how and when to probe for such discrepancies.
Adolescents generally believe in the phenomenon of “outgrowing asthma” and often confuse quiescent periods during adolescence, as well as temporary lack of symptom worsening after reducing or stopping controller medications, as indicating that they have outgrown their asthma. Although about half of all children experience significant improvement in their asthma after puberty, bronchial hyper-reactivity appears to persist, symptoms re-emerge for many latter in life, and there is increased risk of morbidity and mortality in patients who erroneously misclassified themselves as having “outgrown” their asthma (28-30). Clinicians must probe for this belief and construct an adequate plan for shared-decision making concerning whether or not a specific patient has indeed outgrown their asthma.
Having regular behavior rhythm and routines was a major factor promoting adherence. Yet, much of teenage life conspires against adopting regular routines. Fiese and colleagues have discussed the importance of inquiring into family routines for asthma management (31-33). Furthermore, Cramer and colleagues (34, 35) have demonstrated the effectiveness of “cue-dose-training” to improve adherence by determining if a patient has any existing daily behavioral routines in their life to which medication taking can be paired, and if not, working with the patient to develop such a routine. Additionally, the potential value of providing patients with extra inhalers (e.g., helping “forgetful” patients find one; usefulness of having inhalers in multiple locations or homes) deserves further study. Finally, although only raised once in this study, given the frequent co-occurrence of obesity and asthma (36), clinicians and researchers alike should inquire whether some patients increase sedentary behavior as a way of controlling their asthma symptoms rather than taking controller medication.
Regarding interpersonal factors, two findings seem especially important. First, better adherence was linked to having a good, long-term relationship with a provider. Such a relationship facilitates better adherence via improved communication, repetition of key messages, and detection and negotiation of differences in opinion. Unfortunately, many factors in contemporary health care make such relationships difficult, if not actively conspire against them. Yet, many participants expressed the desire for such a partnership with a provider who was genuinely interested and available to them.
Second, the ongoing role of parents in promoting good adherence was emphasized, to a somewhat surprising degree. This is not to say that parents have an easy time given the problems attributed to parents who don’t care enough, as well as parents who care too much. Nonetheless, participants wanted support from their families as they learned how to successfully manage their asthma. Once again, the wise clinician will ask patients whether they are receiving the help and support needed from others to take adequate care of their asthma.
Several strengths and limitations of this study deserve mention. A notable strength was the planned diversity in participant adherence behavior in all focus groups (except for one which by design had only poorer adherers) since their inhaler use had been electronically measured for ≥ 12 months. Limitations are also recognized. Focus groups are cross-sectional and cannot indicate whether the attitudes we found are stable, fluctuate, or evolve as people mature; indeed, given the extensive cognitive changes that occur across adolescence (37), caution needs to be exercised with these findings. Similarly, since the prompts that the participants responded to were prototypic adherence charts and statements from the literature, we cannot be sure that every response indeed reflected the participant’s actual adherence behavior. On the other hand, essentially half (23/47) of the statements included above do appear to be personal. Also, since the adherence data concerning participants was on average collected 3-4 years previously, it is possible that the asthma severity and/or adherence of participants could have been significantly different at the time of the focus groups. Yet, since we solicited their opinions, even if their clinical situation was different in some way, the statements obtained still should represent memories with some validity. Moreover, the vast majority of the findings reported here were consistently observed across all focus groups as well as adolescents of various ages, further supporting their validity. Also, in designing and coding these focus groups, we sought areas of agreement. Another fruitful approach, not pursued in this study, would be to structure the questioning route specifically to look for differences in opinions and disagreements. Finally, participants in these focus groups might differ from non-respondents in important ways. For example, we know that participants had higher IQ and parents with greater educational attainment than those whom we were not able to recruit.
By highlighting potential mechanisms influencing better and worse adherence, these findings provide insight into both challenges and opportunities to improving adherence behavior in adolescents with asthma. Further efforts on the clinical, research, and system level are needed to develop effective interventions for this important clinical problem.
Acknowledgments
The writing of this paper was supported by NIH grants R01-HL53391, R01-HL70267, M01-RR00051 and UL1-RR025780. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Footnotes
DECLARATION OF INTEREST:
REFERENCES
- 1.Bender B, Wamboldt FS, O’Connor SL, Rand C, Szefler S, Milgrom H, et al. Measurement of children’s asthma medication adherence by self report, mother report, canister weight, and Doser CT. Ann Allergy Asthma Immunol. 2000;85(5):416–21. doi: 10.1016/s1081-1206(10)62557-4. [DOI] [PubMed] [Google Scholar]
- 2.Bender BG, Rankin A, Tran ZV, Wamboldt FS. Brief-interval telephone surveys of medication adherence and asthma symptoms in the Childhood Asthma Management Program Continuation Study. Ann Allergy Asthma Immunol. 2008 Oct;101(4):382–6. doi: 10.1016/S1081-1206(10)60314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003 Jul-Aug;28(5):323–33. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 4.Rohan J, Drotar D, McNally K, Schluchter M, Riekert K, Vavrek P, et al. Adherence to pediatric asthma treatment in economically disadvantaged African-American children and adolescents: an application of growth curve analysis. J Pediatr Psychol. 2010 May;35(4):394–404. doi: 10.1093/jpepsy/jsp074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wamboldt FS, Rojas S, Bender B, Boyum L, Ho J, Milgrom H, et al. Patterns of MDI Adherence in Children with Asthma. Am J Respir Crit Care Med. 2001;163(5):A317. [Google Scholar]
- 6.National Heart L, and Blood Institute, editor. National Asthma Education and Prevention Program. U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program; Bethesda, Md.: 2003. Expert panel report : guidelines for the diagnosis and management of asthma : update on selected topics, 2002. [Google Scholar]
- 7.National Heart Lung and Blood Institute . Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health; Bethesda, MD: 1997. [Google Scholar]
- 8.Apter AJ, Boston RC, George M, Norfleet AL, Tenhave T, Coyne JC, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it’s not just black and white. J Allergy Clin Immunol. 2003 Jun;111(6):1219–26. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- 9.Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1810–7. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- 10.Ho J, Bender BG, Gavin LA, O’Connor SL, Wamboldt MZ, Wamboldt FS. Relations among asthma knowledge, treatment adherence, and outcome. J Allergy Clin Immunol. 2003 Mar;111(3):498–502. doi: 10.1067/mai.2003.160. [DOI] [PubMed] [Google Scholar]
- 11.Wamboldt F, Bender B, Wamboldt M, Bihun J, Milgrom H, Szefler S. Psychosocial correlates of pediatric MDI adherence. Am J Respir Crit Care Med. 2000;161(3):A711. [Google Scholar]
- 12.Wamboldt FS, Bender B, Ho J, Milgrom H, Rojas S, Szefler S, et al. Correlates of MDI adherence: A replication study. Am J Respir Crit Care Med. 2002;165(8):A197. [Google Scholar]
- 13.Le TT, Bilderback A, Bender B, Wamboldt FS, Turner CF, Rand CS, et al. Do asthma medication beliefs mediate the relationship between minority status and adherence to therapy? J Asthma. 2008 Jan-Feb;45(1):33–7. doi: 10.1080/02770900701815552. [DOI] [PubMed] [Google Scholar]
- 14.Bender B, Milgrom H, Apter A. Adherence intervention research: what have we learned and what do we do next? J Allergy Clin Immunol. 2003 Sep;112(3):489–94. doi: 10.1016/s0091-6749(03)01718-4. [DOI] [PubMed] [Google Scholar]
- 15.Downs JS, Fischhoff B. Theories and models of adolescent decision making. In: Diclemente RJ, Santellia JS, Crosby RA, editors. Adolescent Health: Understanding and Preventing Risk Behaviors. Jossey-Bass; New York: 2009. [Google Scholar]
- 16.Reyna VF, Farley F. Risk and rationality in adolescent decision making: implications for theory, practice, and public policy. Malden, MA; Blackwell Publishers; 2006. [DOI] [PubMed] [Google Scholar]
- 17.George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ. Qualitative research-enhanced understanding of patients’ beliefs: results of focus groups with low-income, urban, African American adults with asthma. J Allergy Clin Immunol. 2003 May;111(5):967–73. doi: 10.1067/mai.2003.1459. [DOI] [PubMed] [Google Scholar]
- 18.Jones A, Pill R, Adams S. Qualitative study of views of health professionals and patients on guided self management plans for asthma. Bmj. 2000;321(7275):1507–10. doi: 10.1136/bmj.321.7275.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kieckhefer GM, Ratcliffe M. What parents of children with asthma tell us. J Pediatr Health Care. 2000;14(3):122–6. [PubMed] [Google Scholar]
- 20.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspectives. Pediatrics. 2000;106(3):512–9. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 21.Meng A, McConnell S. Decision-making in children with asthma and their parents. J Am Acad Nurse Pract. 2002 Aug;14(8):363–71. doi: 10.1111/j.1745-7599.2002.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 22.Slack MK, Brooks AJ. Medication management issues for adolescents with asthma. Am J Health Syst Pharm. 1995;52(13):1417–21. doi: 10.1093/ajhp/52.13.1417. [DOI] [PubMed] [Google Scholar]
- 23.van Es SM, le Coq EM, Brouwer AI, Mesters I, Nagelkerke AF, Colland VT. Adherence-related behavior in adolescents with asthma: results from focus group interviews. J Asthma. 1998;35(8):637–46. doi: 10.3109/02770909809048966. [DOI] [PubMed] [Google Scholar]
- 24.Wamboldt FS, Ho J, Milgrom H, Wamboldt MZ, Sanders B, Szefler SJ, et al. Prevalence and correlates of household exposures to tobacco smoke and pets in children with asthma. J Pediatr. 2002;141(1):109–15. doi: 10.1067/mpd.2002.125490. [DOI] [PubMed] [Google Scholar]
- 25.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. 3rd ed. Sage Publications; Thousand Oaks, CA: 2000. [Google Scholar]
- 26.Knodel J. The Design and Analysis of Focus Groups Studies. In: Morgan DL, editor. Successful Focus Groups: Advancing the State of the Art. Sage Publications; Thousand Oaks, CA: 1993. pp. 35–50. [Google Scholar]
- 27.Kleinman A. The illness narratives. Basic Books; New York: 1988. [Google Scholar]
- 28.Mochizuki H, Muramatsu R, Hagiwara S, Takami S, Mizuno T, Arakawa H. Relationship between bronchial hyperreactivity and asthma remission during adolescence. Ann Allergy Asthma Immunol. 2009 Sep;103(3):201–5. doi: 10.1016/S1081-1206(10)60182-2. [DOI] [PubMed] [Google Scholar]
- 29.Butland BK, Strachan DP. Asthma onset and relapse in adult life: the British 1958 birth cohort study. Ann Allergy Asthma Immunol. 2007 Apr;98(4):337–43. doi: 10.1016/S1081-1206(10)60879-4. [DOI] [PubMed] [Google Scholar]
- 30.Gerritsen J. Follow-up studies of asthma from childhood to adulthood. Paediatr Respir Rev. 2002 Sep;3(3):184–92. doi: 10.1016/s1526-0542(02)00193-8. [DOI] [PubMed] [Google Scholar]
- 31.Fiese BH, Wamboldt FS. Family routines, rituals, and asthma management: A proposal for family-based strategies to increase treatment adherence. Families, Systems & Health. 2000;18(4):405–18. Win. [Google Scholar]
- 32.Fiese BH, Wamboldt FS, Anbar RD. Family asthma management routines: connections to medical adherence and quality of life. J Pediatr. 2005 Feb;146(2):171–6. doi: 10.1016/j.jpeds.2004.08.083. [DOI] [PubMed] [Google Scholar]
- 33.Fiese BH, Winter MA, Wamboldt FS, Anbar RD, Wamboldt MZ. Do family mealtime interactions mediate the association between asthma symptoms and separation anxiety? J Child Psychol Psychiatry. 2010 Feb;51(2):144–51. doi: 10.1111/j.1469-7610.2009.02138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cramer JA. Optimizing long-term patient compliance. Neurology. 1995 Feb;45(2 Suppl 1):S25–8. [PubMed] [Google Scholar]
- 35.Rigsby MO, Rosen MI, Beauvais JE, Cramer JA, Rainey PM, O’Malley SS, et al. Cue-dose training with monetary reinforcement: pilot study of an antiretroviral adherence intervention. J Gen Intern Med. 2000 Dec;15(12):841–7. doi: 10.1046/j.1525-1497.2000.00127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abramson NW, Wamboldt FS, Mansell AL, Carter R, Federico MJ, Wamboldt MZ. Frequency and correlates of overweight status in adolescent asthma. J Asthma. 2008 Mar;45(2):135–9. doi: 10.1080/02770900701840246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oakley L. Cognitive Development. Routledge Press; Sussex, England: 2004. [Google Scholar]
- 38.Wechsler D. Wechsler Intelligence Scale for Children - III Edition. Harcourt Brace Jovanovich, Inc.; New York: 1991. [Google Scholar]
- 39.Hollingshead AB. Four factor index of social status. Yale University; 1975. Unpublished Manuscript: Department of Sociology. [Google Scholar]
- 40.Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. Am J Respir Crit Care Med. 1994;149:1434–41. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- 41.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Quality of Life Research. 1996;5:35–46. doi: 10.1007/BF00435967. [DOI] [PubMed] [Google Scholar]
- 42.Stein R, Riessman C. The development of an Impact on the Family Scale. Medical Care. 1980;18:465–72. doi: 10.1097/00005650-198004000-00010. [DOI] [PubMed] [Google Scholar]