Abstract
The main aim of this study was to provide anatomical data on the heights of the human intervertebral discs for all levels of the thoracic spine by direct and radiographic measurements. Additionally, the heights of the neighboring vertebral bodies were measured, and the prediction of the disc heights based only on the size of the vertebral bodies was investigated. The anterior (ADH), middle (MDH) and posterior heights (PDH) of the discs were measured directly and on radiographs of 72 spine segments from 30 donors (age 57.43 ± 11.27 years). The radiographic measurement error and the reliability of the measurements were calculated. Linear and non-linear regression analyses were employed for investigation of statistical correlations between the heights of the thoracic disc and vertebrae. Radiographic measurements displayed lower repeatability and were shorter than the anatomical ones (approximately 9% for ADH and 37% for PDH). The thickness of the discs varied from 4.5 to 7.2 mm, with the MDH approximately 22.7% greater. The disc heights showed good correlations with the vertebral body heights (R2, 0.659–0.835, P-values < 0.005; anova), allowing the generation of 10 prediction equations. New data on thoracic disc morphometry were provided in this study. The generated set of regression equations could be used to predict thoracic disc heights from radiographic measurement of the vertebral body height posterior. For the creation of parameterized models of the human thoracic discs, the use of the prediction equations could eliminate the need for direct measurement on intervertebral discs. Moreover, the error produced by radiographic measurements could be reduced at least for the PDH.
Keywords: anatomical measurement, disc morphometry, intervertebral disc height, radiographic measurement, thoracic vertebrae
Introduction
The thoracic spine is the most common site for spinal deformities such as kyphosis and scoliosis (Lord et al. 1995). Despite this, and in contrast to cervical and lumbar discs, the morphometry of the adult thoracic intervertebral disc (TIVD) has received limited attention and until now relatively few data have been available in the current literature. For example, accurate anatomical data on the heights of the TIVD including all levels of the thoracic spine of a representative adult population are very scarce. Previous studies showed limitations either in accuracy, study population, parameters recorded or disc level. Anatomical data on TIVD are a requirement for both the development of new spinal implants and for the creation of mathematical models of the human spine.
Direct measurement on specimens is the best method for extracting morphometric data from anatomical structures. However, relatively few studies on TIVD morphometry have been carried out due to the difficulty in obtaining intact human specimens. Hurxthal (1968) and Manns et al. (1986) measured anterior disc height (ADH) using radiographs of female patients, but only a limited number of thoracic levels (from T5–6 to T11–12) were investigated. Todd & Pyle (1928) measured only ADH and only male cadavers were used, while the age distribution for this sample was not reported; Pooni et al. (1986) used only a few elderly cadavers between 73 and 85 years old, but the data were presented only as a percentage of the total spine height; radiographic measurements by Goh et al. (1999) and Giles & Singer (2000) were used to investigate thoracic kyphosis, but the ADH and posterior heights (PHD) of the disc were not provided and only a segmental trend was reported. Some of these measurements were performed on plain radiographs considering the superior and inferior vertebral corners (Pooni et al. 1986; Goh et al. 1999; Giles & Singer, 2000). Whereas it has the advantage of eliminating the need for sample preparation, in some reports on lumbar discs the accuracy and repeatability of radiographic measurements of disc heights have been questioned (Pope et al. 1977; Andersson et al. 1981). This was due to a lack of the requisites needed to perform geometric measurements with relative accuracy such as the use of a standard vertebral position, control of the film–specimen–focus distances and optimal visualization of the bony landmarks. Furthermore, in some investigations on TIVD morphometry, errors due to radiographic magnification bias or the inter- and intraobserver reliability of the radiographic measurements were not taken into account (Hurxthal, 1968; Manns et al. 1986; Pooni et al. 1986). The error of radiographic measurement of the heights of TIVDs was never accurately investigated.
Statistical correlations between the main anatomical dimensions of the human vertebral structures have been quantified in previous studies (Scoles et al. 1988; Lavaste et al. 1992; Laporte et al. 2000; Breglia, 2006; van der Houwen et al. 2010). Recently, thoracic and lumbar vertebral morphometry was predicted with reasonable accuracy using only the dimension of the vertebral body heights measured on lateral radiographs and a set of regression equations (Kunkel et al. 2010, 2011). A similar method could be used for the prediction of TIVD dimensions as an alternative to anatomical or radiographic measurements. However, the relationships between morphometric dimensions of the TIVD and vertebrae have never been investigated. To the authors’ knowledge, to date no report has investigated the possibility of establishing useful predictors for TIVD dimensions based only on the size of the vertebral bodies. Such a method could provide data for patient-specific modeling of the spine where the shape and size of the TIVD need to be considered.
The main aim of this study was to provide anatomical data on the heights of the human intervertebral discs for all levels of the thoracic spine by direct and radiographic measurements. The radiographic measurements error was also estimated. Additionally, the heights of the neighboring vertebral bodies were measured, and the prediction of the disc heights based only on the size of the vertebral bodies was investigated.
Materials and methods
Study sample and parameters
Seventy-two isolated spine segments (each segment includes a vertebral pair and intervertebral disc between the vertebrae) from a total of 30 human spines were examined. For morphometric measurements and statistical analyses six segments were available for each spinal level from C7–T1 to T11–12. Thirty-seven spine segments were from 15 females (mean age of 58.67 ± 10.74 years, range: 43–80 years) and 35 were from 15 males (mean age of 56.20 ± 11.65 years, range: 37–79 years). The discs were not classified into age or gender groups. Because there is not a grading system for the anatomical or radiographic identification of degenerative change in TIVDs, an overview of features of the discs (nucleus and annulus) and vertebrae (end-plate and vertebral body) of the thoracic spine was proposed based on previous studies on lumbar discs; macroscopic classification schemas (Nachemson, 1979; Galante, 1967; Thompson et al. 1990; Adams et al. 1996; Wilke et al. 2006) and studies taking into account pathological changes to lumbar discs (Friberg & Hirsch, 1949; Hirsch & Schajowicz, 1953; Vernon-Robert & Pirie, 1977). A set of five morphometric parameters was measured both on lateral radiographs obtained in controlled conditions and directly on sagittal sections of the specimens (Fig. 1). From these measurements, three adimensional morphometric indices were calculated based on previous methods for lumbar discs (Twomey & Taylor, 1987; Amonoo-Kuofi, 1991). The junctional segment C7–T1 was also included for the observation of anatomical variations in the cervicothoracic discs in the transition from mobile cervical to rigid thoracic spine.
Fig. 1.
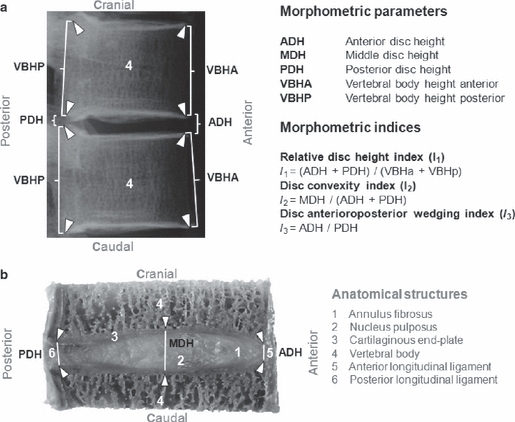
Schematic representation of the parameters and indices that were considered for the morphometric analyses. The anatomical landmarks used are indicated by white arrowheads. (a) In the lateral conventional radiographs of the spinal segments all listed parameters, with the exception of the MDH, were measured. (b) In the sagittal sections of the specimens just the three heights of the intervertebral discs were measured. Images are from a thoracic segment (T9–10) of a 57-year-old female donor. ADH, anterior disc height; MDH, middle disc height; PDH, posterior disc height; VBHA, vertebral body height anterior; VBHP, vertebral body height posterior.
Specimen preparation, radiographic imaging and measurement
The spines were dissected into individual segments free of soft tissues. The ribs were sawn and segments containing the whole disc attached to its upper and lower vertebrae were stored at −28 °C. Lateral and antero-posterior radiographs were taken using a Faxitron automatic X-ray machine (Hewlett Packard, McMinnville, USA). Each segment was placed in a neutral, standard position and a standard film–focus distance of 60 cm, time of 60 s and a tube voltage of 46.5 kV were used. The X-ray beam was centered on the discs. Potential error due to off-center positioning of the spinal segments from the X-ray was examined and a factor for corrections of differences in magnification was calculated. For the radiographic measurements, individual radiographs of the spinal segments were placed on a viewing table and eight anatomical landmarks representing the four corners on the extreme anterior and posterior margins of the end-plates of the vertebrae were marked using Farfan's method (1973) (Fig. 1a). The disc and vertebral heights were measured using an electronic digital caliper (Mitutoyo, Absolute Digimatic, Tokyo, Japan) with an accuracy of ± 0.05 mm. The radiographs were calibrated by means of a scale placed on the rig close to the specimen. Radiographs with overlay from other structures or of deficient film quality were excluded.
Specimen preparation and anatomical measurement
To perform the direct measurements on the discs, frozen spinal segments were sectioned in the horizontal plane through each of the upper and lower vertebral bodies using a high-precision saw (Exacta; PSI Medical, Grünwald, Germany). The posterior elements were removed and segments containing the whole disc attached to a thick portion of the upper and lower vertebral bodies were maintained. Two rods, each 3.0 mm in diameter and 20 mm in length, were fixed into each vertebral body indicating the frontal and median sagittal plane of the TIVD. To produce sagittal sections of the TIVD, each specimen was frozen in an ice block that was individually mounted into a holder with adjustable height for a saw microtome (Leica SP4000; Leica Microsystems, Wetzlar, Germany). The ice blocks were subjected to sagittal sectioning based on the position of the rods. A sliding vernier caliper (Mitutoyo, Absolute Digimatic, Tokyo, Japan) was used for the measurement of TIVD heights, including the cartilaginous end-plates, by using the previously described anatomical landmarks in addition to two mid-vertebral points located on the superior and inferior end-plates for the measurement of the middle disc height (MDH) (Fig. 1b).
Inter- and intra-observer reliability
Each set of radiographic and anatomical measurements was carried out by two observers. Inter-observer errors were examined by repeating the measurement of all parameters in all radiographs and anatomical specimens. Intra-observer errors were examined by one observer making repeated measurements in 10 radiographs from 10 individual specimens at five different spinal levels with some minutes between each repeated measurement. The measurement precision for each parameter was expressed as a coefficient of variation (CV).
Statistical analysis
Linear regression was used to examine the correlation between the radiographic and anatomical measurements of the ADH and PDH, and to calculate the accuracy of the radiographic measurement in relation to the anatomical one. The heights of the discs and the anterior and posterior vertebral bodies (VBHA and VBHP) were individually regressed against the parameters ADH, VBHA and VBHP by a least-square estimation process using a methodology based on Kunkel et al. (2010, 2011). Linear and non-linear regression analyses were employed to find the best functions to fit each of these parameters in a prediction equation. The parameters ADH, VBHA and VBHP were chosen as predictor variables because they could be measured on radiographs with an acceptable accuracy. This was not the case for the MDH and PDH, which were excluded as predictor variables. An anova was performed to define the significance of the prediction equations (P < 0.05) that were evaluated using experimental data of Todd & Pyle (1928).
Results
The grading system proposed to classify the thoracic spinal segments consisted of four grades: (i) no degeneration; (ii) mild degeneration; (iii) moderate degeneration; and (iv) strongly degenerated. The description of the grading scale is as follows. Nucleus: (i) elastic, bright, clear delineation from the annulus; (ii) slightly fibrotic, no clear delineation from the annulus; (iii) fibrous, dry, fissured, discolored, bleeding through cavities, loss of the annulus–nucleus boundary; (iv) fibrous, dry, brownish, brittle, partially replaced by scar tissue. Annulus: (i) concentrically arranged fiber ring plates, regular onion-shaped grain, shiny, sinewy; (ii) sharply contoured, concentrically arranged fiber ring plates (drier appearance); (iii) disordered fibrous structure of the lamellae, fiber faults, fiber fabric ring pronounced dry-looking, sprouting of blood vessels; (iv) ruptures in the annulus, fiber breaks, cracks, fissures, defects. End-plate: (i) well-built hyaline end-plate, even thickness; (ii) hyaline with irregular thickness; (iii) local cartilage defects; (iv) complete destruction of cartilaginous end-plate. Vertebral body: (i) rounded margins; (ii) small projections from the margins; (iii) first osteophytes on the edge < 2 mm; (iv) osteophytes on the anterior vertices > 2 mm. The anatomical and radiographic inspection of the spinal segments selected for this study showed mild to moderate degenerative changes (grades ii and iii).
Inter- and intra-observer reliability of the measurements
Inter-observer reliability showed that measurements of the TIVD heights were better repeated when obtained directly from the specimens (CV = 0.79–0.93) than from the radiographs (CV = 0.49–0.82). A lower repeatability was found for radiographic measurement of the PDH (CV = 0.49). For radiographic measurements of the VBHA and VBHP a high repeatability was found (CV = 0.95–0.98). Intra-observer reliability showed that anatomical measurements were reproduced with errors ranging from 1.7 to 6.1% for ADH, 17 to 26.1% for PDH and 1.7 to 5.1% for VBHA and VBHP. Reproducibility of the measurements from repeat radiographs was generally 15% lower.
Intervertebral discs and vertebral body heights
A wide variation in TIVD heights was found in the anatomical measurements (Table 1). Direct measurement of the ADH varied from approximately 4.5 mm at C7–T1, with a gradual decrease towards T4–5 (approximately 3 mm), increasing again caudally to approximately 7.2 mm at T10–11, and decreasing again to approximately 6 mm at T11–12 (Table 1). PDH measured directly on the specimens followed a trend similar to ADH, but from the disc level T7–8 there was an increase of approximately 21% in the values. The average disc height that corresponded to the average of the ADH and PDH at each vertebral level varied from 3.2 to 6.5 mm (mean value of 4.3 ± 1 mm; Table 1). The average vertebral body height varied from 14.2 to 21.96 mm (Table 2). The MDH was on average 22.7% higher than the average disc height (Tables 1 and 3). Radiographic ADH and PDH values were shorter than the anatomical ones (approximately 9% for ADH and 37% for PDH). From these comparisons, a height linear correlation was found for ADH (R2 = 0.921) (Fig. 2a), but only a moderate correlation for PDH (R2 = 0.690) (Fig. 2b).
Table 1.
Anatomical and radiographic measurements of the anterior, middle and posterior human TIVD heights
| Anterior disc height (ADH) | Posterior disc height (PDH) | Middle disc height (MDH)* | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anatomical measurement | Radiographic measurement | Anatomical–radiographic ratio | Anatomical measurement | Radiographic measurement | Anatomical-Radiographic ratio | Anatomical measurement | |||||||||
| Disc level | Mean | SD | Mean | SD | Difference | % | Mean | SD | Mean | SD | Difference | % | Mean | SD | Average disc height ** |
| C7–T1 | 4.5 | 0.79 | 3.96 | 0.22 | 0.54 | −11.90 | 4.5 | 0.51 | 3.20 | 0.55 | 1.30 | −28.91 | 5.6 | 0.63 | 4.5 |
| T1–2 | 4.5 | 0.77 | 3.69 | 0.62 | 0.81 | −18.01 | 4.3 | 0.62 | 3.04 | 0.56 | 1.26 | −29.40 | 5.7 | 0.66 | 4.4 |
| T2–3 | 3.4 | 0.97 | 3.23 | 0.40 | 0.17 | −4.89 | 3.5 | 0.99 | 1.95 | 0.28 | 1.55 | −44.22 | 5.8 | 0.79 | 3.5 |
| T3–4 | 3.3 | 0.30 | 3.07 | 0.44 | 0.23 | −6.96 | 3.2 | 0.49 | 2.09 | 0.46 | 1.11 | −34.69 | 4.4 | 0.8 | 3.3 |
| T4–5 | 3.0 | 0.74 | 2.85 | 0.36 | 0.15 | −5.11 | 3.3 | 0.45 | 2.00 | 0.21 | 1.30 | −39.54 | 5.0 | 0.61 | 3.2 |
| T5–6 | 3.5 | 0.37 | 3.36 | 0.29 | 0.14 | −3.93 | 3.6 | 0.47 | 2.10 | 0.30 | 1.50 | −41.71 | 4.7 | 0.91 | 3.5 |
| T6–7 | 4.1 | 0.35 | 3.70 | 0.41 | 0.40 | −9.80 | 4.1 | 0.65 | 2.18 | 0.50 | 1.92 | −46.72 | 5.5 | 0.45 | 4.1 |
| T7–8 | 4.2 | 0.97 | 4.06 | 0.67 | 0.14 | −3.35 | 3.6 | 0.90 | 2.47 | 0.50 | 1.13 | −31.44 | 5.3 | 0.58 | 3.9 |
| T8–9 | 5.6 | 1.17 | 4.52 | 0.43 | 1.08 | −19.22 | 5.0 | 0.91 | 2.49 | 0.60 | 2.51 | −50.12 | 6.1 | 0.89 | 5.3 |
| T9–10 | 5.4 | 1.74 | 4.88 | 1.03 | 0.52 | −9.70 | 4.2 | 1.10 | 2.97 | 0.60 | 1.23 | −29.36 | 5.5 | 0.90 | 4.8 |
| T10–11 | 7.2 | 1.21 | 5.91 | 0.77 | 1.29 | −17.94 | 5.8 | 1.00 | 3.66 | 0.70 | 2.14 | −36.83 | 6.7 | 1.18 | 6.5 |
| T11–12 | 6.0 | 1.14 | 5.90 | 0.70 | 0.10 | −1.67 | 4.8 | 1.26 | 3.23 | 0.48 | 1.57 | −32.63 | 6.5 | 1.15 | 5.4 |
Refer to Fig. 1 for abbreviations.
All measurements are in mm.
No radiographic measurement was performed for the MDH.
Average disc height is the average of the anatomical measurement of the ADH and PDH at each vertebral level. o e digital.
Table 2.
Anterior and posterior human thoracic vertebral body heights
| Vertebral body height anterior (VBHA) | Vertebral body height posterior (VBHP) | ||||
|---|---|---|---|---|---|
| Vertebral level | Mean | SD | Mean | SD | Average vertebral body height* |
| C7 | 13.89 | 1.42 | 14.38 | 2.22 | 14.14 |
| T1 | 14.49 | 1.23 | 15.28 | 1.14 | 14.88 |
| T2 | 15.01 | 1.51 | 16.11 | 1.67 | 15.56 |
| T3 | 15.65 | 1.85 | 17.41 | 1.12 | 16.53 |
| T4 | 15.42 | 1.46 | 18.15 | 1.54 | 16.79 |
| T5 | 15.84 | 1.07 | 17.33 | 2.16 | 16.59 |
| T6 | 16.04 | 1.43 | 18.22 | 1.38 | 17.13 |
| T7 | 15.94 | 1.61 | 18.67 | 1.64 | 17.31 |
| T8 | 16.99 | 1.70 | 20.05 | 1.77 | 18.52 |
| T9 | 18.26 | 2.12 | 20.25 | 2.44 | 19.26 |
| T10 | 18.98 | 1.40 | 20.35 | 1.89 | 19.67 |
| T11 | 19.60 | 1.92 | 22.67 | 1.38 | 21.14 |
| T12 | 20.80 | 1.96 | 23.12 | 1.94 | 21.96 |
Refer to Fig. 1 for abbreviations.
All measurements are in mm.
Average vertebral body height is the average of the VBHA and VBHP at each vertebral level.
Table 3.
Morphometric indices derived from measurements on the intervertebral discs and vertebral bodies heights
| Disc level | Relative disc height index (I1) | Disc : vertebral body height ratio | Disc convexity index (I2) | % MDH to average disc height | Disc antero-posterior wedging index (I3) |
|---|---|---|---|---|---|
| C7–T1 | 0.32 | 1:3.1 | 0.63 | 20.55 | 1.00 |
| T1–2 | 0.30 | 1:3.4 | 0.65 | 23.11 | 1.06 |
| T2–3 | 0.22 | 1:4.5 | 0.83 | 39.65 | 0.97 |
| T3–4 | 0.20 | 1:5.1 | 0.67 | 25.17 | 1.03 |
| T4–5 | 0.19 | 1:5.3 | 0.80 | 37.50 | 0.89 |
| T5–6 | 0.21 | 1:4.7 | 0.67 | 25.58 | 0.97 |
| T6–7 | 0.24 | 1:4.2 | 0.68 | 25.95 | 1.01 |
| T7–8 | 0.23 | 1:4.4 | 0.68 | 26.75 | 1.16 |
| T8–9 | 0.29 | 1:3.5 | 0.57 | 12.56 | 1.13 |
| T9–10 | 0.25 | 1:4.0 | 0.58 | 13.74 | 1.29 |
| T10–11 | 0.33 | 1:3.0 | 0.52 | 3.50 | 1.23 |
| T11–12 | 0.26 | 1:3.9 | 0.60 | 16.77 | 1.25 |
Refer to Fig. 1 for abbreviations.
I1 = (ADH + PDH)/(VBHA + VBHP) based on Amonoo-Kuofi (1991).
I2 = MDH/(ADH + PDH) based on Twomey & Taylor (1987).
I3 = ADH/PDH.
The ratio of disc: body was calculated by dividing 1 by the value of I1.
Fig. 2.
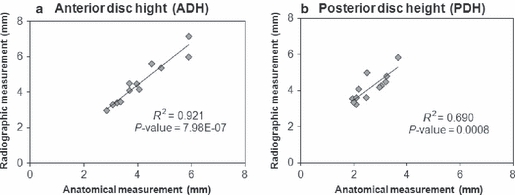
Correlations between anatomical and radiographic measurements of the anterior (a) and posterior (b) disc heights considering mean values from each disc level from C7–T1 to T11–12. See Table 1 for data summaries. ADH, anterior disc height; PDH, posterior disc height.
Morphometric indices
The index I1 enabled a comparison of the TIVD height with the heights of neighboring vertebral bodies (Table 3). There was a constant relationship between the disc thickness and the vertebral bodies’ heights at all levels (ratio disc : body of approximately 1 : 4.1) (Fig. 3). The index I2 indicated that the ovality of the disc did not follow a trend as one descends the thoracic spine. It was more pronounced at the T2–3 level where MDH was almost 40% of the average disc height (Table 3; Fig. 3). The index I3 showed that with the exception of the cervicothoracic discs (C7–T1) all discs were wedge-shaped. There was a trend for a posterior wedge configuration from the T7–8 level onwards, the ADH being approximately 21.25% greater than the PDH. However, in the upper and middle thoracic region (from T1–2 to T6–7) both anteriorly and posteriorly minimal wedge shapes were found with a maximum difference between these values of approximately 2.77%. From these morphometric indices, the TIVD could be classified into three distinct regions as an approximation of the vertebral regions of the thoracic spine (Panjabi et al. 1991a; Fig. 3). The upper region of transition from cervical to thoracic from C7–T1 to T3–4 was characterized by a gradual decrease caudally of the ADH and PDH until the thinnest disc at T4–5, with a sliding posterior wending. The middle region from T4–5 to T6–7 showed sliding anterior wedge-shaped discs, and the lower region from the apex of the thoracic spine T7–8 to T11–12 contained more posterior wedge-shaped discs. Comparisons with the literature were provided for measurements of the disc heights (Fig. 4) and vertebral bodies heights (Fig. 5).
Fig. 3.
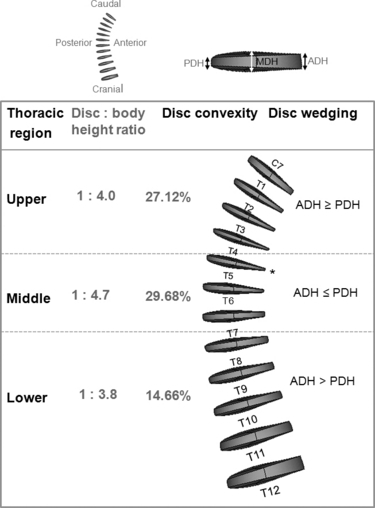
Geometric model of the human thoracic discs from C7–T1 to T11–12 disc level, constructed with parameters derived from the morphometric analyses performed in this study. The thinnest disc was found in the disc level T4–5*. The shape of the human TIVDs was determined by the relationships between the anterior, middle and posterior disc heights (ADH, MDH, PDH).
Fig. 4.
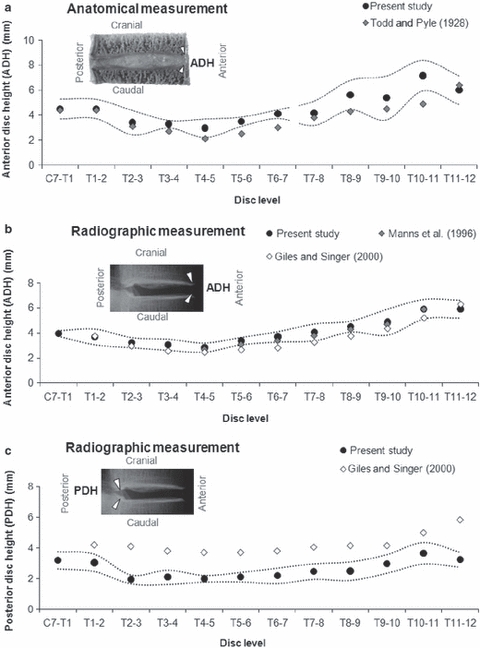
Comparison of the anterior and posterior heights of the human intervertebral discs obtained in the present study with published data. Mean values of anatomical (ADH; a) and radiographic (ADH and PDH; b,c) measurements. Dotted curves indicate SD of the experimental values of the present study. ADH, anterior disc height; PDH, posterior disc height.
Fig. 5.
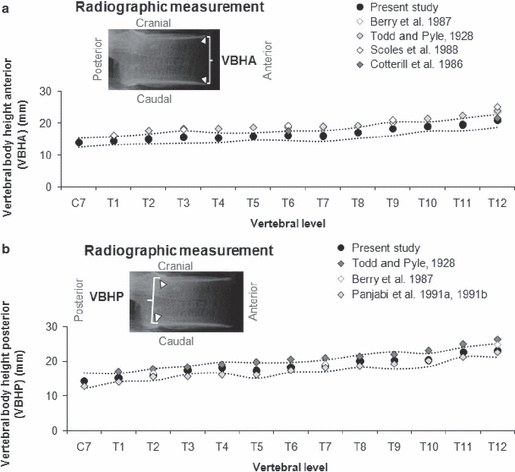
Comparison of the anterior (a) and posterior (b) heights of the human vertebral bodies obtained in the present study with published data. Means values of radiographic measurements. Dotted curves indicate SD of the experimental values of the present study. VBHA, vertebral body height anterior; VBHP, vertebral body height posterior.
Disc and vertebral body height correlations
In general, the heights of the TIVDs presented had good correlations with the vertebral heights, that were significant (R2 = 0.659–0.835, P < 0.005; anova) (Table 4). An exception was the MDH, for which no significant correlations with the vertebral body heights were found (R2 < 0.6, P> 0.05). A set of 10 polynomial equations was generated for the prediction of TIVD heights from parameters that could be accurately measured on the radiographs (ADH, VBHA and VBHP; Table 4). The polynomial predictions, using the generated set of regression equations, were generally within or close to the region of the 95% confidence intervals of the experimental data measured in the current study (Fig. 6). The evaluation of the predictability of the regression equations using VBHA and VBHP of the data set of the radiographic measurements of the current study showed that good results could be found (Figs 7 and 8). Using the data set of Todd & Pyle (1928), a comparison of predicted PDH from radiographic ADH showed a greatest error of approximately −13% in the upper and −17% in the lower regions of the thoracic spine (Fig. 9a). The predictions of the VBHA and VBHP exhibited a mean percent error < 17% (Fig. 9b,c).
Table 4.
Polynomial coefficients (C1, C2, C3 and C4) for prediction equations of the parameters related to the heights of the TIVD and vertebral bodies for all spinal levels from C7–T1 to T11–12. The vertebral parameters come from radiographic measurements, whereas the disc parameters are from anatomical measurements performed in the current study
| Predictor parameter | Predicted parameter | R2 | P-value | SE | C1 | C2 | C3 | C4 |
|---|---|---|---|---|---|---|---|---|
| ADH | MDH | 0.726 | 0.0004 | 0.37 | 3.500 | 0.453 | – | – |
| PDH | 0.906 | 0.0002 | 0.27 | −2.149 | 3.067 | −0.538 | 0.037 | |
| VBHA | ADH | 0.835 | 0.0017 | 0.60 | 544.560 | −97.473 | 5.795 | −0.113 |
| MDH | 0.576 | 0.0640 | – | – | – | – | – | |
| PDH | 0.667 | 0.0260 | 0.52 | 360.580 | −63.935 | 3.783 | −0.074 | |
| VBHP | 0.953 | 2.7E-06 | 0.66 | −180.00 | 31.073 | −1.646 | 0.030 | |
| VBHP | ADH | 0.780 | 0.0053 | 0.66 | 298.43 | −46.993 | 2.561 | −0.045 |
| MDH | 0.571 | 0.0676 | – | – | – | – | – | |
| PDH | 0.659 | 0.0282 | 0.53 | 201.190 | −32.029 | 1.705 | −0.030 | |
| VBHA | 0.943 | 6.5E-06 | 0.58 | 44.199 | −5.305 | 0.286 | −0.004 |
Refer to Fig. 1 for abbreviations.
SE in mm.
The basic form of the prediction equations is y = C1 + C2x + C3x2 + C4x3 where y is the value of the parameter to be predicted and x is the value of the predictor parameter on each spinal level.
Fig. 6.
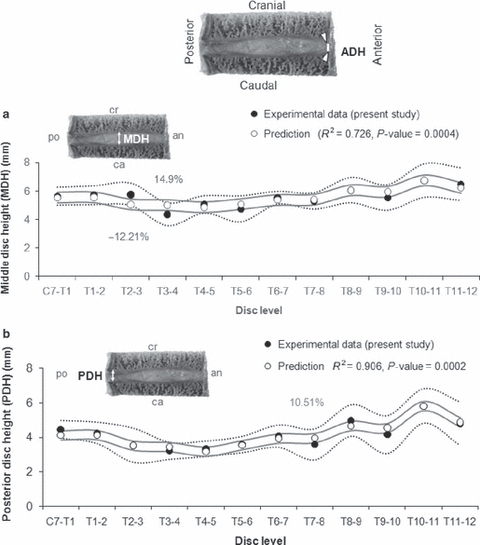
Anatomical values of the ADH were used for predictions of the parameters MDH (a) and PDH (b) at all levels of the thoracic spine. The predicted values were superimposed on experimental data that were measured in the present study. Dotted and continuous curves indicate SD of the experimental and predicted values, respectively. Mean percent errors of the predictions larger than 10% are indicated. ADH, anterior disc height; an, anterior; ca, caudal; cr, cranial; MDH, middle disc height; PDH, posterior disc height; po, posterior.
Fig. 7.
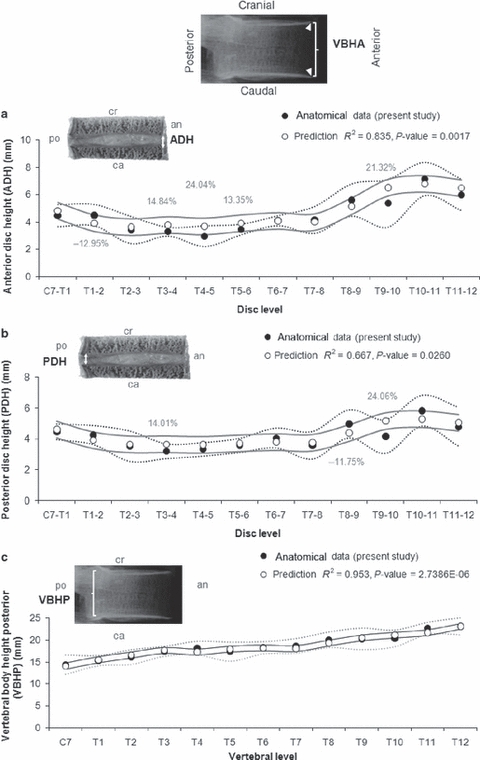
Radiographic values of the VBHA were used for predictions of the parameters ADH (a), PDH (b) and VBHP (c) at all levels of the thoracic spine. The predicted values were superimposed on anatomical data that were measured in the present study. Dotted and continuous curves indicate SD of the experimental and predicted values, respectively. Mean percent errors of the predictions larger than 10% are indicated. ADH, anterior disc height; an, anterior; ca, caudal; cr, cranial; PDH, posterior disc height; po, posterior; VBHA, vertebral body height anterior; VBHP, vertebral body height posterior.
Fig. 8.
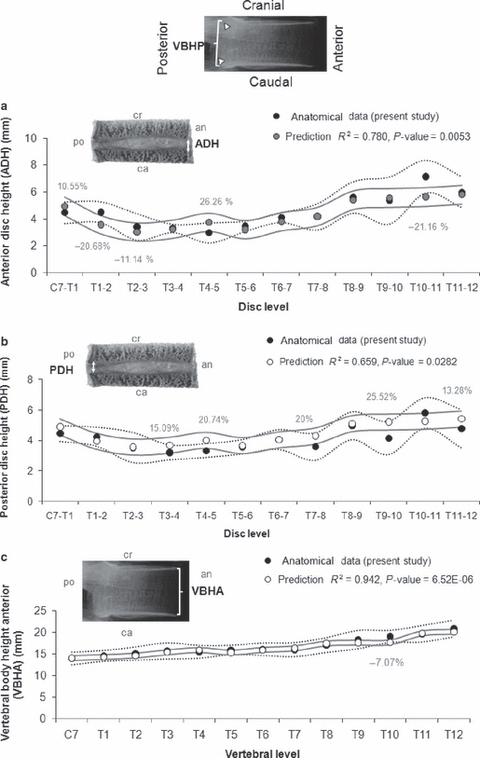
Radiographic values of the VBHP were used for polynomial predictions of the parameters ADH (a), PDH (b) and VBHA (c) at all levels of the thoracic spine. The predicted values were superimposed on anatomical data that were measured in the present study. Dotted and continuous curves indicate SD of the experimental and predicted values, respectively. Mean percent errors of the predictions larger than 10% are indicated. ADH, anterior disc height; an, anterior; ca, caudal; cr, cranial; PDH, posterior disc height; po, posterior; VBHA, vertebral body height anterior; VBHP, vertebral body height posterior.
Fig. 9.

Comparison of some predicted parameters (PDH, VBHP and VBHA) from anatomical measurements of Todd & Pyle (1928) with corresponding radiographic measurements of the current study. The predicted values were superimposed on experimental data. Dotted and continuous curves indicate SD of the experimental and predicted values, respectively. Mean percent errors of the predictions larger than 10% are indicated. ADH, anterior disc height; PDH, posterior disc height; VBHA, vertebral body height anterior; VBHP, vertebral body height posterior.
Discussion
In the present study, the heights of human TIVDs from the C7–T1 to T11–12 spinal level were measured directly on the sagittal section of 72 specimens and on their radiographs. The main aim was to provide these anatomical data and estimate the error of the radiographic measurements. Additionally, heights of the neighboring vertebral bodies were measured for the investigation of predictions of TIVD dimensions based on the size of the vertebral bodies.
Disc height is an important dimension often used as a diagnostic tool in orthopedics as well as in mathematical modeling of the human spine. Although Oliver & Middleditch (1991) reported that TIVDs have a nearly uniform thickness, our anatomical observations indicated that there is no single exact disc height because the planes that bound the TIVD superiorly and inferiorly were not parallel (Fig. 1). A geometric model of the thoracic discs based on these parameters provides a better visualization of this variation, which occurs in different parts of the same disc as well as in different regions of the thoracic spine (Fig. 3). However, this may be due to the age of the subjects (Vernon-Robert & Pirie, 1977; Twomey & Taylor, 1987) or to other factors such as loss of disc height in cases of scoliosis or disc herniation. Possible sources of error in these measurements could also be due to post mortem changes or the degree of disc degeneration (Peacock, 1952; Walmsley, 1953; White & Panjabi, 1990; Goh et al. 2000).
In the current study, the two main sources of ambiguity found in radiographic measurements of disc heights (the disc orientation with respect to the central X-ray beam, and the estimation of differences among different observers) were minimized using the recommendations of Pope et al. (1977) and Andersson et al. (1981). The difficulty in identifying the bony landmarks was overcome by strictly controlling the vertebral position, preserving the relationships between the TIVD and the vertebral bodies. However, even when the specimens were radiographed under these controlled and standard conditions the same degree of accuracy that was seen for the anatomical measurement was still not achieved (Table 1; Fig. 2). This was due to the difficulty in the identification of the vertebral bony landmarks, particularly where many overlapping shadows were found, for example in the measurements of the PDH at the upper thoracic spine. It was not possible to compare radiographic and anatomical measurement of the MDH because the midline distance between the oval radiographic images of the proximal and distal vertebral end-plates could not be identified (Edmondston et al. 1999). Our radiographic ADH and PDH values were shorter than the anatomical ones, probably because the anatomical measurements included the cartilaginous end-plates that cannot be readily indentified on radiographs.
Comparison of our direct and radiographic measurements with other studies on TIVD was difficult due to the fact that there are few comparative data in the literature (e.g. no published data related to MDH were found). For ADH, a good agreement was found with anatomical values of Todd & Pyle (1928; Fig. 4a) and radiographic values of Manns et al. (1986) and Giles & Singer (2000) (Fig. 4b); although the same was not found for the radiographic PDH values compared with Giles & Singer (2000) (Fig. 4c). The small variations between the radiographic measurements could be due to radiographic magnification bias, positioning errors and distortion due to parallax effects.
As expected, the radiographic measurements of the thoracic vertebral bodies heights showed very good agreement with other studies where these values have already been well established (Todd & Pyle, 1928; Cotterill et al. 1986; Berry et al. 1987; Scoles et al. 1988; Panjabi et al. 1991a,b;) (Fig. 5). However, the cartilaginous end-plates were not considered for this measurement, and this could slightly interfere in this measurement. Although this was not a major goal of our study, accurate measurements of these parameters were necessary so that we could perform analysis of the correlations with the measurements of disc height. The morphometric indices for TIVD showed a ratio of disc to vertebral body height of approximately 1 : 4.1, with a progressive increase in the spine motion in the sagittal plane in the lower region (1 : 3.8) where the disc height was greater and the thoracic segments were less impeded by the constraint of the thoracic cage. This agrees with Kapandji (1985) and White & Panjabi (1990) who reported the thoracic region as the least mobile of the spine.
Due to the fact that TIVD heights provided in this study were obtained from in vitro measurements of isolated spine segments of cadavers, the axial load applied to the thoracic spine due to bodyweight could not be considered. Therefore, the measured values in the current study should be slightly larger than the radiographic values of a living person in a sitting or standing position. This could be an important point from both arthroplasty and modeling standpoints.
Using the set of prediction equations generated in this study it was possible to estimate heights of the thoracic discs from initial radiographic measurement of the vertebral heights (Figs 6–8). ADH could be predicted, with a largest error of approximately 26%, from measurements of the VBHA or VBHP. MDH could only be measured with statistical significance from the ADH measurements (largest error of approximately 15%). For estimation of PDH, both ADH and vertebral heights provided good predictions. From the measurement of the vertebral height were predicted values of PDH with approximately 26% error, which was less than the radiographic measurement of this parameter in all thoracic levels (Table 1; Figs 7 and 8). The values of VBHA and VBHP allowed very good predictions with errors of less than 10%. The generated equations are thus valid under these limited circumstances. It is also important to point out that the errors caused by the measurement of radiographic vertebral bodies may lead to errors in predicting the height of the disc. Moreover, further investigations are necessary to evaluate the predictability of the regression equations with a data set from patients.
This study provided an accurate and comprehensive data base to describe the geometry of the TIVD. This may serve as an anthropometric reference for mathematical modeling, as well as for anatomical and biomechanical studies of the human spine, where dimensions and relations of spinal bony segments in the mid-sagittal plane are of importance.
Conclusion
The current increased interest in spinal implants and biomechanical models of spinal deformation, including scoliosis, calls for a detailed knowledge of its anatomy and of relationships between the disc and the vertebrae. The present study contributes by providing new anatomical data on thoracic disc morphometry, particularly the disc heights and their relationships with thoracic vertebral body heights. These data are important for understanding the biomechanics and morphology of the spine. The generated set of prediction equations quantitatively describe these relationships and could be used to produce morphometric data on thoracic disc. For the creation of parameterized models of the human thoracic discs, the use of the prediction equations could eliminate the need for direct measurement on intervertebral discs. Moreover, the error produced by radiographic measurements could be reduced at least for the PDH.
Acknowledgments
This study was financially supported by the German Research Foundation (Wi-1352/12-1).
Conflict of interest statement
Each author of this study did not and will not receive benefits in any form from a commercial party related directly or indirectly to the content of this study.
References
- Adams MA, McNally DS, Dolan P. Stress distributions inside intervertebral discs. The effects of age and degeneration. J Bone Joint Surg Br. 1996;78:965–972. doi: 10.1302/0301-620x78b6.1287. [DOI] [PubMed] [Google Scholar]
- Amonoo-Kuofi HS. Morphometric changes in the heights and anteroposterior diameters of the lumbar intervertebral disc with age. J Anat. 1991;175:159–168. [PMC free article] [PubMed] [Google Scholar]
- Andersson GBJ, Schultz A, Nathan A, et al. Roentgenographic measurement of lumbar intervertebral disc height. Spine. 1981;6:154–157. doi: 10.1097/00007632-198103000-00008. [DOI] [PubMed] [Google Scholar]
- Berry JL, Moran JM, Berg WS, et al. A morphometric study of human lumbar and selected thoracic vertebrae. Spine. 1987;12:362–367. doi: 10.1097/00007632-198705000-00010. [DOI] [PubMed] [Google Scholar]
- Breglia DP. Generation of a 3-D parametric solid model of the human spine using anthropomorphic parameters. Ohio: Ohio University; 2006. Master dissertation. [Google Scholar]
- Cotterill PC, Kostuik JP, D'Angelo GD, et al. An anatomical comparison of the human and bovine thoracolumbar spine. J Orthop Res. 1986;4:298–303. doi: 10.1002/jor.1100040306. [DOI] [PubMed] [Google Scholar]
- Edmondston SJ, Price RI, Valente B, et al. Measurement of vertebral body heights: ex vivo comparisons between morphometric X-ray absorptiometry, morphometric radiography and direct measurements. Osteoporos Int. 1999;10:7–13. doi: 10.1007/s001980050187. [DOI] [PubMed] [Google Scholar]
- Farfan HF. Mechanical disorders of the low back. Philadelphia: Lea and Febiger; 1973. [Google Scholar]
- Friberg S, Hirsch C. Anatomical and clinical studies on lumbar disc degeneration. Acta Orthop Scand. 1949;19:222–242. doi: 10.3109/17453674908991095. [DOI] [PubMed] [Google Scholar]
- Galante JO. Tensile properties of the human lumbar annulus fibrosus. Acta Orthop Scand (Suppl) 1967;100:1–91. doi: 10.3109/ort.1967.38.suppl-100.01. [DOI] [PubMed] [Google Scholar]
- Giles LGF, Singer KP. Clinical anatomy and management of thoracic spine pain. Oxford: Butterworth-Heinemann; 2000. pp. 25–27. [Google Scholar]
- Goh S, Price RI, Leedman PJ, et al. The relative influence of vertebral body and intervertebral disc shape on thoracic kyphosis. Clin Biomech. 1999;14:439–448. doi: 10.1016/s0268-0033(98)00105-3. [DOI] [PubMed] [Google Scholar]
- Goh S, Tan C, Price SRI, et al. Influence of age and gender on thoracic vertebral body shape and disc degeneration: an MR investigation of 169 cases. J Anat. 2000;197:647–657. doi: 10.1046/j.1469-7580.2000.19740647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch MD, Schajowicz MD. Studies on structural changes in the lumbar annulus fibrosus. Acta Orthop Scand. 1953;22:184–231. doi: 10.3109/17453675208989006. [DOI] [PubMed] [Google Scholar]
- van der Houwen EB, Baron PH, Veldhuizen AG, et al. Geometry of the intervertebral volume and vertebral endplates of the human spine. Ann Biomed Eng. 2010;38:33–40. doi: 10.1007/s10439-009-9827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurxthal LM. Measurement of anterior vertebral compressions and biconcave vertebrae. Am J Roentgenol Rad Ther Nucl Med. 1968;103:635–644. doi: 10.2214/ajr.103.3.635. [DOI] [PubMed] [Google Scholar]
- Kapandji IA. Rumpf und Wirbelsäule. Stuttgart: Ferdinand Enke; 1985. [Google Scholar]
- Kunkel ME, Schmidt H, Wilke HJ. Prediction equations for human thoracic and lumbar vertebral morphometry. J Anat. 2010;216:320–328. doi: 10.1111/j.1469-7580.2009.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunkel ME, Schmidt H, Wilke HJ. Prediction of the human thoracic and lumbar articular facet joint morphometry from radiographic images. J Anat. 2011;218:191–201. doi: 10.1111/j.1469-7580.2010.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laporte S, Mitton D, Ismael B, et al. Quantitative morphometric study of thoracic spine. A preliminary parameters statistical analysis. Eur J Orthop Surg Traumatol. 2000;10:85–91. [Google Scholar]
- Lavaste F, Skalli W, Robin S, et al. Three-dimensional geometrical and mechanical modelling of the lumbar spine. J Biomech. 1992;25:1153–1164. doi: 10.1016/0021-9290(92)90071-8. [DOI] [PubMed] [Google Scholar]
- Lord MJ, Ogden JA, Ganey TM. Postnatal development of the thoracic spine. Spine. 1995;20:1692–1698. doi: 10.1097/00007632-199508000-00008. [DOI] [PubMed] [Google Scholar]
- Manns RA, Haddaway MJ, McCall IW, et al. The relative contribution of disc and vertebral morphometry to the angle of kyphosis in asymptomatic subjects. Clin Radiol. 1986;51:258–262. doi: 10.1016/s0009-9260(96)80342-4. [DOI] [PubMed] [Google Scholar]
- Nachemson AL, Schultz AB, Berkson MH. Mechanical properties of human lumbar spine motion segments. Influence of age, sex, disc level and degeneration. Spine. 1979;4:1–8. doi: 10.1097/00007632-197901000-00001. [DOI] [PubMed] [Google Scholar]
- Oliver J, Middleditch A. Functional anatomy of the spine. Oxford: Butterworth-Heinenmann; 1991. pp. 23–24. [Google Scholar]
- Panjabi MM, Takata K, Goel V, et al. Thoracic human vertebrae – quantitative three-dimensional anatomy. Spine. 1991a;16:888–901. doi: 10.1097/00007632-199108000-00006. [DOI] [PubMed] [Google Scholar]
- Panjabi MM, Duranceau J, Goel V, et al. Cervical human vertebrae quantitative three-dimensional anatomy of the middle and lower regions. Spine. 1991b;16:861–869. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- Peacock A. Observations on the postnatal structure of the intervertebral disc in man. J Anat. 1952;86:162–179. [PMC free article] [PubMed] [Google Scholar]
- Pooni JS, Hukins DWL, Harris PF, et al. Comparison of the structure of human intervertebral discs in the cervical, thoracic and lumbar regions of the spine. Surg Radiol Anat. 1986;8:175–182. doi: 10.1007/BF02427846. [DOI] [PubMed] [Google Scholar]
- Pope MH, Hanley EN, Matteri RE, et al. Measurement of intervertebral disc space height. Spine. 1977;2:282–286. [Google Scholar]
- Scoles PV, Linton AE, Buce L, et al. Vertebral body and posterior element morphology: the normal spine in middle life. Spine. 1988;13:1082–1086. doi: 10.1097/00007632-198810000-00002. [DOI] [PubMed] [Google Scholar]
- Thompson JP, Pearce RH, Schechter MT, et al. Preliminary evaluation of a scheme for grading the gross morphology of the human intervertebral disc. Spine. 1990;15:411–415. doi: 10.1097/00007632-199005000-00012. [DOI] [PubMed] [Google Scholar]
- Todd TW, Pyle SI. A quantitative study of the vertebral column by direct and roentgenoscopic methods. Am J Phys Anthropol. 1928;XII:321–338. [Google Scholar]
- Twomey L, Taylor JR. Degenerative age changes in lumbar vertebrae and intervertebral discs. Clin Orthop. 1987;224:97–104. [PubMed] [Google Scholar]
- Vernon-Robert B, Pirie CJ. Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae. Rheumatol Rehab. 1977;16:13–21. doi: 10.1093/rheumatology/16.1.13. [DOI] [PubMed] [Google Scholar]
- Walmsley R. The development and growth of the intervertebral disc. Edinb Med J. 1953;60:341–364. [PMC free article] [PubMed] [Google Scholar]
- White AA, Panjabi MM. Clinical Biomechanics of the Spine. Philadelphia: J. B. Lippincott; 1990. [Google Scholar]
- Wilke HJ, Rohlmann F, Neidlinger-Wilke C, et al. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: part I. Lumbar spine. Eur Spine J. 2006;15:720–730. doi: 10.1007/s00586-005-1029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


