Abstract
The causes of the increased risk for ESRD among African Americans are not completely understood. Here, we examined whether higher levels of urinary albumin excretion among African Americans contributes to this disparity. We analyzed data from 27,911 participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study who had urinary albumin-to-creatinine ratio (ACR) and estimated GFR (eGFR) measured at baseline. We identified incident cases of ESRD through linkage with the United States Renal Data System. At baseline, African Americans were less likely to have an eGFR <60 ml/min per 1.73 m2 but more likely to have an ACR ≥30 mg/g. The incidence rates of ESRD among African Americans and whites were 204 and 58.6 cases per 100,000 person-years, respectively. After adjustment for age and gender, African Americans had a fourfold greater risk for developing ESRD (HR 4.0; 95% CI 2.8 to 5.9) compared with whites. Additional adjustment for either eGFR or ACR reduced the risk associated with African-American race to 2.3-fold (95% CI 1.5 to 3.3) or 1.8-fold (95% CI 1.2 to 2.7), respectively. Adjustment for both ACR and eGFR reduced the race-associated risk to 1.6-fold (95% CI 1.1 to 2.4). Finally, in a model that further adjusted for both eGFR and ACR, hypertension, diabetes, family income, and educational status, African-American race associated with a nonsignificant 1.4-fold (95% CI 0.9 to 2.3) higher risk for ESRD. In conclusion, the increased prevalence of albuminuria may be an important contributor to the higher risk for ESRD experienced by African Americans.
African Americans have a three- to fourfold increased risk of ESRD compared with whites.1 This increased risk contrasts with the comparable or higher prevalence of earlier chronic kidney disease (CKD), defined by GFRs between 15 to 60 ml/min per 1.73 m2, reported for whites in the National Health and Nutrition Survey (NHANES)1,2, the Multi-Ethnic Study of Atherosclerosis (MESA), study3 and the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study.4 The reasons for this discrepancy have not been fully explained.5–7
Albuminuria, defined as an albumin-to-creatinine ratio (ACR) of 30 mg/g or greater is an important risk factor for progression of CKD to ESRD.8–12 The prevalence of albuminuria is higher among African Americans compared with whites in NHANES and other studies even at higher levels of GFR.13–15 However, we are unaware of studies that have examined the degree to which racial disparities in the prevalence of albuminuria contribute to black-white differences in ESRD, and the present study examined this possibility.
RESULTS
The mean (SD) age of participants was 64.8 (9.4) years, 45.6% were men, and 40.5% were African American. Less than high school education was reported by 12.3% of participants, and 17.6% lived in low-income households (reported as below $20,000 annually). Hypertension (59.9%) and diabetes (20.9%) were common. At baseline, African Americans were younger than whites. African Americans were less likely to be men, had a greater waist circumference, were more likely to report a low income, to not have completed high school, and to have hypertension and diabetes (Table 1). In contrast, African Americans were more likely than whites to be treated with a renin-angiotensin system blocking agent.
Table 1.
Baseline characteristics of REGARDS study participants
| Total | African American | White | |
|---|---|---|---|
| Subjects | 27,911 | 40.5% | 59.5% |
| Age (years)a | 64.8 (9.4) | 63.9 (9.2) | 65.4 (9.5) |
| Male (%) | 45.6 | 38.5 | 50.5 |
| Hypertension (%) | 59.9 | 71.1 | 50.5 |
| Diabetes (%) | 20.9 | 29.3 | 15.2 |
| Renin-angiotensin agent (%) | 35.9 | 41.7 | 32.0 |
| Low income (%) | 17.6 | 26.4 | 11.6 |
| Education < HS (%) | 12.3 | 19.7 | 7.2 |
| eGFR (ml/min per 1.73 m2)a | 85.1 (20.0) | 88.8 (23.1) | 82.6 (17.1) |
| Median ACR (mg/g)* | 7.4 | 8.0 | 7.1 |
| Waist circumference (cm)a | 96.1 (15.0) | 98.1 (15.3) | 94.7 (15.5) |
| Albuminuria (%)** | |||
| 30 to 299 mg/g | 12.2 | 14.6 | 10.5 |
| ≥300 mg/g | 2.8 | 4.7 | 1.7 |
| CKD (%)*** | |||
| 30 to 59 ml/min per 1.73 m2 | 10.0 | 9.9 | 10.0 |
| 15 to 29 ml/min per 1.73 m2 | 1.09 | 1.1 | 0.6 |
REGARDS, Reasons for Geographic and Racial Differences in Stroke; eGFR, estimated GFR; ACR, albumin-to-creatinine ratio; CKD, chronic kidney disease.
a Values are mean with SD in parentheses.
Differences between African-Americans and white subjects: *P < 0.0001;
**Wilcoxon rank sum test, P < 0.0001;
***P = 0.0007.
The mean estimated GFR (eGFR) for African Americans was 88.8 (23.1) ml/min per 1.73 m2 and 82.6 (17.1) ml/min per 1.73 m2 in whites. The median ACR for African Americans was 8.0 mg/g and the 25th to 75th percentiles were 4.7 and 19.9 mg/g, respectively, and 7.1 mg/g (25th to 75th percentiles: 4.6 to 14.0 mg/g) for whites. Across levels of eGFR at baseline, the median ACR in African Americans increased from 7.4 mg/g at eGFR ≥90 ml/min per 1.73 m2 to 91.2 mg/g at eGFR levels of 15 to 29 ml/min per 1.73 m2. In contrast, among whites there was an increase from 6.8 to 20.6 mg/g in the median ACR level by level of GFR (Table 2). It should be noted that a large AA:W difference in ACR levels was present at eGFR below 30 ml/min per 1.73 m2. The eGFR among African Americans and whites at higher levels of baseline ACR had a comparable pattern. Among African Americans the eGFR difference was 31.8 ml/min per 1.73 m2 at ACR levels of <10 mg/g to ≥300 mg/g, whereas among whites it was 22.3 ml/min per 1.73 m2. A consequence of the different magnitudes of decrease in GFR by race over levels of baseline ACR was that higher mean eGFR in whites was reversed among individuals with ACR ≥300 mg/g (Table 2).
Table 2.
Levels of estimated glomerular filtration rate and elevated albumin-to-creatinine ratio at baseline by race and the African-American-to-white odds ratio for reduced estimated glomerular filtration rate and elevated albumin-to-creatinine ratio
| African American |
White |
AA:W ORb | |||||
|---|---|---|---|---|---|---|---|
| % | GFR (ml/min per 1.73 m2)a | ACR Median | % | GFR (ml/min per 1.73 m2)a | ACR Median | ||
| GFR | |||||||
| ≥90 | 53.1 | 106.4 (10.1) | 7.4 | 40.0 | 98.0 (5.8) | 6.8 | 1 (ref) |
| 45 to 89 | 36.0 | 77.1 (8.3) | 7.5 | 49.6 | 77.7 (8.2) | 6.9 | 0.59 (0.56, 0.62) |
| 30 to 44 | 7.0 | 53.6 (4.2) | 12.1 | 7.4 | 53.5 (4.3) | 11.0 | 0.78 (0.70, 0.86) |
| 15 to 29 | 3.5 | 31.2 (8.1) | 91.2 | 3.0 | 35.4 (8.1) | 20.6 | 1.15 (1.01, 1.31) |
| ACR | |||||||
| <10 | 58.8 | 91.7 (19.9) | 5.1 | 64.8 | 84.6 (15.1) | 5.2 | 1 (ref) |
| 10 to 29 | 22.9 | 90.7 (21.6) | 15.0 | 23.2 | 81.6 (17.5) | 14.6 | 1.12 (1.05, 1.19) |
| 30 to 299 | 14.5 | 83.9 (26.3) | 65.5 | 10.4 | 76.0 (21.2) | 58.2 | 1.69 (1.57, 1.83) |
| ≥300 | 3.8 | 59.9 (32.7) | 791.7 | 1.6 | 62.3 (27.0) | 644.1 | 3.44 (2.96, 3.99) |
GFR, glomerular filtration rate; ACR, albumin-to-creatinine ratio; AA:W, African American:white; OR, odds ratio; CI, confidence interval.
a Values are mean with SD in parentheses.
b Values are OR adjusted for age and gender, with 95% CI in parentheses.
The age and gender adjusted prevalence of African Americans compared with whites, expressed as the AA:W odds ratio (OR) with 95% confidence interval (CI), increased as both ACR increased and GFR decreased (Table 2).
Over a median of 3.6 years of follow-up, 133 participants developed incident ESRD and an incidence rate of 142 persons per 100,000 person-years of follow-up. There were 96 incident cases of ESRD among African Americans and 37 among white participants with respective incidence rates (95% CI) of 204 and 58.6 ESRD cases per 100,000 person-years. The crude African American-to-white hazard ratio (95% CI) for ESRD was 3.80 (2.60, 5.56). After adjustment for age and gender, the AA:W hazard ratio (HR) was 4.01 (2.73, 5.89).
ESRD incidence in both races increased as level of baseline eGFR declined, and baseline ACR increased (Table 3). The ESRD incidence rate increased among African Americans from 34.8 persons/100,000 person-years for a baseline eGFR of 90 ml/min per 1.73 m2 or greater to 4242.2 persons/100,000 person-years for participants with baseline GFR <29 ml/min per 1.73 m2. Analogous values for whites were 13.6 to 1506.4 persons/100,000 person-years (Table 3).
Table 3.
Incident ESRD by race and level of estimated glomerular filtration rate and elevated albumin-to-creatinine ratio
| African American |
White |
AA:W HR (95% CI)b | |||
|---|---|---|---|---|---|
| Na | Rate per 100,000 Person-Years | Na | Rate per 100,000 Person-Years | ||
| All | 98 | 247.6 | 37 | 65.6 | 3.80 (2.60, 5.56) |
| GFR | |||||
| ≥90 | 7 | 34.8 | 3 | 13.6 | 2.58 (0.67, 9.97) |
| 45 to 89.9 | 10 | 70.5 | 3 | 10.6 | 6.23 (1.68, 23.05) |
| 30 to 44.9 | 6 | 217.4 | 4 | 96.9 | 2.13 (0.60, 7.56) |
| 15 to 29.9 | 75 | 4242.2 | 27 | 1506.4 | 2.82 (1.81, 4.40) |
| ACR | |||||
| 0 to 9.9 | 7 | 31.1 | 6 | 16.5 | 2.82 (1.81, 4.39) |
| 10 to 29.9 | 3 | 33.7 | 3 | 22.9 | 1.56 (0.62, 3.92) |
| 30 to 299.9 | 20 | 355.6 | 10 | 168.7 | 2.21 (1.03, 4.72) |
| ≥300 | 68 | 3762.6 | 18 | 1860.4 | 2.21 (1.31, 3.72) |
AA:W, African American:white; HR, hazard ratio; CI, confidence interval. ACR, albumin-to-creatinine ratio.
a Numbers of participants developing ESRD.
b Values are HR for incident ESRD adjusted for age and gender, with 95% CI in parentheses.
The ESRD rate for African Americans increased from 31.1 to 3763 persons/100,000 person-years and in whites from 16.5 to 1860 persons/100,000 person-years as baseline ACR increased from <10 mg/g to ≥300 mg/g.
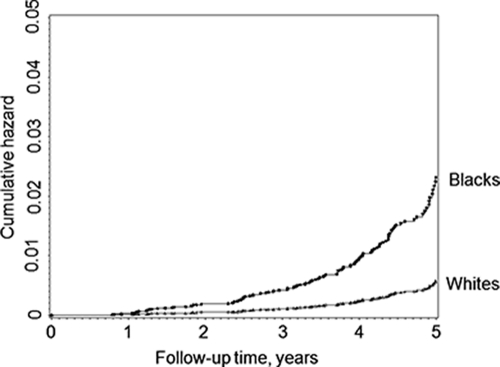
The age-gender adjusted cumulative hazard during follow-up is shown for blacks and whites in Figure 1.
Figure 1.
Age- and gender-related adjusted cumulative hazard for incident ESRD among African Americans and whites. The cumulative hazard during the follow-up is shown for 65-year-old men.
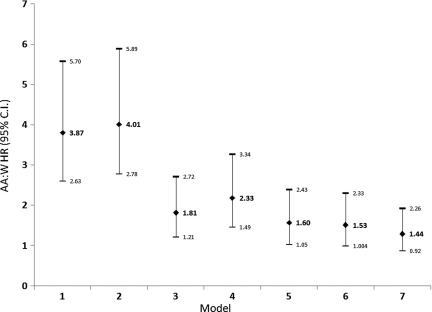
Multivariable models, which control for ACR, attenuated the AA:W HR (95% CI) for ESRD (Figure 2). The AA:W HR (95% CI) for incident ESRD controlling for age, gender, and waist circumference was 3.87 (2.63, 5.70). When log of ACR was added to this model the AA:W HR (95% CI) was substantially reduced to 1.81 (1.21, 2.72). In comparison, when eGFR was substituted for log of ACR the AA:W HR (95% CI) was reduced to 2.23 (1.49, 3.34). Inclusion of both eGFR and log ACR in the model, resulted in a modest reduction over that of ACR alone [AA:W HR (95% CI) = 1.60 (1.05, 2.43)].
Figure 2.
Hazard ratio of incident ESRD for African Americans vs. whites with adjustments for various risk factors progressively added to the model. (♦), the hazard ratio; horizontal line, the 95% CI. Covariates in model: model 1: Race; model 2: model 1 and demographics (age, gender, and waist circumference); model 3: model 2 and log of ACR; model 4: model 2 and eGFR; model 5: model 2 and both eGFR and log of ACR; model 6: model 5 and diabetes, hypertension, and renin-angiotensin system blocking agents; model 7: model 6 and household income and educational attainment.
When we sequentially adjusted the model with age, gender, waist circumference, eGFR, and ACR for diabetes, hypertension, and use of renin-angiotensin system blocking agents as well as for education and household income, the AA:W HR (95% CI) decreased to 1.44 (0.92, 2.56) (Figure 2). We tested for interaction between race, ACR, and GFR in the final model. The three-way interaction term was not significant (P = 0.232). In a model containing only two-way interaction terms neither that for race and ACR (P = 0.824) nor for race and eGFR (P = 0.086) was statistically significant.
DISCUSSION
African Americans have a comparable or lower prevalence of more advanced CKD, measured either by serum creatinine16 or GFR1,17,18 than whites, a finding we have previously reported for REGARDS participants4 that was observed as well in the present study. Lower baseline eGFR was associated with increased risk of ESRD for African Americans compared with whites, although the AA:W HR was attenuated as the severity of CKD increased. These observations are similar to those reported by Choi et al. for a sample of more than two million patients in the Veterans Administration health system, where the AA:W HR for ESRD, adjusted for demographic characteristics, comorbid conditions, and socioeconomic status, declined from 2.14 (1.72 to 2.65) to 1.86 (1.75 to 1.98), for baseline GFR strata ≥90 and 15 to 29 ml/min per 1.73 m2, respectively.19
These observations stand in contrast to three- to fourfold higher ESRD incidence rates among African Americans than whites and suggest that race-specific factors that influence progression of kidney disease may account for the discrepancy.20 One potential risk factor for progressive CKD is the increased albumin excretion among African Americans. Increased urinary albumin excretion is a risk factor for progression of CKD8,12,21–23, and our study suggests that racial differences in the prevalence and magnitude of increased ACR may account for a substantial proportion of this excess risk, at least among the covariates examined in the present study.
Racial differences in ACR have been reported for participants in several studies. For example, the prevalence ACR ≥30 mg/g in the NHANES III population was 12% among African Americans and 8% among whites, AA:W OR (95% CI) of 1.41 (1.12 to 1.77) among individuals without diabetes, and 1.85 (1.18 to 2.91) among those with diabetes, racial differences of comparable magnitude to those we observed.14 In the Kidney Early Evaluation Program study ACR ≥30 mg/g was prevalent in 8% of whites and 11% of African Americans, an OR (95% CI) 1.38, (1.29 to 1.47).24
Increased urinary albumin excretion among African Americans has been noted early in life. During early adulthood (age 20 to 37 years), African American participants in the Bogalusa Heart Study were observed to have higher ACR. ACR levels were associated with higher BP between ages 5 and 17 years in African-American, but not in whites participants.15 Hanevoid et al. reported that healthy, normotensive African-American adolescents were more likely to have an increased albumin excretion that was associated with impaired stress-induced pressure natriuresis and, in African-American men, with higher BP.25 African-American participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study, aged 50 years and younger, had a geometric mean ACR, adjusted for gender and race differences in creatinine excretion, which was higher among African Americans.26 Of interest, higher geometric mean ACR in both races in the CARDIA study was independently associated with higher BP.
Despite the higher prevalence of elevated ACR in both hypertension19 and diabetes27 and the strong association with risk of ESRD9,28 the role of ACR as a factor contributing factor to the racial disparities in progressive CKD has not been well studied. At baseline, African Americans in REGARDS had an increased prevalence of albumin excretion evident at levels of ACR currently regarded as within the normal range, and the racial disparity in ESRD incidence increased with increasing level of ACR. African Americans and whites with either high (ACR 30 to 299.9 mg/g) or very high (≥300 mg/g) levels of albuminuria had increased risk of ESRD.
The fourfold increased risk of ESRD among African Americans in our study is consistent with data from the United States Renal Data System (USRDS) for the US population and this excess risk was substantially attenuated after controlling for ACR. The reduction in the AA:W HR for ESRD controlling for ACR was greater than that observed when controlling for eGFR alone. Furthermore, the reduction in AA:W HR for ESRD in models controlling for both ACR and eGFR was comparable to that controlling for ACR alone. These results suggest that the increased prevalence of ACR ≥30 mg/g among African Americans may contribute importantly to the increased risk for ESRD experienced by this population.
These observations raise the question as to what factors might mediate racial differences in the prevalence of albuminuria. Increased excretion of albumin in the urine may reflect increased filtration of serum albumin or decreased proximal tubular reabsorption of filtered albumin.29–31 Factors that may be related to racial differences in albuminuria include elevated BP and cardiovascular risk factors,30–32 obesity33 and the metabolic syndrome,34 smoking,35 vitamin D levels,36 genetic polymorphisms,37–39 geographic origin40,41, lower socioeconomic status42,43, and low birth weight44,45. These factors may act at different times during a subject's life.46 The relevance of these issues to the attenuation of ESRD risk among blacks in the REGARDS study compared with whites is likely to be complex and will require further study.
Our findings differ from a recent report where African Americans remained three times more likely than whites to develop ESRD even after controlling for multiple risk factors.47 Factors that may account for this difference include the assessment of albuminuria using a semiquantitative dip-stick method in the previous work, compared with the quantitative measurement of ACR in this work.
There are limitations to our study. We used a single measurement of ACR and eGFR, and some individuals may be misclassified by these measures. Additionally, follow-up was only available through August 2008, and our inferences apply to short-term incidence. Our power to test for interactions was limited by the low number of cases. REGARDS does not include information that allows estimation of the duration or severity of either CKD or the underlying comorbid conditions. It was possible that more severe disease of longer duration in blacks may account for some of the increased prevalence of albuminuria and incident ESRD among these individuals. Finally, our conclusions are based on observational data and thus cannot be construed as reflecting causal associations.
Despite these limitations, the current analysis maintains several strengths. We enrolled a geographically diverse sample of African-American and white adults. Additionally, study data were collected following a standardized protocol with strict quality control procedures with isotope dilution mass spectrometry-traceable48 serum creatinine and quantitative measurements of urinary ACR. Case ascertainment by the USRDS identifies more than 90% of incident ESRD patients.
In conclusion, our results suggest differences in albumin excretion may be an important risk factor for racial disparities in progression of chronic kidney disease. The strong and consistent associations we report here provide additional evidence to support a role for albuminuria in the progression of CKD, underscoring the urgent need to conduct clinical trials to test the benefit of interventions to reduce albuminuria in preventing or delaying the occurrence of ESRD. Our observations, in part, further support the potential importance of prospective targeted reductions of albumin excretion among individuals with CKD and suggest that this may be an important strategy to reduce racial disparities in ESRD occurrence, as well as reducing the rate of progression to ESRD for all CKD patients. This possibility is supported by extensive evidence that reduction of proteinuria may delay and even prevent ESRD.49,50
CONCISE METHODS
Study Design.
The REGARDS study is a population-based ongoing cohort study of adults aged 45 years and older in the United States designed so that residents of the southeastern United States and African Americans were oversampled.51 The overall goal of REGARDS is to understand increased stroke mortality by African Americans and residents of the southeastern United States. Overall, 30,239 participants were enrolled. We excluded individuals missing either eGFR or ACR, with ESRD by self-report or based on data from the USRDS indicating the incidence of ESRD that occurred before enrollment in the REGARDS study. After these exclusions, data from 27,911 participants were available for analysis. This study was approved by the institutional review boards of the participating institutions.
Data.
The data collection procedures have been described in detail previously.51 Briefly, data were obtained by a telephone interview and a subsequent in-home examination that included two sitting BP measurements using a standard technique, assessment of waist circumference, and ascertainment of medication use reported for the 2 weeks preceding the in-home visit. Renin-angiotensin system blocking agent use was defined as reported use of either an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker. Serum creatinine, fasting blood glucose, and a random morning urine sample for measurement of creatinine and albumin were collected during the in-home visit. eGFR was calculated by the CKD-EPI equation using isotope dilution mass spectrometry-calibrated creatinine. The equation has been validated in African Americans and whites, adults with ages ranging from less than 40 to 80 years, both genders, and individuals with diabetes. We measured urinary albumin at the Department of Laboratory Medicine and Pathology at the University of Minnesota, using the BN ProSpec Nephelometer from Dade Behring (Marburg, Germany).52
Low annual household income was defined as below $20,000, and low educational attainment was defined as not having completed high school. Hypertension was defined as either self-reported use of antihypertensive medications or a mean SBP ≥140 mmHg or mean DBP ≥90 mmHg. Diabetes was defined as (1) self-reported use of insulin or oral hypoglycemics, (2) a fasting blood glucose greater than or equal to 126 mg/dl, or (3) a nonfasting blood glucose greater than or equal to 200 mg/dl.
Incident cases of ESRD were identified through linkage of REGARDS study participants with the USRDS, which records more than 90% of incident ESRD cases in the United States. A finder file containing unique individual identifiers (social security number, date of birth, and last and first name) was submitted for linkage with the USRDS Database. Sequential matching was accomplished using different configurations of full and partial individual identifiers. Individual records that did not produce a match candidate were again processed in subsequent rounds. For individuals with a match, but who did not match on all identifiers, visual inspection of nonmatching variables was performed in the following rounds to confirm valid matches. Data from the USRDS included all incident ESRD cases, regardless of treatment modality, through August 2008. Thus, person-time was censored at death, date of ESRD incidence, or September 1, 2008, whichever occurred first.
Analysis.
Baseline characteristics were calculated as means or percentages for the overall population and for whites and African Americans. We used t tests, ANOVA, and χ2 tests to test differences between races as appropriate. Log-transformed ACR was used, and we report the geometric means. We calculated incidence rates as the number of incident ESRD cases divided by the person-years of follow-up multiplied by 100,000. Incident rate ratios for African Americans compared with whites were computed as the ratios of each group's incidence rates.
We used logistic regression models to examine the independent association between race and baseline kidney function controlling for other participant characteristics. Cox proportional hazards models were fitted to examine the association between the African-American and the white race and ESRD. In these analyses we accounted for the small numbers of participants in some cells by categorizing GFR as ≥60 and <60 ml/min per 1.73 m2 and ACR as <30 and ≥30 mg/g.
First, we controlled the association between race and ESRD for age and gender. Next, models adjusting for either albuminuria (log transformed) or for GFR, and then with both were conducted to assess the degree to which the individual and combined measures of kidney function could attenuate the association between race and ESRD. Next, we determined if further adjustment for other risk factors for ESRD would modify the attenuation of the association between race and ESRD by measures of kidney function. We proceeded by adding as covariates to successive models: (1) hypertension and diabetes and (2) income and education.
We note that the sequence of covariate entry into our models may influence the interpretation of our results. Any reduction in the AA:W HR seen after first adding albuminuria to the age- and gender-adjusted model might not be as profound had we had first entered socioeconomic and comorbid covariates. We chose this sequence a priori based on the underlying biologic models for progressive kidney disease that place increased ACR and reduced GFR as proximate risk factors in the etiology of ESRD.
We assessed potential interaction between race and albuminuria or eGFR, separately, on ESRD risk, using interaction terms for race and albuminuria, race and eGFR, and a three-way interaction term for race, albuminuria, and eGFR. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
Disclosures
None.
Acknowledgments
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurologic Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurologic Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors acknowledge the staff at the USRDS Coordinating Center for their assistance with the linkage to the USRDS under a data use agreement between the USRDS and the University of Alabama at Birmingham. The authors acknowledge the participating REGARDS participating investigators and institutions for their valuable contributions: The University of Alabama at Birmingham, Birmingham, AL (Study PI, Statistical and Data Coordinating Center, Survey Research Unit): George Howard, DrPH; Leslie McClure, PhD; V. A. Howard, PhD; Libby Wagner, MA; V. A. Wadley, PhD; Rodney Go, PhD; Monika Safford MD; Ella Temple, PhD; Margaret Stewart, MSPH; J. David Rhodes, BSN; University of Vermont (Central Laboratory): Mary Cushman, MD; Wake Forest University (ECG Reading Center): Ron Prineas, MD, PhD; Alabama Neurologic Institute (Stroke Validation Center, Medical Monitoring): Camilo Gomez, MD; Susana Bowling, MD; University of Arkansas for Medical Sciences (Survey Methodology): LeaVonne Pulley, PhD; University of Cincinnati (Clinical Neuroepidemiology): Brett Kissela, MD; Dawn Kleindorfer, MD; Examination Management Services, Incorporated (In-Person Visits): Andra Graham; Medical University of South Carolina (Migration Analysis Center): Daniel Lackland, DrPH; Indiana University School of Medicine (Neuropsychology Center): Frederick Unverzagt, PhD; National Institute of Neurologic Disorders and Stroke, National Institutes of Health (funding agency): Claudia Moy, PhD. Additional funding was provided by an investigator-initiated grant-in-aid from Amgen Corporation. Amgen did not have any role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation or approval of the manuscript. The manuscript was sent to Amgen for review before submission for publication.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1. Clase CM, Garg AX, Kiberd BA: Prevalence of low glomerular filtration rate in nondiabetic Americans: Third National Health and Nutrition Examination Survey (NHANES III). J Am Soc Nephrol 13: 1338–1349, 2002 [DOI] [PubMed] [Google Scholar]
- 2. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 3. Kramer H, Palmas W, Kestenbaum B, Cushman M, Allison M, Astor B, Shlipak M. Chronic kidney disease prevalence estimates among racial/ethnic groups: The Multi-Ethnic Study of Atherosclerosis. Clin J Am Soc Nephrol 3: 1391–1397, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McClellan W, Warnock DG, McClure L, Campbell RC, Newsome BB, Howard V, Cushman M, Howard G: Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol 17: 1710–1715, 2006 [DOI] [PubMed] [Google Scholar]
- 5. Tarver-Carr ME, Powe NR, Eberhardt MS, Laveist TA, Kington RS, Coresh J, Brancati FL: Excess risk of chronic kidney disease among African-American versus white subjects in the United States: A population-based study of potential explanatory factors. J Am Soc Nephrol 13: 2363–2370, 2002 [DOI] [PubMed] [Google Scholar]
- 6. Krop JS, Coresh J, Chambless LE, Shahar E, Watson RL, Szklo M, Brancati FL: A community-based study of explanatory factors for the excess risk for early renal function decline in blacks vs whites with diabetes—The atherosclerosis risk in communities study. Arch Intern Med 159: 1777–1783, 1999 [DOI] [PubMed] [Google Scholar]
- 7. Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Hernandez GT, O'Hare AM: White/black racial differences in risk of end-stage renal disease and death. Am J Med 122: 672–678, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ishani A, Grandits GA, Grimm RH, Svendsen KH, Collins AJ, Prineas RJ, Neaton JD. Association of single measurements of dipstick proteinuria, estimated glomerular filtration rate, and hematocrit with 25-year incidence of end-stage renal disease in the multiple risk factor intervention trial. J Am Soc Nephrol 17: 1444–1452, 2006 [DOI] [PubMed] [Google Scholar]
- 9. Halbesma N, Kuiken DS, Brantsma AH, Bakker SJ, Wetzels JF, De Zeeuw D, De Zeeuw D, De Jong PE, Gansevoort RT. Macroalbuminuria is a better risk marker than low estimated GFR to identify individuals at risk for accelerated GFR loss in population screening. J Am Soc Nephrol 17: 2582–2590, 2006 [DOI] [PubMed] [Google Scholar]
- 10. Ikeda A, Konta T, Takasaki S, Hao Z, Suzuki K, Sato H, Shibata Y, Takeishi Y, Kato T, Kawata S, Kubota I: In a non-diabetic Japanese population, the combination of macroalbuminuria and increased urine beta 2-microglobulin predicts a decline of renal function: The Takahata study. Nephrol Dial Transplant 24: 841–847, 2009 [DOI] [PubMed] [Google Scholar]
- 11. Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N, Mogensen CE, Cooper M, Marre M, Williams B, Hamet P, Mancia G, Woodward M, Macmahon S, Chalmers J; ADVANCE Collaborative Group Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 20: 1813–1821, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR: Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol 20: 1069–1077, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jiang X, Srinivasan SR, Radhakrishnamurthy B, Dalferes ER, Jr., Bao W, Berenson GS. Microalbuminuria in young adults related to blood pressure in a biracial (black-white) population. The Bogalusa Heart Study. Am J Hypertens 7: 794–800, 1994 [DOI] [PubMed] [Google Scholar]
- 14. Bryson CL, Ross HJ, Boyko EJ, Young BA: Racial and ethnic variations in albuminuria in the US Third National Health and Nutrition Examination Survey (NHANES III) population: Associations with diabetes and level of CKD. Am J Kidney Dis 48: 720–726, 2006 [DOI] [PubMed] [Google Scholar]
- 15. Hoq S, Chen W, Srinivasan SR, Berenson GS: Childhood blood pressure predicts adult microalbuminuria in African Americans, but not in whites: The Bogalusa Heart Study. Am J Hypertens 15: 1036–1041, 2002 [DOI] [PubMed] [Google Scholar]
- 16. Jones CA, McQuillan GM, Kusek JW, Eberhardt MS, Herman WH, Coresh J, Salive M, Jones CP, Agodoa LY: Serum creatinine levels in the US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 32: 992–999, 1998 [DOI] [PubMed] [Google Scholar]
- 17. Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS: Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 41: 1–12, 2003 [DOI] [PubMed] [Google Scholar]
- 18. Trivedi HS, Pang MM: Discrepancy in the epidemiology of nondiabetic chronic renal insufficiency and end-stage renal disease in black and white Americans: The third National Health and Nutrition Examination Survey and United States Renal Data System. Am J Nephrol 23: 448–457, 2003 [DOI] [PubMed] [Google Scholar]
- 19. Ritz E, Nowicki M, Fliser D, Horner D, Klimm HP: Proteinuria and hypertension. Kidney Int Suppl 47: S76–S80, 1994 [PubMed] [Google Scholar]
- 20. Hsu CY, Lin F, Vittinghoff E, Shlipak MG: Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol 14: 2902–2907, 2003 [DOI] [PubMed] [Google Scholar]
- 21. Brantsma AH, Bakker SJL, Hillege HL, de Zeeuw D, de Jong PE, Gansevoort RT, PREVEND Study Group: Cardiovascular and renal outcome in subjects with K/DOQI stage 1–3 chronic kidney disease: The importance of urinary albumin excretion. Nephrol Dial Transpl 23: 3851–3858, 2008 [DOI] [PubMed] [Google Scholar]
- 22. Iseki K, Kinjo K, Iseki C, Takishita S: Relationship between predicted creatinine clearance and proteinuria and the risk of developing ESRD in Okinawa, Japan. Am J Kidney Dis 44: 806–814, 2004 [PubMed] [Google Scholar]
- 23. Lea J, Greene T, Hebert L, Lipkowitz M, Massry S, Middleton J, Rostand SG, Miller E, Smith W, Bakris GL: The relationship between magnitude of proteinuria reduction and risk of end-stage renal disease—Results of the African American study of kidney disease and hypertension. Arch Intern Med 165: 947–953, 2005 [DOI] [PubMed] [Google Scholar]
- 24. Jolly SE, Burrows NR, Chen SC, Li SY, Jurkovitz CT, Narva AS, Norris KC, Shlipak MG: Racial and ethnic differences in albuminuria in individuals with estimated GFR greater than 60 mL/min/1.73 m(2): Results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 55: S15–S22, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hanevold CD, Pollock JS, Harshfield GA: Racial differences in microalbumin excretion in healthy adolescents. Hypertension 51: 334–338, 2008 [DOI] [PubMed] [Google Scholar]
- 26. Murtaugh MA, Jacobs DR, Jr., Yu X, Gross MD, Steffes M: Correlates of urinary albumin excretion in young adult blacks and whites: The Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol 158: 676–686, 2003 [DOI] [PubMed] [Google Scholar]
- 27. Goldschmid MG, Domin WS, Ziemer DC, Gallina DL, Phillips LS: Diabetes in urban African-Americans. II. High prevalence of microalbuminuria and nephropathy in African-Americans with diabetes. Diabetes Care 18: 955–961, 1995 [DOI] [PubMed] [Google Scholar]
- 28. Levey AS, Cattran D, Friedman A, Miller WG, Sedor J, Tuttle K, Kasiske B, Hostetter T: Proteinuria as a surrogate outcome in CKD: report of a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis 54: 205–226, 2009 [DOI] [PubMed] [Google Scholar]
- 29. Cirillo M, Senigalliesi L, Laurenzi M, Alfieri R, Stamler J, Stamler R, Panarelli W, De Santo NG: Microalbuminuria in nondiabetic adults—Relation of blood pressure, body mass index, plasma cholesterol levels, and smoking: The Gubbio Population Study. Arch Intern Med 158: 1933–1939, 1998 [DOI] [PubMed] [Google Scholar]
- 30. Klausen KP, Parving HH, Scharling H, Jensen JS: The association between metabolic syndrome, microalbuminuria and impaired renal function in the general population: Impact on cardiovascular disease and mortality. J Intern Med 262: 470–478, 2007 [DOI] [PubMed] [Google Scholar]
- 31. O'Seaghdha CM, Hwang SJ, Upadhyay A, Meigs JB, Fox CS: Predictors of incident albuminuria in the Framingham Offspring Cohort. Am J Kidney Dis 56: 852–860, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gerstein HC, Mann JFE, Pogue J, Dinneen SF, Halle JP, Hoogwerf B, Joyce C, Rashkow A, Young J, Zinman B, Yusuf S: Prevalence and determinants of microalbuminuria in high-risk diabetic and nondiabetic patients in the heart outcomes prevention evaluation study. Diabetes Care 23: B35–B39, 2000 [PubMed] [Google Scholar]
- 33. Afshinnia F, Wilt TJ, Duval S, Esmaeili A, Ibrahim HN: Weight loss and proteinuria: Systematic review of clinical trials and comparative cohorts. Nephrol Dial Transpl 25: 1173–1183, 2010 [DOI] [PubMed] [Google Scholar]
- 34. Palaniappan L, Carnethon M, Fortmann SP. Association between microalbuminuria and the metabolic syndrome: NHANES III. Am J Hypertens 16: 952–958, 2003 [DOI] [PubMed] [Google Scholar]
- 35. Orth SR, Hallan SI: Smoking: A risk factor for progression of chronic kidney disease and for cardiovascular morbidity and mortality in renal patients - Absence of evidence or evidence of absence? Clin J Am Soc Nephro 3: 226–236, 2008 [DOI] [PubMed] [Google Scholar]
- 36. Agarwal R: Vitamin D, proteinuria, diabetic nephropathy, and progression of CKD. Clin J Am Soc Nephrol 4: 1523–1528, 2009 [DOI] [PubMed] [Google Scholar]
- 37. Freedman BI, Kopp JB, Langefeld CD, Genovese G, Friedman DJ, Nelson GW, Winkler CA, Bowden DW, Pollak MR: The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol 21: 1422–1426, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ned RM, Yesupriya A, Imperatore G, Smelser DT, Moonesinghe R, Chang MH, Dowling NF: Inflammation gene variants and susceptibility to albuminuria in the U.S. population: Analysis in the Third National Health and Nutrition Examination Survey (NHANES III), 1991–1994. BMC Med Genet 11: 155, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bostrom MA, Freedman BI: The spectrum of MYH9-associated nephropathy. Clin J Am Soc Nephro 5: 1107–1113, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Peralta CA, Li YM, Wassel C, Choudhry S, Palmas W, Seldin MF, Risch N, Siscovick D, Arnett D, Psaty B, Shlipak MG: Differences in albuminuria between Hispanics and whites: An evaluation by genetic ancestry and country of origin The Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Genet 3: 240–247, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. White SL, McGeechan K, Jones M, Cass A, Chadban SJ, Polkinghorne KR, Perkovic V, Roderick PJ: Socioeconomic disadvantage and kidney disease in the United States, Australia, and Thailand. Am J Public Health 98: 1306–1313, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Martins D, Tareen N, Zadshir A, Pan DY, Vargas R, Nissenson A, Norris K: The association of poverty with the prevalence of albuminuria: Data from the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 47: 965–971, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sabanayagam C, Shankar A, Saw SM, Lim SC, Tai ES, Wong TY: Socioeconomic status and microalbuminuria in an Asian population. Nephrol Dial Transpl 24: 123–129, 2009 [DOI] [PubMed] [Google Scholar]
- 44. Painter RC, Roseboom TJ, van Montfrans GA, Bossuyt PMM, Krediet RT, Osmond C, Barker DJ, Bleker OP: Microalbuminuria in adults after prenatal exposure to the Dutch famine. J Am Soc Nephrol 16: 189–194, 2005 [DOI] [PubMed] [Google Scholar]
- 45. Yudkin JS, Martyn CN, Phillips DIW, Gale CR: Associations of micro-albuminuria with intra-uterine growth retardation. Nephron 89: 309–314, 2001 [DOI] [PubMed] [Google Scholar]
- 46. Shoham DA, Vupputuri S, Kaufman JS, Kshirsagar AV, Roux AVD, Coresh J, Heiss G: Kidney disease and the cumulative burden of life course socioeconomic conditions: The Atherosclerosis Risk in Communities (ARIC) Study. Soc Sci Med 67: 1311–1320, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hsu C-y, Iribarren C, McCulloch CE, Darbinian J, Go AS: Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med 169: 342–350, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hunsicker LG, Adler S, Caggiula A, England BK, Greene T, Kusek JW, Rogers NL, Teschan PE: Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int 51: 1908–1919, 1997 [DOI] [PubMed] [Google Scholar]
- 50. Ruggenenti P, Perticucci E, Cravedi P, Gambara V, Costantini M, Sharma SK, Perna A, Remuzzi G: Role of remission clinics in the longitudinal treatment of CKD. J Am Soc Nephrol 19: 1213–1224, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G: The Reasons for Geographic and Racial Differences in Stroke Study: Objectives and design. Neuroepidemiology 25: 135–143, 2005 [DOI] [PubMed] [Google Scholar]
- 52. Warnock DG, Muntner P, McCullough PA, Zhang XA, McClure LA, Zakai N, Cushman M, Newsome BB, Kewalramani R, Steffes MW, Howard G, McClellan WM: Kidney function, albuminuria, and all-cause mortality in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. Am J Kidney Dis 56: 861–871, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]