Abstract
After total knee arthroplasty (TKA) the technique of wound management is not standardised. In this prospective study the efficacy of autologous blood reinfusion from the wound was investigated. One hundred patients (100 TKAs) were enrolled in this sequential cohort study. In one-half of the operations, a reinfusion system with suction and in the other half one wound drain without suction were used. Blood loss, transfusion requirements, range of motion, Insall scores and the incidence of complications were studied. The use of a reinfusion system did not decrease the homologous transfusion requirements. The blood loss in the group with a suction drainage system was significantly higher. Our experiences since May 2002 with one drain without suction in 787 consecutive TKAs confirm all findings of the current study.
Résumé
Après une arthroplastie totale du genou le problème des pertes sanguines, n’est pas aujourd’hui un problème standardisé. Lors d’une étude prospective, l’efficacité de l’autotransfusion a été appréciée. Cent prothèses totales ont été enrôlées dans une cohorte. La moitié d’entre eux ont bénéficié d’une retransfusion des pertes sanguines du redon et pour l’autre moitié, le redon simple a été utilisé, sans récupération du sang post-opératoire. Les pertes de sang, la nécessité de transfusion, la mobilité, le score Insall et les complications ont été étudiés. L’utilisation d’une récupération avec retransfusion du sang post-opératoire ne diminue pas le nombre de transfusions homologues. Les pertes sanguines dans le groupe avec drainage simple sont plus importantes. Notre expérience depuis mai 2002 avec l’utilisation d’un drain sans aspiration dans 787 prothèses totales du genou consécutives confirment ses données.
Introduction
There is no generally accepted or standardised technique for postoperative wound management after total knee arthroplasty (TKA) [17]. Some surgeons use a reinfusion system of autologous blood [19, 23] and others use closed suction drainage [11] following elective knee arthroplasty. Theoretically, a wound drain should minimise postoperative haematoma and all of the complications with which it is associated [4]. However, wound drains may potentially introduce different complications including infection [3, 25]. The purpose of a re-transfusion system of autologous blood from the wound is to reduce the need for homologous blood transfusion. Re-transfusion of autologous blood as well as transfusion of homologous blood may influence the patient’s immune system [8]. The reported results of studies where postoperative wound drainage is not used, vary considerably. There are some studies showing a higher and others no higher complication rates compared with patient groups managed with closed suction drain systems.
The purpose of this study was to compare the method of re-transfusion of the collected autologous unwashed blood from the wound with a closed non-suction drainage system.
Materials and methods
Primary total knee replacements were performed in 100 patients. The following knee prostheses were used: the NexGen Mobile Bearing Knee (MBK), NexGen Legacy Posterior Stabilized (LPS), NexGen Legacy Posterior Stabilized Flex mobile (LPS-Flex mobile) and NexGen Legacy Constrained Condylar Knee (LCCK) (Zimmer Inc., Warsaw, IL, USA). All operations were done without tourniquets. A standard medial parapatellar exposure was used. A lateral approach [10] was applied for severe valgus deformities with a fixed lateral collateral ligament contracture. All operations were performed by experienced knee surgeons. Preoperatively and 3 months postoperatively the range of motion and the Insall knee score [9] were measured. The haemoglobin value was determined 1 day preoperatively, on the day of surgery, and 3 and 7 days postoperatively. A preoperative analysis of the blood coagulation parameters was performed if indicated, either co-morbidity or prescription drug usage. The indications for a blood transfusion were influenced by the clinical symptoms of anaemia (hypotension, tachycardia, vertigo, hyperhidrosis, nausea and vomiting), the haemoglobin value (haemoglobin <8.0 g/dl) and a history of cardiovascular disease. A low molecular weight heparin (Enoxaparin 40 mg; the corresponding approximate anti-Factor Xa activity of 4,000 IU) was used once a day for prophylaxis of venous thrombosis beginning the day before operation and continued for 6 weeks postoperatively.
Patient group A
From March to April 2002, 50 patients received a TKA using three Redon-drains [20] (Oriplast Inc., Neunkirchen-Saar, Germany) attached to low-pressure suction and a re-transfusion system of the collected autologous unwashed blood from the wound (Transolog, Heim Medizintecnik, Glattbeck, Germany). Two drains (Charrière 12) were placed intra-articularly and one drain (Charrière 10) subcutaneously. The wound was closed by suturing the capsule and the subcutaneous tissue, and a skin closure with staples was performed. The postoperative dressing consisted of the following layers: gauze, abdominal pads, surgical cotton and an elastic bandage. Postoperatively, the leg was positioned in full extension. Blood collected over the next 4 h was re-transfused to the patient. Then the drains were reattached to a low-pressure suction reservoir.
Patient group B
From May to July 2002, 50 patients received a TKA using one intra-articular Redon-drain (Charrière 12) without suction. The drain was not attached to a re-transfusion system. The wound closure procedure, the dressing and the postoperative management were the same as in group A. This wound drainage technique was used in our department from May 2002 to January 2006. Our experience over 45 months (787 TKAs) with this method is reported.
The drains were removed on the second day postoperatively in both study groups. A compressive bandage was applied for two additional days. Therapy with a continuous passive motion machine began after the removal of the drains. The patient was mobilised with two canes and full weight bearing on the operated limb on the third postoperative day. The skin staples were removed on the tenth postoperative day if wound healing was uncomplicated.
Results
Patient group A
The mean patient age was 70.9 years (54.6–85.2). The ratio of male:female was 13:37 (26:74%). The mean body mass index was 29.4 (17.1–44.1). Forty-nine patients had a diagnosis of primary osteoarthritis and 1 patient had avascular necrosis of the medial femoral condyle. Each patient received a NexGen MBK. Twenty-nine (58%) of the TKAs were performed on the right side and 21 (42%) on the left side. Eighty-four percent of the operations were performed by orthopaedic surgeons and 16% by senior residents under the supervision of an orthopaedic surgeon. The mean operating time was 79 min (39–134). The total mean postoperative blood loss via the drains was 1,424 ml (600–2,760). The mean re-transfused autologous blood volume collected from the wound after the first 4 h postoperatively was 835 ml (300–1,300). In this study group 25 patients (50%) received an additional blood transfusion (autologous or homologous). The mean transfused blood volume in these 25 patients was 2.16 units (1–4). The blood transfusions were given at a mean haemoglobin value of 8.9 g/dl (7.2–10.0). In 43 cases (86%) wound healing was uncomplicated. In seven cases (14%) a delay in wound healing (wound secretion longer than 7 days postoperatively) was found. A severe delay or complication in wound healing was not seen. The haemoglobin values preoperatively and at various days postoperatively are shown in Table 1. During rehabilitation in 14 patients (28%) a complication was reported as listed in Table 2. The range of motion preoperatively was 109° and 3 months postoperatively 99°. The maximal flexion contracture preoperatively was 25° and postoperatively 15°. The preoperative flexion range was 70°–140° and postoperative was 80°–130°. The mean preoperative Insall knee score was 108 (47–156) and 3 months postoperatively 155 (100–197).
Table 1.
Detailed haemoglobin values (g/dl) at the routine control 1 day preoperatively, at the surgery day, 3rd and 7th postoperative day (POD)
| Surgery | ||||
|---|---|---|---|---|
| preOP | Day | POD 3 | POD 7 | |
| Haemoglobin value (g/dl) group A | ||||
| Mean | 13.9 | 11.1 | 10.0 | 10.7 |
| Standard deviation | 1.38 | 1.37 | 1.16 | 1.36 |
| Maximum | 17.9 | 15.5 | 13.3 | 13.6 |
| Minimum | 10.1 | 8.4 | 7.7 | 7.2 |
| Haemoglobin value (g/dl) group B | ||||
| Mean | 14.2 | 11.3 | 10.0 | 10.5 |
| Standard deviation | 1.14 | 1.17 | 1.15 | 0.83 |
| Maximum | 16.8 | 14.5 | 12.8 | 12.8 |
| Minimum | 11.8 | 8.6 | 7.9 | 8.9 |
Table 2.
Reported postoperative complications in both study groups
| Complications | Number of patients | |
|---|---|---|
| Group A | Group B | |
| Haematoma | 8 | 8 |
| Swelling | 3 | 1 |
| Deep venous thrombosis | 2 | 1 |
| Intra-articular effusion | 2 | 1 |
| Superficial wound infection | 1 | – |
| Fissure of medial femoral condyle | – | 1 |
| Infection of femoral nerve pain catheter | – | 1 |
| Angina pectoris | 1 | – |
| Sub-acute cardiac infarction | – | 1 |
| Tachycardia | 1 | – |
| Atrial fibrillation | 1 | 1 |
| Pulmonary embolism | 1 | – |
| Pneumonia | – | 2 |
Patient group B
The mean age of the patients was 70.2 years (50.5–89.1). Fourteen patients (28%) were male and 36 patients (72%) were female. The mean body mass index was 29.9 (20.2–41.9). All patients had a diagnosis of primary osteoarthritis. In this patient group 40 NexGen MBK (80%), 7 NexGen LPS-Flex mobile and 3 NexGen LPS (6%) were used. Twenty-nine patients (58%) had the operation on the right side and 21 (42%) on the left side. Ninety-six percent of the operations were done by orthopaedic surgeons and the others by senior residents under supervision of an orthopaedic surgeon. The mean operating time was 79.8 min (42–157). The mean volume of the collected blood in the reservoir of the drain was 247 ml (40–1,000). No significant difference was found for postoperative blood loss between the different types of prosthesis [NexGen MBK: mean 255 ml (40–1,000); NexGen LPS and LPS-Flex mobile: mean 215 ml (50–500)]. In 18 patients (36%) a postoperative blood transfusion was required. The mean transfused blood volume in these 18 patients was 2.22 units (2–4). The mean haemoglobin value at the time of blood transfusion was 8.6 g/dl (7.1–9.9). In 48 patients (96%) the wound healing was uncomplicated. In two patients (4%) a delay of the wound healing was noted. Table 1 shows the pre- and postoperative haemoglobin values. The reported postoperative complications in 15 patients (30%) are listed in Table 2. Preoperatively, the mean range of motion was 105° and postoperatively 103°. The maximal flexion contracture preoperatively was 15° and postoperatively 30°. The patient with 30° flexion contracture developed this 4 months postoperatively. The mean preoperative flexion was 70°–140° and postoperative 80°–140°. The mean Insall knee score preoperatively was 102 (28–149) and 159 (77–192) 3 months postoperatively.
Discussion
Different studies [6, 7, 18, 19, 23, 24] have reported a decreased blood transfusion requirement using a postoperative autologous blood reinfusion system. Peter et al. [19] reported a blood transfusion requirement in the study group without an autologous blood reinfusion system in 67 of 93 patients (72%) which dropped to 19% using a reinfusion system. A transfusion rate of 72% seems to be high in comparison to the results of Parker et al. [17]. In a meta-analysis they found a rate of 40% in 447 patients managed with a drain without re-transfusion. On the contrary, other research groups [1, 12–14] reported no significant differences for the transfusion rate using a re-transfusion system.
Kim et al. [11] studied 69 patients (139 knees) undergoing a bilateral TKA. One side was managed with a closed suction drainage system and the other side without wound drainage. In the group without wound drainage, more wound healing complications were found. The postoperative range of motion showed no significant difference in the two groups. Martin et al. [14] reported a higher wound healing complication rate and no reduced transfusion rate in the group without wound drainage. Mengal et al. [15] found a higher blood loss and transfusion requirement when wounds were not drained. Other studies [2, 5, 16, 17, 21, 22] found no differences with respect to wound healing, range of motion and blood transfusion requirements with or without wound drainage.
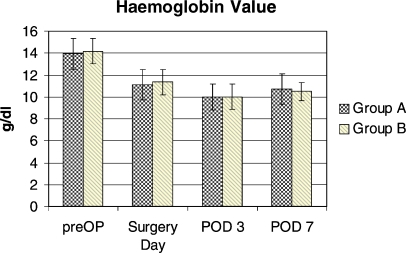
In our study, the reinfusion of the collected blood from the wound drains (mean 835 ml, standard deviation 225 ml) did not lead to a decreased homologous blood transfusion requirement (P>0.05). On the contrary, in patient group B the transfusion rate was lower. This can be attributed to the significantly higher blood loss (P<0.001) in group A using three drains with suction. The required transfusion units were not significantly different in the two groups (P>0.05). In both group A and group B, there were no incompatibility-related transfusion reactions seen. No differences can be attributed to the different methods of wound drainage or the complication rate (Table 2). The haemoglobin values on the seventh postoperative day showed an increasing trend (Fig. 1). The early indication for transfusion in relation to the mean haemoglobin values (group A 8.9 g/dl; group B 8.6 g/dl) can be attributed to the patient’s age and the co-morbidities.
Fig. 1.
Haemoglobin values (mean and standard deviation): preoperative (preOP), day of operation and the 3rd and 7th postoperative day (POD). Between both study groups no significant differences can be noted. An increasing haemoglobin value was found on the 7th postoperative day
No significant differences between both groups were found with respect to: patient age, gender, body mass index, surgeon and surgery time. In addition, the range of motion and Insall knee score showed no significant differences between the two groups.
The described technique of one intraarticular drain without suction has been applied in our department since May 2002. All the findings in this study using this drainage technique can be ratified by our experience over 45 months and 787 total knee replacements.
References
- 1.Adalberth G, Bystrom S, Kolstad K, Mallmin H, Milbrink J. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand. 1998;69(5):475–478. doi: 10.3109/17453679808997781. [DOI] [PubMed] [Google Scholar]
- 2.Beer KJ, Lombardi AV, Jr, Mallory TH, Vaughn BK. The efficacy of suction drains after routine total joint arthroplasty. J.Bone Joint Surg Am. 1991;73(4):584–587. [PubMed] [Google Scholar]
- 3.Casey BH. Bacterial spread in polyethylene tubing. A possible source of surgical wound contamination. Med J Aust. 1971;2(14):718–719. doi: 10.5694/j.1326-5377.1971.tb92504.x. [DOI] [PubMed] [Google Scholar]
- 4.Cobb JP. Why use drains? J Bone Joint Surg Br. 1990;72(6):993–995. doi: 10.1302/0301-620X.72B6.2246304. [DOI] [PubMed] [Google Scholar]
- 5.Crevoisier XM, Reber P, Noesberger B. Is suction drainage necessary after total joint arthroplasty? A prospective study. Arch Orthop Trauma Surg. 1998;117(3):121–124. doi: 10.1007/s004020050210. [DOI] [PubMed] [Google Scholar]
- 6.Dalen T, Skak S, Thorsen K, Fredin H. The efficacy and safety of blood reinfusion in avoiding homologous transfusion after total knee arthroplasty. Am J Knee Surg. 1996;9(3):117–120. [PubMed] [Google Scholar]
- 7.Grosvenor D, Goyal V, Goodman S. Efficacy of postoperative blood salvage following total hip arthroplasty in patients with and without deposited autologous units. J Bone Joint Surg Am. 2000;82-A(7):951–954. doi: 10.2106/00004623-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Handel M, Winkler J, Hornlein RF. Increased interleukin-6 in collected drainage blood after total knee arthroplasty: an association with febrile reactions during retransfusion. Acta Orthop Scand. (2001) ;72(3):270–272. doi: 10.1080/00016470152846600. [DOI] [PubMed] [Google Scholar]
- 9.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop. 1989;248(248):13–14. [PubMed] [Google Scholar]
- 10.Keblish PA. The lateral approach to the valgus knee. Surgical technique and analysis of 53 cases with over two-year follow-up evaluation. Clin Orthop. 1991;271(271):52–62. [PubMed] [Google Scholar]
- 11.Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop. 1998;347(347):188–193. [PubMed] [Google Scholar]
- 12.Mac HL, Reynolds MA, Treston-Aurand J, Henke JA. Comparison of autoreinfusion and standard drainage systems in total joint arthroplasty patients. Orthop Nurs. 1993;12(3):19–25. doi: 10.1097/00006416-199305000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Marks RM, Vaccaro AR, Balderston RA, et al. Postoperative blood salvage in total knee arthroplasty using the Solcotrans autotransfusion system. J Arthroplasty. 1995;10(4):433–437. doi: 10.1016/S0883-5403(05)80142-1. [DOI] [PubMed] [Google Scholar]
- 14.Martin A, Prenn M, Spiegel T, Sukopp C, Strempel A. Relevance of wound drainage in total knee arthroplasty-a prospective comparative study. Z Orthop Ihre Grenzgeb. 2004;142(1):46–50. doi: 10.1055/s-2004-817656. [DOI] [PubMed] [Google Scholar]
- 15.Mengal B, Aebi J, Rodriguez A, Lemaire R. A prospective randomized study of wound drainage versus non-drainage in primary total hip or knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(1):29–39. [PubMed] [Google Scholar]
- 16.Niskanen RO, Korkala OL, Haapala J, et al. Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: a prospective randomized study. J Arthroplasty. 2000;15(5):567–569. doi: 10.1054/arth.2000.6616. [DOI] [PubMed] [Google Scholar]
- 17.Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2004;86-A(6):1146–1152. doi: 10.2106/00004623-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Pertl D, Kaltenecker G. Minimizing allogeneic blood transfusion in knee prosthesis implantation. Unfallchirurg. 2001;104(9):808–812. doi: 10.1007/s001130170050. [DOI] [PubMed] [Google Scholar]
- 19.Peter VK, Radford M, Matthews MG. Re-transfusion of autologous blood from wound drains: the means for reducing transfusion requirements in total knee arthroplasty. Knee. 2001;8(4):321–323. doi: 10.1016/S0968-0160(01)00122-3. [DOI] [PubMed] [Google Scholar]
- 20.Redon H, Jost G, Torques Y. La fermature sous depression des paies étendues. Med Acad Chir. 1954;80:394–396. [PubMed] [Google Scholar]
- 21.Reilly TJ, Gradisar IA, Jr, Pakan W, Reilly M. The use of postoperative suction drainage in total knee arthroplasty. Clin Orthop. 1986;208(208):238–242. [PubMed] [Google Scholar]
- 22.Ritter MA, Keating EM, Faris PM. Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am. 1994;76(1):35–38. doi: 10.2106/00004623-199401000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Sinha A, Sinha M, Burgert S. Reinfusion of drained blood as an alternative to homologous blood transfusion after total knee replacement. Int Orthop. 2001;25(4):257–259. doi: 10.1007/s002640100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strumper D, Weber EWG, Gielen-Wijffels S, et al. Clinical efficacy of postoperative autologous transfusion of filtered shed blood in hip and knee arthroplasty. Transfusion. 2004;44(11):1567–1571. doi: 10.1111/j.1537-2995.2004.03233.x. [DOI] [PubMed] [Google Scholar]
- 25.Willett KM, Simmons CD, Bentley G. The effect of suction drains after total hip replacement. J Bone Joint Surg Br. 1988;70(4):607–610. doi: 10.1302/0301-620X.70B4.3403607. [DOI] [PubMed] [Google Scholar]