Abstract
Focus group interviews were conducted with parents of children with sickle cell disease to explore parent-sibling communication about sickle cell disease. Communication was influenced by attributes and behaviors of the parent, the child with sickle cell disease, and the sibling; extended family, neighbors, friends, and church members or social networks; and available, accessible resources related to the child’s health, child’s school, and parent employment. Outcomes that influenced and were influenced by factors within and outside the parent-sibling dyad and nuclear family included parent satisfaction, parent roles, family intactness, and status attainment. These findings support previous research with African American families and expand our views of the importance of educating parents, family members, and others about sickle cell disease. The findings suggest a need to explore sibling perception of this communication, parent and sibling perception of the impact of frequent hospitalizations and clinic visits on the sibling and family, and variations within families of children with sickle cell disease.
Keywords: African American families, family communication, parent-sibling communication, siblings, sickle cell disease
Introduction
Sickle cell disease (SCD) is a genetic condition that is the result of a single point mutation in the β-globin gene (β), producing the abnormal Hemoglobin (Hb) S. Individuals homozygous for this mutation (Hb SS), or with a combination of the sickle mutation and other β-globin gene mutations (e.g. Hb SC, HbSβ-thalassemia) experience a variety of acute complications, including painful events (also known as painful crises), acute splenic sequestration, stroke, and acute chest syndrome. Sickle cell disease is a life-long condition which is characterized by progressive and inevitable organ damage interspersed with episodic acute complications. Children with SCD are particularly vulnerable to infection, since their splenic function is lost at a very early age. This loss of function places these youngsters at great risk for invasive infection by pneumococcus bacteria and other encapsulated organisms (Pearson, Spencer, & Cornelius, 1969; Serjeant & Serjeant, 2001). Chronic ischemic insult to the brain, in the form of silent cerebral infarction, leads to progressive cognitive dysfunction and increases the risk of overt stroke in persons with SCD (Miller et al., 2001; Schatz, Brown, Pascual, Hsu, & DeBaun, 2001). In addition, cardiac, pulmonary, renal, and retinal damage are among the observed organ dysfunctions which persons with SCD experience with aging. Taken together, the acute and chronic aspects of SCD produce a condition that requires continued medical attention for prevention and treatment of complications.
Sickle cell disease affects approximately one of every 500 African American births. It also affects persons of Mediterranean, Middle Eastern, and East Indian ancestry. In the U.S., one in 10 African Americans have sickle cell trait, and it is estimated that more than two million persons have sickle cell trait (Lerner, Platania, & LaBella, 2009; National Heart, Lung, and Blood Institute, 2002). The mortality rate for SCD is highest during the first three years of life. Clinic visits for routine well-child care are recommended every two to three months during the child’s first two years and every six months thereafter (National Heart, Lung, and Blood Institute, 2002; Vichinsky & Lubin, 1987). Careful monitoring of children with SCD can help prevent life-threatening complications, serious disability, and can decrease the economic and emotional burden related to their care. Parents must learn physical assessment skills, how to navigate the medical system, and how to keep health records on their child in case of an emergency (National Heart, Lung, and Blood Institute, 2002). Hospitalizations occur on a regular basis for some children with SCD. An average of 75,000 hospitalizations due to SCD occurred in the U.S. between 1989 and 1993 at a cost of approximately $475 million (Ashley-Koch, Yang, & Olney, 2000).
The care of the child with SCD demands increased attention from the parent(s), which may be at the expense of the time and care available for siblings of the child with SCD (Gold, Treadwell, Weissman, & Vichinsky, 2008). Communication within families of children with SCD is very important in trying to reconcile possible “shifts” in demanded attention toward a child with this disorder. Although communication within families that include children with SCD has not been adequately investigated, research on parent-sibling communication that includes children with other chronic disorders can give some clues about families of children with SCD. In their study of families of children with physical disabilities,Pit-ten Cate and Loots (2000) found that most siblings experienced open communication with their parents and most appreciated the opportunity to talk openly; however, other studies have indicated that parents communicate little with siblings (Fanos, Puck, & Davis, 2001; Horsely & Patterson, 2006).
Open and problem-solving communication can lead to better psychological adjustment for siblings (Giallo & Giavidia-Payne, 2006). For parents who struggle with how to communicate openly, interventions can successfully provide guidance (Horsely & Patterson, 2006). The purpose of this study is to explore parent-sibling communication in families of children with SCD by identifying factors within and outside the parent-sibling dyad that influence parent-sibling communication. An increased understanding of parent-sibling communication about SCD can guide the development of useful educational and counseling strategies for these families and contribute to improved outcomes for the child with SCD.
Conceptual Framework
This study was guided by Fitzpatrick and Caughlin’s (2002) taxonomy on families and family communication. Fitzpatrick and Caughlin proposed that family communication be studied by examining the links among endogenous factors (i.e., internal, performance, and outcome variables). Internal variables (i.e., communication structure, information-processing structure, and family roles) were measured using family members’ verbal and nonverbal messages. Performance variables included behaviors that involved verbal and nonverbal exchanges such as relationship adjustment, child socialization, and tension management. The outcome variables were measures of satisfaction and family stability. Fitzpatrick and Caughlin also proposed that a complete view of family communication must take into consideration the exogenous factors or aspects of the environment and their influence on and relationship to endogenous variables. Exogenous factors included variables such as the social, political, and economic environment of a family; family value orientations; social class; and access to resources and social networks. We used some elements of Fitzpatrick and Caughlin’s (2002) taxonomy to guide the development of an interview guide. Given the limited research on communication within families of children with SCD, this taxonomy offers an open approach to explore communication within families of children with SCD.
Fitzpatrick and Caughlin (2002) discussed three classes of definitions of family, family structure, psychosocial task, and transactional process. Family structure definitions refer to the family of origin (i.e., persons have established biological or sociolegal legitimacy through shared genetics, marriage, or adoption) and family of procreation (i.e., persons living in the same household). Psychosocial task definitions of family refer to having at least one adult member and one or more persons who work together to fulfill the needs of the group, nurture, and develop its members. Transactional process definitions consider the family as a group of individuals who are intimate or have a sense of home and group identity, have strong ties of loyalty and emotion, and have experience with a past and expect to experience a future. Communication is the means to establishing interdependence and commitment, forming ties of loyalty and identity, and conveying family identity, history, and future. Transactional process definitions allow families to define themselves rather than basing relationships on legal or genetic criteria and to recognize the importance of communication in families. Communication is necessary but inadequate in itself to understand, explain, or predict family outcomes (Fitzpatrick & Caughlin, 2002). Communication links the endogenous factors, but also must consider exogenous factors that influence and affect internal family processes.
Method
This qualitative descriptive study used focus group interviews to explore parents’ perspectives of their communication with siblings of children with SCD. Focus group interviews provide participants with opportunities to share their views about a certain topic of interest by interacting with others in a group. This interaction can provide participants with insights into another’s experiences and opinions as participants compare and contrast their experiences (Morgan, 1997). In addition to being more efficient than individual interviews, focus group interviews may place fewer burdens on participants to respond and can be helpful when participants may not have thought out the topic or are hesitant to share their views (Krueger & Casey, 2000).
Participants and Setting
Following approval of study procedures by the hospital and the university institutional review boards, a purposive sample was recruited from families whose children received services through the Sickle Cell Center (Center). This Center serves approximately 800 children and adolescents with SCD in the mid-southern United States. Parents eligible to participate in the study had children with SCD who were cared for at the Center and were between one and 21 years of age. Eligible parents also had one or more children without SCD (siblings) who were between 5 and 21 years of age. These siblings did not have a genetic disorder, chronic illness, or disability but could be carriers of SCD.
Participants were recruited through an advertisement-letter that was mailed to parents whose children were receiving services through the Center. Parent eligibility was determined at the time parents telephoned to express interest in participating in the study. Each group was limited to 12 persons. Fifty-two parents telephoned to express interest in the focus group interviews. The parent contacting the investigator was selected as the group participant. During the initial conversation with each parent, investigators informed eligible parents of the time, date, and location of the focus group interview. As parents and Center staff identified Monday evening or Saturday morning as the most convenient for parents to attend a focus group interview, parents chose to attend one of these two focus group interviews. A reminder letter was mailed one week prior to each interview date, and a reminder telephone call was made the day before the interview. The focus group interviews were conducted on the Center’s campus in a quiet and comfortable conference room located in an office building adjacent to the SCD outpatient clinic.
Interviews
The moderator, a highly skilled social worker, conducted the semi-structured interviews using a guide (Table 1) to provide direction to the group discussion. The assistant moderator was a doctoral nursing student. Prior to the interview, the moderator and assistant moderator received training on conducting a focus group interview and recording the discussion. The training and scripts for the moderator and assistant moderator were developed using guidelines recommended by Krueger and Casey (2000). A broad opening question was followed by more specific questions that focused on the content and structure of parent-sibling communication.
Table 1.
Interview Guide
Introduction: The purpose of this meeting is for you to share your thoughts and ideas about how you talk with the brothers and sisters of your child with sickle cell disease. Some parents and the brothers and sisters or siblings of children with special needs have said that their communication with each other is open and easy. Other parents and the siblings have said it is hard or difficult to talk about a chronic illness.
|
As parents arrived for the interview, the assistant moderator obtained informed consent and asked each participant to complete a demographic form. Refreshments were available prior to and during the focus group interview. The moderator and assistant moderator carefully followed their scripts to create an environment that was safe, responsive, and conducive to participant sharing. The moderator’s script included: (a) introductions; (b) purpose of focus group interview; (c) establishing ‘ground rules’ (i.e., there are no right or wrong answers, participant views will differ, you are free to respond to what other participants are saying and ask each other questions, talk one at a time, avoid having side conversations with participant beside you); and (d) the Interview Guide, which facilitated discussion. The assistant moderator’s script included directions for audio recording and making written notes during each focus group interview. Audio recording began with the moderator’s introduction and ended after parents validated, revised, and expanded on the assistant moderator’s summary and observations.
The opportunity for member validation (Smith, 1996) of the assistant moderator’s summary was welcomed by participants, who offered their own summaries of the group discussion and shared additional information and insights. Each focus group interview lasted two hours. Parents received a payment of $30 to cover the cost of transportation and childcare. A debriefing session between the moderator and assistant moderator was held following each focus group interview.
Analysis
The recordings were transcribed verbatim and the transcripts were checked against the audio recordings to ensure accuracy. The final transcript was imported into NVivo7 (QSR International Pty Ltd, 2007) software to assist with data organization and analysis. Two researchers read each transcript and identified text units to be coded. After independently coding text units, both researchers compared codes, resolved differences, and defined each code. Codes were organized into categories and categories were organized into themes. Both researchers used an iterative process in which they returned to the data to ensure that the categories and themes represented the coded data. The researchers engaged in discussions to review their analytical memos, re-contextualize the data, explore biases and disagreements, and build consensus (Denzin & Lincoln, 2005). The resulting categories and themes were further examined from the perspective of Fitzpatrick and Caughlin’s taxonomy to identify factors influencing communication.
Results
Parent, child, and sibling characteristics are presented in Table 2. Participants were African American and ranged in age from 26 to 60 years with a mean age of 40.6 years. Participants will be referred to as parents, as all but two of the participants were mothers. One father and one grandmother participated in the study. Parent # 1 through 10 participated in the Saturday morning focus group interview; parent #11 through 16 participated in the Monday evening focus group interview. Children with SCD ranged in age from two to 17 years, with a mean age of 10.4 years. Parents rated the health of their children with SCD as very good (n = 2), good (n = 7), fair (n = 4), or poor (n = 3). Birth order of the children with SCD ranged from 1 to 7. Using a scaled response item, with 1 = “know very little” and 10 = “know a lot,” parents responded to the question, “How knowledgeable are you about your child’s diagnosis of sickle cell disease?” Parents rated their knowledge of SCD with a mean score of 8.8 (SD = 1.3). Using the scaled response item, with 1 = “know very little” and 10 = “know a lot,” parents responded to the question, “How knowledgeable are your children (except the child with sickle cell disease) about sickle cell disease?” Parents rated siblings’ knowledge of SCD (M = 7.0, SD = 2.8). The mean age of siblings was 15.1 years.
Table 2.
Parent, child, and sibling characteristics
| Parent* | Education | Parent age | Parent gender | Child age | Child gender | Child birth order | Health rating** | Number of siblings | Parent knowledge | Sibling knowledge |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | High school | 27 | Female | 10 | Male | 1 | 4 | 3 | 9 | 9 |
| 2 | High school | 34 | Female | 9 | Male | 1 | 4 | 2 | 10 | 1 |
| 3 | High school | 48 | Female | 4 | Male | 1 | 3 | 5 | 7 | 7 |
| 4 | Partial college | 26 | Female | 2 | Male | 2 | 3 | 1 | 6 | 3 |
| 5 | High school | 36 | Female | 14 | Male | 1 | 2 | 1 | - | - |
| 6 | Undergraduate | 37 | Female | 12 | Male | 1 | 3 | 1 | 10 | 10 |
| 7 | High school | 35 | Female | 13 | Male | 2 | 2 | 1 | 10 | 10 |
| 8 | Partial college | 54 | Female | 17 | Male | 4 | 1 | 3 | 7 | 4 |
| 9 | High school | 60 | Male | 17 | Male | 4 | 1 | 3 | 8 | 5 |
| 10 | Partial college | 39 | Female | 13 | Male | 1 | 3 | 1 | 8 | 5 |
| 11 | Partial college | 33 | Female | 10 | Male | 3 | 3 | 2 | 10 | 5 |
| 12 | High school | - | Female | 12 | Female | 1 | 2 | 1 | 10 | 10 |
| 13 | High school | 53 | Female | 10 | Male | 7 | 1 | 6 | 10 | 9 |
| 14 | Partial college | 49 | Female | 16 | Male | 3 | 3 | 2 | 8 | 8 |
| 15 | - | - | Female | 5 | Female | 5 | 2 | 4 | 9 | 9 |
| 16 | High school | 37 | Female | 2 | Female | 4 | 3 | 2 | 10 | 10 |
Note. Dashes indicate missing data.
Parent 3 is a grandmother
Health rating: 1=poor, 2=fair, 3=good, 4=very good
Exogenous Factors
The categories and themes evolving from the focus group interviews reveal that parents focused much of their discussion on social networks and the availability and accessibility of resources. The coded data did not support categories and themes that were related to other exogenous factors such as the social, political, and economic environment of families; family value orientations; and social class (Fitzpatrick & Caughlin, 2002).
Social Networks
Social networks were made up of extended family, neighbors, friends, and church members. Parents discussed support they received from extended family members and the responses of neighbors, friends, and church members.
Extended family
Parents’ perceptions of support from extended family members (i.e., grandparents, aunts, cousins, and a godparent) varied within and across individuals. Extended family members’ knowledge of SCD, prior experience with a relative with SCD, and observation of the child during a painful crisis contributed to their ability and willingness to support and help parents and the child with SCD.
Family members’ limited knowledge of SCD and incorrect perceptions of the etiology of SCD created challenges for Parent 4.
At first, I didn’t understand it all. We had school education but I was not educated about sickle cell. Her grandparents, even her dad—her grandmother told me that she would grow out of it. I could have fell through the floor. Then her dad listens to the grandmother (who) would tell her that she ate too many sweets and that if she would stop eating sweets that she would feel better.
Having a relative with SCD prepared some parents. Parent 1 assisted her father who had SCD and he, in turn, supported her. “One (time) my daddy had a bone crisis. I had to take him to get some morphine, and he would be alright.” Her parents were understanding and patient because they “know more about what it is… My parents are willing to learn more. Like my daddy coming to the appointment (for my son).”
Family members who observed a child in a painful crisis gained a greater understanding of SCD and respect for a parent’s concerns. Parent 2 described her family in the following:
But a lot of folks told me I was trying to make him sicker than he was. Once they saw and realized it … Well actually, my aunt, thank God that she saw it. They know that my son has sickle cell. They called me at work. They thought he was going to die. They took him to the hospital. He was in so much pain he couldn’t even walk.
Neighbors and friends
Social networks included the family’s neighbors and friends, and friends of the child with SCD. Their responses to the child reflected affection, concern, and support for the child; curiosity; and a limited understanding of SCD. Although neighbors were positive, accepting, and loving toward her two year old daughter with SCD, Parent 16 observed that her neighbors were also afraid.
Seem like they (neighbors) treat her more like an angel. Because my baby is well loved all through the neighborhood. They love her every time they see her. They just love her. And you know, my little girl, they be scared. Even though she’ll be hollering, they be thinking that she is like that all the time.
Friends and parents of friends were curious about SCD, but resorted to teasing. According to Parent 14, the friends and parents of her 16 year old son with SCD “would always ask why? Even when we try to explain to them about the disease, they would just tease. They make him feel really bad.”
Some children with SCD received support from their friends, while others were isolated and teased by their peers, who had limited understanding of SCD. Parent 15 explained, “One little girl at school found out that (my daughter) had sickle cell. They did her a little card. The kids got to the point where they didn’t want to be around her because they thought it was contagious.”
Church members
Most parents viewed church members as providing support through their expressions of concern for the child, having limited knowledge of SCD, and treating the child and siblings equally. Parent 8 described her church as having “a solid membership. And the people that’s there, if they don’t see my son with SCD coming, they’re very concerned. They say, ‘How is he feeling?’ So they just show concern when he does not come to church.” Parent 7 also pointed to church members’ limited knowledge of SCD, “My church family was like most people, uneducated, because they absolutely do not know of anybody in the church that knows about sickle cell. But they show concern.”
Resources
Parents discussed the availability and accessibility of resources related to health, school, and employment. Parents wanted health professionals, school staff, and employers who understood SCD and the challenges associated with SCD for their children and family.
Health
Parents interacted with health professionals and staff in various clinical settings to address the health needs of the child with SCD. They accessed health care for (a) specialized care at the Center with hematologists and social workers, (b) emergency care at local hospitals with nurses and physicians, (c) acute care at a pediatric hospital with nurses and physicians, (d) routine examinations in a pediatrician’s office, and (e) dental care in pediatric dentist’s office. Parents encountered problems maintaining health insurance for their children, especially their child with SCD.
Parents praised nurses, physicians, and staff who easily obtained a blood sample from their child or could “get it on one stick.” They preferred the Center staff over the emergency room and hospital staff. The Center was set up for patients with SCD and included an observation room. Parents’ unfamiliarity with the IV skills of nurses and physicians in the emergency room and hospital added to their stress. Parent 15 shared the problems her daughter experienced with having an IV started in the hospital.
Because it’s hard for them to get her blood. It takes a long time and it takes like 5 or 6 doctors to get her IV started because her veins, you can’t get her veins. Some of them I have problems with. Some of them talk smart. Some say, “We’ve got to do this.” I know they have to. It’s just the way they do it, because some do it messy. And it just irritates me how they do the blood.
Most distressing to parents were trips to the emergency room for painful crisis, childhood illnesses, and injuries. Waiting in the emergency room was stressful because parents were unable to follow through with directions they received at the Center to seek immediate medical attention when their child required such care. Parent 16 explained,
They (professionals at the Center) always said, “Whenever you go to the emergency room, tell them your baby is a sickle cell patient.” It didn’t do no good. We still set out there and waited. You still got to wait. One day my baby was throwing up and I told them that she was a sickle cell patient. So, we had to wait right back out (in the waiting room) until they get a room.
Parent 5 experienced problems with emergency care in rural areas where professionals had less experience with providing care for children with SCD.
Health insurance was a problem for Parent 8:
I had a negative experience one time at the doctor’s office. They had took my money to see him. I signed him up and I used co-pay and then I mentioned that he had sickle cell. They said, “We can’t even see him.”
Parent 2 explained, “My children were insurable and I signed him up and I got a letter like a couple of months ago. They said that they had to cancel his policy and (I should) reimburse them for every dime they paid.” Similarly, Parent 1 related, “Well, see, I had that same experience. My boy had been insured since he was 4 years old and then cancellation.”
School
Important areas for children with SCD at school were peer support and school staff having knowledge of SCD, following up on the child’s behaviors and symptoms during the school day, and making needed accommodations. Parents discussed the extent to which the child’s teachers, guidance counselors, and other students understood SCD and supported the child. Teachers were helpful to parents and the child with SCD when they possessed knowledge of SCD and recognized and followed up on certain child behaviors, signs, and symptoms. This follow up included contacting the parent to take the child home from school and giving the child a break from classroom activities.
Parents discussed accommodations for their child in classroom and extra-curricular activities. Parent 5 proudly stated that her 14 year old son “is now allowed to take water and extra fluid to class.” Parent 1 described her son’s football coach as understanding that her son “can’t get too hot or can’t get too cold … That’s one thing I liked about him.”
Students in the child’s school were not always a resource for the child. Some students supported the child with SCD, while other students teased, isolated, and treated the child differently. Parents praised the sickle cell educator’s efforts to inform students, teachers, and school staff about SCD. Parent 4 concluded,
Just try to inform, help the children to understand, the teachers to understand. Once we got the information to them, then they could understand it wasn’t something that could be helped and it wasn’t something that they could catch from him.
Employment
Parents discussed their difficulties and concerns about keeping a job; balancing work, childcare, and other responsibilities such as attending college; obtaining unemployment benefits, and the future employment of their child with SCD. Parents expressed gratitude for social workers who guided them to sources of financial assistance. Parent 3 described her employer as supportive and her employment as secure.
I’ve been blessed with my job. I work in a hospital. Once he (child with SCD) got sick, it was no problem. If I need a leave of absence, my job was always there. My boss always guaranteed that. You take care of your children because they’re first. So, my job was always secured.
Other parents described their employers as not understanding the demands of having a child with SCD. Parents who lost jobs because of absences due to their child’s health were hesitant to share information about their child with SCD with future employers. Parent 15 explained her dilemma.
But sometimes when you fill out an application, you really want to tell that you have a child with sickle cell. But it’s not really good because they won’t hire you because they need you there. Missing work, you know you need to tell them. But, in another way, it’s bad to tell them. Because they will be like, “Well, she’s going to be off and she is going to be another problem. She going to be coming around saying her child has to go to the hospital.
Parent 7 shortened her career in the military to take care of her son with SCD. She wondered if that decision may have strained her relationship with the sibling.
I done 14 years of military service. I couldn’t even get to 20 because my son was having so many problems… They (military supervisor) called me and wanted me to leave my son in the hospital to go to (military) school. I said, “No.” Basically, I just had to say, “Well, it’s not my time.” I had to put my child with sickle cell before me. I guess, some kind of way that’s how I lost my 16-year-old (sibling) because he’s saying that I’m not having a life.
Endogenous Factors
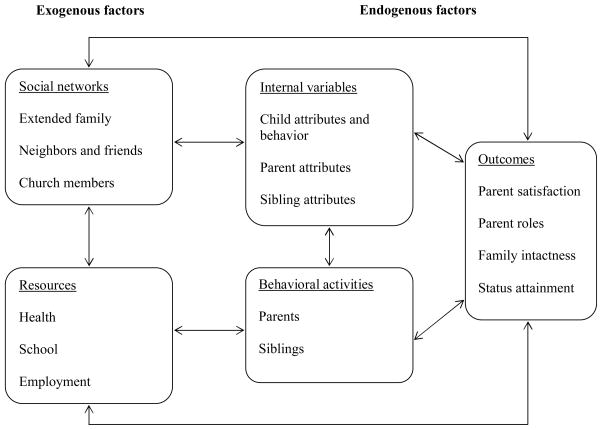
Parent discussion in the focus group interviews revealed three endogenous factors, internal variables, behavioral activities, and outcomes (Figure 1). As previously mentioned, understanding and examining endogenous factors and the links between them is important to the study of family communication (Fitzpatrick & Caughlin, 2002).
Figure 1.
Factors Influencing Parent Communication About Sickle Cell Disease
Internal Variables
Internal variables explain the patterns present in behavioral activities (Fitzpatrick & Caughlin, 2002). In this study, internal variables included the attributes of the child, parent, and sibling of the child with SCD and the behavior of the child with SCD. Attributes and behaviors of the child with SCD relate to and influence parent and sibling behaviors. Although parents were asked questions to elicit their views on their communication with siblings about SCD, most of their discussion was about their children with SCD and their own experiences as the parent of a child with SCD.
Child attributes and behavior
Parent descriptions of their children with SCD focused on pain, a sick child, a healthy-appearing child, depression, and immaturity. Some parents described their child as “always aching” and immobilized or unable to walk because of pain. Parent 5 described her child’s refusal to acknowledge his pain.
My 14 year old would get to the point where he actually sit up there be in pain because he doesn’t want to go to the hospital. He just sit up there, maybe go to the bathroom and take (oral pain) medicine and just sit up there and be in pain rather than saying, “Let’s go.”
Some parents viewed their child with SCD as a sick child because of visible signs of being sick and the need for frequent clinic visits and hospitalizations. Having a sick child was based on the child’s bed-wetting, chronic leg ulcers, crying, excessive thirst, fatigue, fever, frequent urination, inactivity, irritability, sleepiness, tired-looking, and yellow eyes.
Other parents described their child with SCD as healthy-appearing and in charge. Parent 1 noted, “But my son weighs 125 pounds and plays football. When you look at him, you would never think that he had sickle cell. He eats up everything and don’t turn down nothing.” Parent 14 described how her son paced himself. “He knows what his limits are. He stops himself. ‘I am at my limit now.’ It’s like an overload even in school with information. ‘I can’t take it anymore.’”
Parent 12 expressed concern about her daughter’s depression because her daughter “was homebound for about 3 months because she got to the point, straight A student, she wasn’t doing her work. She just got depressed.” Parent 7 was concerned about her son with SCD having “a lot of other issues besides sickle cell … He is getting older and he’s so immature.”
Parent attributes
Parents’ knowledge of SCD, their emotional response to having a child with SCD, and characteristics of their relationship with the child with SCD influenced their behavioral activities. Parents described themselves as being uneducated or undereducated about SCD, having difficulty explaining SCD, yet motivated to continue learning about SCD. Parent 15 pointed out, “I’m still learning because my daughter is young.” Parents described themselves as being scared and shocked over learning about their child’s diagnosis, isolated from others, misunderstood, and stressed. Several parents discussed the stress related to being the only decision maker and caregiver for their child. In their relationship with their child with SCD, parents portrayed themselves as attentive, caring, sensitive, and protective.
Sibling attributes
Siblings’ knowledge of SCD, relationship with the child with SCD, emotions, and caregiving traits contributed to sibling behavior. Siblings had varying levels of knowledge and awareness of SCD as shown by their curiosity, inquisitiveness, and interest. Parent 5 described the sibling as knowing “what it is but she don’t know what causes them (painful crises) when he has them.” Sibling relationships with the child with SCD were described as affectionate, close, concerned, empathetic, and loving. Some relationships were characterized by sibling jealousy of the parental attention given to the child with SCD. Sibling anger and unhappiness were attributed to SCD and the impact of SCD on the family. Parent 7 described the sibling: “So, my oldest son—he is really, really angry about it. He doesn’t like it all. Even though he is 16 (years old), it still bothers him.”
Behavioral Activities
Behavioral activities include parent and sibling activities that focused on the child with SCD and the family. These activities evolved from and were influenced by social networks; available and accessible resources; child, parent, sibling attributes; and child behavior. These activities reflect parent and sibling commitment to the child with SCD and their family, parent commitment to their responsibilities as parents of children with SCD, and sibling desire to learn and be involved with their brother or sister with SCD.
Parents
Parents were committed to their responsibility of taking care of their child with SCD and the siblings. To meet this responsibility, parents educated themselves about SCD, applied information about SCD to prevent and treat problems, managed their household and family while managing the care of their child, advocated for the child, educated their child with SCD to advocate for themselves, involved or excluded siblings in the care of the child, and prayed for the child’s well-being. Parent 14 related,
After I learned about sickle cell, because I didn’t really understand, I told my two daughters. I told them what I learned … We learned, we took the information, the information about fever, what to do, the signs to watch for, the weather, how they dehydrate in the summer and winter with the temperature drop like today and yesterday. We put those preventive and we work with them. We were on top of it, staying on top.
Parents provided care to their child with SCD and decided how much to involve the siblings in the care of the child. Some parents provided siblings with opportunities to learn about SCD by including them on visits to the clinic and hospital. Several parents used sibling age to determine when to begin sharing information about SCD with the sibling. Most agreed that they could begin explaining SCD to siblings when siblings reach the age of eight years. Parent 5 suggested,
Maybe a little younger than eight. Eight and up for exactly explaining to them about the sickle cell and the shape but they are already seeing it from a baby until eight years old. What do you tell them in the meantime? Nothing.
Parents advocated for their child in the child’s school, with friends and neighbors, and at church. Advocacy involved educating others about SCD and the relationship between the child’s behavior and SCD. Parents taught the child to advocate for themselves, with the goal of the child moving toward increased independence. Parent 10 described her efforts to promote her son’s independence.
So you talk to them and help them to understand. The main thing is that he is 13. He helps himself. You ask him, “What should you do when things start to happen?” to make sure he knows. We are trying to train him to take care of himself as an adult. “Keeping information with you” because he’ll need it until he gets the hang of taking care of himself. And he can let other people know, too. Because people don’t really understand it unless they are around when something happens --- but if he gives them the information to help educate them, and then everybody can help.
Siblings
Parents described sibling behaviors that reflected sibling knowledge of SCD, sibling relationship with the parent and the child with SCD, emotional responses, and other caregiving traits. Siblings learned about SCD by observing the child at home, accompanying the child to clinic appointments, spending time with the child in the hospital, playing a computer game about SCD, spending time with relatives (i.e., cousins and grandparents) with SCD, and asking questions. Parent 15 related that the oldest sibling “knows a lot because she was in the hospital with her a lot when she was little. I had both of them and she would just sit there and look. She learned just by sitting there watching.”
Parent 2 described sibling jealousy and desire for parent attention. “She (sibling) sees me holding him or hugging him or he’s not feeling well, she says, ‘You don’t love me,’ or she says, ‘You love him more than you love me. Why don’t you love me?’ ” Parent 15 described her seven year old son as “always jealous… He’ll tell me, ‘Why do you always baby (child with SCD) and do this for her?’”
Even though siblings were described as jealous of the attention given to the child with SCD, some sibling behavior toward the child with SCD was positive and reflected a typical sibling relationship. Parent 14 described the relationship between her son with SCD and an older sibling as “just normal … They argue. They do it in a teasing kind of way, aggravating kind of way. They always end up laughing.”
Siblings were helpful and took responsibility to help the child with SCD. Siblings suggested ways to treat the child with SCD (e.g., placing the child in hot water) and intervened on behalf of their brother or sister with SCD. Parent 2 recalled,
One day, my son had a crisis. He couldn’t move. I was in a deep sleep because I work on the graveyard shift. My four-year-old daughter came in and woke me up. She said, “Momma, he won’t play. He’s crying.” So, I got up and found him with a swollen foot, in pain, and unable to move his foot… It was good that my daughter was there because there is no telling what would have happened.
Siblings promoted independence by encouraging the child’s participation in activities and by having the same expectations for the child with SCD and other siblings without SCD.
Outcomes
Outcomes identified by parents in this study include parent satisfaction, parent roles, family intactness, and status attainment. As noted by Fitzpatrick and Caughlin (2002), outcomes are based on values and assumptions about these values. The outcomes discussed here reflect parent views of themselves, their children, their families, and communities and reflect, to some extent, their values and assumptions about their values.
Parent satisfaction
In the context of the nuclear family, the health of the child with SCD, parent knowledge of SCD, and sibling behavior contributed to parent satisfaction. When the context was broadened to include the extended family, those extended family members who were knowledgeable about and understood SCD were more supportive of the child and family and contributed to parent satisfaction.
Parent roles
Participants discussed their roles as parents and heads of households. They spoke seriously about their roles as parents of children with SCD and their unaffected siblings. They described themselves as learning about SCD, teaching others about SCD, advocating for their child with SCD, and training their child with SCD to be independent. Parents were the heads of households and primary decision makers for their children. Mothers who were single parents described varying degrees of assistance and support from their children’s father and other family members.
Family intactness
Paternal involvement ranged from frequent contacts with the child and family to denying being the child’s father. Similarly, some extended family members were very involved with the child with SCD and the nuclear family, while other extended family members refused to be involved or to acknowledge the child was part of their family.
Status attainment
Parents were concerned about whether the child with SCD would reach an equal or higher socioeconomic status than they did. Parent 14 was concerned that her son and daughter with SCD would not attain a socioeconomic status equal to or higher than her own. She described the problems her 25-year-old daughter with SCD had keeping a job, “As soon as they (employer) discover that she has sickle cell and cannot attend work on a normal basis, she lost her job.” As a result of this experience, she had concerns about the future employment of her 16-year-old son with SCD and encouraged him to become “an entrepreneur, to have his own company. He does lawn service now.”
Discussion
The purpose of this study was to explore parent-sibling communication in families of children with SCD by identifying and examining factors within and outside the parent-sibling dyad that influence parent-sibling communication. Parents recognized the shift in attention toward the child with SCD and siblings’ desire to be involved and understand SCD. Parents were sometimes frustrated with the questions siblings posed about SCD, yet they provided or attempted to provide information about SCD to siblings who asked questions. Siblings were thought to be ready to learn about SCD when they reached the age of eight years. Parents structured learning opportunities for siblings by allowing them to attend clinic with the child and make hospital visits. Some parents expected siblings to learn by observing activities in the clinic or hospital and others thought siblings would learn by spending time with relatives who have SCD. Some parents initiated communication about SCD with siblings to share new information with siblings after returning from a clinic or hospital visit. They shared information, sometimes detailed information, about the inheritance pattern of SCD, the physiology of a painful crisis, and the child’s overall status.
Use of Fitzpatrick and Caughlin’s (2002) taxonomy revealed the important influence of exogenous factors on communication within the families represented by the study participants. Fitzpatrick and Caughlin’s claim that “communication is central to understanding connections” (p. 759) is supported when the variables in Figure 1 are considered within the context of the African American family. Parent reflections on and discussion about their communication about SCD with siblings and family members revealed a broad context in which this communication occurred. This context included social networks, available and accessible resources, and attributes and behaviors of the child with SCD. Underlying much of the discussion about extended family, neighbors and friends, church members, health professionals, school staff, and employers was the need for these persons to be knowledgeable about and understand SCD. Parents learned about SCD to take care of their child, to educate others about the child’s needs, and assure that health professionals and school staff were properly addressing their child’s needs. Parents’ efforts to educate family members about SCD support the view that roles within African American families tend to be egalitarian and flexible (Hines & Boyd-Franklin, 2005). This sharing of roles and responsibilities between parents, with grandparents, and other adult relatives can be viewed as a strength for handling crises (Boyd-Franklin, 1989).
The support provided by church members and the positive view of the church is consistent with Hill’s (1972) view that the Black church supports and sustains families who face adversity through mutual caring, shared responsibility, and faith. The strong dependence on the church was shown by one parent who expressed her frustration with a church which included her own extended family members and successfully transitioned to a different church.
The hope or expectation of African American parents that their children will surpass them socioeconomically (Boyd-Franklin, 1989) was evident in Parent 14’s desire that her son and daughter would be employed and reach a socioeconomic status that exceed her and her husband’s status. African American parents promote the value of education and hard work by teaching their children to share in family responsibilities that involve them in household tasks and child care (Barnes, 1989; Kane, 2000). Parents’ encouragement of children with SCD to manage their own care as early as possible and involvement of siblings in the care of the child with SCD is consistent with reports by Hines and Boyd-Franklin (2005) and Kane (2000) that children should share in family responsibilities. According to Lewis (1972), African American children are viewed as powerful, self-willed, and active participants in the context in which they live. Teaching children to accept responsibility and training children in coping skills would contribute to personal autonomy (Boyd-Franklin, 1989; Hill, 1972).
Future research could explore differences in family experiences and factors that contribute to these differences. For example, Wilson (1987) proposed that African American families who have greater exposure to families that accept divisions between nuclear and extended families may be associated with families with a higher socioeconomic status. Obtaining information about socioeconomic status may have explained some differences in family experiences. Boyd-Franklin (1989) found that changes in socioeconomic status do not dilute family ties and connection. Stewart (2007) showed that the strength and vitality of the extended family continue to be important in the lives of African Americans regardless of socioeconomic status.
Sibling perceptions of parent-sibling communication and the experience of having a brother or sister with SCD are indicated to identify those siblings in need of additional support from parents and extended family members and possibly from mental health professionals. Poorer sibling adjustment was associated with the number of emergency room visits made by the child with SCD (Gold et al., 2008). Sibling distress was associated with visits to the emergency room which included family separations, disruptions that focus on the child with SCD, and possible death of the child with SCD. Similarly, the number of visits to the emergency room was associated with behavior problems in the child with SCD such as withdrawal, anxiety, depression, and aggression. Research that explores the sibling perspective of distress related to clinic and hospital visits by the child with SCD, parent-sibling communication, and the experience of having a brother or sister with SCD is indicated. Developmental level of the sibling and the relationship with parent, sibling, and family stress should also be explored. Barakat, Patterson, Tarazi, and Ely (2007) found significantly more parenting stress was associated with disease-related communication among parents of adolescents with SCD than among parents of preschoolers.
Based on these findings, parents could benefit from education on and modeling of strategies to educate children and adults about SCD. Learning ways to impart information about SCD to others could occur as parents learn new information about SCD. Education of other members of the nuclear family (i.e., siblings) and education of extended family members by health professionals working with children with SCD could reinforce the importance of prevention and treatment of complications and offer a level of support to parents who have multiple roles in these families.
Contributor Information
J. Carolyn Graff, University of Tennessee Health Science Center, College of Nursing and Boling, Center for Developmental Disabilities, Memphis, TN, USA.
Jane S. Hankins, St. Jude Children’s Research Hospital, Department of Hematology, Memphis, TN, USA.
Belinda T. Hardy, University of Tennessee Health Science Center, Boling Center for Developmental Disabilities, Memphis, TN, USA
Heather R. Hall, University of South Alabama, College of Nursing, Mobile, AL, USA.
Ruth J. Roberts, University of Tennessee Health Science Center, Boling Center for Developmental Disabilities, Memphis, TN, USA.
Susan L. Neely-Barnes, University of Tennessee, College of Social Work, Nashville, TN, USA.
References
- Ashley-Koch A, Yang Q, Olney RS. Sickle hemoglobin (HbS) allele and sickle cell disease: A HuGE review. American Journal of Epidemiology. 2000;151:839–845. doi: 10.1093/oxfordjournals.aje.a010288. [DOI] [PubMed] [Google Scholar]
- Barakat LP, Patterson CA, Tarazi RA, Ely E. Disease-related parenting stress in two sickle cell disease caregiver samples: Preschool and adolescent. Families, Systems, & Health. 2007;25:147–161. [Google Scholar]
- Barnes AS. The Black middle class family. Bristol, IN: Wyndham Hall; 1989. [Google Scholar]
- Boyd-Franklin N. Five key factors in the treatment of Black families. In: Saba SW, Karrer BM, Hardy KV, editors. Minorities in family therapy. New York, NY: Haworth; 1989. pp. 53–69. [Google Scholar]
- Denzin NK, Lincoln YS. Handbook of qualitative research. 3. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- Fanos JH, Davis J, Puck JM. Sib understanding of genetics and attitudes towards carrier testing for x-linked severe combined immunodeficiency. American Journal of Medical Genetics. 2001;98:46–56. [PubMed] [Google Scholar]
- Fitzpatrick MA, Caughlin JP. Interpersonal communication in family relationships. In: Knapp ML, Daly JA, editors. Handbook of interpersonal communication. Vol. 3. Thousand Oaks, CA: Sage; 2002. pp. 726–777. [Google Scholar]
- Giallo R, Gavidia-Payne S. Child, parent and family factors as predictors of adjustment for siblings of children with a disability. Journal of Intellectual Disability Research. 2006;50:937–948. doi: 10.1111/j.1365-2788.2006.00928.x. [DOI] [PubMed] [Google Scholar]
- Gold JI, Treadwell M, Weissman L, Vichinsky E. An expanded Transactional Stress and Coping Model for siblings of children with sickle cell disease: Family functioning and sibling coping, self-efficacy and perceived social support. Child: Care, health and development. 2008;34:491–502. doi: 10.1111/j.1365-2214.2008.00810.x. [DOI] [PubMed] [Google Scholar]
- Hill R. The strengths of Black families. New York, NY: Emerson-Hall; 1972. [Google Scholar]
- Hines PM, Boyd-Franklin N. African American families. In: McGoldrick M, Giordano J, Garcia-Preto N, editors. Ethnicity and family therapy. New York, NY: Guilford; 1982. pp. 87–100. [Google Scholar]
- Horsely H, Patterson T. The effects of a parent guidance intervention on communication among adolescents who have experienced the sudden death of a sibling. The American Journal of Family Therapy. 2006;34:119–137. [Google Scholar]
- Kane CM. African American family dynamics as perceived by family members. Journal of Black Studies. 2000;30:691–702. [Google Scholar]
- Krueger RA, Casey MA. Focus groups: A practical guide for applied research. 3. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Lerner NB, Platania BL, LaBella S. Newborn sickle cell screening in a region of Western New York State. The Journal of Pediatrics. 2009;154(1):121–125. doi: 10.1016/j.jpeds.2008.06.039. [DOI] [PubMed] [Google Scholar]
- Lewis D. The Black family: Socialization and sex roles. Phylon. 1972;2:221–237. [Google Scholar]
- Miller ST, Macklin EA, Pegelow CH, Kinney TR, Sleeper LA, Bello JA, et al. Silent infarction as a risk for over stroke in children with sickle cell anemia: A report from the Cooperative Study of Sickle Cell Disease. Journal of Pediatrics. 2001;139(3):385–390. doi: 10.1067/mpd.2001.117580. [DOI] [PubMed] [Google Scholar]
- Morgan DL. Focus groups as qualitative research. 2. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- National Heart, Lung, and Blood Institute. NIH Publication No. 02-2117. Bethesda, MD: Author; 2002. The management of sickle cell disease. Retrieved November 14, 2009 from http://www.nhlbi.nih.gov/health/prof/blood/sickle/sc_mngt.pdf. [Google Scholar]
- Pearson HA, Spencer RP, Cornelius EA. Functional asplenia in sickle-cell anemia. New England Journal of Medicine. 1969;281:923–926. doi: 10.1056/NEJM196910232811703. [DOI] [PubMed] [Google Scholar]
- Pit-ten Cate IM, Loots GMP. Experiences of siblings of children with physical disabilities: An empirical investigation. Disability and Rehabilitation. 2000;22:399–408. doi: 10.1080/096382800406013. [DOI] [PubMed] [Google Scholar]
- QSR International. NVivo7. [Computer software] 2007 Retrieved from http://www.qsrinternational.com/default.aspx.
- Schatz J, Brown RT, Pascual JM, Hsu L, DeBaun MR. Poor school and cognitive functioning with silent cerebral infarcts and sickle cell disease. Neurology. 2001;56:1109–1111. doi: 10.1212/wnl.56.8.1109. [DOI] [PubMed] [Google Scholar]
- Serjeant GR, Serjeant BE. The spleen. In: Serjeant GR, Serjeant BE, editors. Sickle Cell Disease. New York, NY: Oxford University Press; 2001. pp. 149–169. [Google Scholar]
- Smith JA. Evolving issues for qualitative psychology. In: Richardson JTE, editor. Handbook of qualitative research methods for psychology and the social sciences. Malden, MA: BPS Blackwell; 1996. pp. 189–201. [Google Scholar]
- Stewart P. Who is kin? Family definition and African American families. Journal of Human Behavior in the Social Environment. 2007;15:163–181. [Google Scholar]
- Vichinsky E, Lubin BH. Suggested guidelines for the treatment of children with sickle cell anemia. Hematology/Oncology Clinics of North America. 1987;1(3):483–501. [PubMed] [Google Scholar]
- Wilson WJ. The truly disadvantaged: The inner city underclass and public policy. Chicago, IL: University of Chicago; 1987. [Google Scholar]