Abstract
There is increasingly evidence that the interactions between vitamin D, fibroblast growth factor 23 (FGF-23), and klotho form an endocrine axis for calcium and phosphate metabolism, and derangement of this axis contributes to the progression of renal disease. Several recent studies also demonstrate negative regulation of the renin gene by vitamin D. In chronic kidney disease (CKD), low levels of calcitriol, due to the loss of 1-alpha hydroxylase, increase renal renin production. Activation of the renin-angiotensin-aldosterone system (RAAS), in turn, reduces renal expression of klotho, a crucial factor for proper FGF-23 signaling. The resulting high FGF-23 levels suppress 1-alpha hydroxylase, further lowering calcitriol. This feedback loop results in vitamin D deficiency, RAAS activation, high FGF-23 levels, and renal klotho deficiency, all of which associate with progression of renal damage. Here we examine current evidence for an interaction between the RAAS and the vitamin D-FGF-23-klotho axis as well as its possible implications for progression of CKD.
The renin-angiotensin-aldosterone system (RAAS) plays a pivotal role in renal progression and its complications. Accordingly, RAAS blockade has been the cornerstone of renoprotective interventions. Vitamin D deficiency is traditionally recognized as a key factor in the bone and mineral disturbances of chronic kidney disease (CKD), and vitamin D supplementation is standard treatment for many renal patients. As reviewed elsewhere,1 vitamin D interacts with the more recently identified moieties, fibroblast growth factor 23 (FGF-23) and klotho. As such, vitamin D, FGF-23, and klotho represent an endocrine axis involved in the regulation of calcium and phosphate metabolism.
Besides having effects on mineral metabolism, vitamin D deficiency is also associated with progressive renal disease and with mortality in chronic kidney disease (CKD).2,3 In line with these observations, the use of vitamin D analogues may provide with a survival advantage in dialysis patients,4 and preclinical and clinical data indicate that vitamin D analogues have additional renoprotective effects in addition to RAAS blockade,5–8 supporting their clinical relevance. Multiple mechanisms are likely involved in the protective effects of vitamin D, including autocrine anti-inflammatory and antifibrotic effects, as well as a suppressive effect on the RAAS. Several lines of evidence support the impact of vitamin D on RAAS activity at the clinical, pathophysiological, and molecular level. The other way round, RAAS activity influences the vitamin D-FGF-23-klotho axis. Recent studies show that angiotensin II reduces renal expression of klotho, which, in turn, modulates FGF-23-signaling and 1-alpha hydroxylase, the enzyme converting calcidiol to calcitriol. As derangement of the vitamin D-FGF-23-klotho axis associates with cardiovascular complications in several studies, the interactions of this axis with the RAAS may have therapeutic implications in CKD patients, regarding both renal and cardiovascular outcomes.
MODULATION OF THE RAAS BY VITAMIN D
The first clinical studies suggesting an inverse relationship between calcitriol and renin levels were published two decades ago9,10 and were recently confirmed in a large cohort study.11 Vitamin D deficiency, defined as calcidiol levels below 15 ng/ml, associates with reduced renal plasma flow responses to infused angiotensin II, suggesting endogenous intrarenal RAAS activation in vitamin D deficient subjects,12 and intervention with calcitriol decreases plasma renin and angiotensin II levels in hemodialysis patients with secondary hyperparathyroidism.13
Several mechanistic studies confirming negative regulation of the renin gene by calcitriol have been published by the group of Li et al., who demonstrated increased renin gene expression in kidneys of vitamin D receptor (VDR) null mice, accompanied by increased plasma angiotensin II levels, hypertension, and cardiac hypertrophy.14 In wild-type mice, conversely, treatment with calcitriol reduces renal renin production. The negative regulation of renin by calcitriol seems independent of calcium and PTH.15 On a molecular level, calcitriol binds to the VDR and subsequently blocks formation of the CRE-CREB-CBP complexes in the promoter region of the renin gene, reducing its level of expression.16
Together, the associations found in clinical studies and the supporting mechanistic studies make it plausible that vitamin D deficiency could indeed contribute to an inappropriately activated RAAS, as a mechanism for progression of CKD and/or cardiovascular disease. This may well be relevant for therapeutic purposes. Pharmacologic blockade of the RAAS is the main therapeutic modality in CKD, and, despite its proven efficacy, renoprotection is usually far from complete.17 Several lines of evidence indicate that persistent RAAS-activity, either by incomplete pharmacologic blockade or related to the reactive rise in renin during therapy, can hamper its therapeutic efficacy. This is suggested by the added antiproteinuric effect of renin inhibition to AT1 receptor blockade.18 These findings hypothesize that treatment with a vitamin D receptor agonist, on top of conventional RAAS-blockade, would give additional renoprotection through its negative regulation of renin.
In line with this notion, several experimental studies confirm that the renoprotective effects of vitamin D are mediated at least in part through the suppression of renal renin expression.5,7 In a recent randomized controlled trial, paricalcitol given in addition to RAAS blockade further reduces albuminuria compared with RAAS blockade alone in patients with diabetic nephropathy, although it remains unclear whether this therapeutic benefit was obtained by an effect on renal renin activity.19 Vitamin D analogues may also have cardioprotective effects in association with suppression of renin in the kidney and heart.20,21 Whether paricalcitol reduces left ventricular hypertrophy in stage III/IV CKD patients is currently under investigation in the PRIMO study (ClinicalTrials.gov Identifier: NCT00497146).
Interactions between vitamin D and other RAAS components have been studied as well. Aldosterone acts through the mineralocorticoid receptor, which belongs to the same superfamily of nuclear receptors as the VDR. Therefore, cross talk between these receptors and their agonists could potentially exist, but this has not been studied so far. Mice that are genetically deficient for klotho, a protein associated with downregulation of 1-alpha hydroxylase and, thus, limited production of calcitriol, show excessive levels of calcitriol but also hyperaldosteronism, which is similarly reversed by a vitamin D-deficient diet.22 Although these findings suggest a possible interaction between vitamin D and aldosterone synthesis, it is uncertain whether hyperaldosteronism is a direct consequence of hypervitaminosis D. Data from in vitro studies do not support positive regulation of aldosterone synthesis by vitamin D, as treatment of cultured adrenocortical cells with calcitriol reduce aldosterone levels.23 In VDR null mice, although there seems to be a trend toward increased aldosterone levels, the elevation is not significant as compared with wild-type mice,24 which is in contrast with the strong downregulation of renal renin,5 suggesting that the effect on aldosterone may in fact be through renin. Treatment of spontaneous hypertensive rats (SHR) with cholecalciferol also reduces plasma aldosterone levels, but here, also, a direct suppressive effect on renin transcription cannot be excluded.25 Vice versa, aldosterone may potentiate the effects of calcitriol, as demonstrated in cultured renal thick ascending limb cells.26 In this study, calcitriol negatively regulates HCO3− absorption in the rat medullary thick ascending limb, which may contribute to net urine acid and/or calcium excretion. Addition of aldosterone potentiated the effects of calcitriol through an ERK-dependent, nongenomic pathway. This implicates that cross talk between the mineralocorticoid receptor and VDR may indeed be present, and requires further study.
Whether vitamin D modulates the expression of angiotensin II receptors is unknown. The only study on this subject reports that in adipocytes, vitamin D downregulates expression of the AT1 receptor in a dose-dependent manner,27 but, to our knowledge, these findings have never been replicated in other cell types.
In conclusion, both clinical and mechanistic studies suggest that calcitriol, through the VDR, has a negative regulatory role on renin gene transcription. Whether vitamin D also interacts with other RAAS components is unclear. Correcting vitamin D deficiency may have renal and cardioprotective effects, at least in part, through suppression of the RAAS. The direct suppressive effect of calcitriol on the renin gene raises the question whether a feedback loop exists, that is, if the RAAS also influences vitamin D metabolism. Recent data suggest that indeed activation of vitamin D, through klotho and 1-alpha hydroxylase, could be affected by angiotensin II.
POSSIBLE EFFECTS OF THE RAAS ON KLOTHO, FGF-23, AND VITAMIN D
The possible regulation of vitamin D metabolism by the RAAS is less well defined than the opposite regulation of the renin gene by calcitriol. Although there is no evidence that any RAAS component directly influences the enzyme 1-alpha hydroxylase or VDR, indirect effects of angiotensin II on 1-alpha hydroxylase, through klotho and FGF-23, may play a role.
Negative Regulation of Klotho by Angiotensin II
Accumulating data suggests that angiotensin II negatively regulates the renal expression of klotho.28–31 In an animal model, Mitani et al. demonstrated downregulation of renal klotho expression in response to angiotensin II infusion. Klotho downregulation also followed infusion of angiotensin II in a nonpressor dose.28 The downregulation of klotho was angiotensin II type 1 (AT1) receptor-dependent, since it was completely abolished by losartan and not by hydralazine. Intriguingly, subsequent restoration of klotho abundance in the kidney by gene transfer improved angiotensin II-induced proteinuria, suggesting that nonpressor-driven angiotensin II-induced proteinuria, at least in part, depends on loss of klotho.
In cultured tubular epithelial cells, angiotensin II-induced AT1-receptor-mediated downregulation of klotho was confirmed.29 In a recent elegant study, Yoon et al. demonstrated, in a mouse model, that salt restriction, a well-known RAAS-activating intervention, reduced klotho expression, which was reversed by losartan.30 The same study revealed that cyclosporin-induced damage associates with downregulation of renal klotho in association with upregulation of renal RAAS activation; addition of losartan completely prevented the loss of klotho expression.30
Several other animal models characterized by an activated RAAS, including SHR, noninsulin-dependent diabetic nephropathy (Otsuka Long-Evans Tokushima Fatty rats), and 5/6 nephrectomy, all demonstrate downregulation of renal klotho.32 The fact that renal klotho expression is also reduced in the DOCA salt rat model, characterized by RAAS suppression and renal damage, also suggests that other factors, such as tubular injury, contribute to downregulation of klotho in renal damage. Studies in patients suggest reduced renal klotho expression per nephron in kidney sections from CKD patients, as compared with control kidneys, but whether this is associated with RAAS activation is unclear.33 Interestingly, calcitriol has been shown to enhance renal klotho expression in vivo,34 possibly as a consequence of reduced RAAS activation.
Mechanisms of Klotho Downregulation
The mechanisms of klotho downregulation by angiotensin II are incompletely understood. Although direct negative regulation through the AT1 receptor is possible, other factors, such as oxidative stress, may contribute. Like angiotensin II, oxidative stress itself can cause downregulation of renal klotho.31,35 Subsequent administration of a free-radical scavenger prevented klotho downregulation induced not only by oxidative stress but also by infusion of angiotensin.31 It is well established that angiotensin II influences oxidative stress through the NADPH oxidase system.36–38 Conversely, inhibitors of the RAAS ameliorate the production of reactive oxygen species,39 which could, at least in part, explain the effects of RAAS inhibitors on klotho expression.
Interestingly, TNF alpha converting enzyme (TACE or ADAM17), which is upregulated in the presence of vitamin D deficiency,40 may be involved in cleavage of the extracellular domain of klotho.41 Moreover, angiotensin II itself also upregulates TACE,42 providing another mechanism for klotho downregulation. It may be through this mechanism that even distant inflammation downregulates renal klotho.43 These preliminary data suggest that klotho function could be affected by vitamin D deficiency through proteolytic activity of TACE, especially under inflammatory conditions.
Consequences of Downregulated Klotho and FGF-23 Resistance
The klotho gene encodes two proteins from five exons: membrane bound klotho (mKlotho; molecular weight 130 kD) and secreted klotho (sKlotho; 80 kD), which is a product of alternative splicing.44,45 A third form of klotho, a cleavage product of the extracellular domain of mKlotho, is referred to as cut-Klotho (cKlotho).45 Although, under physiologic conditions, the klotho gene is expressed only in selected tissues, including distal tubular segments of the kidney, klotho null mice have the phenotype of generalized aging.46 A recent study demonstrated that klotho deficiency causes vascular calcification in CKD.47 The similarity between klotho and FGF-23 mice led to the discovery that klotho is mandatory for FGF-23 signaling by modification of the low-affinity FGF receptor (FGFR1), leading to the high-affinity receptor that comprises the membrane-bound FGFR1/klotho complex.48,49 Only mKlotho, and not one of the circulating forms, can form an FGF-23 receptor from FGFR1.50
As a consequence of klotho downregulation, the high-affinity FGFR1/klotho complex is reduced, inducing FGF-23-resistance. Thus, by its effect on klotho, angiotensin II could theoretically be involved in induction of FGF-23 resistance. In CKD, FGF-23 resistance abates fractional excretion of phosphate, leading to further hyperphosphatemia and thus providing another trigger for FGF-23 release.51 As a consequence of high FGF-23 levels, vitamin D activation is suppressed. Administration of recombinant FGF-23 to normal mice reduces renal expression of 1-alpha hydroxylase and increases renal CYP24A1, resulting in low calcitriol levels;52 this effect is mediated by extracellular signal-regulated kinase (ERK).53 Both FGF-23 and klotho null mice display increased expression of 1-alpha hydroxylase.54,55 This suggests that klotho, in concert with FGF-23, participates in an inhibitory feedback loop that results in the suppression of calcitriol synthesis.34 High levels of FGF-23 suppress activation of vitamin D and are associated with progression of CKD,56 left ventricular mass and geometry,57,58 atherosclerosis,59 and mortality in dialysis patients.60 Clinical data suggest that the mechanisms underlying the association between FGF-23 and vascular complications are multiple, including suppression of vitamin D activation, reduced fetuin-A levels, and endothelial dysfunction, partially through asymmetrical dimethyl arginine (ADMA).61 Moreover, higher FGF23 is associated with proteinuria throughout several ranges of CKD,61 independently of levels of active vitamin D.62
Besides its role as part of the FGF-23 receptor complex, the β-glucuronidase activity of klotho is important in stabilizing the abundance of the TRPV5 in the apical membrane of tubular cells.55,63 Loss of renal klotho in CKD33 may thus lead to renal calcium loss, providing another impulse for vitamin D activation. In addition, overexpression of klotho provides renoprotection in mouse64 and rat65 models of renal damage, suggesting that renal loss of klotho, as observed in CKD, may result in renal damage.
Finally, klotho appears to have distant effects, especially on the vasculature. Although it is possible that the originally described phenotype of premature aging in klotho-deficient mice46 is the consequence of disturbed regulation of calcium, phosphate, and vitamin D metabolism in the kidney, several recent reports suggests that klotho has specific functions at distant tissues. Klotho, for example, protects endothelial cells against oxidative-stress induced apoptosis.66,67 An elegant study demonstrated that klotho-deficient mice have endothelial dysfunction, which could be restored by parabiosis with wild-type mice, suggesting that klotho might be involved in nitric oxide synthesis.68 At least part of the beneficial effects of klotho may be mediated by inhibition of insulin/IGF-1 signaling, thereby improving resistance against oxidative stress.69 Recently it was shown that klotho modulates intracellular calcium handling in endothelial cells through the VEGF receptor and TRPC-1, and thus protects these cells from loss of integrity through apoptosis.70 The resemblance of the abovementioned observations with the effects of RAAS activation suggests that a part of the clinical picture as observed in a state of RAAS activation in CKD might in fact be due to klotho deficiency.
CAN THE VITAMIN D-FGF-23-KLOTHO AXIS BE MONITORED AND TARGETED?
The data summarized here suggest a relationship between RAAS activation, low renal klotho levels, and high FGF-23 levels in CKD patients, all of which associate with adverse outcomes. Future studies are needed to address whether adequate renal klotho, as measured, for instance, by fractional phosphate excretion, vitamin D, or FGF23 levels, (possibly) circulating klotho, or a combination of these factors, could be a therapeutic target. Targeting klotho deficiency in CKD, which could be achieved by optimizing RAAS blockade and correction of vitamin D deficiency, may further reduce cardiovascular disease and progression of kidney injury.
Conclusions
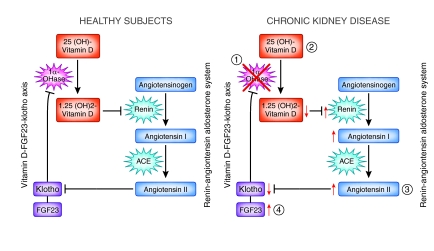
Emerging evidence demonstrates the negative regulation of the RAAS by calcitriol, providing renoprotective effects of vitamin D analogues in addition to RAAS blockade in CKD. A growing number of studies support suppression of 1-alpha hydroxylase by angiotensin II through renal downregulation of klotho and subsequent FGF-23 resistance (summarized in Figure 1, left panel). Besides its effects on vitamin D metabolism, high levels of FGF-23 or FGF-23 resistance, due to klotho deficiency, are associated with endothelial dysfunction, cardiovascular morbidity and mortality, and progression of CKD.71 In CKD, loss of capacity for excreting phosphate by reduced nephron mass and loss of klotho due to RAAS activation and tubulointerstitial damage both further enhance circulating levels of FGF-23 and reduce levels of active vitamin D (Figure 1, right panel). Further derangement of these interconnected axes may well contribute to the cardiovascular complications of CKD.
Figure 1.
Cross talk between vitamin D (red), FGF-23-Klotho (yellow), and the RAAS (blue) in healthy subjects and patients with chronic kidney disease. In the normal situation (left panel), active vitamin D (1,25(OH)2 vitamin D), generated by renal 1-alpha hydroxylase, suppresses renal renin production. When the RAAS is not activated (low angiotensin II), renal klotho levels are sufficient to allow normal function of the FGF-23 receptor. Therefore, levels of FGF-23, a negative regulator of 1-alpha hydroxylase, are normal under these conditions. In chronic kidney disease (right panel), the RAAS, vitamin D, FGF-23 and klotho are concertedly disturbed. (1) Activity of 1α-hydroxylase is reduced due to nephron loss and high FGF-23 in CKD, leading to (2) reduced production of 1,25(OH)2-vitamin D, which in turn upregulates renal renin production. (3) The subsequent higher levels of angiotensin II cause renal klotho loss and (4) disrupted FGF-23 signaling, impairing phosphaturia and rising FGF-23 levels. RAAS activation, vitamin D deficiency, high FGF-23 levels and low renal klotho have all been associated with adverse renal outcome in CKD.
RAAS inhibition and supplementation of vitamin D deficiency are well-established interventions for prevention of progressive renal function loss and its extrarenal complications, as recommended by current guidelines72 (http://www.nice.org.uk/cg73). Interestingly, these interventions appear to share a part of their beneficial effects by interrupting the vicious cycle of increasing FGF23 resistance due to klotho deficiency. However, the protection against renal progression and its extrarenal complications by current therapy is far from complete, prompting for improvement of treatment strategies. Currently, management of blood pressure and proteinuria by RAAS blockade and vitamin D supplementation are independent components of the treatment regimen. Their separate and combined impact on the FGF-23-klotho axis is not monitored, nor is it a treatment target. It would be attractive to hypothesize that targeting optimization of this axis, particularly optimal levels of renal klotho, could enhance therapeutic efficacy, either by adapting titration strategies for currently available drugs or by novel agents.
Disclosures
Dr. De Borst is supported by personal development grants from the Dutch Kidney foundation (KJPB.08.07) and the University Medical Center Groningen (Mandema stipend), and by the European Union (FP7, Systems Biology towards Novel Chronic Kidney Disease Diagnosis and Treatment Project consortium [SysKid], project number 241544).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1. Razzaque MS: The FGF23-klotho axis: Endocrine regulation of phosphate homeostasis. Nat Rev Endocrinol 5: 611–619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Melamed ML, Astor B, Michos ED, Hostetter TH, Powe NR, Muntner P: 25-hydroxyvitamin D levels, race, and the progression of kidney disease. J Am Soc Nephrol 20: 2631–2639, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, Steele D, Chang Y, Camargo CA, Jr, Tonelli M, Thadhani R: Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int 72: 1004–1013, 2007 [DOI] [PubMed] [Google Scholar]
- 4. Teng M, Wolf M, Lowrie E, Ofsthun N, Lazarus JM, Thadhani R: Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med 349: 446–456, 2003 [DOI] [PubMed] [Google Scholar]
- 5. Zhang Y, Kong J, Deb DK, Chang A, Li YC: Vitamin D receptor attenuates renal fibrosis by suppressing the renin-angiotensin system. J Am Soc Nephrol 21: 966–973, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Y, Deb DK, Kong J, Ning G, Wang Y, Li G, Chen Y, Zhang Z, Strugnell S, Sabbagh Y, Arbeeny C, Li YC: Long-term therapeutic effect of vitamin D analog doxercalciferol on diabetic nephropathy: Strong synergism with AT1 receptor antagonist. Am J Physiol Renal Physiol 297: F791–801, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tan X, He W, Liu Y: Combination therapy with paricalcitol and trandolapril reduces renal fibrosis in obstructive nephropathy. Kidney Int 76: 1248–1257, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang Z, Zhang Y, Ning G, Deb DK, Kong J, Li YC: Combination therapy with AT1 blocker and vitamin D analog markedly ameliorates diabetic nephropathy: Blockade of compensatory renin increase. Proc Natl Acad Sci U S A 105: 15896–15901, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burgess ED, Hawkins RG, Watanabe M: Interaction of 1,25-dihydroxyvitamin D and plasma renin activity in high renin essential hypertension. Am J Hypertens 3: 903–905, 1990 [DOI] [PubMed] [Google Scholar]
- 10. Resnick LM, Muller FB, Laragh JH: Calcium-regulating hormones in essential hypertension. Relation to plasma renin activity and sodium metabolism. Ann Intern Med 105: 649–654, 1986 [DOI] [PubMed] [Google Scholar]
- 11. Tomaschitz A, Pilz S, Ritz E, Grammer T, Drechsler C, Boehm BO, Marz W: Independent association between 1,25-dihydroxyvitamin D, 25-hydroxyvitamin D and the renin-angiotensin system: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Clin Chim Acta 411: 1354–1360, 2010 [DOI] [PubMed] [Google Scholar]
- 12. Forman JP, Williams JS, Fisher ND: Plasma 25-hydroxyvitamin D and regulation of the renin-angiotensin system in humans. Hypertension 55: 1283–1288, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Park CW, Oh YS, Shin YS, Kim CM, Kim YS, Kim SY, Choi EJ, Chang YS, Bang BK: Intravenous calcitriol regresses myocardial hypertrophy in hemodialysis patients with secondary hyperparathyroidism. Am J Kidney Dis 33: 73–81, 1999 [DOI] [PubMed] [Google Scholar]
- 14. Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP: 1,25-dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110: 229–238, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kong J, Qiao G, Zhang Z, Liu SQ, Li YC: Targeted vitamin D receptor expression in juxtaglomerular cells suppresses renin expression independent of parathyroid hormone and calcium. Kidney Int 74: 1577–1581, 2008 [DOI] [PubMed] [Google Scholar]
- 16. Yuan W, Pan W, Kong J, Zheng W, Szeto FL, Wong KE, Cohen R, Klopot A, Zhang Z, Li YC: 1,25-dihydroxyvitamin D3 suppresses renin gene transcription by blocking the activity of the cyclic AMP response element in the renin gene promoter. J Biol Chem 282: 29821–29830, 2007 [DOI] [PubMed] [Google Scholar]
- 17. de Jong PE, Navis G: Proteinuria lowering needs a multifactorial and individualized approach to halt progression of renal disease. Nat Clin Pract Nephrol 4: 654–655, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Parving HH, Persson F, Lewis JB, Lewis EJ, Hollenberg NK, AVOID Study Investigators: Aliskiren combined with losartan in type 2 diabetes and nephropathy. N Engl J Med 358: 2433–2446, 2008 [DOI] [PubMed] [Google Scholar]
- 19. de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, Parving HH, Pritchett Y, Remuzzi G, Ritz E, Andress D: Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): A randomised controlled trial. Lancet 376: 1543–1551, 2010 [DOI] [PubMed] [Google Scholar]
- 20. Kong J, Kim GH, Wei M, Sun T, Li G, Liu SQ, Li X, Bhan I, Zhao Q, Thadhani R, Li YC: Therapeutic effects of vitamin D analogs on cardiac hypertrophy in spontaneously hypertensive rats. Am J Pathol 177: 622–631, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bodyak N, Ayus JC, Achinger S, Shivalingappa V, Ke Q, Chen YS, Rigor DL, Stillman I, Tamez H, Kroeger PE, Wu-Wong RR, Karumanchi SA, Thadhani R, Kang PM: Activated vitamin D attenuates left ventricular abnormalities induced by dietary sodium in dahl salt-sensitive animals. Proc Natl Acad Sci U S A 104: 16810–16815, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fischer SS, Kempe DS, Leibrock CB, Rexhepaj R, Siraskar B, Boini KM, Ackermann TF, Foller M, Hocher B, Rosenblatt KP, Kuro-O M, Lang F: Hyperaldosteronism in klotho-deficient mice. Am J Physiol Renal Physiol 299: F1171–1177, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lundqvist J, Norlin M, Wikvall K: 1alpha,25-dihydroxyvitamin D3 affects hormone production and expression of steroidogenic enzymes in human adrenocortical NCI-H295R cells. Biochim Biophys Acta 1801: 1056–1062, 2010 [DOI] [PubMed] [Google Scholar]
- 24. Simpson RU, Hershey SH, Nibbelink KA: Characterization of heart size and blood pressure in the vitamin D receptor knockout mouse. J Steroid Biochem Mol Biol 103: 521–524, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Santos Rde S, Vieira da Costa VA, Vianna LM: Cholecalciferol treatment changes urinary sodium-potassium ratio and plasma aldosterone of spontaneously hypertensive rats. Clin Chim Acta 376: 253–254, 2007 [DOI] [PubMed] [Google Scholar]
- 26. Good DW, George T, Watts BA, 3rd: Aldosterone potentiates 1,25-dihydroxyvitamin D3 action in renal thick ascending limb via a nongenomic, ERK-dependent pathway. Am J Physiol Cell Physiol 285: C1122–1130, 2003 [DOI] [PubMed] [Google Scholar]
- 27. Morris KL, Zemel MB: 1,25-dihydroxyvitamin D3 modulation of adipocyte glucocorticoid function. Obes Res 13: 670–677, 2005 [DOI] [PubMed] [Google Scholar]
- 28. Mitani H, Ishizaka N, Aizawa T, Ohno M, Usui S, Suzuki T, Amaki T, Mori I, Nakamura Y, Sato M, Nangaku M, Hirata Y, Nagai R: In vivo klotho gene transfer ameliorates angiotensin II-induced renal damage. Hypertension 39: 838–843, 2002 [DOI] [PubMed] [Google Scholar]
- 29. Zhou Q, Lin S, Tang R, Veeraragoo P, Peng W, Wu R: Role of fosinopril and valsartan on klotho gene expression induced by angiotensin II in rat renal tubular epithelial cells. Kidney Blood Press Res 33: 186–192, 2010 [DOI] [PubMed] [Google Scholar]
- 30. Yoon HE, Ghee JY, Piao S, Song JH, Han DH, Kim S, Ohashi N, Kobori H, Kuro-O M, Yang CW: Angiotensin II blockade upregulates the expression of klotho the anti-ageing gene, in an experimental model of chronic cyclosporine nephropathy. Nephrol Dial Transplant 26: 800–813, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Saito K, Ishizaka N, Mitani H, Ohno M, Nagai R: Iron chelation and a free radical scavenger suppress angiotensin II-induced downregulation of klotho, an anti-aging gene, in rat. FEBS Lett 551: 58–62, 2003 [DOI] [PubMed] [Google Scholar]
- 32. Aizawa H, Saito Y, Nakamura T, Inoue M, Imanari T, Ohyama Y, Matsumura Y, Masuda H, Oba S, Mise N, Kimura K, Hasegawa A, Kurabayashi M, Kuro-o M, Nabeshima Y, Nagai R: Downregulation of the klotho gene in the kidney under sustained circulatory stress in rats. Biochem Biophys Res Commun 249: 865–871, 1998 [DOI] [PubMed] [Google Scholar]
- 33. Koh N, Fujimori T, Nishiguchi S, Tamori A, Shiomi S, Nakatani T, Sugimura K, Kishimoto T, Kinoshita S, Kuroki T, Nabeshima Y: Severely reduced production of klotho in human chronic renal failure kidney. Biochem Biophys Res Commun 280: 1015–1020, 2001 [DOI] [PubMed] [Google Scholar]
- 34. Tsujikawa H, Kurotaki Y, Fujimori T, Fukuda K, Nabeshima Y: Klotho, a gene related to a syndrome resembling human premature aging, functions in a negative regulatory circuit of vitamin D endocrine system. Mol Endocrinol 17: 2393–2403, 2003 [DOI] [PubMed] [Google Scholar]
- 35. Mitobe M, Yoshida T, Sugiura H, Shirota S, Tsuchiya K, Nihei H: Oxidative stress decreases klotho expression in a mouse kidney cell line. Nephron Exp Nephrol 101: e67–74, 2005 [DOI] [PubMed] [Google Scholar]
- 36. Sachse A, Wolf G: Angiotensin II-induced reactive oxygen species and the kidney. J Am Soc Nephrol 18: 2439–2446, 2007 [DOI] [PubMed] [Google Scholar]
- 37. Zuo Z, Lei H, Wang X, Wang Y, Sonntag W, Sun Z: Aging-related kidney damage is associated with a decrease in klotho expression and an increase in superoxide production. Age (Dordr) Epub ahead of print, September 10, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW: Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ Res 74: 1141–1148, 1994 [DOI] [PubMed] [Google Scholar]
- 39. Doran DE, Weiss D, Zhang Y, Griendling KK, Taylor WR: Differential effects of AT1 receptor and Ca2+ channel blockade on atherosclerosis, inflammatory gene expression, and production of reactive oxygen species. Atherosclerosis 195: 39–47, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dusso A, Arcidiacono MV, Yang J, Tokumoto M: Vitamin D inhibition of TACE and prevention of renal osteodystrophy and cardiovascular mortality. J Steroid Biochem Mol Biol 121: 193–198, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chen CD, Podvin S, Gillespie E, Leeman SE, Abraham CR: Insulin stimulates the cleavage and release of the extracellular domain of klotho by ADAM10 and ADAM17. Proc Natl Acad Sci U S A 104: 19796–19801, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lautrette A, Li S, Alili R, Sunnarborg SW, Burtin M, Lee DC, Friedlander G, Terzi F: Angiotensin II and EGF receptor cross-talk in chronic kidney diseases: A new therapeutic approach. Nat Med 11: 867–874, 2005 [DOI] [PubMed] [Google Scholar]
- 43. Thurston RD, Larmonier CB, Majewski PM, Ramalingam R, Midura-Kiela M, Laubitz D, Vandewalle A, Besselsen DG, Muhlbauer M, Jobin C, Kiela PR, Ghishan FK: Tumor necrosis factor and interferon-gamma down-regulate klotho in mice with colitis. Gastroenterology 138: 1384–1394, 1394.e1–2, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Imura A, Iwano A, Tohyama O, Tsuji Y, Nozaki K, Hashimoto N, Fujimori T, Nabeshima Y: Secreted klotho protein in sera and CSF: Implication for post-translational cleavage in release of klotho protein from cell membrane. FEBS Lett 565: 143–147, 2004 [DOI] [PubMed] [Google Scholar]
- 45. Matsumura Y, Aizawa H, Shiraki-Iida T, Nagai R, Kuro-o M, Nabeshima Y: Identification of the human klotho gene and its two transcripts encoding membrane and secreted klotho protein. Biochem Biophys Res Commun 242: 626–630, 1998 [DOI] [PubMed] [Google Scholar]
- 46. Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kaname T, Kume E, Iwasaki H, Iida A, Shiraki-Iida T, Nishikawa S, Nagai R, Nabeshima YI: Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390: 45–51, 1997 [DOI] [PubMed] [Google Scholar]
- 47. Hu MC, Shi M, Zhang J, Quinones H, Griffith C, Kuro-o M, Moe OW: Klotho deficiency causes vascular calcification in chronic kidney disease. J Am Soc Nephrol 22: 124–136, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S, Hu MC, Moe OW, Kuro-o M: Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem 281: 6120–6123, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, Fujita T, Fukumoto S, Yamashita T: Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature 444: 770–774, 2006 [DOI] [PubMed] [Google Scholar]
- 50. Farrow EG, Davis SI, Summers LJ, White KE: Initial FGF23-mediated signaling occurs in the distal convoluted tubule. J Am Soc Nephrol 20: 955–960, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Vervloet MG, van Ittersum FJ, Buttler RM, Heijboer AC, Blankenstein MA, Ter Wee PM: Effects of dietary phosphate and calcium intake on fibroblast growth factor-23. Clin J Am Soc Nephrol 6: 383–389, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T: FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res 19: 429–435, 2004 [DOI] [PubMed] [Google Scholar]
- 53. Perwad F, Zhang MY, Tenenhouse HS, Portale AA: Fibroblast growth factor 23 impairs phosphorus and vitamin D metabolism in vivo and suppresses 25-hydroxyvitamin D-1alpha-hydroxylase expression in vitro. Am J Physiol Renal Physiol 293: F1577–1583, 2007 [DOI] [PubMed] [Google Scholar]
- 54. Nakatani T, Sarraj B, Ohnishi M, Densmore MJ, Taguchi T, Goetz R, Mohammadi M, Lanske B, Razzaque MS: In vivo genetic evidence for klotho-dependent, fibroblast growth factor 23 (Fgf23) -mediated regulation of systemic phosphate homeostasis. FASEB J 23: 433–441, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alexander RT, Woudenberg-Vrenken TE, Buurman J, Dijkman H, van der Eerden BC, van Leeuwen JP, Bindels RJ, Hoenderop JG: Klotho prevents renal calcium loss. J Am Soc Nephrol 20: 2371–2379, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fliser D, Kollerits B, Neyer U, Ankerst DP, Lhotta K, Lingenhel A, Ritz E, Kronenberg F, MMKD Study Group, Kuen E, Konig P, Kraatz G, Mann JF, Muller GA, Kohler H, Riegler P: Fibroblast growth factor 23 (FGF23) predicts progression of chronic kidney disease: The mild to moderate kidney disease (MMKD) study. J Am Soc Nephrol 18: 2600–2608, 2007 [DOI] [PubMed] [Google Scholar]
- 57. Mirza MA, Larsson A, Melhus H, Lind L, Larsson TE: Serum intact FGF23 associate with left ventricular mass, hypertrophy and geometry in an elderly population. Atherosclerosis 207: 546–551, 2009 [DOI] [PubMed] [Google Scholar]
- 58. Kirkpantur A, Balci M, Gurbuz OA, Afsar B, Canbakan B, Akdemir R, Ayli MD: Serum fibroblast growth factor-23 (FGF-23) levels are independently associated with left ventricular mass and myocardial performance index in maintenance haemodialysis patients. Nephrol Dial Transplant 26: 1346–1354, 2011 [DOI] [PubMed] [Google Scholar]
- 59. Mirza MA, Hansen T, Johansson L, Ahlstrom H, Larsson A, Lind L, Larsson TE: Relationship between circulating FGF23 and total body atherosclerosis in the community. Nephrol Dial Transplant 24: 3125–3131, 2009 [DOI] [PubMed] [Google Scholar]
- 60. Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, Smith K, Lee H, Thadhani R, Juppner H, Wolf M: Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med 359: 584–592, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Yilmaz MI, Sonmez A, Saglam M, Yaman H, Kilic S, Demirkaya E, Eyileten T, Caglar K, Oguz Y, Vural A, Yenicesu M, Zoccali C: FGF-23 and vascular dysfunction in patients with stage 3 and 4 chronic kidney disease. Kidney Int 78: 679–685, 2010 [DOI] [PubMed] [Google Scholar]
- 62. Vervloet MG, Van Zuilen AD, Blankestijn PJ, Ter Wee PM, Wetzels JF: Fibroblast growth factor 23 is associated with proteinuria [Abstract]. J Am Soc Nephrol 21: 186A, 2010 [Google Scholar]
- 63. Chang Q, Hoefs S, van der Kemp AW, Topala CN, Bindels RJ, Hoenderop JG: The beta-glucuronidase klotho hydrolyzes and activates the TRPV5 channel. Science 310: 490–493, 2005 [DOI] [PubMed] [Google Scholar]
- 64. Haruna Y, Kashihara N, Satoh M, Tomita N, Namikoshi T, Sasaki T, Fujimori T, Xie P, Kanwar YS: Amelioration of progressive renal injury by genetic manipulation of klotho gene. Proc Natl Acad Sci U S A 104: 2331–2336, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Wang Y, Sun Z: Klotho gene delivery prevents the progression of spontaneous hypertension and renal damage. Hypertension 54: 810–817, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Ikushima M, Rakugi H, Ishikawa K, Maekawa Y, Yamamoto K, Ohta J, Chihara Y, Kida I, Ogihara T: Anti-apoptotic and anti-senescence effects of klotho on vascular endothelial cells. Biochem Biophys Res Commun 339: 827–832, 2006 [DOI] [PubMed] [Google Scholar]
- 67. Kuro-o M: Klotho as a regulator of oxidative stress and senescence. Biol Chem 389: 233–241, 2008 [DOI] [PubMed] [Google Scholar]
- 68. Saito Y, Yamagishi T, Nakamura T, Ohyama Y, Aizawa H, Suga T, Matsumura Y, Masuda H, Kurabayashi M, Kuro-o M, Nabeshima Y, Nagai R: Klotho protein protects against endothelial dysfunction. Biochem Biophys Res Commun 248: 324–329, 1998 [DOI] [PubMed] [Google Scholar]
- 69. Yamamoto M, Clark JD, Pastor JV, Gurnani P, Nandi A, Kurosu H, Miyoshi M, Ogawa Y, Castrillon DH, Rosenblatt KP, Kuro-o M: Regulation of oxidative stress by the anti-aging hormone klotho. J Biol Chem 280: 38029–38034, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kusaba T, Okigaki M, Matui A, Murakami M, Ishikawa K, Kimura T, Sonomura K, Adachi Y, Shibuya M, Shirayama T, Tanda S, Hatta T, Sasaki S, Mori Y, Matsubara H: Klotho is associated with VEGF receptor-2 and the transient receptor potential canonical-1 Ca2+ channel to maintain endothelial integrity. Proc Natl Acad Sci U S A 107: 19308–19313, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wolf M: Forging forward with 10 burning questions on FGF23 in kidney disease. J Am Soc Nephrol 21: 1427–1435, 2010 [DOI] [PubMed] [Google Scholar]
- 72. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group: KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 113: S1–130, 2009 [DOI] [PubMed] [Google Scholar]