Summary
CD8α+ dendritic cells (DCs) are important in vivo for cross-presentation of antigens derived from intracellular pathogens and tumors. Additionally, secretion of interleukin-12 (IL-12) by CD8α+ DCs suggests a role for these cells in response to Toxoplasma gondii antigens, although it remains unclear whether these cells are required for protection against T. gondii infection. Towards this goal, we examined T. gondii infection of Batf3−/− mice, which selectively lack only lymphoid-resident CD8α+ DCs and related peripheral CD103+ DCs. Batf3−/− mice were extremely susceptible to T. gondii infection, with decreased production of IL-12 and interferon-γ. IL-12 administration restored resistance in Batf3−/− mice, and mice in which IL-12 production was ablated only from CD8α+ DCs failed to control infection. These results reveal that the function of CD8α+ DCs extends beyond a role in cross-presentation and includes a critical role for activation of innate immunity through IL-12 production during T. gondii infection.
Introduction
Although cell-mediated immunity is critical for defense against the intracellular pathogen Toxoplasma gondii, the precise cells responsible for initiating the protective innate and adaptive responses have been difficult to identify. Toxoplasma gondii is an intracellular protozoan parasite whose elimination requires production of interferon-γ (IFNγ) that activates various cell-intrinsic anti-parasitic defense pathways within infected cells (Yap et al., 2006). The production of IFNγ in T. gondii infection is dependent on interleukin-12 (IL-12) (Gazzinelli et al., 1993), and while a number of studies have identified cells capable of producing IL-12 in response to T. gondii, none has unambiguously identified the cellular source of IL-12 in T. gondii infection relevant to protection in vivo. Several different cells have been proposed to be important sources of IL-12 during T. gondii infection, including neutrophils (Bliss et al., 1999; Bliss et al., 2000), macrophages (Gazzinelli et al., 1994; Robben et al., 2004), plasmacytoid dendritic cells (pDCs) (Pepper et al., 2008), conventional dendritic cells (cDCs) (Liu et al., 2006), and the subset of conventional dendritic cells expressing CD8α (Reis e Sousa et al., 1997).
Neutrophils have been reported to produce IL-12 in vitro in response to T. gondii antigens, but it is unlikely that they are required for protective immunity to T. gondi in vivo. Neutrophils are rapidly recruited to the peritoneum after infection with high doses of virulent strains of T. gondii, where they co-stain for IL-12 by microscopy (Bliss et al., 1999; Bliss et al., 2000). However, influx of neutrophils is not observed following oral infection with low virulence isolates, mimicking natural routes of infection (Dunay et al., 2008). Initial in vivo studies in which neutrophils were depleted using the Ly6C-specific antibody RB6-8C5 suggested a crucial function for neutrophils in protective immunity against T. gondii (Sayles and Johnson, 1996; Bliss et al., 2001; Scharton-Kersten et al., 1997b). However, inflammatory monocytes expressing the same marker Ly6C were later identified (Mordue and Sibley, 2003; Serbina and Pamer, 2006), and all studies conducted with RB6-8C5 were confounded by dual elimination of both neutrophils and inflammatory monocytes. In a more recent study, Dunay et al. depleted only neutrophils in vivo using the Ly-6G specific monoclonal antibody 1A8, and demonstrated that specific ablation of neutrophils does not increase the susceptibility of mice to T. gondii infection or alter serum concentrations of IL-12 (Dunay et al., 2010). These recent data argue that neutrophils are less likely to be a critical in vivo source of IL-12 that is relevant to protection during T. gondii infection.
Several cells other than neutrophils are viable candidates as an important source of IL-12 in providing protective immunity to T. gondii, including monocytes and macrophages. Gazzinelli et al. first demonstrated that thioglycolate elicited peritoneal macrophages produce IL-12 in response to in vitro stimulation with soluble tachyzoite antigen (STAg) (Gazzinelli et al., 1994). In addition, IL-12 mRNA could be detected in peritoneal exudate cells (PECs) of mice infected with T. gondii, although individual cell types from the exudate were not distinguished in this study. Low density splenocytes as well as bone marrow-derived macrophages (BMMs) were also capable of producing IL-12 in response to in vitro T. gondii infection (Robben et al., 2004). These studies demonstrate that activated or in vitro derived macrophages can produce IL-12, but do not demonstrate an in vivo function for these cells. In a model of oral infection, Gr1+ inflammatory monocytes that are recruited to the intestine express IL-12 in vivo (Dunay et al., 2008), although a functional requirement for IL-12 production by these cells was not demonstrated. pDCs can also produce IL-12 in response to in vitro infection by T. gondii (Pepper et al., 2008), although in this study, only in vitro generated bone-marrow derived pDCs were examined, and an in vivo requirement for pDCs during T. gondii infection was not tested. Thus, while various monocyte, macrophage, and pDC populations can produce IL-12 in response to T. gondii, their importance as a source of IL-12 for in vivo protection against T. gondii infection has not been demonstrated and remains uncertain.
Several studies suggested that conventional DCs were important as a source of IL-12 in T. gondii infection, but neither excludes macrophages nor identifies the type of DC that might be responsible for protection. One study used a lineage ablation approach in which the Diphtheria toxin receptor (DTR) was expressed under control of the Itgax gene promoter (encoding CD11c, referred to as CD11c-DTR mice), in order to ask whether DCs were involved in protection against infection by T. gondii (Liu et al., 2006). Diphtheria toxin (DT) administration in these mice caused the depletion of CD11c-expressing cells and greatly increased susceptibility to T. gondii infection. Enhanced susceptibility was attributed to the depletion of IL-12-producing DCs, but could also result from loss of macrophages because CD11c-DTR also depletes several subsets of splenic macrophages (Probst et al., 2005). Although transfer of wild-type DCs, but not IL-12-deficient DCs, did rescue susceptibility in DT-treated mice, this rescue does not exclude macrophages as the cell that normally provides protection againt T. gondii infection in vivo. A recent study used selective expression of Cre recombinase in CD11c-expressing (Itgax-Cre) or Lysozyme M-expressing (Lyz2-Cre) cells in an attempt to exclusively delete the toll-like receptor (TLR) adaptor protein MyD88 from DCs and macrophages, respectively (Hou et al., 2011). Deletion of Myd88 by CD11c-Cre was sufficient to decrease early IL-12 production during T. gondii infection and led to increased susceptibility, suggesting that IL-12 production by a CD11c-expressing cell was critical for resistance to T. gondii infection. However, as with the study by Liu et al. above, CD11c is expressed by certain macrophage populations, making it difficult to discern unambiguously which cell is protective in vivo.
A few studies have addressed the potential function of the CD8α+ DC subset in resistance to T. gondii. Studies of Irf8-deficient mice have suggested a role for the CD8α+ DC subset as a protective source of IL-12 in T. gondii infection (Scharton-Kersten et al., 1997a), but such studies are inconclusive because these mice harbor additional defects beyond the loss of CD8α+ DCs. Irf8-deficient mice lack development of both CD8α+ DCs as well as pDCs (Aliberti et al., 2003; Tsujimura et al., 2003), and additionally have defects in activation of IFNγ-inducible genes (Tamura and Ozato, 2002). Thus, the increased susceptibility of Irf8−/− mice to T. gondii infection (Scharton-Kersten et al., 1997a) could result from the absence of either CD8α+ DCs or pDCs, or from a failure of IFNγ-induced effector mechanisms. Consistent with the latter, administration of IL-12 to Irf8−/− mice produces only a partial and temporary reduction in susceptibility to T. gondii (Scharton-Kersten et al., 1997a). In addition, CD8α+ DCs are the major source of IL-12 after intravenous administration of STAg (Reis e Sousa et al., 1997), although the relevance of this IL-12 to protection against live T. gondii has not been shown. In summary, although several cell types have been shown to be capable of producing IL-12 in response to T. gondii, the important cell type required for in vivo production of IL-12 after T. gondii infection has not been established.
In this study, we used Batf3−/− mice (Hildner et al., 2008) that are specifically defective in the generation of the CD8α+ DC subset to address the importance of these cells as a source of IL-12 during T. gondii infection. Batf3−/− mice exhibit decreased IL-12 and IFNγ production and a dramatically increased susceptibility to T. gondii, dying within 9 days after infection. Furthermore, this susceptibility in Batf3-deficient mice was reversed by administration of IL-12. Finally, we showed that the CD8α+ DCs were the only cells within the innate immune system whose IL-12 production was required for resistance to acute T. gondii infection.
Results
Batf3−/− mice are highly susceptible to T. gondii infection
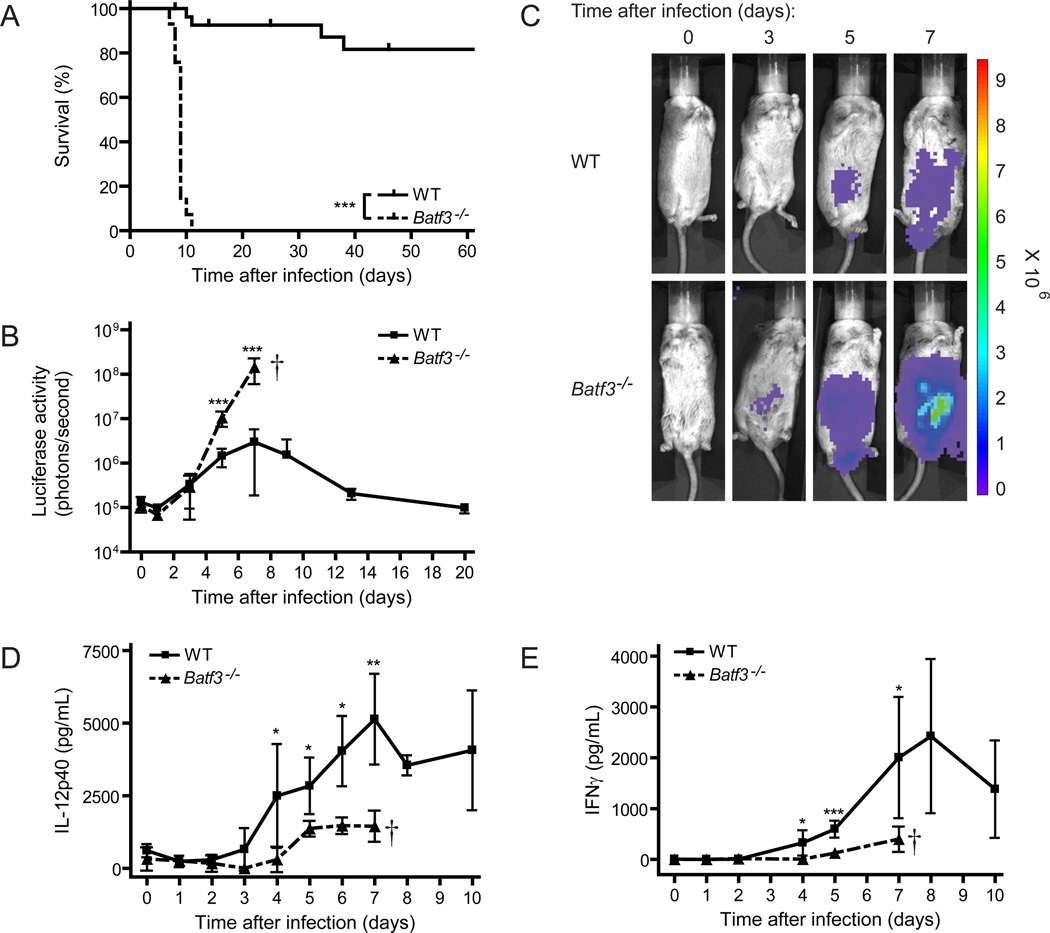
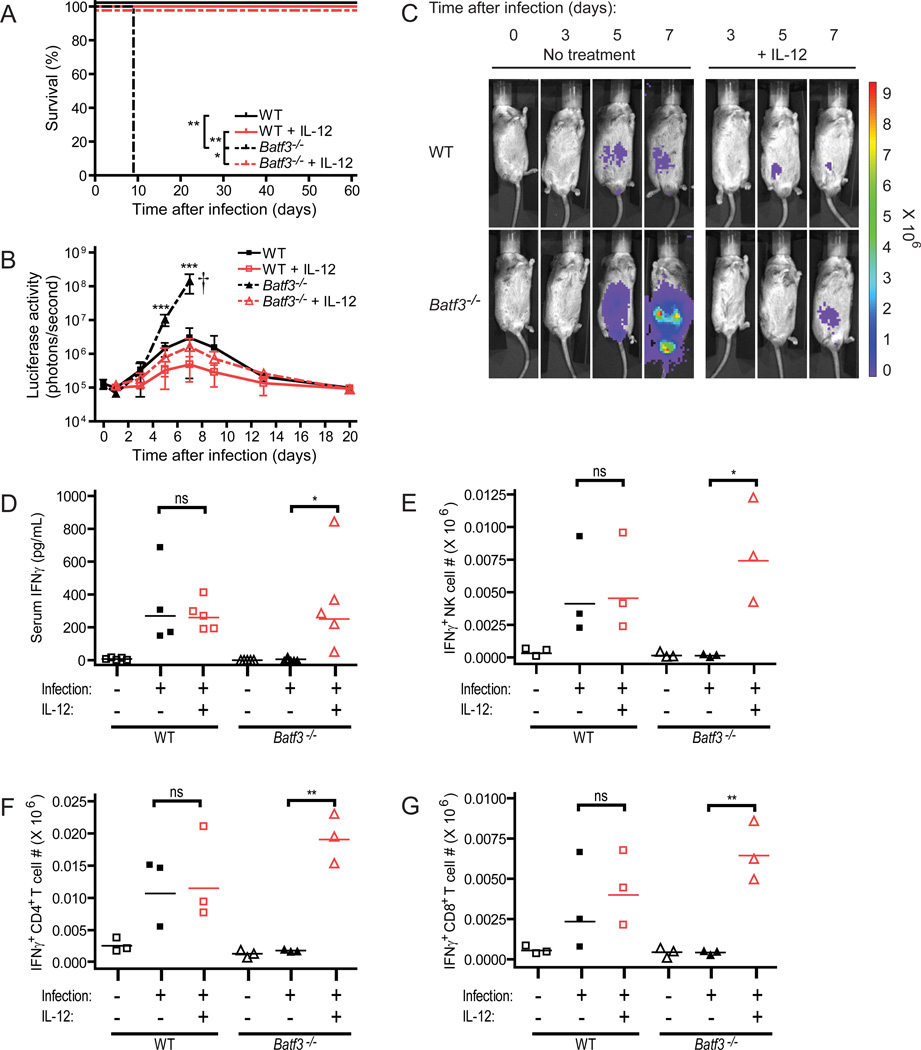
We first compared the survival of wild-type and Batf3−/− mice to infection with T. gondii (Figure 1). Intraperitoneal (ip) infection by tachyzoites of the type II avirulent Prugniaud (Pru) strain of T. gondii revealed a markedly increased susceptibility of Batf3−/− mice relative to wild-type mice (Figure 1A). While wild-type mice were resistant to T. gondii infection, infection of Batf3−/− mice was uniformly lethal in all genetic backgrounds tested and led to death within 9 to 10 days after infection. Using a T. gondii strain harboring a firefly luciferase transgene reporter, we observed approximately 100-fold increased parasite burden within 5 days following infection in Batf3-deficient mice compared to wild-type mice (Figure 1B and 1C). This exponential parasite growth continued in the Batf3−/− mice throughout the course of infection.
Figure 1. Batf3−/− mice rapidly succumb to infection with an avirulent strain of Toxoplasma gondii.
Mice were infected with T. gondii, monitored for survival (A) and parasite burden (B and C), and bled to measure serum cytokines (D and E). (A) Combined survival data from infected C56BL/6, 129S6/SvEV and BALB/c wild-type (solid line, n=30) and Batf3−/− (dashed line, n=29) mice from 8 independent experiments. (B) Infected wild-type (squares) and Batf3−/− (triangles) mice underwent whole body in vivo imaging throughout the course of infection to measure bioluminescence. Data shown is combined parasite burden from infected 129S6/SvEV mice from 2 independent experiments (n=5–8 at each time-point, representative of 6 independent experiments). (C) Representative bioluminescence images of infected 129S6/SvEV mice throughout the course of infection. (D and E) Infected 129S6/SvEV wild-type (squares) and Batf3−/− (triangles) mice were bled at various time-points after infection, and serum analyzed for cytokine concentrations. Data represents combined serum concentrations of IL-12p40 (D) and IFNγ (E) through the course of infection from 2–3 independent experiments (n=3–5 at each time-point). (B, D, E) Data are represented as mean +/− standard deviation. *: 0.01<P<0.05, **: 0.001<P<0.01, ***: P<0.001.
To extend our findings, we challenged wild-type and Batf3−/− mice with T. gondii cysts by oral gavage, which simulates the natural route of infection. Oral challenge of Batf3−/− mice demonstrated a similar susceptibility of these animals to T. gondii infection, with acute lethality and a failure to control parasite replication (Figure S1A and S1B). In addition, histological analysis of the spleen and ileum revealed extensive inflammation and destruction of tissue architecture in Batf3−/− mice 9 days after infection (Figure S1C). However, the underlying mechanism for this susceptibility is likely to be complex, and will be the focus of future studies. Specifically, gut CD103+ DCs are also absent in the Batf3−/− mice (Edelson et al., 2010), and may play a role during oral infection. All other experiments in this study were performed following intraperitoneal tachyzoite challenge.
To determine if the crucial effector cytokines IL-12 and IFNγ were being produced normally in Batf3−/ mice, we next examined the serum amounts of these cytokines. The IL-12 subunit p40, which is shared with the cytokine IL-23, is used as the readout for IL-12 in all cases, since IL-23 plays no role in acute T. gondii infection in the mouse (Lieberman et al., 2004). IL-12p40 concentrations in serum were markedly reduced in Batf3−/− mice relative to wild-type mice infected with T. gondii (Figure 1D). In wild-type mice, serum IL-12p40 began to increase on day 3 after infection, and increased until 7 days after infection. In contrast, IL-12p40 remained at basal amounts in Batf3−/− mice until day 5 after infection, at which point its increase was significantly reduced relative to wild-type mice for the remainder of infection. The decrease in IL-12p40 production in Batf3−/− mice correlated with significantly reduced concentrations of serum IFNγ (Figure 1E). In wild-type mice, IFNγ production began to increase after 4 to 5 days of infection, reaching a peak at day 8. By contrast, IFNγ showed no increase in Batf3−/− mice for 5 days after infection, and showed only a slight increase on day 7, when it was significantly reduced relative to wild-type mice.
CD8+ T cell priming to T. gondii-derived antigens is defective in Batf3−/− mice
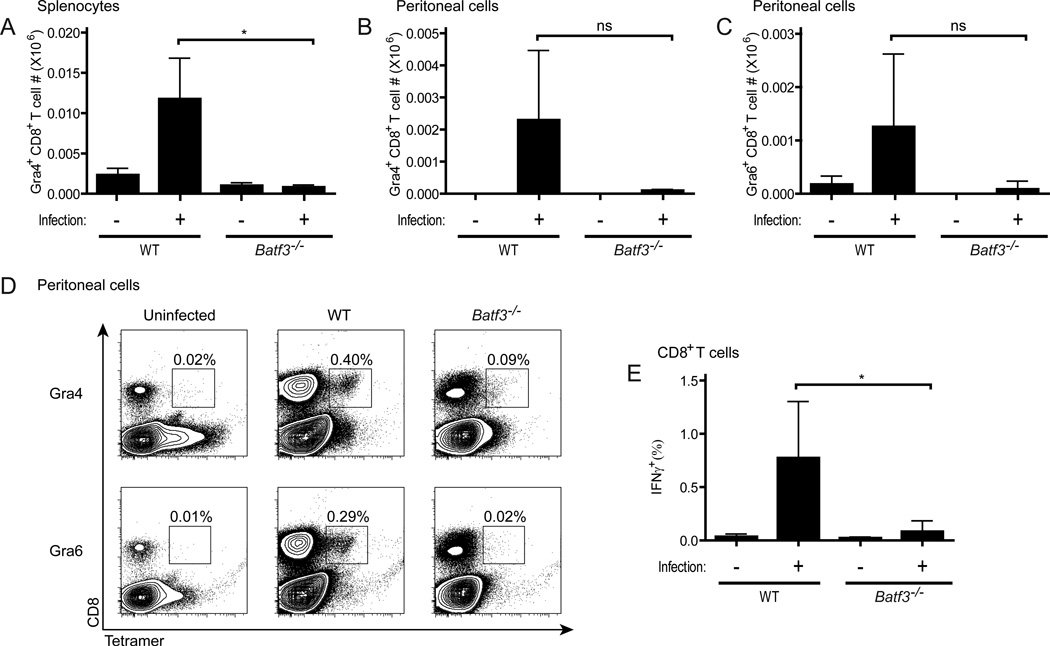
Since CD8α+ DCs are important for generation of virus-specific CD8+ effector T cells (Hildner et al., 2008), we examined T cell responses in Batf3−/− mice after infection by T. gondii (Figure 2). First, we used two MHCI tetramers to measure the expansion of CD8+ T cells specific for peptides derived from the GRA4 and GRA6 dense granule proteins of T. gondii (Frickel et al., 2008). Tetramer positive CD8+ T cells were significantly increased 8 days after infection with T. gondii in the spleen of wild-type mice, but not in Batf3−/− mice (Figure 2A). Tetramer staining in the peritoneum suggested a similar trend, although the data did not reach significance due to substantial variability in the observed response in wild-type mice (Figure 2B–2D). Total splenic CD8+ T cell numbers were comparable between wild-type and Batf3−/− mice both before and after infection (Figure S2B). However, the total number of peritoneal CD8+ T cells appeared to be highest in infected wild-type mice (Figure S2A), suggesting local proliferation or recruitment of activated cells, although again this increase did not reach significance as compared to Batf3−/− numbers. In addition, using the GRA4 peptide to activate splenic antigen-specific CD8+ T cells harvested 8 days after infection, we observed a significant increase in peptide induced IFNγ production from wild-type CD8+ T cells, but not from Batf3−/− CD8+ T cells (Figure 2E). Thus, Batf3−/− mice have reduced priming of IFNγ-producing CD8+ T cells after infection by T. gondii, suggesting that CD8α+ DCs contribute to the priming of CD8+ T cells against this intracellular pathogen.
Figure 2. CD8+ T cell priming to T. gondii is defective in Batf3-deficient mice.
BALB/c wild-type and Batf3−/− mice were infected with T. gondii, sacrificed on day 8 after infection, and analyzed for CD8+ T cell priming by tetramer staining ex vivo (A–D) and intracellular cytokine staining following peptide re-stimulation in vitro (E). (A) Representative plots of Ld-GRA4 and Ld-GRA6 tetramer staining in the peritoneum, with percentage of total peritoneal cells that are tetramer positive shown. (B–D) Absolute numbers of CD8+ tetramer-positive cells in the peritoneum (B and C) or spleen (D) specific for GRA4 (B and D) or GRA6 (C) on day 8 after infection (n=3, representative of 2 independent experiments). (E) Absolute numbers of IFNγ-positive CD8+ T cells as measured by intracellular cytokine staining after overnight re-stimulation of whole splenocytes with the GRA4 peptide (n=5). (B–E) Data are represented as mean +/− standard deviation. Not significant (ns): P>0.05, *: 0.01<P<0.05.
In summary, Batf3−/− mice are highly susceptible to T. gondii infection compared with wild-type mice, and have substantially reduced IL-12 and IFNγ production during early infection (Figure 1). In addition, priming of T. gondii-specific CD8+ T cells is reduced in infected Batf3−/− mice (Figure 2), although the rapid lethality of T. gondii infection in Batf3−/− mice suggests a defect in an innate rather than adaptive immune response. To further exclude a role for Batf3 in T cells in the acute lethality observed, we transferred wild-type purified T cells into Rag2-deficient mice that were either wild-type or deficient for Batf3. Rag2−/− mice cannot generate T or B cells due to a failure to recombine and express the required receptors, and therefore the only T cells present in these mice will be the transferred wild-type cells. Batf3−/−Rag2−/− animals that were given wild-type T cells were indistinguishable from Batf3−/− mice when examined for parasite burden after T. gondii infection (Figure S2C), suggesting that the defect observed in Batf3−/− mice is restricted to the innate compartment. Therefore, we next focused on identifying the cellular source of IL-12 relevant for protection against T. gondii infection in wild-type mice.
CD8α+ DCs increase in early infection by T. gondii and are the major producers of IL-12
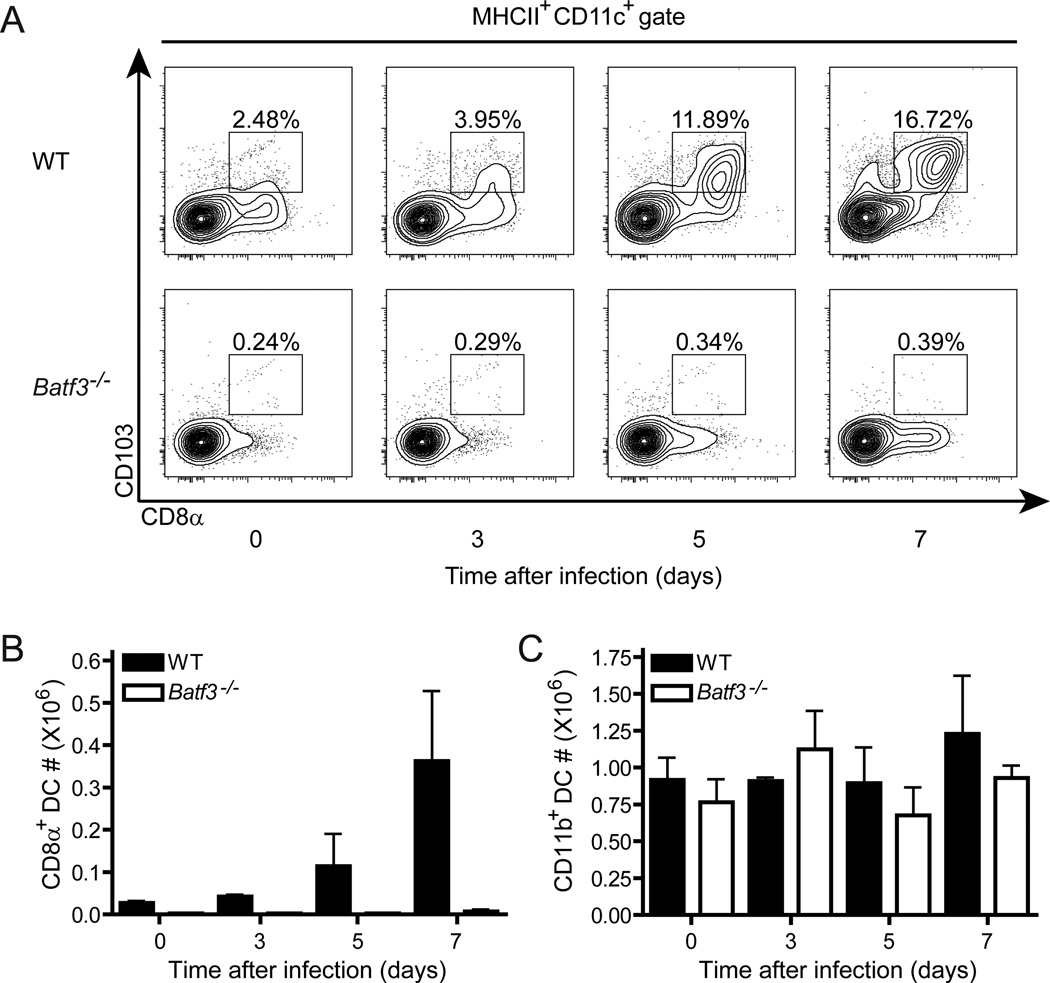
In uninfected wild-type mice, the CD8α+ subset of conventional DCs comprises approximately 5–10% of the total DC compartment in the spleen, depending on the mouse strain (Hildner et al., 2008). CD8α+ DCs also express several surface markers such as CD103, CD24 and DEC205 that distinguish it from the newly described CX3CR1+ CD8α+ DC subset that is distinct from classical CD8α+ DCs (Bar-On et al., 2010), and one of these additional markers is used in every experiment to ensure exclusion of the CX3CR1-expressing subset. The remainder of conventional DCs are distributed between those expressing high or low levels of CD11b. After infection by T. gondii, we observed that the percentage of CD8α+ DCs in wild-type mice increased to represent approximately 20% of the total DC compartment in the spleen by 7 days after infection (Figure 3A). By contrast, Batf3−/− mice lacked CD8α+ DCs as previously reported (Hildner et al., 2008) and showed no increase at any time after infection. Beyond this increase in their percentage, CD8α+ DCs also increased in absolute numbers in the spleens of wild-type mice after T. gondii infection (Figure 3B). By contrast, CD11b+ DCs were present in similar numbers during all times after T. gondii infection in both wild-type and Batf3−/− mice (Figure 3C and S3).
Figure 3. Splenic CD8α+ dendritic cells expand after T. gondii infection in wild-type mice.
129S6/SvEV wild-type and Batf3−/− mice were infected with T. gondii, sacrificed on days 0, 3, 5 and 7 after infection, and analyzed for changes in dendritic cell subsets by flow cytometry. (A) Representative flow cytometry plots gated on Aqua-negative, MHCII+, CD11c+ conventional dendritic cells. (B and C) Absolute numbers of CD8α+ CD103+ DCs (B) and CD11b+ DCs (C) in the spleen of wild-type (black bars) and Batf3−/− (white bars) mice throughout the course of infection (n=3, representative of 2 independent experiments). Data are represented as mean +/− standard deviation.
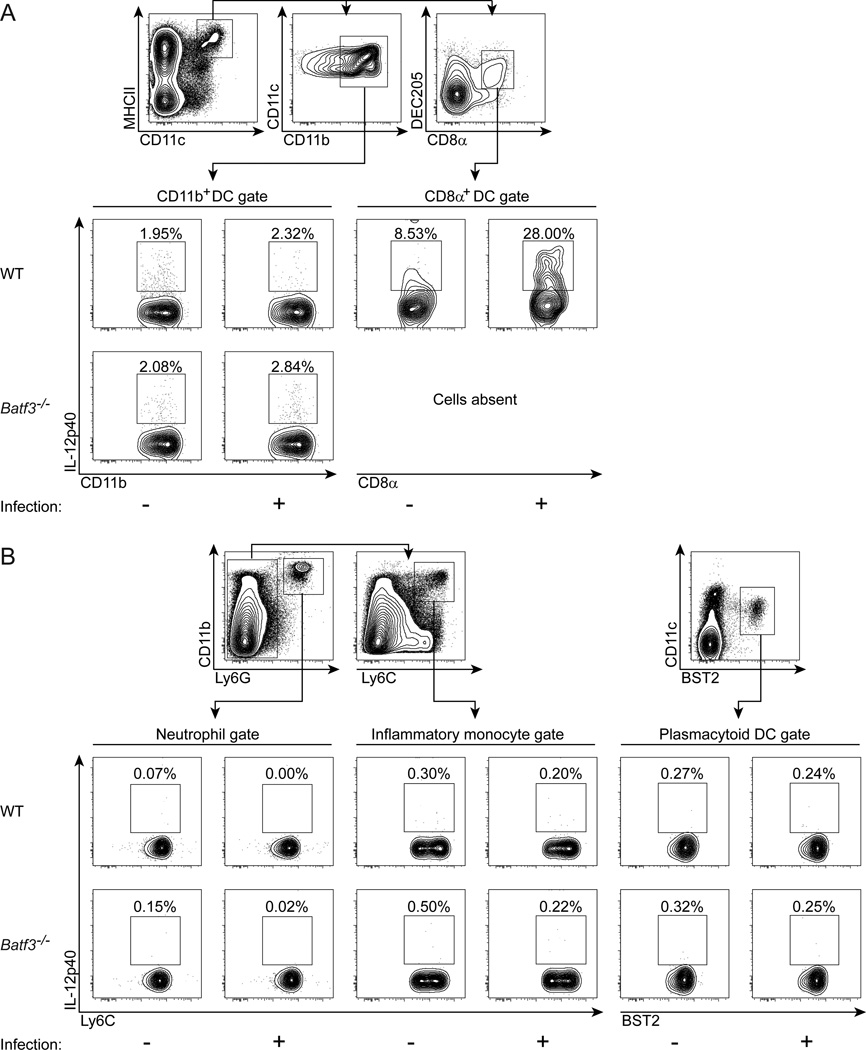
Increased numbers of CD8α+ DCs after T. gondii infection suggests a role in protection against this parasite. Therefore, production of IL-12p40 by various cell types was measured in wild-type and Batf3−/− mice after infection by T. gondii (Figure 4). We examined day 3 after infection specifically, since we were interested in cells producing IL-12p40 early enough after infection that could control the exponential growth of T. gondii observed as early as day 4 in Batf3−/− mice (Figure 1B). We used intracellular cytokine staining (ICS) to quantify IL-12p40 production by CD8α+ DCs, CD11b+ DCs, pDCs, inflammatory monocytes and neutrophils. The percentage of CD8α+ DCs producing IL-12p40 was increased from basal levels in uninfected mice to approximately 25–30% at day 3 after infection (Figure 4A). By contrast, the percentage of CD11b+ DCs that produced IL-12p40 was not significantly altered by infection, being approximately 2 to 3% in both infected and uninfected mice (Figure 4A). Furthermore, inflammatory monocytes, neutrophils and plasmacytoid DCs displayed no induction of IL-12p40 by T. gondii infection (Figure 4B). Accordingly, CD8α+ DCs express the highest amounts of the T. gondii profilin sensor TLR11 as compared with a variety of immune cell types (Figure S4A), suggesting that this cell is optimally poised for sensing T. gondii and producing initial IL-12 during early infection. In addition, since the IL-12p40 chain is shared between the cytokines IL-12 and IL-23, we formally excluded a role for IL-23 in our system by examining CD8α+ DC induction of the IL-23-specific subunit p19 and the IL-12-specific subunit p35 upon infection. Uninfected and infected CD8α+ DCs express the IL-12p40 subunit (Figure S4C), as shown above, in conjunction with the IL-12p35 subunit (Figure S4D), but not the IL-23p19 subunit (Figure S4B), clearly showing production of IL-12 and not IL-23 by these cells. In addition, expression of IL-12p40 is significantly increased in these cells on day 3 after infection (Figure S4D). Thus, CD8α+ DCs are the major IL-12-producing cells in the spleen 3 days after infection by T. gondii.
Figure 4. CD8α+ dendritic cells are the major producers of IL-12 after T. gondii infection in wild-type mice.
129S6/SvEV wild-type and Batf3−/− mice were infected with T. gondii, sacrificed on day 3 after infection, and analyzed for the cellular source of IL-12 by intracellular cytokine staining. (A) Representative flow cytometry plots gated on MHCII+ CD11c+ expressing CD11b+ DCs or CD8α+ DEC205+ DCs. (B) Representative flow cytometry plots gated on Ly-6G+ CD11b+ neutrophils, Ly-6G− Ly-6C+ CD11b+ inflammatory monocytes, or CD11c+ Bst2+ plasmacytoid DCs. (n=3, representative of 3 independent experiments).
IL-12 administration to Batf3−/− mice restores IFNγ production and controls T. gondii infection
If susceptibility of Batf3−/− mice to T. gondii results from decreased IL-12 production caused by the absence of CD8α+ DCs, then administration of IL-12 to Batf3−/− mice should restore their resistance to infection. Administration of recombinant murine IL-12 to wild-type mice had no impact on their susceptibility to infection by T. gondii (Figure 5A). In contrast, administration of IL-12 to Batf3−/− mice during the first 5 days of infection dramatically reversed their susceptibility, promoting their survival after infection for more than 60 days. Moreover, IL-12 treatment of Batf3−/− mice reduced their pathogen burden compared to untreated Batf3−/− mice, bringing parasite loads to levels in wild-type mice (Figure 5B and 5C).
Figure 5. Administration of IL-12 rescues Batf3-deficient mice during T. gondii infection.
129S6/SvEV mice were infected with T. gondii and injected with saline or 0.5µg of recombinant murine IL-12 on days 0, 1, 2, 3, and 4 after infection. (A) Survival data from infected mice (WT: solid black line; WT + IL-12: solid red line; Batf3−/−: dashed black line; Batf3−/− + IL-12: dashed red line) (n=3–5, representative of 3 independent experiments). (B) Combined parasite burden from whole body in vivo bioluminescence imaging of infected mice (WT: black squares; WT + IL-12: red squares; Batf3−/−: black triangles; Batf3−/− + IL-12: red triangles) from 2 independent experiments (n=3–8 at each time-point, representative of 4 independent experiments). Data are represented as mean +/− standard deviation. (C) Representative bioluminescence images of infected mice throughout the course of infection. (D) Serum concentrations of IFNγ on day 4 after infection (n=4–5). (E–G) Absolute numbers of IFNγ-positive NK (E), CD4+ T (F), and CD8+ T (G) cells in the spleen directly ex vivo on day 3 after infection as measured by intracellular cytokine staining (n=3). (D–G) Horizontal lines represent the geometric mean. Not significant (ns): P>0.05, *: 0.01<P<0.05, **: 0.001<P<0.01, ***: P<0.001.
Since reduced IL-12 in Batf3−/− mice may cause susceptibility to T. gondii by lowering early IFNγ production, we asked whether IL-12 administration to Batf3−/− mice also restored normal IFNγ production during infection (Figure 5D–5G). IL-12 administration to wild-type mice did not influence serum IFNγ concentrations at day 4 after infection (Figure 5D). However, IL-12 administration to Batf3−/− mice significantly increased serum IFNγ on day 4, which approximated amounts found in infected wild-type mice. The IFNγ induced by IL-12 in Batf3−/− mice appeared to arise from several cell types (Figure 5E–5G and S5A–S5C). NK, CD4+ and CD8+ T cells from infected wild-type mice produced IFNγ by ICS on day 3 when examined immediately ex vivo, but NK, CD4+ and CD8+ T cells from infected Batf3−/− mice were devoid of IFNγ at this time. However, administration of IL-12 to Batf3−/− mice infected with T. gondii substantially restored IFNγ production by all three cell types. In summary, IL-12 administration to Batf3−/− mice reverses their susceptibility to T. gondii infection, decreases pathogen burden, and increases IFNγ production by natural killer cells and T lymphocytes.
CD8α+ DCs are the only cell whose IL-12 production is required to control acute T. gondii infection
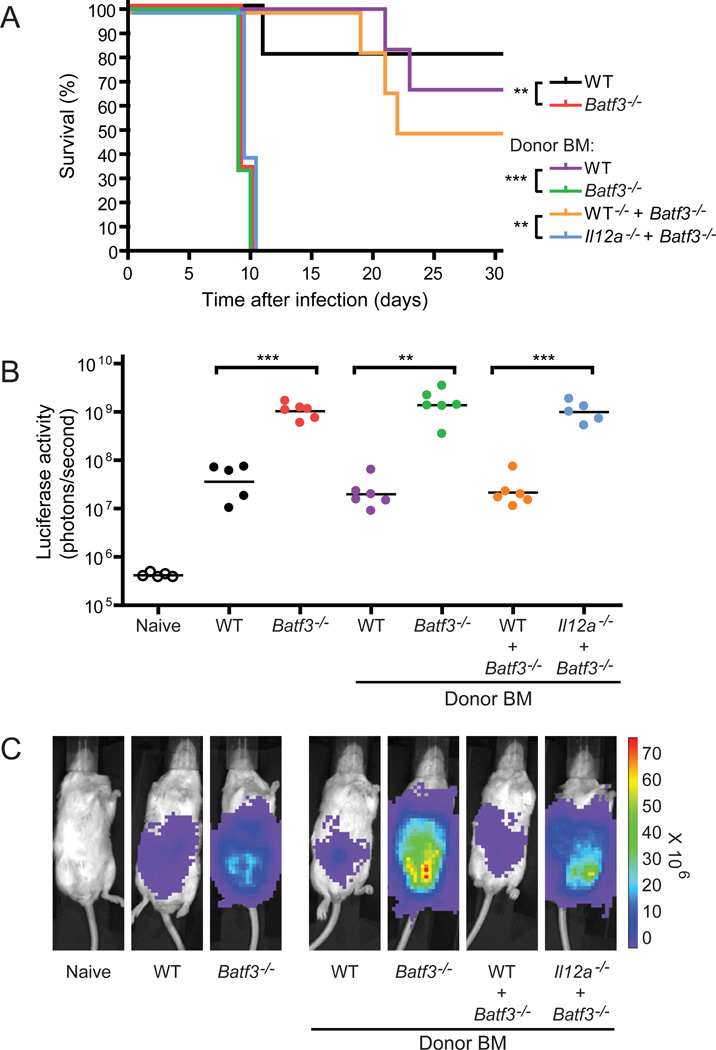
The fact that CD8α+ DCs are a major source of IL-12 during acute T. gondii infection does not prove that they are the only source of IL-12 capable of controlling infection, and their requirement for protection against acute infection may derive from different, unknown functions. To test whether IL-12 production by CD8α+ DCs is relevant for resistance to acute T. gondii infection, we generated mixed chimeras using bone marrow (BM) derived from Il12a−/− (encoding IL-12p35 subunit) and Batf3−/− mice. CD8α+ DCs can develop from Il12a−/− BM, but not Batf3−/− BM. This protocol allows the generation of chimeras in which CD8α+ DCs now develop but are unable to produce IL-12, while all other immune cell types can produce IL-12. If CD8α+ DCs are solely required for providing an early source of IL-12, then the mixed chimeras will remain susceptible to infection.
For this experiment, several other chimeras are necessary as controls. We generated chimeras receiving only wild-type, Batf3−/−, or Il12a−/− BM, as well as mixed chimeras receiving wild-type BM with either Batf3−/− or Il12a−/− BM (Figure 6 and S6A). Chimeras of all 6 types were infected with T. gondii and analyzed along with non-chimera controls for survival and parasite burden. First, chimeras reconstituted with wild-type BM controlled parasite numbers as expected, with burden equivalent to wild-type non-chimeric mice (Figure 6B and 6C). The majority of these mice also survived acute infection (Figure 6A). Chimeras reconstituted either with Batf3−/− or Il12a−/− BM succumbed to acute infection as expected and showed high parasite burdens, each approximately 100-fold higher that wild-type, reflecting the phenotype of the respective mutant non-chimeric mice (Figure 6A–6C and S6A).
Figure 6. CD8α+ dendritic cells are the only cells whose IL-12 production is protective against acute T. gondii infection.
BALB/c chimeras and control non-chimeric mice were infected with T. gondii and monitored for survival (A) and parasite burden (B–C). (A) Survival data from non-chimeric wild-type (black line) and Batf3−/− (red line) mice were compared to lethally irradiated recipients which received only wild-type (purple line) or Batf3−/− (green line) BM, or a 1:1 mixture of wild-type with Batf3−/− BM (orange line) or Il12a−/− with Batf3−/− BM (blue line) (n=5–6, representative of 2 independent experiments). Parasite burden (B) and representative images (C) on day 7 after infection from the groups in (A). (B) Horizontal lines represent the geometric mean. **: 0.001<P<0.01, ***: P<0.001.
We next examined mixed bone marrow chimeras. Mixed chimeras reconstituted with wild-type plus Batf3−/− BM or Il12a−/− BM showed low parasite burdens, equivalent to wild-type mice and chimeras reconstituted with wild-type BM (Figure 6B, 6C and S6A). In both of these mixed chimeras, only half of the cells would harbor a defect, and the other half would be normal. Thus, a half cell complement of normal cells appears sufficient for normal control of parasite burden.
Finally, we analyzed chimeras reconstituted with a mixture of Batf3−/− and Il12a−/− BM (Figure 6 and S6A). In these chimeras, CD8α+ DCs develop only from Il12a−/− BM, whereas all other cells develop from both IL-12-sufficient and Il12a−/− BM. Thus, in these chimeras, the CD8α+ DCs uniformly lack the capacity to produce IL-12, whereas all other cell types retain the capacity to produce IL-12. These mixed chimeras are highly susceptible to infection and have extremely high parasite burden, comparable to levels in Batf3−/− mice (Figure 6A–6C and S6A). These results indicate that the CD8α+ DCs are the only cell whose IL-12 production is sufficient for controlling parasite burden and maintaining resistance to acute T. gondii infection.
Discussion
The present study identifies a second critical activity for the CD8α+ DC subset beyond its recognized role in priming CD8+ T cells responses to viruses. Previously, we demonstrated that the CD8α+ DC was critical in promoting effective CTL responses against West Nile virus, and was crucial in that setting for cross-presentation of virus-derived antigens involved in immune activation (Hildner et al., 2008). Additionally, priming of Sendai virus-specific CTLs has also been shown to be dependent on the peripheral cross-presenting CD103+ DC which is also absent in the Batf3-deficient mice (Edelson et al., 2010). Here we show that priming of CD8+ T cells to endogenous T. gondii antigen is also defective in Batf3-deficient mice early after infection. Additionally, we demonstrate that the same DC subset provides a critical but distinct function by acting as an important early sensor of infection by T. gondii. The inability of mixed chimeras generated from bone marrow of Il12a-deficient and Batf3-deficient mice to control T. gondii infection demonstrates that the CD8α+ DC is the only cell whose IL-12 production significantly contributes to reducing pathogen burden during acute infection. Thus, in each of these pathogen settings, the CD8α+ dendritic cell is unique in its provision of effective defense mechanisms, but the mechanisms by which this cell mediates defenses are different.
Mice lacking Batf3 show a very selective elimination of the subset of DCs characterized by the selective expression of CD8 α, CD103, DEC205, CLEC9a, and Langerin (Hildner et al., 2008; Edelson et al., 2010; Sancho et al., 2009). In uninfected mice, DCs of this subset comprise between 5–10% of the total DC compartment, and are distributed both to the secondary lymphoid organs, including spleen and lymph nodes, where they express CD8α as a marker, as well as to various peripheral tissues, such as the dermis, lung, and lamina propria, where they lack CD8α but express the remaining markers (Edelson et al., 2010). Batf3-deficient mice do not exhibit any apparent global immunodeficiency, being generally healthy in the absence of overt infection, and generating essentially normal CD4+ T cells responses and antibody responses to viruses including West Nile virus (Hildner et al., 2008). Since control of many pathogens can be mediated by one of several immune effector mechanisms, the intact CD4+ T cell responses and antibody responses in Batf3-deficient mice would appear to be responsible for the overall general health. However, certain immune responses appear to be critically dependent on an intact cross-presentation pathway, such as the rejection of syngeneic fibrosarcoma, which is completely defective in Batf3-deficient mice (Hildner et al., 2008). Until now, studies of Batf3-deficient mice have largely focused on features of the adaptive immune response rather than examining innate immunity. Therefore, the present study identifies a critical role uniquely for the CD8α+ DC in innate immune responses against pathogens in vivo.
The role of CD8α+ DCs in protection against T. gondii infection was previously suggested through the observation that this subset was the major cell type to produce IL-12 in response to intravenous administration of T. gondii antigen STAg (Reis e Sousa et al., 1997). Furthermore, CD8α+ DCs express TLR11 at much higher levels than CD8α− DCs (Yarovinsky et al., 2005), neutrophils, and monocytes. However, pDCs also express TLR11 (Pepper et al., 2008), so that the correlation between sensitivity to activation by T. gondii does not exclusively identify the CD8α+ DC as the main responder. Thus, no clear evidence previously was able to uniquely identify the CD8α+ DCas a cell type required for controlling T. gondii infection in vivo. In addition, while Tlr11-deficient mice show impaired IL-12 production following infection by T. gondii (Yarovinsky et al., 2005), these mice only show a modest change in susceptibility compared to the dramatic increase seen in Myd88-deficient mice (Scanga et al., 2002), implying that additional sensors for T. gondii infection may exist. Our data strongly demonstrate that the CD8α+ DC is the main cell induced to produce IL-12 after acute challenge with T. gondii tachyzoites, which agrees with selective expression of TLR11 and potentially other uncharacterized T. gondii-specific sensors by this cell type. Nonetheless, other DC subsets may dominate in infections initiated by T. gondii cysts in the peritoneal cavity (data not shown).
It is unclear what advantage the immune system gains from limiting either cross-presentation or the production of IL-12 during infection to a single subset of dendritic cells. On the one hand, if cross-presentation is an important requirement for generation of CD8+ T cell responses against intracellular pathogens, one might reason that allowing all dendritic cells to exercise this function in vivo would better suite robust CTL responses. On the other hand, it is unclear what advantage the immune system gains by restricting IL-12 production in response to T. gondii infection to a single subset. CD8α+ DCs, which possess both peripheral and lymphoid resident populations, clearly express a unique pattern of innate sensors that distinguish these cells from other populations of conventional DCs and macrophage and/or monocytes subsets. Conceivably, restricting production of IL-12 to this unique subset could act to limit immunopathology that may derive from overproduction of IL-12 during infection. An example of the importance of this balance between immune activation and control is seen in the Il10-deficient mice, which succumb to T. gondii infection due to immunopathology caused by overproduction of IL-12 (Gazzinelli et al., 1996). Whatever the reasons, the present results clearly demonstrate a second critical function in vivo for the CD8α+ DC, in which selective activation of CD8α+ DCs and their subsequent production of IL-12 is a major pathway leading to early IFNγ-mediated control of Toxoplasma gondii infection.
Experimental Procedures
Mice
Wild-type 129S6/SvEv, BALB/c, C57BL/6, and B6.SJL mice were originally purchased from Taconic and then bred in-house for experimental use. C57BL/6 Rag2−/− mice were purchased from Taconic. Il12a−/− mice were purchased from Jackson Labs on both C57BL/6 and BALB/c backgrounds. Additional experimental C57BL/6 and B6.SJL mice were also purchased from Jackson Labs. Some experiments on the BALB/c background were done using C.Cg-Foxp3tm2Tch/J purchased from Jackson Labs that express an IRES-EGFP downstream of the Foxp3 gene; these mice were used as wild-type controls. Batf3−/− mice were previously generated in our laboratory (Hildner et al., 2008) on a 129S6/SvEv background, and subsequently backcrossed for 10 generations onto both C57BL/6 and BALB/c backgrounds. Mice were age and sex-matched for each experiment, and were generally between 8–15 weeks old. All mice were maintained under specific-pathogen-free conditions according to institutional guidelines and with protocols approved by the Animal Studies Committee of Washington University.
Parasites and infections
The type II Prugniaud strain of T. gondii expressing a firefly luciferase and GFP transgene (PRU-FLuc-GFP) (provided by J. Boothroyd, Stanford University, Palo Alto, CA) was used in all tachyzoite experiments. The parasites were grown in culture in human foreskin fibroblasts as previously described (Robben et al., 2004). For infections, freshly egressed parasites were filtered, counted, and injected intraperitoneally into mice. C57BL/6, 129S6/SvEv, and BALB/c mice were infected with 100, 200, and 1,000 tachyzoites, respectively, for most experiments. BALB/c mice used for tetramer studies were infected with 5,000 tachyzoites. BALB/c bone marrow chimeras and controls were infected with 100 tachyzoites.
Cell preparation
For all experiments except tetramer analysis, spleens were digested in 5mL Iscove’s Modified Dulbecco’s Media (IMDM, Invitrogen) containing 10% fetal calf serum (HyClone) with 250µg/mL collagenase B (Roche) and 30 U/mL DNase I (Sigma-Aldrich) for 1 hour at 37 degrees with agitation using stir-bars. For experiments analyzing intracellular cytokines, brefeldin A was added at 1 µg/mL during collagenase B and DNase I treatment, after which the cells were incubated for an additional 3 hours in IMDM with brefeldin A. Red blood cells were lysed by incubation in ACK lysis buffer. Cells were filtered through 80-µm strainers and counted on an analyzer (Vi-CELL, Beckman Coulter). 1–5 × 106 cells were stained for flow cytometric analysis.
For T cell analysis using tetramers, spleens were disrupted in 2mL ACK lysis buffer, filtered through 80-µm strainers and counted on a Vi-CELL analyzer. 1–3 × 106 cells were stained for flow cytometric analysis.
For analysis of peritoneal cells, a peritoneal lavage was performed with 10mL Dulbecco’s PBS (DPBS). Harvested cells were lysed in ACK buffer, filtered, counted, and stained for flow cytometry.
Flow cytometry
Cells were incubated for 5 minutes at 4 degrees with Fc Block (clone 2.4G2, BD) in FACS buffer (DPBS + 0.5% BSA + 2mM EDTA). Dead cells were excluded using LIVE/DEAD Aqua Fixable Dead Cell Stain Kit (Invitrogen). Surface staining was done for 20 minutes at 4 degrees in FACS buffer. For tetramer staining, cells were incubated in the presence of tetramer and surface antibodies for 45 minutes at 4 degrees. Absolute cell numbers were calculated using the total cell count multiplied successively by the percentages for the appropriate gates obtained through flow cytometry. Cells were analyzed on a BD FACSCantoII flow cytometer and data analyzed using FlowJo software (Tree star, Inc.).
Intracellular Cytokine Staining
For intracellular cytokine staining, cells were first surface stained, then fixed in 2% paraformaldehyde for 15 minutes at room temperature. Cells were then re-suspended in permeabilization buffer (DPBS + 0.1% BSA + 0.5% saponin) and stained with anti-IL-12p40 or anti-IFNγ for 30 minutes at 4 degrees.
In vitro T cell re-stimulation
4 × 106 splenocytes from day 8 infected mice were incubated overnight in 100 µL cIMDM with 100µg/mL GRA4 peptide (SPMNGGYYM). Brefeldin A at 1 µg/mL was added during the last 4 hours of incubation. Cells were then harvested and analyzed for IFNγ production using the intracellular cytokine staining protocol described above.
Luciferase imaging
Imaging was done as previously described (Saeij et al., 2005). Briefly, mice were given intraperitoneal injections of D-Luciferin (Biosynth AG, Switzerland) at 150mg/kg and allowed to remain active for 5 minutes. Animals were then anesthetized with 2% isoflurane for 5 minutes, and then imaged using a Xenogen IVIS 200 machine (Caliper Life Sciences). Data was analyzed using the Living Image software (Caliper Life Sciences).
ELISA/CBA
IL-12p40 concentration was measured from serum samples using the Mouse IL-12p40 OptEIA ELISA set (BD Bioscience). IFNγ serum concentration was measured using the BD CBA Mouse Inflammation Kit (BD Biosciences).
Administration of IL-12
Recombinant murine IL-12 (Peprotech) was resuspended in pyrogen-free saline at a concentration of 2.5µg/mL, aliquoted and frozen at −80 degrees. Mice were injected ip with 0.5µg of IL-12 on days 0, 1, 2, 3, and 4 after infection.
BM Chimera generation
This experiment was performed once on mice on the C57BL/6 background, and once on mice on the BALB/c background. Bone marrow from femurs and tibias were harvested, red blood cells lysed in ACK lysis buffer, filtered through 80-µm strainers, and counted using the Vi-CELL analyzer (Vi-CELL, Beckman Coulter). Recipient mice were irradiated with 800 (BALB/c) or 1,200 (C57BL/6) rads of whole body irradiation. In the experiment using C57BL/6 mice, all recipients were WT C57BL/6 or B6.SJL. In the experiment using BALB/c mice, WT recipients were used for the WT donor BM condition, while Batf3−/− recipients were used for the Batf−/−, WT + Batf3−/−, and Il12a−/−− + Batf3−/− donor BM conditions. The following day after irradiation, the recipients were injected intravenously with 2–4 million bone marrow cells from either a single donor or a 1:1 mixture from two donors. Mice were allowed to re-constitute for 10 (C57BL/6) to 18 (BALB/c) weeks after transfer, and subsequently bled to determine chimerism. In experiments using C57BL/6 mice, the congenic markers CD45.1 and CD45.2 were used to determine percent chimerism using flow cytometry. In experiments using BALB/c mice, male/female donors were mixed to allow for analysis of chimerism using the Y-chromosome. Peripheral blood from chimeras was lysed for genomic DNA and analyzed by quantitative real time PCR for the presence of the gene Zfy1 on the Y-chromosome using the following primers: Zfy1 (encoding zinc finger protein 1) Zfy1-forward, 5’-GCGTATCCTCATAAATGTGAC-3’, and Zfy1-reverse, 5’-CATCTCTTACACTTGAATGG-3’. Rag2 (encoding recombination activation gene 2) was used as a normalization control, Rag2-forward, 5’- GGGAGGACACTCACTTGCCAGTA-3’, and Rag2-reverse, 5’- AGTCAGGAGTCTCCATCTCACTGA-3’. Known mixtures of male-to-female DNA were used to generate a standard curve (100, 60, 50 and 40% male DNA), and to determine the percent of male DNA per sample.
Statistics
For analyses of survival data the log-rank test was used. For analyses of all other data, an unpaired, two-tailed Student’s t test with a 95% confidence interval was used (Prism; GraphPad Software, Inc.). All data are represented as means +/− SD.
Highlights.
-
➢
Batf3−/− mice missing CD8α+ DCs succumb to Toxoplasma gondii tachyzoite infection
-
➢
Batf3−/− mice have reduced amounts of IL-12 and IFNγ after infection
-
➢
IL-12 restores IFNγ and rescues survival in infected Batf3−/− mice
-
➢
CD8α+ DCs are the only critical source of IL-12 during T. gondii infection in vivo
Supplementary Material
Acknowledgements
This work was supported by the Howard Hughes Medical Institute (K.M. Murphy), the American Heart Association Midwest Affiliate Predoctoral Fellowship Program (M. Mashayekhi), and AI059176 (L.D. Sibley).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicting financial interests.
References
- Aliberti J, Schulz O, Pennington DJ, Tsujimura H, Sousa Reis E, Ozato K, Sher A. Essential role for ICSBP in the in vivo development of murine CD8alpha + dendritic cells. Blood. 2003;101:305–310. doi: 10.1182/blood-2002-04-1088. [DOI] [PubMed] [Google Scholar]
- Bar-On L, Birnberg T, Lewis KL, Edelson BT, Bruder D, Hildner K, Buer J, Murphy KM, Reizis B, Jung S. CX3CR1+ CD8alpha+ dendritic cells are a steady-state population related to plasmacytoid dendritic cells. Proc. Natl. Acad. Sci U. S A. 2010;107:14745–14750. doi: 10.1073/pnas.1001562107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss SK, Butcher BA, Denkers EY. Rapid recruitment of neutrophils containing prestored IL-12 during microbial infection. J Immunol. 2000;165:4515–4521. doi: 10.4049/jimmunol.165.8.4515. [DOI] [PubMed] [Google Scholar]
- Bliss SK, Gavrilescu LC, Alcaraz A, Denkers EY. Neutrophil depletion during Toxoplasma gondii infection leads to impaired immunity and lethal systemic pathology. Infect. Immun. 2001;69:4898–4905. doi: 10.1128/IAI.69.8.4898-4905.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss SK, Zhang Y, Denkers EY. Murine neutrophil stimulation by Toxoplasma gondii antigen drives high level production of IFN-gamma-independent IL-12. J Immunol. 1999;163:2081–2088. [PubMed] [Google Scholar]
- Dunay IR, Damatta RA, Fux B, Presti R, Greco S, Colonna M, Sibley LD. Gr1(+) inflammatory monocytes are required for mucosal resistance to the pathogen Toxoplasma gondii. Immunity. 2008;29:306–317. doi: 10.1016/j.immuni.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunay IR, Fuchs A, Sibley LD. Inflammatory monocytes but not neutrophils are necessary to control infection with Toxoplasma gondii in mice. Infect. Immun. 2010;78:1564–1570. doi: 10.1128/IAI.00472-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelson BT, Wumesh KC, Juang R, Kohyama M, Benoit LA, Klekotka PA, Moon C, Albring JC, Ise W, Michael DG, Bhattacharya D, Stappenbeck TS, Holtzman MJ, Sung SSJ, Murphy TL, Hildner K, Murphy KM. Peripheral CD103(+) dendritic cells form a unified subset developmentally related to CD8 alpha(+) conventional dendritic cells. J. Exp. Med. 2010;207:823–836. doi: 10.1084/jem.20091627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frickel EM, Sahoo N, Hopp J, Gubbels MJ, Craver MP, Knoll LJ, Ploegh HL, Grotenbreg GM. Parasite stage-specific recognition of endogenous Toxoplasma gondii-derived CD8+ T cell epitopes. J Infect. Dis. 2008;198:1625–1633. doi: 10.1086/593019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzinelli RT, Hieny S, Wynn TA, Wolf S, Sher A. Interleukin 12 is required for the T-lymphocyte-independent induction of interferon gamma by an intracellular parasite and induces resistance in T-cell-deficient hosts. Proc. Natl. Acad. Sci U. S A. 1993;90:6115–6119. doi: 10.1073/pnas.90.13.6115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzinelli RT, Wysocka M, Hayashi S, Denkers EY, Hieny S, Caspar P, Trinchieri G, Sher A. Parasite-induced IL-12 stimulates early IFN-gamma synthesis and resistance during acute infection with Toxoplasma gondii. J Immunol. 1994;153:2533–2543. [PubMed] [Google Scholar]
- Gazzinelli RT, Wysocka M, Hieny S, Scharton-Kersten T, Cheever A, Kuhn R, Muller W, Trinchieri G, Sher A. In the absence of endogenous IL-10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accompanied by overproduction of IL-12, IFN-gamma and TNF-alpha. J Immunol. 1996;157:798–805. [PubMed] [Google Scholar]
- Hildner K, Edelson BT, Purtha WE, Diamond M, Matsushita H, Kohyama M, Calderon B, Schraml BU, Unanue ER, Diamond MS, Schreiber RD, Murphy TL, Murphy KM. Batf3 deficiency reveals a critical role for CD8alpha+ dendritic cells in cytotoxic T cell immunity. Science. 2008;322:1097–1100. doi: 10.1126/science.1164206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou B, Benson A, Kuzmich L, DeFranco AL, Yarovinsky F. Critical coordination of innate immune defense against Toxoplasma gondii by dendritic cells responding via their Toll-like receptors. Proc. Natl. Acad. Sci U. S A. 2011;108:278–283. doi: 10.1073/pnas.1011549108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman LA, Cardillo F, Owyang AM, Rennick DM, Cua DJ, Kastelein RA, Hunter CA. IL-23 provides a limited mechanism of resistance to acute toxoplasmosis in the absence of IL-12. J Immunol. 2004;173:1887–1893. doi: 10.4049/jimmunol.173.3.1887. [DOI] [PubMed] [Google Scholar]
- Liu CH, Fan YT, Dias A, Esper L, Corn RA, Bafica A, Machado FS, Aliberti J. Cutting edge: dendritic cells are essential for in vivo IL-12 production and development of resistance against Toxoplasma gondii infection in mice 1. J Immunol. 2006;177:31–35. doi: 10.4049/jimmunol.177.1.31. [DOI] [PubMed] [Google Scholar]
- Mordue DG, Sibley LD. A novel population of Gr-1+-activated macrophages induced during acute toxoplasmosis. J Leukoc. Biol. 2003;74:1015–1025. doi: 10.1189/jlb.0403164. [DOI] [PubMed] [Google Scholar]
- Pepper M, Dzierszinski F, Wilson E, Tait E, Fang Q, Yarovinsky F, Laufer TM, Roos D, Hunter CA. Plasmacytoid dendritic cells are activated by Toxoplasma gondii to present antigen and produce cytokines. J Immunol. 2008;180:6229–6236. doi: 10.4049/jimmunol.180.9.6229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst HC, Tschannen K, Odermatt B, Schwendener R, Zinkernagel RM, Van Den BM. Histological analysis of CD11c-DTR/GFP mice after in vivo depletion of dendritic cells. Clin. Exp. Immunol. 2005;141:398–404. doi: 10.1111/j.1365-2249.2005.02868.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis e Sousa C, Hieny S, Scharton-Kersten T, Jankovic D, Charest H, Germain RN, Sher A. In vivo microbial stimulation induces rapid CD40 ligand-independent production of interleukin 12 by dendritic cells and their redistribution to T cell areas. J. Exp. Med. 1997;186:1819–1829. doi: 10.1084/jem.186.11.1819. [see comments] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robben PM, Mordue DG, Truscott SM, Takeda K, Akira S, Sibley LD. Production of IL-12 by macrophages infected with Toxoplasma gondii depends on the parasite genotype. J Immunol. 2004;172:3686–3694. doi: 10.4049/jimmunol.172.6.3686. [DOI] [PubMed] [Google Scholar]
- Saeij JP, Boyle JP, Grigg ME, Arrizabalaga G, Boothroyd JC. Bioluminescence imaging of Toxoplasma gondii infection in living mice reveals dramatic differences between strains. Infect. Immun. 2005;73:695–702. doi: 10.1128/IAI.73.2.695-702.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancho D, Joffre OP, Keller AM, Rogers NC, Martinez D, Hernanz-Falcon P, Rosewell I, Sousa Reis E. Identification of a dendritic cell receptor that couples sensing of necrosis to immunity. Nature. 2009;458:899–903. doi: 10.1038/nature07750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayles PC, Johnson LL. Exacerbation of toxoplasmosis in neutrophil-depleted mice. Nat Immun. 1996;15:249–258. [PubMed] [Google Scholar]
- Scanga CA, Aliberti J, Jankovic D, Tilloy F, Bennouna S, Denkers EY, Medzhitov R, Sher A. Cutting edge: MyD88 is required for resistance to Toxoplasma gondii infection and regulates parasite-induced IL-12 production by dendritic cells. J Immunol. 2002;168:5997–6001. doi: 10.4049/jimmunol.168.12.5997. [DOI] [PubMed] [Google Scholar]
- Scharton-Kersten T, Contursi C, Masumi A, Sher A, Ozato K. Interferon consensus sequence binding protein-deficient mice display impaired resistance to intracellular infection due to a primary defect in interleukin 12 p40 induction. J. Exp. Med. 1997a;186:1523–1534. doi: 10.1084/jem.186.9.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharton-Kersten TM, Yap G, Magram J, Sher A. Inducible nitric oxide is essential for host control of persistent but not acute infection with the intracellular pathogen Toxoplasma gondii. J Exp. Med. 1997b;185:1261–1273. doi: 10.1084/jem.185.7.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat Immunol. 2006;7:311–317. doi: 10.1038/ni1309. [DOI] [PubMed] [Google Scholar]
- Tamura T, Ozato K. ICSBP/IRF-8: its regulatory roles in the development of myeloid cells. J Interferon Cytokine Res. 2002;22:145–152. doi: 10.1089/107999002753452755. [DOI] [PubMed] [Google Scholar]
- Tsujimura H, Tamura T, Ozato K. Cutting edge: IFN consensus sequence binding protein/IFN regulatory factor 8 drives the development of type I IFN-producing plasmacytoid dendritic cells. J Immunol. 2003;170:1131–1135. doi: 10.4049/jimmunol.170.3.1131. [DOI] [PubMed] [Google Scholar]
- Yap GS, Shaw MH, Ling Y, Sher A. Genetic analysis of host resistance to intracellular pathogens: lessons from studies of Toxoplasma gondii infection. Microbes Infect. 2006;8:1174–1178. doi: 10.1016/j.micinf.2005.10.031. [DOI] [PubMed] [Google Scholar]
- Yarovinsky F, Zhang D, Andersen JF, Bannenberg GL, Serhan CN, Hayden MS, Hieny S, Sutterwala FS, Flavell RA, Ghosh S, Sher A. TLR11 activation of dendritic cells by a protozoan profilin-like protein. Science. 2005;308:1626–1629. doi: 10.1126/science.1109893. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.