Abstract
Microsurgical hand reconstruction can be the first option to consider in some particular and complex clinical situations. An algorithm based on anatomical considerations and functional outcomes, may be useful for the plastic surgeon that deals with these challenging cases.
Keywords: Hand, soft tissue; Microsurgical reconstruction; Algorithm
Introduction
A free flap is a one-stage transfer of composite complex soft tissue units, tailoring of the flap to suit the reconstructive needs of the wound.
Microsurgical free tissue transfers expanded our options for more refinement in hand soft-tissue reconstruction, and have changed the standards for a successful outcome.
They can be used for hand reconstruction whenever local, regional or distant pedicled flaps are precluded, and which are often no satisfactory and lead to bulky flaps of tissue. Actually, microsurgical hand reconstruction can constitute the first option in particular clinical situations. Their main indications are first web space reconstruction, extensive dorsal hand defects, extensive dorsal hand defects with extensor tendon loss, and multi-digit distal coverage.
We present a review of 52 free flaps for upper limb, and an algorithm is proposed, for selection of the best microsurgical procedure in hand reconstruction.
Material and Methods
During 1995 to 2009, 52 free flaps were performed at our department for upper extremity reconstruction; 42 patients were males and nine females. Their average age was 28 (17–74 years old).
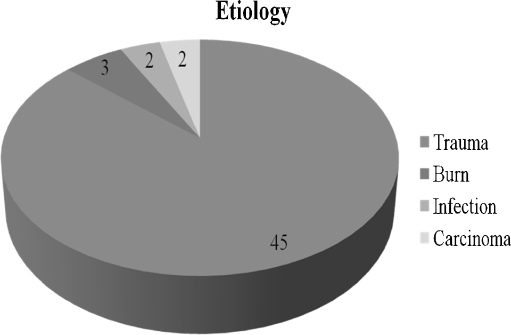
The etiology of the injuries and flaps applications are summarized as following (Fig. 1 and Table 1 respectively).
Fig. 1.
Etiology of injuries
Table 1.
Free flaps for upper limb reconstruction
| Free flap | No | Free flap | No |
|---|---|---|---|
| Second toe transfer | 12 | Gracilis myocutaneous flap | 3 |
| Temporalis fascia flap | 8 | Scapular flap | 3 |
| Contralateral radial forearm | 4 | Groin flap | 1 |
| Gracilis muscle flap | 4 | Tensor fascia lata flap | 1 |
| Toe pulp flap | 4 | Fíbula osteoseptocutaneous | 2 |
| Dorsalis pedis composite | 3 | Parascapular flap | 1 |
| Lateral arm | 3 | Greater omentum | 1 |
Our complications included three anastomosis revisions, and three total necrosis, two with the temporal fascia free flap, and one with gracilis myocutaneous free flap.
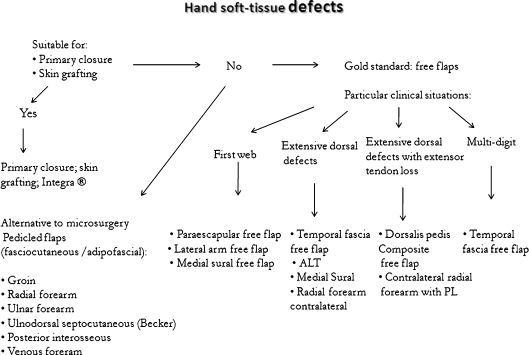
Based in anatomical considerations, functional outcomes, and the characteristics of the defect, we found out that a simple but useful algorithm can guide the plastic surgeon in dealing with complex situations. Thumb reconstruction with toe-to-hand free flaps, or isolated finger’s reconstruction were not considered.
Discussion
Free flaps are indicated in selected cases for coverage of the hand and fingers, but no algorithm was previously described to assist in resolving these cases.
Careful preoperative planning, delicate intraoperative management, and postoperative physiotherapy are the mainstays for success in functional recovery and aesthetic result.
Thin and well-vascularized flaps are favored for coverage of the hand and fingers. For hand surgeons, the lateral arm fasciocutaneous, and free vascularized temporoparietal fascial flaps covered with full-thickness skin grafts are currently the treatment of choice for most complex wounds, because are applicable in most situations [1–3].
However, others have concluded that muscle flaps with skin graft revealed better esthetic results than fasciocutaneous flaps [4].
An algorithm is proposed for selection of the best microsurgical procedure in hand reconstruction, based in our experience (Fig. 2).
Fig. 2.
Algorithm for hand microsurgical reconstruction
For first web reconstruction we prefer the paraescapular flap; it has a consistent vascular anatomy (cutaneous paraescapular branch of the circumflex scapular artery), easily accessible vascular pedicle, desirable vessel diameter. It also provides a moderate amount of subcutaneous tissue and hairless skin [5]; The lateral arm flap based on posterior branch of the radial collateral artery, may be used as an alternative, and also can be transferred in a tendofasciocutaneous pattern with a central strip of triceps tendon, but it’s usually more bulky and there is a tendency to hairiness in males [6].
For extensive dorsal hand defects we prefer the temporal fascia free flap [7, 8], which is a very thin, nonbulky, highly vascularized from its consistent and reliable pedicle (superficial temporal vessels). It restores a gliding apparatus for tendons denuded of paratendon, and can be transferred as osteofascial flap, incorporating the outer table of the frontoparietal calvarium. However, experienced plastic surgery departments also use frequently the ALT [9–11] (fasciocutaneous, septofasciocutaneous, chimeric) free flap, based on perforators form the descending branch of the lateral femoral circumflex artery. It is a very good option in thin patients with minimal morbidity, despite it often requires a posterior debulking procedure [12].
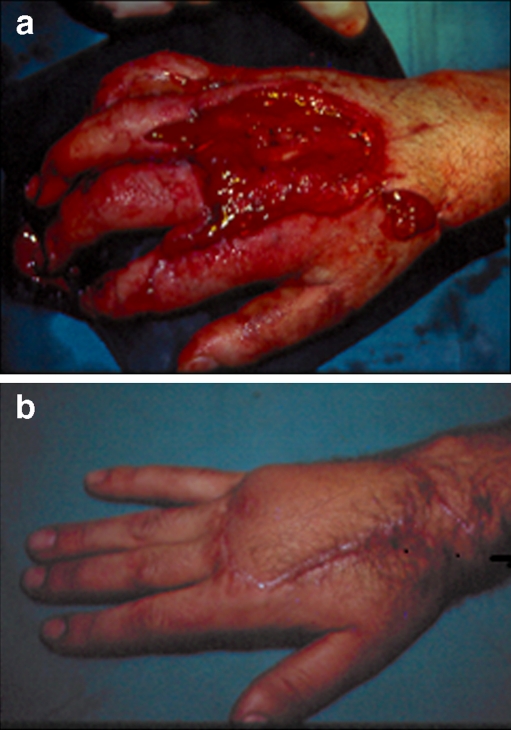
Traumatic hand injuries involving large-scale substance loss, which leave the tendinous, vascular or bone structures exposed, require the use also of a larger flap such as a contralateral antebrachial radial free flap which can incorporate palmaris longus tendon for extensor tendon reconstruction (Fig. 3a–d).
Fig. 3.
a Serious necrosis with extense substance loss in the hand and forearm b Dissection of a contralateral fasciocutaneous radial forearm flap c Outcome at 10 months
The free medial sural artery perforator flap transfer is other option, and can be appropriate for small- to medium-sized hand defect reconstruction. The donor site not only supplies a thin fasciocutaneous flap but also provides the option to harvest a segment of tendon or nerve graft through the same incision for composite tissue reconstruction in a single stage. However, its dissection is more difficult and appropriate perforators may not be present [13, 14].
In the presence of extensive dorsal hand defects with extensor tendon loss the dorsalis pedis composite flap free flap, based on dorsalis pedis—first dorsal metatarsal vascular axis, is the best option. It can be compounded as an osteocutaneous or tendinocutaneous flap with the second metatarsal or extensor tendons, and has a close resemblance to the hand (Fig. 4a,b). Donor-site sequelae is not inconspicuous, despite its low morbidity [15–17]. In our experience, one-stage soft tissue reconstruction with a free dorsalis pedis flap has been associated with minimal morbidity and good acceptance by patients. In one case there was delayed healing of donor area and the wound healed by secondary intention, but the donor site on the dorsum of the foot had no obvious scar contracture and without obviously influence on walking. The reconstructed fingers had a satisfactory appearance and performed such functions as grasping, and gripping.
Fig. 4.
Dorsalis pedis composite free flap a extensive dorsal defect with extensor tendon loss b Final result after 6 months
Considering multi-digit distal coverage, we think that the temporal fascia free flap is the best option for the same reasons we previously reported for coverage of severe dorsal defects. It can contour into bony concavities and provides a gliding apparatus for tendons, maintaining the definition of the underlying framework. Donor’s site alopecia is usually transient and resolves in months (Fig. 5a–c).
Fig. 5.
Temporal fascia free flap a Multi-digit defect; exposure of extensor tendons b Excellent functional outcome after 6 months c Transient alopecia
Complex multi-tissue reconstructions were achieved with better anatomic and functional quality, low morbidity, in one single procedure.
Free flaps are a first option to consider in specific clinical situations of hand surgery.
Acknowledgments
Financial Disclosure None of the authors has a financial interest in any products, devices, or drugs mentioned in this manuscript
References
- 1.Brown DM, Upton J, Khouri RK. Free flap coverage of the hand. Clin Plast Surg. 1997;24(1):57–62. [PubMed] [Google Scholar]
- 2.Chen HC, Buchman MT, Wei FC. Free flaps for soft tissue coverage in hands and fingers. Hand Clin. 1999;15(4):541–554. [PubMed] [Google Scholar]
- 3.Upton J, Havlik RJ, Khouri RK. Refinements in hand coverage with microvascular free flaps. Clin Plast Surg. 1992;19(4):841–857. [PubMed] [Google Scholar]
- 4.Wechselberger G, Schoeller T, Pülzl P, Piza-Katzer H. Free tissue transplantation for defect coverage of the dorsum of the hand: aesthetic and functional aspects. Handchir Mikrochir Plast Chir. 2003;35(4):245–250. doi: 10.1055/s-2003-42135. [DOI] [PubMed] [Google Scholar]
- 5.Nassif TM, Vidal L, Bovet JL, Baudet J. The paraescapular flap: a new cutaneous microsurgical free flap. Plast Reconstr Surg. 1982;69:591. doi: 10.1097/00006534-198204000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Sheker L, Lister G. The lateral arm fasciocutaneous flap. In: Strauch B, Vasconez LO, Hall-Findlay E, editors. Grabb’s Encyclopedia of flaps. Vol. 2. Boston: Little, Brown; 1990. p. 1127. [Google Scholar]
- 7.Biswas G, Dip NB, Ohani I, Chari PS. The sandwich temporoparietal free fascial flap for tendon gliding. Plast and Reconst Surg. 2001;108:1639. doi: 10.1097/00006534-200111000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Chowdary RP. Use of temporoparietal fascia free flap in digital reconstruction. Ann Plast Surg. 1989;23:543. doi: 10.1097/00000637-198912000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Wei F-C, Jain V, Celik N, et al. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002;109:2219. doi: 10.1097/00006534-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Celik N, Wei F-C, Lin C-H, et al. Technique and strategy in anterolateral thigh perforator flap surgery, based on analysis of 15 complete and partial failures in 439 cases. Plast Reconst Surg. 2002;109:2211. doi: 10.1097/00006534-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap based on the septocutaneous artery. Br J Plast Surg. 1984;37:149. doi: 10.1016/0007-1226(84)90002-X. [DOI] [PubMed] [Google Scholar]
- 12.Kuo Y-R, Jeng S-F, Kuo M-H, et al. Free anterolateral thigh flap for extremity reconstruction: clinical experience and functional assessment of the donor site. Plast Reconst Surg. 2001;107:1766. doi: 10.1097/00006534-200106000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Cavadas PC, Sanz-Giménez-Rico JR, Gutierrez-de la Cámara A. The medial sural artery perforator free flap. Plast Reconstr Surg. 2001;108(6):1609–1615. doi: 10.1097/00006534-200111000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Lin CH, Lin CH, Lin YT. The medial sural artery perforator flap: a versatile donor site for hand reconstruction. J Trauma. 2011;70(3):736–743. doi: 10.1097/TA.0b013e318203179e. [DOI] [PubMed] [Google Scholar]
- 15.Zuker RM, Manktelow RT. The dorsalis pedis free flap: technique of elevation, foot closure, and flap application. Plast Reconst Surg. 1986;77:93. doi: 10.1097/00006534-198601000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Samson MC, Morris SF, Tweed AEJ. Dorsalis pedis flap donor site: acceptable or not? Plast Reconstr Surg. 1998;102:1549. doi: 10.1097/00006534-199810000-00031. [DOI] [PubMed] [Google Scholar]
- 17.Ju J, Zhao Q, Liu Y. Repair of whole-hand destructive injury and hand degloving injury with transplant of pedis compound free flap. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23(10):1153–1156. [PubMed] [Google Scholar]