Abstract
Background
Osteonecrosis (ON) is a major complication after treatment of developmental dysplasia of the hip (DDH). Several studies have explored the absence of the femoral head ossific nucleus at the time of hip reduction as a risk factor for the development of ON, but findings have been inconsistent.
Questions/purposes
We therefore determined the incidence of ON in children who underwent reduction of a dislocated hip in the presence or absence of the ossific nucleus.
Patients and Methods
We retrospectively reviewed the radiographs of 105 hips in 89 patients treated for DDH at the age of 18 months or younger. Radiographs were graded for the presence of the ossific nucleus at the time of hip reduction and for the presence of ON, as graded by the Bucholz and Ogden classification, for patients at a mean age of 10 years. We used log-binomial regression to estimate if the presence of the ossific nucleus was associated with a lower incidence of ON.
Results
We identified ON in 37 of the 105 hips (35%). The incidence of ON at 10 years was 40% in the absence of the ossific nucleus and 32% in the presence of the ossific nucleus (adjusted relative risk, 0.86; 95% confidence interval, 0.36–1.81). When only radiographic changes of Grade II and greater were considered ON, the risk was still not increased (relative risk, 1.26; 95% confidence interval, 0.62–2.56).
Conclusion
Patients with an ossific nucleus at the time of hip reduction showed a slight tendency toward better outcomes. The ossific nucleus did not protect for ON.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
ON of the capital femoral epiphysis is a major complication of the treatment of DDH, with the potential risk for long-term disability and premature osteoarthritis. Among several risk factors for the development of ON, the presence of the femoral head ossific nucleus on preoperative radiographs [13] or ultrasound [4] has been suggested to decrease the risk for development of ON.
Treatment strategies aimed at delaying the reduction of a dislocated hip in the absence of the ossific nucleus have been proposed [4] in the belief this would minimize the risk of ON in the postoperative course. However, delaying the treatment of a dislocated hip until the ossific nucleus can be seen may increase the risk for residual acetabular dysplasia because it bypasses the period of maximal acetabular remodeling [9]. Such treatment strategies therefore have the potential to increase the need for future operations to treat residual acetabular dysplasia [9].
Although some authors report an increased risk for the development of ON if the reduction was done in the absence of the ossific nucleus [1, 3, 4], others did not observe such a relationship [7, 10]. A meta-analysis of all relevant studies suggested the absence of the ossific nucleus could increase the risk for the development of severe forms of ON [11]. However, the authors had some concerns regarding the included studies such as insufficient length of followup, small sample size, unblinded assessment of exposure and outcomes, and inappropriate statistical analyses. Therefore, the authors concluded the low quality of the individual studies compromised the confidence in this observation, and that there was a need for a comparative study addressing several of the shortcomings inherent to previous studies [11].
We therefore (1) determined the incidence of ON of Grades I to IV according to Bucholz and Ogden [2] in children who underwent reduction of a dislocated hip in the presence or absence of the femoral head ossific nucleus, (2) determined the effect of the ossific nucleus on the development of ON of Grade II or greater; (3) determined the overall incidence of ON in this cohort of patients, and (4) explored several other potential risk factors for ON.
Patients and Methods
In this retrospective cohort study, we included 89 patients (105 hips) with DDH treated by either closed or open reduction. A multicenter design was chosen to include several surgeons and enhance the generalizability and adequately power the study. Hospital admission databases, operating logs, and the individual databases of surgeons were used to identify all patients aged 1 to 18 months at the time of hip reduction. Two hundred eight-five patients were identified during a 10-year period. We excluded patients who had a simultaneous osteotomy because a simultaneous osteotomy was considered a potential effect modifier in the association of interest syndromes. We also excluded patients with skeletal dysplasias and hip dysplasias that were associated with neurologic or metabolic disorders. Six patients with DDH (eight hips of which seven showed ON) were excluded because the ossific nucleus status could not be ascertained owing to missing preoperative imaging. We performed sensitivity analysis on these six patients.
We decided a priori to statistically control for age at reduction. There were 74 girls (83%). The right hip was affected in 38 (36%). Sixteen patients had bilateral hip involvement. The mean age of patients at the index procedure was 8.96 ± 4.0 months (range, 1.6–17.8 months). Patients treated in one study center were younger (p = 0.003) than those of the other center, with a mean difference of 2.3 months. Patients with 79 hips (75%) were younger than 12 months when the index procedure was performed. The mean age of patients at the latest radiographic followup was 9.9 ± 3.7 years (range, 3.2–18 years). The mean followup was 9.1 ± 3.6 years (range, 3–17.6 years). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. The study was granted approval from the Institutional Review Boards at both centers.
Sample size calculation was based on a synthesis of relevant studies [3, 10, 13], and suggested the mean proportion of patients who had ON develop would be 38% if the ossific nucleus were absent and 8% if present. Choosing a more conservative approach, our study was powered (β = 0.20, α = 0.05) to detect a difference of at least 25% in the incidence of ON between groups.
For 85 of the 105 hips (81%), preoperative radiographs allowed us to evaluate the severity of dislocation according to Tönnis [15], indicating dislocation of Grade I in 12 hips, Grade II in 12 hips, Grade III in 15 hips, and Grade IV in 23 hips. The remaining radiographs were taken with the patients’ hips in abduction, which is an inadequate position to ascertain this variable.
The ossific nucleus was present in 63 of 105 hips (60%). Hips without an ossific nucleus were reduced at an earlier time (p = 0.01) than those with an ossific nucleus: mean age of 7.7 ± 6.6 months versus 9.8 ± 3.9 months, respectively (mean difference, 2.1 months).
Three surgeons (JHW, DHAJ, JF) were involved in the treatment of all patients. All infants were examined while under general anesthesia. An attempt was made to perform a closed reduction [5] after performing a percutaneous tenotomy of the adductor longus in infants younger than 15 months. As per individual preference, two surgeons routinely used arthrography to determine the position of the hip before reduction, whereas one surgeon used intraoperative ultrasound or image intensification for this purpose. If a satisfactory reduction could not be achieved, the surgeons proceeded to perform an open reduction. A medial approach technique [16] was chosen for infants younger than 12 months, whereas an anterior approach to the hip with capsulorraphy was used in older infants. The presence or absence of the ossific nucleus did not influence the surgeons’ decision-making regarding the timing or nature of the operation. The following interventions had been performed before referral to one of the two centers: abduction harness treatment in 50 hips with an average duration of 3.38 ± 4.80 weeks; examination while the patient was under general anesthesia including an arthrogram in 10 hips; and closed reduction including adductor tenotomy and a spica cast for 12 weeks for one patient. The same surgical techniques were used for all patients and were described previously [14]. Sixty-five dislocated hips were reduced by closed means, including a percutaneous tenotomy of the adductor longus, and 40 hips were reduced by open means. Skin traction was used in 57 hips (54%) before reduction of the dislocated hip (mean, 10.85 ± 6.63 days) with the rationale that it would ease the reduction and protect for ON. During the period of study, surgeons discontinued the use of skin traction and 48 hips (46%) were treated without traction. Traction was used in older patients (mean age at reduction, 9.6 ± 3.7 years) and 70% were dislocations of Tönnis Grade III or IV [15]. Twenty-seven open reductions were performed with a medial approach and 12 were performed with an anterior approach. Patients who underwent a closed reduction on average were 8.9 ± 3.6 months old and those who underwent an open reduction were 8.9 ± 4.7 months old (p = 0.97). Arthrograms were obtained of 46 hips before the closed or open reduction.
The patients’ hips were immobilized for 12 weeks in a spica cast in the human position [12] with slight internal rotation such that they were not externally rotated if a closed or open reduction by medial approach was performed. Hips were immobilized in 20° flexion, 30° to 40° abduction, and 10° to 20° internal rotation for 6 weeks if open reduction was performed via an anterior approach. Casts were changed after 6 weeks as per routine protocol. Splints were not used after removal of the cast.
All patients had radiographic followup at the time of removal of the cast, 6 weeks, 3 months, and 6 months later, followed by annual followup or at 2-year intervals for older children.
One investigator (OO) abstracted all medical records and was blinded to outcomes to identify diagnosis, gender, laterality, age of patient at reduction of the hip, and details of any interventions performed before presentation to our institutions. Because some patients underwent preceding interventions elsewhere and presented to us with a dislocated hip, for the purpose of this study, we defined “index procedure” as the reduction of the dislocated hip performed in either of our centers. Any preceding interventions that had been performed elsewhere were considered risk factors for ON and therefore were ascertained.
A standard radiographic protocol was used for all patients. A radiograph of the pelvis with the patient supine, centered on the hips and with both feet in 15° internal rotation, was made depending on age, at 60 to 80 kV, 4 to 40 mA, and a focus-to-film distance of 150 cm on a digital imaging system (5000R CR, Fuji, Bedford, UK). Pelvic AP (and frog-lateral where available) radiographs taken within 4 weeks before surgery were assessed for the presence of the femoral head ossific nucleus [10] on both sides and for severity of dislocation according to Tönnis [15]. We defined “presence of the femoral head ossific nucleus of the dislocated hip” as clear calcification proximal to the femoral metaphysis observed on a radiograph (AP and/or frog leg lateral) taken at the time of treatment. For patients with unilateral hip dislocation, we compared the nondislocated hip with the dislocated hip. If the normal hip clearly showed an ossified nucleus, the ossification of the dislocated hip must have been of the same radiographic density (but not necessarily of the same size) to be interpreted as present. The presence of ON was determined according to Bucholz and Ogden [2]; Grade I changes are limited to the femoral head with irregular ossification or hypoplasia of the femoral head but normal ossification of the metaphysis (Fig. 1). In Grade II, the lateral metaphysis is injured and the femoral head will grow into valgus (Fig. 2). For Grade III, the entire metaphysis is involved resulting in shortening of the femoral neck with trochanteric overgrowth (Fig. 3). An injury or defect along the medial metaphysis is present in Grade IV causing varus of the proximal femur (Fig. 4).
Fig. 1.
A pelvic radiograph obtained 8.5 years after closed reduction and adductor tenotomy in a female at the age of 10.4 months shows Grade I ON of the left hip. The changes are limited to the epiphysis, which appears hypoplastic compared with the right hip.
Fig. 2.
A pelvic radiograph obtained 13.1 years after open reduction shows Grade II ON of the left hip in a female at the age of 9 months. There is valgus alignment with a horizontally oriented physis.
Fig. 3.
A pelvic radiograph obtained 9.7 years after closed reduction and subsequent shelf acetabuloplasty shows Grade III ON of the left hip in a female at the age of 6.8 months. Typically, trochanteric overgrowth is seen with additional changes in the metaphysis and epiphysis.
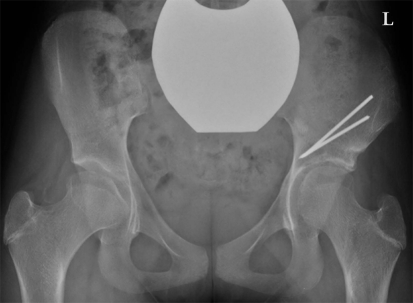
Fig. 4.
A pelvic radiograph obtained 9.6 years after open reduction shows Grade IV ON of the right hip in a female at the age of 5.3 months. The changes are subtle but varus alignment of the proximal femur can be seen.
We analyzed the radiographs of 105 hips electronically using magnified views and contrast control (Centricity PACS; GE Medical Systems, Chalfont St. Giles, UK, or Sienet Sky; Siemens AG Medical Solutions, Erlangen, Germany). We first used a random set of radiographs for training purposes to agree on definitions. Any patient identifiers were removed and radiographs were mixed before grading. All radiographs were graded blinded to treatment, exposure, and outcome. A research fellow (OO), a pediatric radiologist (ASD), and a pediatric hip surgeon (AR) graded all radiographs individually for the presence of the ossific nucleus and ON. These individuals were not involved in any of the surgical procedures. Their interobserver reliability was established. For grading the ossific nucleus, the kappa was 0.79 (95% confidence interval, 0.66–0.91), showing “substantial” reliability [8]. For grading ON, the kappa was 0.47 (95% confidence interval, 0.34–0.60), showing “moderate” reliability [8]. Radiographs also were graded separately by a senior pediatric hip surgeon (JHW) for the presence and type of ON. All gradings were compared and disagreements were resolved via consensus. We performed this multistep approach to ensure a thorough discussion of all radiographs on several occasions, which should minimize the potential for misclassification.
We used a univariable analysis to compare both groups for confounders and complications using chi square or exact test and t test. We explored collinearity and considered variables with r > 0.60 as collinear. Covariates significant at the 5% level were included in a log-binomial regression model to calculate the adjusted relative risk. Multivariable analysis was performed to control for factors other than the ossific nucleus that potentially could have caused ON; these included age at index reduction treatment center, and whether a revision hip reduction was performed. Eighteen percent of patients had bilateral hip involvement. We treated each hip as an independent event. The correlation in outcomes between the right and left hips in patients with bilateral hip involvement was marginal (r = 0.06). However, to test our assumption of independency, we performed a separate analysis after excluding the second hip randomly. No changes were noted. Sensitivity analyses were performed for eight hips in which data were missing regarding the ossific nucleus. We repeated the main analysis including these hips and classified them as “ossific nucleus present” and as “absent”. Both strategies did not significantly change the results of the main analysis. All analyses were performed using the SAS 9.2 statistical package (SAS Institute Inc, Cary, NC, USA).
Results
We found no association (relative risk, 1.27; 95% confidence interval, 0.76–2.13; p = 0.35) between the femoral head ossific nucleus and the presence of Grade I, II, III, or IV ON (Table 1).
Table 1.
Incidence of osteonecrosis in relation to the ossific nucleus
| Ossific nucleus | Osteonecrosis Grades I–IV* | No osteonecrosis | Adjusted p value | |
|---|---|---|---|---|
| Absent | 17 (40%) | 25 (60%) | 42 | |
| Present | 20 (32%) | 43 (68%) | 63 | |
| 37 (35%) | 68 (65%) | 105 | 0.61 |
| II–IV* | ||||
|---|---|---|---|---|
| Absent | 11 (26%) | 31 (74%) | 42 | |
| Present | 13 (21%) | 50 (79%) | 63 | |
| 24 (23%) | 81 (77%) | 105 | 0.76 |
* Bucholz and Ogden grades [2]. Two definitions for osteonecrosis, ie, Grades I-IV (top) and II-IV (bottom) are given. Based on the definition of osteonecrosis, the incidence was 35% or 24%, respectively.
If only radiographic changes of Grade II and greater were considered ON, the risk still was not increased (relative risk, 1.26; 95% confidence interval, 0.62–2.56; p = 0.51).
The incidence of ON was 35% (37 of 105). If only Bucholz and Ogden Grades II and greater were considered ON, the incidence was 23% (24 of 105). Bucholz and Ogden Grade II changes were observed most frequently with 17 of 105 hips showing changes, Grade I changes were observed in 13 of 105 hips, Grade III changes were observed in three of 105 hips, and Grade IV changes were observed in four of 105 hips. The incidences of ON were similar (p = 0.69) in patients younger than 12 months when treated and those older than 12 months when treated: 34% (27 of 79) versus 38% (10 of 26), respectively (Table 2).
Table 2.
Group differences based on univariate analysis.
| Variable | All hips or patients | Hips with osteonecrosis | Hips without osteonecrosis | Difference† |
|---|---|---|---|---|
| Baseline | ||||
| Dislocated hips | 105 | 37 (35%) | 65 (65%) | NA |
| Patients with bilateral dislocation | 16 | 7 (41%) | 9 (59%) | NA |
| Patients with unilateral dislocation | 73 | 24 (34%) | 49 (66%) | NA |
| Left hip: right hip | 67 : 38 | 23 : 14 | 44 : 24 | p = .699 |
| Mean age at index procedure (months) | 8.96 ± 4.04 | 9.38 ± 3.98 | 8.72 ± 4.08 | p = .719 |
| Risk factors | ||||
| Ossific nucleus present | 63 | 20 | 43 | p = .350 |
| Age at index reduction < 12 months (hips) | 79 | 27 | 52 | p = .717 |
| Severity of dislocation (Tonnis grade) | p = .102 | |||
| I | 12 | 2 | 10 | NA |
| II | 12 | 4 | 8 | NA |
| III | 15 | 6 | 9 | NA |
| IV | 26 | 15 | 11 | NA |
| Preceding failed harness treatment | 50 | 19 | 31 | p = .732 |
| Preoperative skin traction | 60 | 21 | 39 | p = .990 |
| Preceding arthrogram of hip | 13 | 6 | 7 | p = .164 |
| Preceding closed reduction | 2 | 2 | 0 | p = .035† |
| Index procedure | ||||
| Arthrogram | 47 | 20 | 27 | p = .124 |
| Adductor tenotomy | 89 | 31 | 58 | p = .867 |
| Closed reduction | 67 | 20 | 47 | p = .137 |
| Open reduction | 42 | 19 | 23 | p = .081 |
| Outcomes after index procedure | ||||
| Failed index reduction* | 18 | 12 | 6 | p = .002† |
| Subluxation | 5 | 3 | 2 | p = .330 |
| Redislocation* | 13 | 9 | 4 | p = .006† |
| Revision closed reduction | 3 | 0 | 3 | p = .549 |
| Revision open reduction* | 15 | 12 | 3 | p < .0001† |
| Surgeon* | p = .0007† | |||
| 1 | 47 | 10 (21%) | 37 | NA |
| 2 | 22 | 15 (68%) | 7 | NA |
| 3 | 36 | 12 (33%) | 24 | NA |
| Center* | 105 | 37 | 68 | p = .007† |
| 1 | 58 | 27 | 31 | NA |
| 2 | 47 | 10 | 37 | NA |
* Denotes collinearity; †significant; NA, not applicable.
Six of the 14 variables explored for their association with ON in univariable analysis were significant and some were collinear (Table 2). Statistical adjustment for the covariates mentioned led to a change of the crude relative risk of ON in the presence of an ossific nucleus but the risk still was not decreased (adjusted relative risk, 0.86; 95% confidence interval, 0.36–1.81; p = 0.61). If only radiographic changes of Grade II and greater were considered ON, the adjusted relative risk was 1.12 (95% confidence interval, 0.54–2.30; p = 0.76).
Sixteen patients (18 hips) underwent revision operations performed by the same surgeon who performed the index procedures (Table 3). The mean age of the patients at the time of the revision surgery was 17.7 ± 9.7 months. The radiographic followup for these 16 patients (18 hips) was 10.2 ± 4.6 years, which was similar to that (p = 0.15) for other patients in the study. ON developed in 12 of 18 hips (67%) (p = 0.002). The number of revision operations did not increase the risk (p = 0.48; exact test) for ON.
Table 3.
Details of 18 patients who required revision surgery.
| Patient number | Side | Gender | Ossific nucleus | ON* | Followup (years) | Age at index surgery (months) | Failed abduction harness | Index procedure | Adductor release | Surgeon | Outcome after index procedure | Revision operation | Total number of revision operations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | R | F | Present | 0 | 10.68 | 5.00 | Yes | OR | Yes | B | Subluxation | IO | 1 |
| 2 | R | F | Present | 4 | 5.12 | 7.33 | Yes | CR | Yes | A | Subluxation | OR, IO | 1 |
| 3 | L | F | Present | 2 | 13.25 | 6.15 | No | OR | Yes | C | Subluxation | OR | 1 |
| 4 | L | F | Absent | 2 | 6.33 | 11.24 | Yes | OR | Yes | B | Subluxation | OR, VDRO | 2 |
| 5 | L | F | Absent | 0 | 5.52 | 6.90 | Yes | CR | Yes | B | Subluxation | OR, VDRO | 1 |
| 6 | L | M | Absent | 1 | 16.16 | 16.80 | No | CR | Yes | A | Dislocation | CR | 1 |
| 7 | L | M | Absent | 1 | 8.88 | 1.78 | Yes | CR | No | A | Dislocation | OR | 1 |
| 8 | L | M | Absent | 0 | 9.31 | 3.39 | Yes | OR | Yes | A | Dislocation | OR, IO | 1 |
| 9 | R | M | Absent | 0 | 17.65 | 3.29 | Yes | CR | Yes | A | Dislocation | OR | 1 |
| 9 | L | M | Absent | 2 | 17.65 | 3.29 | Yes | CR | Yes | A | Dislocation | OR | 1 |
| 10 | R | F | Absent | 3 | 14.47 | 17.85 | No | OR | Yes | C | Dislocation | OR, VDRO | 1 |
| 10 | L | F | Absent | 3 | 14.47 | 17.85 | No | OR | Yes | C | Dislocation | OR, VDRO | 1 |
| 11 | L | F | Present | 3 | 9.67 | 6.74 | Yes | CR | Yes | B | Dislocation | OR, VDRO | 3 |
| 12 | L | F | Absent | 4 | 3.59 | 12.72 | No | CR | No | B | Dislocation | OR, VDRO | 1 |
| 13 | L | F | Absent | 0 | 5.64 | 5.46 | Yes | CR | Yes | B | Dislocation | CR | 1 |
| 14 | R | F | Absent | 0 | 7.02 | 10.62 | No | CR | Yes | B | Dislocation | OR | 1 |
| 15 | R | F | Present | 1 | 5.47 | 5.62 | Yes | CR | Yes | C | Dislocation | OR, IO | 1 |
| 16 | L | F | Absent | 2 | 13.72 | 4.04 | No | CR | Yes | C | Dislocation | OR, VDRO | 1 |
ON = osteonecrosis; CR = closed reduction; OR = open reduction; IO = innominate osteotomy; VDRO = varus-derotation osteotomy;
* According to Bucholz and Odgen.
Discussion
Controversy remains whether the presence of the femoral head ossific nucleus at the time of hip reduction protects against the development of ON. Although some authors have suggested that the present ossific nucleus at the time of hip reduction can protect against the development of ON [4, 13], others have not observed this effect [7, 10, 11]. Previous studies were limited in that they were too small, lacked controls, had limited followup, or did not report adequate statistics [11]. We performed the current study to determine the incidence of ON in children undergoing treatment for hip dislocation and the presence and absence of the ossific nucleus.
Our study has limitations. First, there were differences in baseline characteristics and cointerventions between groups. We addressed this by the statistical analysis. Second, retrospective studies risk measurement bias. However, we took several steps to mitigate this risk as outlined. The interobserver reliability was “moderate” for grading ON; however, all disagreements were resolved in consensus among three experienced professionals. We could not ascertain the preoperative severity of dislocation for some hips because adequate radiographs were not available. Third, although the surgical protocol was the same for all patients as confirmed by a review of all case notes, we cannot exclude small variations of the protocol between surgeons. Because we adjusted the analysis for surgeon, potential variations should not significantly influence the estimates of effect. Fourth, the study was powered to detect a difference greater than 24% in the incidence of ON. It was underpowered to detect smaller differences. However, we believe 25% is a plausible cutoff considering the results of previous studies [1, 7, 10, 13]. Fifth, because the radiographic changes associated with ON develop with time, a minimum followup of 3 years is required [2, 4]. However, Grade II ON was first evident in patients at an age of 10 years, as reported in one study [6]. Our patients (42 hips) had a followup age younger than 10 years (mean, 7 ± 1.9 years) with no signs of ON. It remains purely speculative if a proportion of these patients could have ON develop in the future and we will follow these patients, however, we suspect there will be relatively few who have ON develop and these would not alter our findings.
We found only small and insignificant differences in the crude and adjusted relative risks of ON among patients with and without an ossific nucleus. The presence of the ossific nucleus did not protect against the development of ON, regardless if mild radiographic Grade I changes were considered ON or normal hips. Hips showing an ossific nucleus at the time of hip reduction showed an insignificant tendency toward better outcomes. Our results are consistent with those of two previous studies that found no protective effect of the ossific nucleus [7, 10], and do not strengthen the evidence for strategies aimed at delaying the treatment of hip dislocation in the absence of the ossific nucleus [1, 4].
Our observations also clarified the question regarding a protective effect of the ossific nucleus for ON of Grade II and greater [11]. In a previous meta-analysis, a relative risk reduction of 60% was reported for the development of ON of Grade II or greater in hips with an ossific nucleus [11]. In contrast, we found a relative risk reduction of only 20%.
The incidence of ON in our study was similar to incidences reported in previous studies [1, 4, 7, 13] (Table 1). The age range of patients was similar to those reported in other studies [1, 7, 10]. In estimating the effect of the ossific nucleus, we controlled for age and found that children treated at a younger age were not more likely to have ON develop. As in previous studies [11], we also included patients who underwent closed or open reductions but we did not find that the technique itself was a predictor for ON.
We deliberately included more than one surgeon to increase the generalizability of the results. The rates of open and closed reductions and the number of preceding treatments were similar among the surgeons. For each surgeon’s subgroup, the ages of the patients at hip reduction were 7, 10, and 10 years, and their ages at followup were 11, 11, and 9 years, respectively. However, the incidence of ON differed among surgeons. Proficiency bias (a situation in which the treatments are not applied equally to all subjects because of skill mix among surgeons) could explain the different incidences of ON among surgeons. We adjusted the statistical analysis for the difference in surgeon-related incidence, and still found no decreased risk of ON in the presence of an ossific nucleus. The surgeons were experienced pediatric orthopaedic specialists. It is unlikely that a study involving less experienced surgeons would show different results; hypothetically, their overall rate of ON could be greater regardless of the ossific nucleus.
Whether an infant underwent a revision reduction was a major predictor for the development of ON, a plausible observation considering that such treatment poses additional risk to the femoral head blood supply. Unsuccessful treatment with an abduction device such as a Pavlik harness was not associated with an increased risk for ON, an observation made by others [3, 10, 13].
The femoral head ossific nucleus was not associated with the development of ON in this sample, regardless of the definition of ON. The overall incidence of ON was similar to that reported in the literature, suggesting we studied a representative sample of children with DDH. Patient followup was well beyond the commonly suggested 3 years. Adjusted effect estimates were derived after examining all potential confounders, which further underpins the robustness of the data. The results of our study patients are likely to be generalizable to other similar patients with DDH. We believe our study provides the strongest evidence to date regarding the relationship between the femoral head ossific nucleus and the development of ON. Our study was not designed to determine if the treatment of DDH should be delayed in the absence of the ossific nucleus. This question of intervention ideally is studied in a randomized clinical trial.
Acknowledgments
We thank D.H.A. Jones and J. Fixsen whose former patients were part of this research.
Footnotes
One or more of the authors has received funding from Royal College of Surgeons of England (AR, OO) and Arthritis Research UK (AR).
Each author certifies that his institution has approved for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Institute of Child Health, University College London, London, UK.
References
- 1.Agus H, Omeroglu H, Ucar H, Bicimoglu A, Turmer Y. Evaluation of the risk factors of avascular necrosis of the femoral head in developmental dysplasia of the hip in infants younger than 18 months of age. J Pediatr Orthop B. 2002;11:41–46. doi: 10.1097/01202412-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bucholz RW, Ogden JA. Patterns of Ischemic Necrosis of the Proximal Femur in Nonoperatively Treated Congenital Hip Disease. St Louis, MO: CV Mosby Company; 1978:43–63.
- 3.Carney BT, Clark D, Minter CL. Is the absence of the ossific nucleus prognostic for avascular necrosis after closed reduction of developmental dysplasia of the hip? J Surg Orthop Adv. 2004;13:24–29. [PubMed] [Google Scholar]
- 4.Clarke NM, Jowett AJ, Parker L. The surgical treatment of established congenital dislocation of the hip: results of surgery after planned delayed intervention following the appearance of the capital femoral ossific nucleus. J Pediatr Orthop. 2005;25:434–439. doi: 10.1097/01.bpo.0000158003.68918.28. [DOI] [PubMed] [Google Scholar]
- 5.Fleissner PR, Jr, Ciccarelli CJ, Eilert RE, Chang FM, Glancy GL. The success of closed reduction in the treatment of complex developmental dislocation of the hip. J Pediatr Orthop. 1994;14:631–635. doi: 10.1097/01241398-199409000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Kim HW, Morcuende JA, Dolan LA, Weinstein SL. Acetabular development in developmental dysplasia of the hip complicated by lateral growth disturbance of the capital femoral epiphysis. J Bone Joint Surg Am. 2000;82:1692–1700. doi: 10.2106/00004623-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Konigsberg DE, Karol LA, Colby S, O’Brien S. Results of medial open reduction of the hip in infants with developmental dislocation of the hip. J Pediatr Orthop. 2003;23:1–9. doi: 10.1097/00004694-200301000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 9.Luhmann SJ, Bassett GS, Gordon JE, Schootman M, Schoenecker PL. Reduction of a dislocation of the hip due to developmental dysplasia: implications for the need for future surgery. J Bone Joint Surg Am. 2003;85:239–243. doi: 10.2106/00004623-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Luhmann SJ, Schoenecker PL, Anderson AM, Bassett GS. The prognostic importance of the ossific nucleus in the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am. 1998;80:1719–1727. doi: 10.2106/00004623-199812000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Roposch A, Stohr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip: a meta-analysis. J Bone Joint Surg Am. 2009;91:911–918. doi: 10.2106/JBJS.H.00096. [DOI] [PubMed] [Google Scholar]
- 12.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961;43:518–539. [PubMed] [Google Scholar]
- 13.Segal LS, Boal DK, Borthwick L, Clark MW, Localio AR, Schwentker EP. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19:177–184. doi: 10.1097/00004694-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Spence G, Hocking R, Wedge JH, Roposch A. The effect of innominate and varus-derotation osteotomy on acetabular development in developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:2622–2636. doi: 10.2106/JBJS.H.01392. [DOI] [PubMed] [Google Scholar]
- 15.Tönnis D. Nomenclature and classification of congenital hip dislocation. In: Tönnis D, ed. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987:80–83.
- 16.Weinstein SL. The medial approach in congenital dislocation of the hip. Isr J Med Sci. 1980;16:272–275. [PubMed] [Google Scholar]