Abstract
OBJECTIVE
To prospectively measure women’s daily cigarette, alcohol and caffeine use, while attempting pregnancy in relation to intentions to change.
STUDY DESIGN
Cohort comprising 90 women enrolled upon discontinuing contraception and followed prospectively until pregnant. Women reported number of daily cigarettes, alcoholic and caffeinated beverages for 459 menstrual cycles while attempting pregnancy.
RESULTS
A significant mean reduction in daily caffeinated drinks (estimate (EST) = −0.52; 95% confidence interval (CI) = −0.70 to −0.33) was observed when compared to baseline usage. Intention to change was associated with a reduction in caffeinated drinks (EST = −0.32; 95% CI = −0.64 to 0.00), and with alcohol and cigarette usage from the first menstrual cycle (EST = −0.15; 95% CI = −0.28 to −0.02 and EST = −1.65; 95% CI = −3.12 to −0.19, respectively).
CONCLUSION
A reduction in daily caffeine intake while attempting pregnancy was observed, but not in alcohol or cigarette use, underscoring need for preconception guidance.
Keywords: alcohol, caffeine, cigarettes, cohort, preconception
INTRODUCTION
Healthy lifestyles during pregnancy are recognized to be positively associated with pregnancy outcomes for both mothers and offspring, and have become embedded in effective prenatal care guidance. Of late, discussion has arisen about the need for preconception guidance in light of growing recognition regarding the importance of environmental exposures including lifestyle during the preconception window for a spectrum of sensitive reproductive and developmental endpoints.1,2 Despite little prospective information on what women actually do while attempting to become pregnant possibly reflecting the limited number of prospective cohort studies conducted worldwide,3 support for preconception guidance continues to grow. With the possible exception of folate supplementation or care of diabetic women,4,5 there has been little systematic implementation into clinical practice.6,7 A recent Cochrane Review noted the absence of randomized trials to assess the effect of preconception advice on fertility outcomes.8
At the population level, the U.S. Centers for Disease Control and Prevention released preconception recommendations to increase awareness of healthy lifestyles and to cease risky behaviors (e.g., use of alcohol, caffeine and cigarettes).9 While some observational studies have shown that women adopt healthy behaviors during pregnancy,10–14 only a few have examined women’s behaviors while trying to become pregnant and these relied upon retrospective reporting by women after delivery despite the modest validity of such information.10,11,13–15 In response to these critical data gaps, we prospectively assessed women’s use of cigarettes, alcohol and caffeine during the preconception period, particularly in relation to their intentions to modify behavior given their interest in becoming pregnant. We focused on these specific lifestyle behaviors because of their purported role in increasing the time required for conception and other adverse perinatal outcomes.16–20
MATERIALS AND METHODS
Investigators targeted women who had participated in a cohort focusing on fish consumption and adverse pregnancy outcomes21–22 to identify those planning pregnancy, consistent with the intention to recruit women who would be trying to become pregnant. Eligibility criteria included ages 18–34 years and no self-reported history of fecundity impairments or infertility. Of the 244 eligible women, 113 (46%) agreed to participate in this prospective pregnancy study and discontinued contraception with the intention of becoming pregnant in the next six months. Fourteen (12%) women were excluded because they were found pregnant during enrollment.
A research nurse conducted a standardized interview in the women’s homes to ascertain socio-demographic information, reproductive and medical history and average usage of alcohol, cigarettes and caffeine during the past 12 months or prior to attempting pregnancy along with intentions to change each of these three behaviors while trying to become pregnant. We calculated body mass index (BMI, kg/m2) from self-reported height and weight. For baseline consumption, participants reported the daily average number of cigarettes smoked and daily average number of servings of caffeinated (coffee, tea and caffeinated soft drinks) drinks over the past year. Alcohol use was ascertained in a two-part question comprising how many occasions per month the participant drank on average in the past year, and how many alcoholic beverages (beer, wine, wine coolers, and liquor) per occasion. For consistency in scale, we converted these answers to the daily number of alcoholic drinks by multiplying the number of occasions per month by the number of drinks per occasion and dividing by 28, as the women were likely approximating a month by four weeks. To measure baseline intentions for changing (or not) each behavior, the nurse asked participants, “Have you changed (or do you plan to change) your (cigarettes/alcohol/caffeine) consumption (type of beverage, frequency or amount) in anticipation of becoming pregnant?” Participants were given the following response options: “yes, abstain now”, “yes, drink less now”, “plan to change but haven’t yet”, “no” or “never (smoked/drank).” In this analysis, we dichotomized intent by grouping the former three responses into “intend to change” and the latter two responses into “do not intend to change.” Not all abstainers, defined as such by baseline consumption or intention, refrained from consumption while attempting pregnancy, thereby necessitating their inclusion in the latter category.
Women completed daily diaries and recorded the number of cigarettes smoked and the number of alcoholic and caffeinated beverages consumed while trying to become pregnant. The women were followed prospectively until a positive home pregnancy test conducted on the expected date of menstruation or up to 12 menstrual cycles at risk for pregnancy. A few couples informed the study that they had paused trying for reasons such as unemployment or birth month preference. These non-at risk cycles were excluded irrespective of reason. Full human subject approval was awarded, and all participants gave informed consent prior to enrollment.
We defined menstrual cycles using bleeding reported in the daily diaries, with the first day of menses corresponding to the first day of the cycle. The first day of menses was designated by a day of bleeding or spotting followed within one day by at least two additional days of bleeding or spotting. We calculated average daily consumption for each cycle by summing the number of cigarettes smoked or the number of alcoholic or caffeinated beverages consumed as recorded for the cycle and then dividing by the number of diary entries in that cycle. The primary outcome, change in consumption relative to baseline, was calculated as the difference between the average daily consumption in a cycle and the daily baseline consumption. This continuous value was computed for each cycle, with up to 12 measurements (menstrual cycles) per woman for a total of 459 cycles. To assess the effects of reporter bias at baseline, change in consumption was also determined relative to average daily consumption observed in the first trying cycle. For the women who completed at least two cycles, this value was calculated for each cycle with a maximum of 11 measurements (menstrual cycles) per woman for a total of 369 cycles. Once a woman withdrew or conceived, the values of change in consumption for subsequent cycles were missing. For both measurements, a negative value of change indicated a decrease in consumption whereas a positive value denoted an increase; 95% confidence intervals (CIs) were calculated for assessing statistical significance.
We compared baseline characteristics by intention to change using Chi-square or Fisher’s exact test when cell counts were small. We modeled the mean change in consumption and the association between mean change and determinants including intent to change using linear regression with the generalized estimating equations method23,24 for correlated outcomes via PROC GENMOD in SAS software (version 9.1) (SASInstitute, Inc., Cary, North Carolina). We assumed that the correlation between outcomes from the same woman was a function of time between observations; thus, we chose an M-dependent or autoregressive working correlation structure, and we used robust standard errors for inference. Since the women did not record daily consumption following pregnancy, we conducted a sensitivity analysis to assess the effects of dropout bias. In this analysis, we used a last observation carried forward (LOCF) approach, replacing the missing values due to attrition with the last observed change in consumption and repeating the analysis.
RESULTS
The women were highly compliant with 91% submitting daily diaries, resulting in a final cohort of 90 women contributing 459 cycles for analysis. The cohort comprised mostly college educated (66%), employed (76%), married (98%), parous (70%) women self-defined as of white non-Hispanic ethnicity (100%). Seventy-three percent of the women conceived during the study while 14% withdrew after submitting some diary data and 12% did not conceive. At baseline, the majority of women reported consuming alcohol (84%) and caffeinated beverages (94%), though few smoked cigarettes (17%). Most women reported planning to change or refrain from these behaviors while attempting to become pregnant.
For the purpose of determining what risk factors were important to consider in later analyses, Table 1 demonstrates subgroups of women who were more likely to report intentions to change usage at baseline. Overall, few differences in distribution of intent between strata were observed save for overweight women who reported fewer intentions to change any behavior. Nulliparous women were more likely to report intentions to change alcohol and caffeine use than parous women. Intent to change also seemed to be dependent upon baseline consumption; medium to heavier users were more likely to report intending to change than women abstaining or engaging less frequently in a behavior. For cigarette consumption, a difference in education was observed with college educated women less likely to report an intention to change than women with lower educational attainments. This difference is possibly due to the large amount of abstainers who reported no intention to change.
TABLE 1.
Distribution of intention to change behavior for strata of baseline characteristics of study cohort
| Characteristic | Intend to change alcohol use
|
Intend to change cigarette use
|
Intend to change caffeine use
|
|||
|---|---|---|---|---|---|---|
| No % | Yes % | No % | Yes % | No % | Yes % | |
| All women | 31 | 69 | 82 | 18 | 42 | 58 |
|
| ||||||
| Age (years)
| ||||||
| 24–29 | 30 | 70 | 81 | 19 | 38 | 62 |
|
| ||||||
| 30–34 | 32 | 68 | 83 | 17 | 45 | 55 |
|
| ||||||
| BMI (kg/m2)
| ||||||
| Underweight (BMI < 18.5) | 25 | 75c | 50 | 50 | 25 | 75 |
|
| ||||||
| Normal (18.5 ≤ BMI < 25) | 24 | 76 | 84 | 16 | 40 | 60 |
|
| ||||||
| Overweight (BMI ≥ 25) | 45 | 55 | 84 | 16 | 48 | 52 |
|
| ||||||
| College graduate
| ||||||
| No | 23 | 77 | 68 | 32b | 45 | 55 |
|
| ||||||
| Yes | 36 | 64 | 90 | 10 | 41 | 59 |
|
| ||||||
| Employed
| ||||||
| No | 41 | 59 | 91 | 9 | 45 | 55 |
|
| ||||||
| Yes | 28 | 72 | 79 | 21 | 41 | 59 |
|
| ||||||
| Previous pregnancy
| ||||||
| No | 15 | 85c | 95 | 5c | 25 | 75c |
|
| ||||||
| Yes | 36 | 64 | 79 | 21 | 47 | 53 |
|
| ||||||
| Previous spontaneous pregnancy loss
| ||||||
| No | 30 | 70 | 88 | 12b | 42 | 58 |
|
| ||||||
| Yes | 33 | 67 | 62 | 38 | 43 | 57 |
|
| ||||||
| Previous live birth
| ||||||
| No | 11 | 89b | 81 | 19 | 19 | 81b |
|
| ||||||
| Yes | 40 | 60 | 83 | 17 | 52 | 48 |
|
| ||||||
| Baseline alcohol (# monthly drinks)
| ||||||
| 0 | 93 | 7a | 100 | 0 | 36 | 64a |
|
| ||||||
| <4 | 29 | 71 | 84 | 16 | 68 | 32 |
|
| ||||||
| 4–12 | 10 | 90 | 76 | 24 | 17 | 83 |
|
| ||||||
| 13+ | 19 | 81 | 75 | 25 | 44 | 56 |
|
| ||||||
| Baseline cigarettes (# daily)
| ||||||
| 0 | 33 | 67 | 97 | 3a | 45 | 55 |
|
| ||||||
| 1–9 | 22 | 78 | 0 | 100 | 22 | 78 |
|
| ||||||
| 10+ | 17 | 83 | 17 | 83 | 33 | 67 |
|
| ||||||
| Baseline caffeinated drinks (# daily)
| ||||||
| 0 | 20 | 80 | 80 | 20 | 100 | 0a |
|
| ||||||
| 1 | 40 | 60 | 93 | 7 | 60 | 40 |
|
| ||||||
| 2 | 36 | 64 | 82 | 18 | 36 | 64 |
|
| ||||||
| 3+ | 19 | 81 | 70 | 30 | 19 | 81 |
Baseline denotes upon enrollment into the cohort.
Tests performed using Chi-square or Fisher’s exact test when cell counts were small.
P < .001
P < .01
P < .15
Table 2 compares the prevalence of consumption at baseline, in the first cycle, and in the last cycle of participation in the study. In addition to a decrease in the prevalence of women drinking multiple daily cups of caffeine, 14 women who reported consuming caffeine daily on their baseline interview decreased their consumption to less than 1 daily cup, including four women who quit drinking caffeinated beverages entirely by the end of follow-up. Although 14 women ceased drinking alcohol entirely, the prevalence of women drinking large amounts of alcohol actually increased from baseline. The prevalence of binge (5+ drinks at one time) drinking decreased; however, it is important to note that half of the women reporting binge drinking in the last cycle did not report it in the 12 months before enrollment. Only one woman quit smoking during the study. Finally, not all women who reported abstaining from a behavior at baseline did so while attempting pregnancy. Specifically, three abstainers reported some caffeine consumption, four alcohol abstainers reported some consumption, and 13 non-smokers reported some cigarette smoking in their daily diaries.
TABLE 2.
Prevalence of lifestyle behaviors at baseline and during the first and last cycle of participation
| Lifestyle Behavior | Baseline (n=90) | First Cycle (n=90) | Last Cyclea (n=90) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Monthly alcoholic beverages (# drinks) | |||
| None | 14 (16) | 25 (28) | 26 (29) |
| <4 | 31 (34) | 13 (14) | 16 (18) |
| 4–12 | 29 (32) | 25 (28) | 31 (34) |
| 13+ | 16 (18) | 27 (30) | 17 (19) |
| Binge drinking (≥5 drinks on one occasion) | |||
| Never drank | 12 (13) | 25 (28) | 26 (29) |
| No | 50 (56) | 49 (54) | 54 (60) |
| Yes | 28 (31) | 16 (18) | 10 (11) |
| Daily cigarette use (# cigarettes) | |||
| None | 75 (83) | 72 (80) | 72 (80) |
| <0.5 | 0 (0) | 3 (3) | 3 (3) |
| 1–9 | 9 (10) | 10 (11) | 10 (11) |
| 10+ | 6 (7) | 5 (6) | 5 (6) |
| Daily caffeinated beverages (# drinks) | |||
| None | 5 (6) | 5 (6) | 6 (7) |
| <0.5 | 0 (0) | 15 (17) | 13 (14) |
| 1 | 30 (33) | 23 (26) | 30 (33) |
| 2 | 28 (31) | 26 (29) | 19 (21) |
| 3+ | 27 (30) | 21 (23) | 22 (24) |
NOTE: Alcohol use in the first and last cycle was standardized to a 28-day menstrual cycle for comparison purposes. Cigarette and caffeine use in the first and last cycle were averaged over days and rounded to the nearest integer.
For 21 women, the first cycle was also their last cycle.
Change measured relative to baseline
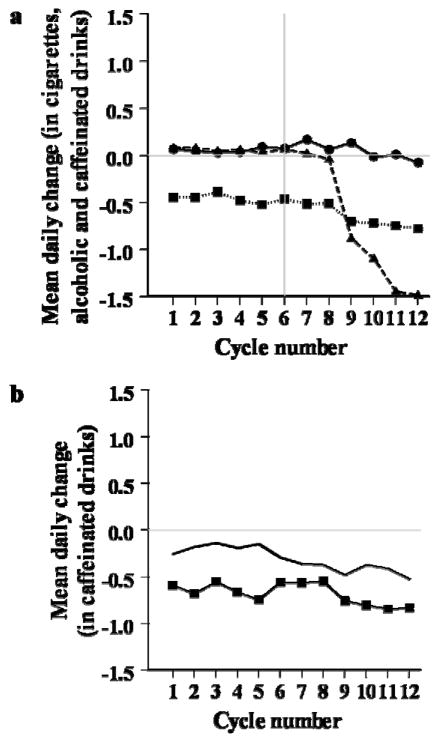
Although all women were planning pregnancy and over half reported intentions to change alcohol consumption, few women reported actual changes in alcohol use in comparison to baseline usage (Figure a). Similarly, little change in cigarette smoking was observed until the later cycles, when cigarette smoking was reduced by approximately 1.5 daily cigarettes in relation to baseline smoking. In contrast to alcohol and smoking, a significant reduction of approximately −0.52 (95% CI = −0.70 to −0.33) daily caffeinated drinks was observed throughout the study in comparison to baseline usage. This reduction in caffeine use magnified with time eventually reaching −0.8 daily drinks in the 12th cycle.
In unadjusted linear regression analysis using GEE method for correlated data, a significant difference in the average reduction of daily caffeinated drinks was observed for women who reported an intention to change in comparison to those who did not (Table 3). Figure b reflects that this relation was true for every cycle of the study. After adjusting for age group (<30 versus ≥30 years), previous live birth (yes/no) and BMI (continuous), the strength of the association between intent to change caffeine use and mean change in caffeine use lessened only slightly. In contrast, intent to change alcohol or cigarette usage was not associated with corresponding mean changes in either behavior. Further, the unadjusted models for change in consumption for each behavior did not identify an association between mean change and the following covariates: education, employment, vigorous exercise, age group and previous history of a live birth or spontaneous loss (data not shown). However, a small effect was found between increasing BMI and an increase in mean change in caffeine use from baseline.
TABLE 3.
Unadjusted and adjusted estimates for differences in women’s mean change in behaviors by intention to change at baseline (1=do intend to change/0=do not intend to change)
| Difference in mean change (# drinks/cigarettes) | Unadjusted EST (95% CI) | Adjusteda EST (95% CI) |
|---|---|---|
| Relative to baseline use | ||
| Daily behaviors (459 cycles) | ||
| Alcohol | 0.09 (−0.15, 0.34) | 0.12 (−0.06, 0.30) |
| Cigarettes | −0.61 (−2.34, 1.12) | −0.61 (−2.27, 1.05) |
| Caffeine | −0.40 (−0.72, −0.08) | −0.32 (−0.64, 0.00) |
| Daily behaviors – sensitivity analysis (1,080 cycles)b | ||
| Alcohol | 0.01 (−0.13, 0.15) | 0.02 (−0.10, 0.14) |
| Cigarettes | −0.58 (−2.21, 1.05) | −0.58 (−2.14, 0.99) |
| Caffeine | −0.47 (−0.77, −0.17) | −0.43 (−0.77, −0.09) |
| Relative to first cycle use | ||
| Daily behaviors (369 cycles) | ||
| Alcohol | −0.15 (−0.29, −0.01) | −0.15 (−0.28, −0.02) |
| Cigarettes | −1.75 (−3.64, 0.15) | −1.65 (−3.12, −0.19) |
| Caffeine | −0.24 (−0.68, 0.20) | −0.24 (−1.19, 0.71) |
| Daily behaviors – sensitivity analysis (990 cycles)b | ||
| Alcohol | −0.16 (−0.33, 0.00) | −0.17 (−0.31, −0.02) |
| Cigarettes | −1.61 (−3.16, −0.05) | −1.57 (−2.91, −0.24) |
| Caffeine | −0.09 (−0.33, 0.15) | −0.13 (−0.39, 0.13) |
EST, estimated regression coefficient; CI, carried forward. confidence interval; LOCF, last observation
Adjusted for age (<30 versus ≥30 years), previous live birth (yes/no) and BMI (continuous).
Sensitivity based on LOCF analysis.
Our sensitivity analysis revealed very little dropout bias, suggesting that attrition due to either conception or withdrawal from the study did not affect results (Table 3). Using the LOCF dataset comprising 12 cycles for each woman, a similar overall decrease was seen in caffeine use (estimate (EST) = −0.51; 95% CI = −0.68 to −0.35) along with a similar lack of substantial change in alcohol and cigarette use. Furthermore, the unadjusted and adjusted associations between intention to change and actual mean change in caffeine strengthened slightly.
Change measured relative to first cycle
With respect to change measured relative to first cycle, we found that women did not change their daily alcohol, cigarette or caffeine use, though a very small decline in cigarette use in the later cycles of the study was observed. As Table 3 reflects, women who expressed an intent to change alcohol use did tend to decrease usage from the first cycle more than women who did not express an intent to change in the unadjusted and adjusted models. Intent to change cigarette use also was associated with actual mean change in cigarette use in adjusted models; however, intent to change caffeine use was not associated with actual mean change in caffeine use from the first cycle. In agreement with the previous sensitivity analysis, the estimates found using the LOCF for replacement of values missing due to conception or withdrawal were very similar to those found in the dataset with no replacement.
COMMENT
In this prospective cohort study with longitudinal measurement of lifestyle behaviors, we did not observe change in women’s use of alcohol or cigarettes, and we observed only a moderate decrease in caffeinated beverages during the preconception window or when attempting to become pregnant. Moreover, adoption of healthier behaviors irrespective of intentions tended to occur after six months of trying or later, perhaps as women became concerned about not becoming pregnant. While women reporting an intention to change at baseline were more likely to do so than unintending women, we observed varying degrees of actual change by type of behavior. Analyses of the association between intention to change and actual change excluding women who abstained yielded results (data not shown) in agreement with those that did not exclude women who abstained. Unfortunately, we did not have information on relevant factors that affect intention such as attitude toward the behavior, subjective norms and perceived behavioral control.25–27
We observed a slight increase in alcohol use relative to baseline and observed that women who intended to change actually increased their alcohol consumption relative to women who did not intend to change by approximately two drinks per cycle. These findings may be explained by a tendency to underreport unhealthy behaviors at baseline, or that reporting is more subject to error given that alcohol use is more variable relative to smoking or caffeine usage. However, a very small decrease in alcohol use was observed relative to first cycle usage, and intention to change was associated with a decrease in actual change. This finding coupled with that for caffeine underscores the importance of comparing actual usage with varying references such as baseline or cycle one. Our results for change in cigarette use are likely biased toward the null, since only 17% of women reporting smoking at baseline. Our analysis did show some promising indication of a decrease in cigarette use in the later cycles of the study as the women failed to conceive. Lastly, our findings did not vary in relation to study outcome (data not shown).
We were able to identify only two other prospective cohort studies that assessed preconception lifestyle behaviors,15,20 one of which was in relation to compliance with preconception guidelines.15 Specially, the novel Southampton Women’s Survey reported that 74% of women becoming pregnant within three months of interview were nonsmokers and that the median alcohol consumption at interview was 4 units (8 g. of alcohol) per week, whereas 83% of our cohort were nonsmokers and drank on average one weekly drink. Combined, these studies suggest that women are engaging in behaviors with potential adverse consequences for reproduction while attempting pregnancy.
We acknowledge the potential limited generalizability of the findings, particularly given its reliance on a limited cohort size yielding 459 cycles for analysis. However, this sample is very similar in terms of race, education, marital status and cigarette use to other studies focusing on behavior change during pregnancy and related outcomes.11,12 We further recognize our inability to assess the type and timing of changes during pregnancy, given that funding was restricted to following women to a human chorionic pregnancy.
In summary, our findings suggest that women at risk for pregnancy report intentions to adopt healthier lifestyles while attempting pregnancy, but few actually do so and not until six or more months of unsuccessful trying. The high incidence of caffeine and alcohol consumption and continued use of cigarettes among smokers suggest that women do not recognize the preconception window as a sensitive one for successful reproduction. Cautious interpretation of these results is necessary due to the limited number of smokers. We await corroboration from other prospective studies of behavior change in the preconception window. Our findings support continual efforts to refine and implement preconception guidance. Clinicians have a unique opportunity to complete comprehensive evaluations with women about prior reproductive history and behaviors that may be amenable to intervention to promote healthy behaviors during the preconception window.28 Such intervention and guidance may carry through pregnancy and across the lifespan.
Figure 1. Mean change in daily consumption over time.
(a), Mean change in daily cigarettes, alcoholic and caffeinated drinks compared to baseline use. (b), Mean change in daily caffeinated drinks compared to baseline use stratified by intention to change.
a
 Alcohol
Alcohol
 Cigarettes
Cigarettes
 Caffeine
Caffeine
b
 Do not intend to change
Do not intend to change
 Intend to change
Intend to change
Acknowledgments
Financial Support
Funded in part by the Agency for Toxic Substances and Disease Registry (H751 ATH 298338); and the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Conflicts of Interest Disclosure Statement
None of the authors have a conflict of interest.
Presentation Information
Findings of this submission were presented at Preconception Care and Preconception Health, 1st European Congress 2010, ONE, in Brussels, Belgium on October 8, 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13:1532–9. doi: 10.1093/humrep/13.6.1532. [DOI] [PubMed] [Google Scholar]
- 2.Hassan MA, Killick SR. Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril. 2004;81:384–92. doi: 10.1016/j.fertnstert.2003.06.027. [DOI] [PubMed] [Google Scholar]
- 3.Buck GM, Lynch CD, Stanford JB, et al. Prospective pregnancy study designs for assessing reproductive developmental toxicants. Environ Health Perspect. 2004;112:79–86. doi: 10.1289/ehp.6262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blencowe H, Cousens S, Modell B, Lawn J. Folic acid to reduce neonatal mortality from neural tube disorders. Int J Epidemiol. 2010;39(Suppl 1):i110–21. doi: 10.1093/ije/dyq028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahmud M, Mazza D. Preconception care of women with diabetes: a review of current guideline recommendations. BMC Womens Health. 2010;10:5. doi: 10.1186/1472-6874-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heyes T, Long S, Mathers N. Preconception care: practice and beliefs of primary care workers. Fam Pract. 2004;21:22–7. doi: 10.1093/fampra/cmh106. [DOI] [PubMed] [Google Scholar]
- 7.Morgan MA, Hawks D, Zinberg S, Schulkin J. What obstetrician-gynecologists think of preconception care. Matern Child Health J. 2006;10:S59–65. doi: 10.1007/s10995-006-0086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson K, Norman RJ, Middleton P. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst Rev. 2010;4:CD008189. doi: 10.1002/14651858.CD008189.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care-United States. MMWR Recomm Rep. 2006;55(RR-6):1–23. [PubMed] [Google Scholar]
- 10.Prager K, Malin H, Spiegler D, Van Natta P, Placek PJ. Smoking and drinking behavior before and during pregnancy of married mothers of live-born infants and stillborn infants. Public Health Rep. 1984;99:117–27. [PMC free article] [PubMed] [Google Scholar]
- 11.Hellerstedt WL, Pirie PL, Lando HA, et al. Differences in preconceptional and prenatal behaviors in women with intended and unintended pregnancies. Am J Public Health. 1998;88:663–6. doi: 10.2105/ajph.88.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pirie PL, Lando H, Curry SJ, McBride CM, Grothaus LC. Tobacco, alcohol, and caffeine use and cessation in early pregnancy. Am J Prev Med. 2000;18:54–61. doi: 10.1016/s0749-3797(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 13.Tough S, Tofflemire K, Clarke M, Newburn-Cook C. Do women change their drinking behaviors while trying to conceive? An opportunity for preconception counseling. Clin Med Res. 2006;4:97–105. doi: 10.3121/cmr.4.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elsinga J, de Jong-Potjer LC, van der Pal-de Bruin KM, le Cessie S, Assendelft WJ, Buitendijk SE. The effect of preconception counselling on lifestyle and other behaviour before and during pregnancy. Womens Health Issues. 2008;18(6 Suppl):S117–25. doi: 10.1016/j.whi.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Inskip HM, Crozier SR, Godfrey KM, et al. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: general population cohort study. BMJ. 2009;338:b481. doi: 10.1136/bmj.b481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baird DD, Wilcox AJ. Cigarette smoking associated with delayed conception. JAMA. 1985;253:2979–83. [PubMed] [Google Scholar]
- 17.Zaadstra BM, Seidell JC, Van Noord PA, et al. Fat and female fecundity: prospective study of effect of body fat distribution on conception rates. BMJ. 1993;306:484–7. doi: 10.1136/bmj.306.6876.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jensen TK, Henriksen TB, Hjollund NH, et al. Caffeine intake and fecundability: a follow-up study among 430 Danish couples planning their first pregnancy. Reprod Toxicol. 1998a;12:289–95. doi: 10.1016/s0890-6238(98)00002-1. [DOI] [PubMed] [Google Scholar]
- 19.Jensen TK, Hjollund NH, Henriksen TB, et al. Does moderate alcohol consumption affect fertility? Follow up study among couples planning first pregnancy. BMJ. 1998b;317:505–10. doi: 10.1136/bmj.317.7157.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Louis GMB, Lum KJ, Sundaram R, et al. Stress reduces conception probabilities across the fertile window: evidence in support of relaxation. Fertil Steril. 2010 doi: 10.1016/j.fertnstert.2010.06.078. In Press, Corrected Proof. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vena JE, Buck GM, Kostyniak P, et al. The New York Angler Cohort Study: exposure characterization and reproductive and developmental health. Toxicol Ind Health. 1996;12:327–34. doi: 10.1177/074823379601200305. [DOI] [PubMed] [Google Scholar]
- 22.Buck Louis GM, Dmochowski J, Lynch C, Kostyniak P, McGuinness BM, Vena JE. Polychlorinated biphenyl serum concentrations, lifestyle and time-to-pregnancy. Hum Reprod. 2009;24:451–8. doi: 10.1093/humrep/den373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 24.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 25.Fishbein M, Ajzen I. Reading. Addison-Wesley; 1975. Belief, attitude, intention, and behavior: An introduction to theory and research. [Google Scholar]
- 26.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs: Prentice-Hall; 1980. [Google Scholar]
- 27.Fishbein M, Ajzen I. Predicting and changing behavior: The reasoned action approach. New York: Psychology Press; 2010. [Google Scholar]
- 28.Stubblefield PG, Coonrod DV, Reddy UM, et al. The clinical content of preconception care: reproductive history. Am J Obstet Gynecol. 2008;(suppl):S373–83. doi: 10.1016/j.ajog.2008.10.048. [DOI] [PubMed] [Google Scholar]