Abstract
Aims
Data suggest that hyperpalatable foods may be capable of triggering an addictive process. Although the addictive potential of foods continues to be debated, important lessons learned in reducing the health and economic consequences of drug addiction may be especially useful in combating food-related problems.
Methods
In the current paper, we review the potential application of policy and public health approaches that have been effective in reducing the impact of addictive substances to food-related problems.
Results
Corporate responsibility, public health approaches, environmental change, and global efforts all warrant strong consideration in reducing obesity and diet-related disease.
Conclusions
Although there exist important differences between foods and addictive drugs, ignoring analogous neural and behavioral effects of foods and drugs of abuse may result in increased food-related disease and associated social and economic burdens. Public health interventions that have been effective in reducing the impact of addictive drugs may have a role in targeting obesity and related diseases.
Keywords: Food, obesity, addiction, public health
The food environment has changed dramatically with the influx of hyperpalatable foods that are engineered in ways that appear to surpass the rewarding properties of traditional foods (e.g., vegetables, fruits, nuts) by increasing fat, sugar, salt, flavors, and food additives to high levels (Table 1). Foods share multiple features with addictive drugs. Food cues and consumption can activate neurocircuitry (e.g., meso-cortico-limbic pathways) implicated in drug addiction [1, 2]. Animals given intermittent access to sugar exhibit behavioral and neurobiological indicators of withdrawal and tolerance, cross-sensitization to psychostimulants, and increased motivation to consume alcohol [3]. Rats consuming diets high in sugar and fat demonstrate reward dysfunction associated with drug addiction, downregulation of striatal dopamine receptors, and compulsive eating including continued consumption despite receipt of shocks [4].
Table 1.
Composition of traditional and hyperpalatable1
| Food | Portion Size | Type of Food | Sugar | Fat | Sodium | # of Ingredients |
|---|---|---|---|---|---|---|
| Apple | 1 medium | Traditional | 19 g | 0 g | 2 mg | 1 |
| Chicken breast, roasted | 3 ounces | Traditional | 0 g | 3 g | 63 mg | 1 |
| Lettuce | 1 cup shredded | Traditional | 0 g | 0 g | 10 mg | 1 |
| Tomato | 1 medium | Traditional | 3 g | 0 g | 6 mg | 1 |
| Orange | 1 cup, sections | Traditional | 17 g | 0 g | 0 mg | 1 |
| Coca-cola | 1 can | Hyperpalatable | 39 g | 0 g | 45 mg | 6 |
| Dairy Queen Chocolate Ice Cream Cone | 1 medium cone | Hyperpalatable | 34 g | 10 g | 160 mg | 22 |
| McDonald's French Fries | 1 medium | Hyperpalatable | 0 g | 19 g | 270 mg | 9 |
| Cinnamon Toast Crunch Cereal | ¾ cup (milk not included) | Hyperpalatable | 10 g | 3 g | 217 mg | 27 |
| DiGiorno Pepperoni Pizza | ⅙ of pizza | Hyperpalatable | 7 g | 13 g | 910 mg | 8 |
Foods were chosen based on their inclusion in the USDA report on foods commonly eaten in the United States. All nutrition information is based on the United States Department of Agriculture Nutrition Facts, nutrition information from the company website, or nutrition information provided on the product's packaging.
In humans, diminished striatal dopamine receptor availability and striatal dysfunction have been associated with obesity [5] and prospective weight gain [6]. Foods and abused drugs may induce similar behavioral sequelae including craving, continued use despite negative consequences, and diminished control over consumption [7]. If foods are capable of triggering addictive processes, applying lessons learned from drug addiction to obesity, associated metabolic problems, and diet-related diseases would suggest policy directions and prevention and treatment interventions [2, 8].
Substance-Related Focus
Genetic and environmental (e.g., psychosocial) factors contribute to drug addiction. These factors can interact with drugs that may directly alter brain function, reinforce drug-seeking behaviors, and shift attention to substance-related cues; i.e., substances may promote repeated over-consumption [9]. Although an acknowledgment of personal responsibility for one's behaviors remains an important component of many addiction interventions, progress was made in addressing drug addiction when a focus changed from blaming individuals with addictions to understanding that drugs may “hijack” brain circuitry. A similar conceptual shift may help in the food and obesity arena.
Consider tobacco. It can be argued that for years tobacco companies emphasized personal responsibility over corporate responsibility for developing addictive products. This perspective likely delayed drug-related interventions and policy changes by focusing attention on individual-based treatments [10]. Although individual-focused treatments for drug addictions are helpful and cost-effective [11], a more constructive view of tobacco-related behaviors ultimately also incorporated a focus on the addictive drug and implemented bold legal and policy alterations to the tobacco environment (e.g., taxation, limits on marketing and access, and actions of the state attorneys general).
Initial approaches to obesity and associated metabolic disorders focused primarily on individual risk factors (e.g., genetics, personal responsibility, and individual behavior change) [12], mirroring early “individualistic” approaches to tobacco use that had important but arguably limited public health impact. Little attention has been given to how the engineering and marketing of food may interact with possible risk factors to generate brain responses like those to traditional drugs of abuse. If hyperpalatable foods have a fraction of the effects of addictive drugs, the public health significance could be substantial because of widespread access and exposure to highly marketed, low-cost, nutrient-poor, and calorie-dense products. If the biological effects approach those of addictive drugs, far-reaching policies may be indicated. Given the public health impact, attention should be given to the properties of foods and industry's responsibility in creating them.
Public Health Perspective
Considering addictions within a public health model is important. A sizable proportion of the population develops addictions, and an additional proportion experiences “sub-clinical” problems with addictive substances, resulting in significant social cost. For example, although 12.5% of Americans develop alcohol dependence [13], alcohol misuse contributes to 4.0% of the global burden of disease [14]. With food, the public health significance may not occur solely from a relatively small group who might become clinically dependent on foods, but from the likely larger group of adults and children who overeat enough to compromise their health. Reports of emotional eating, strong food cravings, difficulty controlling high-calorie food consumption despite known consequences, and sub-clinical binge eating are widespread, with health care costs associated with being overweight or obese projected to exceed 850 billion dollars annually by 2030 in the United States alone [15]. To reduce these costs, it will be necessary to focus beyond personal responsibility or clinical disorders, a lesson learned from addressing nicotine and drug use. Policy focused on changing the availability, attributes and costs of tobacco products has resulted in significant public health gains. Similar environmental interventions may be needed to reduce problematic over-consumption of potentially addictive foods.
Divergent Approaches
Contrasts between historical tobacco-related versus current food-related interventions are both striking and illustrative. First, the cost of tobacco products in the Western world has increased primarily due to taxation and discontinued government subsidies [16]. In contrast, ingredients for potentially addictive foods (e.g., corn, sugar) are inexpensive because they are heavily subsidized by many governments. Suggestions to tax hyperpalatable foods, like soda, are currently being debated [17]. Evidence from tobacco suggests that that increasing the price of hyperpalatable foods through taxation and shifting subsidies could have beneficial effects on consumption. Second, restrictions placed on marketing tobacco directly to children have contributed to reduced tobacco use. In contrast, hyperpalatable foods are the most frequently marketed products specifically targeting children and adolescents [18]. Food advertising has become increasingly difficult for parents to monitor, given the increase in product placements, advergaming (i.e., the use of videogames to promote products or ideas), and school-related marketing enterprises [19]. Following the tobacco precedent, restricting childhood exposure to advertising of potentially addictive foods may be an important public health strategy.
In addition to cost and marketing issues, accessibility is another critical factor in limiting tobacco use. Cigarettes were once widely sold in vending machines in public locations. In addition to providing greater general access, tobacco vending machines provided a major point of access for minors to illegally purchase cigarettes [20]. As of 2003, most American states have restricted the use of tobacco vending machines [20], and similar regulations limit accessibility to alcohol, with greater restrictions for more potent alcoholic beverages. Beer is typically more widely available for purchase (e.g., in gas stations, grocery stores) and subject to less taxation than liquor. Alcohol potency is associated with abuse potential; hence, liquor sales are sometimes restricted to state-run stores and subject to higher taxes [21]. In contrast, foods with lower nutritional value and arguably greater abuse potential (i.e., high sugar, high fat) typically are more widely available and cost less than foods with higher nutritional value and arguably lower abuse potential (i.e., fruits, vegetables) [22]. Based on approaches to alcohol, food-related problems may be diminished by reducing the availability of less nutritious, hyperpalatable foods while increasing access to healthier ones.
Global Impact
Another important issue is the global marketing and sale of addictive products. Facing declining sales in the Western world, tobacco companies appeared to become more aggressive elsewhere. As tobacco use decreased by approximately 50% over the past three decades in the United States, it simultaneously increased by 3.4% per a year in developing countries [23]. As the diet of hyperpalatable, heavily-marketed foods becomes a global phenomenon, protective policies across nations warrant consideration.
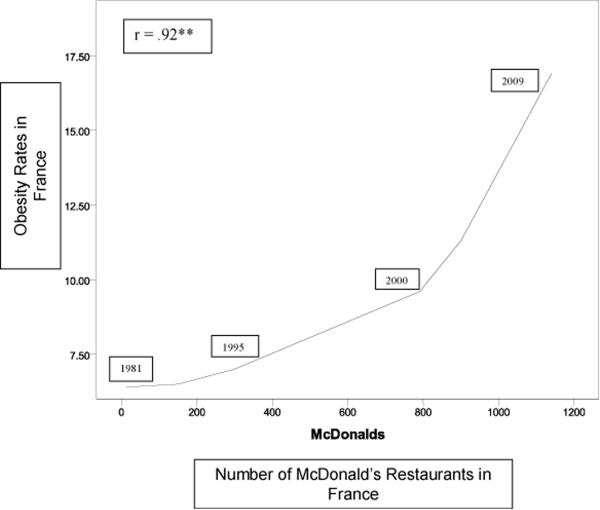
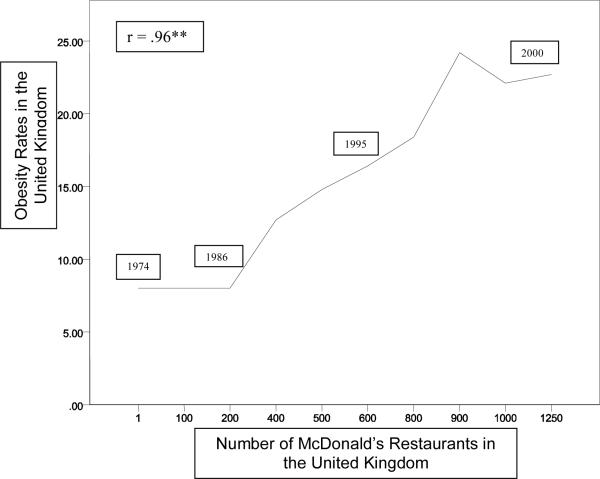
Obesity rates have been rising rapidly throughout the world, first in developed nations and more recently in poorer countries. Although many contributing factors may exist, the changing food environment warrants particular attention. For example, obesity rates in countries such as France and the United Kingdom have been rising in parallel with increases in availability of highly processed foods and fast-food chains [24, 25] (Fig. 1a, and b). Similar trends have been found between sugar-sweetened beverage consumption and obesity rates [17], with increased sugar-sweetened beverage consumption prospectively predicting obesity in children [26]. Countries that have historically been successful in reducing diet-related disease, such as Finland, have seen rising obesity rates in the current food environment [27]. As food markets become more global, trade boundaries between countries become more porous, allowing for a greater influx of hyperpalatable foods. Traditionally, addiction prevention across borders (e.g., supply-focused efforts to restrict drug trafficking) has been challenging and costly, and applying lessons learned from such international endeavors could be valuable. As food advertising increasingly focuses on global forms of media, such as the Internet and product placements in film, it becomes increasingly difficult for any single government to effectively regulate food marketing. As with tobacco, global interventions may best reduce the worldwide impact of potentially addictive foods.
Figure 1a.
Temporal plots of obesity rates and McDonald's fast food venues in France2,3
2All obesity data were acquired from the World Health Organization and the United Kingdom Health Behavior Survey. All McDonald's data were acquired from press releases, McDonald's fact sheets, Fantasia 199521, and DeBres 200522.
3**. Correlation is significant at .01 level (1-sided)
Figure 1b.
Temporal plots of obesity rates and McDonald's fast food venues in the United Kingdom4
4**. Correlation is significant at .01 level (1-sided)
Relevant Differences
Although foods share characteristics with addictive drugs, important differences exist. Unlike drugs, foods are necessary for survival. The essential nature of eating contrasts with the use of traditionally addictive substances and complicates food-related interventions. Multiple addictive drugs include few ingredients and the addictive component has been identified (e.g., ethanol, heroin). In contrast, hyperpalatable foods typically include multiple ingredients and research into which components may be addictive is at a relatively early stage. Policy and regulatory efforts will be aided by research into which food elements may trigger addictive processes. Such information may help generate improved interventions early in development. As foods are consumed more frequently and earlier in life than are abused drugs, early and repeated exposure during childhood may have long-lasting effects and prevention strategies targeting youth could have important implications as people mature.
Summary
Foods, particularly hyperpalatable ones, demonstrate similarities with addictive drugs. Although the potential addictive nature of foods may not fully explain obesity or excessive food consumption, important lessons learned from drug addictions can inform methods to reduce escalating food-related problems and the associated personal, public health and economic costs. Corporate responsibility, public health approaches, environmental change, and global efforts all seem essential in reducing food- and substance-related problems. Such approaches could be enacted in conjunction with individual-focused behavioral and pharmacological efforts that could also benefit from considering similarities between food-related conditions like obesity and drug addiction [2, 8]. Ignoring the analogous neural and behavioral effects of foods and drugs of abuse may result in a substantial loss of time, resources, and lives, as we rediscover lessons learned in reducing the impact of addictive substances.
Acknowledgments
This research was supported by the National Institutes of Health grants P50 DA016556, UL1-DE19586, K24 DK070052, RL1 AA017537, and RL1 AA017539, the Office of Research on Women's Health, the NIH Roadmap for Medical Research/Common Fund, the VA VISN1 MIRECC, and the Rudd Center. The contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the other funding agencies.
Dr. Potenza has received financial support or compensation for the following: Dr. Potenza consults for and is an advisor to Boehringer Ingelheim; has financial interests in Somaxon; has received research support from the National Institutes of Health, Veteran's Administration, Mohegan Sun Casino, the National Center for Responsible Gaming and its affiliated Institute for Research on Gambling Disorders, and Forest Laboratories pharmaceuticals; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for law offices on issues related to addictions or impulse control disorders; has provided clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has guest-edited journal sections; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts.
Footnotes
All authors report no conflict of interest with respect to the content of this paper.
Conflicts of Interest All authors report no conflict of interest with respect to the content of this paper. Dr. Potenza has received financial support or compensation for the following: Dr. Potenza consults for and is an advisor to Boehringer Ingelheim; has financial interests in Somaxon; has received research support from the National Institutes of Health, Veteran's Administration, Mohegan Sun Casino, the National Center for Responsible Gaming and its affiliated Institute for Research on Gambling Disorders, and Forest Laboratories pharmaceuticals; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for law offices on issues related to addictions or impulse control disorders; has provided clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has guest-edited journal sections; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts.
References
- 1.Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci. 2008;363:3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blumenthal DM, Gold MS. Neurobiology of food addiction. Curr Opin Clin NutrMetab Care. 2010;13:359–365. doi: 10.1097/MCO.0b013e32833ad4d4. [DOI] [PubMed] [Google Scholar]
- 3.Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32:20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson PM, Kenny PJ. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nature. 2010;13:635–641. doi: 10.1038/nn.2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang G-J, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. Brain dopamine and obesity. Lancet. 2010;357:354–357. doi: 10.1016/s0140-6736(00)03643-6. [DOI] [PubMed] [Google Scholar]
- 6.Stice E, Spoor S, Bohon C, Small DH. Relation between obesity and blunted striatal response to food is moderated by Taq1A A1 Allele. Nature. 2008;322:449–452. doi: 10.1126/science.1161550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3:1–7. doi: 10.1097/ADM.0b013e318193c993. [DOI] [PubMed] [Google Scholar]
- 8.Merlo LJ, Stone AM, Gold MS. Co-occurring addiction and eating disorders. In: Riess RK, Fiellin D, Miller S, Saitz R, editors. Principles of Addiction Medicine. 4th Edition Lippincott Williams & Wilkins; Kulwer (NY): 2009. pp. 1263–1274. [Google Scholar]
- 9.Volkow ND, Li T-K. Drug addiction: the neurobiology of behavior gone awry. Nat Rev Neurosci. 2004;5:963–970. doi: 10.1038/nrn1539. [DOI] [PubMed] [Google Scholar]
- 10.Brownell KD, Warner KE. The perils of ignoring history: big tobacco played dirty and millions died. How similar is big food? Milbank Q. 2009;87:259–94. doi: 10.1111/j.1468-0009.2009.00555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ettner SL, Huang D, Evans E, Ash DR, Hardy M, Jourabchi M, et al. Benefit-cost in the California treatment outcome project: Does substance abuse treatment “pay for itself”? Health Services Research. 2006;41:192–213. doi: 10.1111/j.1475-6773.2005.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brownell KD, Kersh R, Ludwig DS, Post RC, Puhl RM, Schwartz MB, et al. Personal responsibility and obesity: a constructive approach to a controversial issue. Health Aff. 2010;29:379–87. doi: 10.1377/hlthaff.2009.0739. [DOI] [PubMed] [Google Scholar]
- 13.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 14.Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16:2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 16.Frieden TR, Bloomberg MR. How to prevent 100 million deaths from tobacco. Lancet. 2007;369:1758–61. doi: 10.1016/S0140-6736(07)60782-X. [DOI] [PubMed] [Google Scholar]
- 17.Brownell KD, Frieden TR. Ounces of prevention - The public policy case for taxes on sugared beverages. NEJM. 2009;360:1805–1808. doi: 10.1056/NEJMp0902392. [DOI] [PubMed] [Google Scholar]
- 18.Powell LM, Szczypka G, Chaloupka FJ, Braunschweig CL. Nutritional content of television food advertisements seen by children and adolescents in the United States. Pediatrics. 2007;120:576–583. doi: 10.1542/peds.2006-3595. [DOI] [PubMed] [Google Scholar]
- 19.Harris JL, Pomeranz JL, Lobstein T, Brownell KD. A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health. 2009;30:211–25. doi: 10.1146/annurev.publhealth.031308.100304. [DOI] [PubMed] [Google Scholar]
- 20.State Cancer Legislative Database Update. State laws addressing youth access to tobacco products through vending machines. 2003;53:7. [Google Scholar]
- 21.Alcohol Control Systems: Retail Distribution Systems for Spirits [Internet] Alcohol Policy Information System. [Updated 2009 January 1; cited 2010 May 5 2010]. Available from: http://www.alcoholpolicy.niaaa.nih.gov/Alcohol_Control_Systems_Retail_Distrib ution_Systems_for_Spirits.html?tab=Maps.
- 22.Jetter KM, Cassady DL. The availability and cost of healthier food alternatives. Am J Prev Med. 2006;30:38–44. doi: 10.1016/j.amepre.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization . Combating the Tobacco Epidemic. Geneva, Switzerland: 1999. World Health Report 1999. [Google Scholar]
- 24.Fantasia R. Fast food in France. Theory Soc. 1995;24:201–243. [Google Scholar]
- 25.DeBres K. Burgers for Britain: A cultural geography of McDonald's UK. J Cult Geogr. 2005;22:115–139. [Google Scholar]
- 26.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: A prospective, observational analysis. Lancet. 2001;357:505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 27.Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–18. doi: 10.1093/ije/dyp330. [DOI] [PubMed] [Google Scholar]