Abstract
The aim of this retrospective study was to report the preliminary results of femoral peri-prosthetic bone defect reconstruction with a synthetic bone substitute. Twenty-one revisions of the femoral component in 20 patients were evaluated. The mean age at operation was 65.7 years (range, 30 to 79 years). Preoperative femoral deficiencies were rated grade II in 7 cases and grade III in 14 cases according to the SOFCOT classification. None was rated grade IV. Femoral revision was indicated for loosening in 18 hips (including 8 septic cases), femoral osteolysis (1 hip), persistent pain (1 hip) and recurrent dislocation (1 hip). Once the loose prosthesis had been removed, calcium phosphate ceramic (CPC) granules (14 cases) or ceramic granules + cancellous allograft (5 cases) or autograft (2) were firmly impacted in the femoral canal. The stem was standard and always cemented using modern cementing technique. At a mean follow-up of 36 months (range, 14 to 76 months), 90% of the hips were rated good or very good according to the Merle d’Aubigné score. Two diaphyseal femoral fractures occurred and later united. Two hips required re-revision (aseptic loosening; septic recurrence). The absence of radiological osteolysis in 17 cases suggested direct bonding between ceramic granules and bone. Stem subsidence occurred in two cases and was limited (5 and 8 mm). Femoral bone reconstruction using impacted CPC or CPC in conjunction with bone graft in revision hip replacement commonly provided restoration of the bone stock in the short to mid-term. Further long-term studies will be necessary to support this conclusion.
Résumé
Le but de cette étude rétrospective est de rapporter les résultats préliminaires de la reconstruction des défects osseux fémoraux péri prothétiques avec des substituts osseux. Vingt et un révisions du composant fémoral chez 20 patients ont été évaluées de la sorte. L’âge moyen de l’intervention était de 65,7 ans (30 à 79). Les pertes de substances osseuses préopératoires ont été classées selon la classification de la SOFCOT : 7 cas de grade II, 14 cas de grade III, aucun cas de grade IV. L’indication opératoire était secondaire à un descellement dans 18 hanches (dont 8 descellements septiques), à une ostéolyse fémorale, à une douleur persistante et à une luxation récidivante. Après ablation du composant fémoral descellé des granules de calcium, phosphate, céramique, CPC ont été mises en place dans 14 cas, association de granules céramiques et d’os spongieux (allogreffe) dans 5 cas ou d’autogreffes dans deux cas. La céramique et l’os spongieux ont été impactés dans le fut fémoral. La pièce fémorale a toujours été une prothèse standard en utilisant les techniques de cimentation moderne. Après un suivi moyen de 36 mois (14 à 76 mois), 90% hanches ont été classées avec un résultat bon ou très bon selon le score de Postel Merle d’Aubigné. Deux fractures diaphysaires sont survenues et deux hanches ont nécessité une reprise (une pour descellement aseptique et une pour récidive de l’infection). Dans 17 cas nous n’avons constaté aucune ostéolyse radiologique. Une migration de la tige a été constatée dans deux cas mais de façon limitée (5 à 8 mm). La reconstruction osseuse en utilisant des granules CPC impactées ou des granules CPC mélangées à des greffons osseux dans les révisions de prothèses totales de hanche entraîne de façon habituelle une bonne restauration du stock osseux à court et moyen terme. Des études à long terme seront nécessaires pour confirmer cette conclusion.
Introduction
Management of bone stock loss remains one of the most challenging problems at the time of revision hip replacement. Femoral reconstruction provides a stable support for the stem and potentially allows for the recovery of bone stock. During the past decade, authors have reported successful results of femoral reconstruction with the morsellised impacted bone allograft technique [11, 17, 19, 24]. Limited aseptic failure rates, ranging from 0 to 6%, have been observed in the mid to long term [8, 20]. Recently, Exeter authors have reported a 90.5% global survival rate at 10 to 11 years with an evolution of the original technique [14]. However, the initial stability of the stem-graft composite is still far from optimal. Subsidence of the stem has been commonly reported [7, 9, 11, 15, 25, 27]. Among various variables, intrinsic allograft properties (particle morphology and size, composition, quality and preparation) have been shown to influence the initial stability of the composite [1, 6]. Synthetic ceramic bone grafts have been demonstrated to exhibit both much greater mechanical stability and reproducibility than pure allograft in experimental tests [12]. Therefore, ceramic graft may be an interesting alternative to allograft in femoral revision.
Several studies have reported the in vitro performance of calcium phosphate ceramics (CPC), described as hydroxyapatite (HA) and tricalcium phosphate (TCP) [2, 10, 21]. The CPC, regardless of the composition (HA or TCP), are biocompatible and physicochemically bound to the host bone [10]. Oonishi et al. [22] showed that bone stock restoration was regularly achieved in acetabular reconstruction with impacted HA granules during revision total hip replacement.
The aim of this study was to present the results of a retrospective and consecutive series of femoral reconstructions with impacted calcium phosphate ceramics. Special attention will be given to the radiological aspects of the reconstruction and to the eventual subsidence of the stem.
Materials and methods
Patients
From March 1996 to February 2001, 21 consecutive femoral reconstructions with impacted calcium phosphate ceramics during revision hip replacement were done in 20 patients at the Department of Orthopaedic Surgery of the Lariboisiere Hospital. There were 6 men and 14 women. The age of the patients at the time of revision ranged from 30 to 79 years (mean, 65.7±12.4 years; median, 71 years). Their mean weight was 70±15 kg (range, 50 to 100 kg; median, 70 kg). The right hip was treated in 11 patients, the left hip was treated in 8 patients, and a bilateral revision was done in 1 patient. All the revision procedures were performed by a senior author. Under the French regulations, informed consent from the patients was not required.
The original hip replacement was performed for osteoarthritis in 11 hips (10 patients), avascular necrosis of the femoral head in 3 hips (3 patients), trauma in 4 hips (4 patients), rheumatoid arthritis in 2 hips (2 patients), and osteomyelitis sequellae in 1 hip (1 patient). The previous hip replacement was total in 19 cases and unipolar in 2 cases. All femoral devices had been previously cemented.
Femoral revision was indicated for loosening in 18 hips (including 8 septic cases), femoral osteolysis (1 hip), persistent pain (1 hip) and recurrent posterior dislocation (1 hip). In 11 hips, the index operation was the first revision, in 5 the second, in 3 the third and in 2 the fifth, resulting in an average of 1.95 previous procedures per hip. The time elapsed between the most recent replacement and the revision averaged 6.1±5.8 years (range, 8 months to 22 years; median, 4.5 years).
Inclusion criteria in this study were failure of the previous hip replacement with contained femoral deficiencies on the preoperative radiographs. Specifically, bone stock loss was assessed as grade II in 7 hips and as grade III in 14 hips according to the SOFCOT Classification [29]. None was assessed as type IV.
Operative technique
A one-stage procedure was performed in all hips, including the septic cases. In these cases, bacteriological identification was obtained preoperatively. All procedures were performed in a clean-air environment with laminar flow. Surgical approaches included a posterolateral approach in 19 hips, trochanteric osteotomy in 1 hip and transfemoral approach in 1 hip. The loose prosthesis was removed. The cup was revised in 14 cases, including the 8 septic cases. In five cases, the cup was treated conservatively. In two cases, a primary implantation was performed. All cement, debris and fibrous membranes were cleared from the femoral canal with conventional instrumentation. The canal was then irrigated, sucked dry and occluded by a polyethylene plug (Ceraplug, Ceraver-Osteal, Roissy, France) placed distally to the most distal area of bone lysis. Defect reconstruction was achieved with porous granules of macroporous biphasic calcium phosphate (MBCP), consisting of 75% hydroxyapatite (HA) and 25% β-tricalcium phosphate (β-TCP) (Biosel, Depuy Bioland, France). HA granules were irregular in shape and size (2-3 mm). Macropores ranged from 200 to 500 μm in diameter, resulting in a 70% overall porosity of the material. Granules were employed as a pure graft in 14 hips. Granules were mixed with cancellous allograft prepared from fresh frozen femoral heads in five hips. In two hips, MBCP granules were employed as an autograft extender. The ratio of HA granules/bone graft was always at least 2:1 in weight. The indication for using either MBCP granules alone, or with allograft or with autograft was based upon the operator experience and bone graft availability at the time of surgery. The graft was mixed with blood obtained from peroperative suction in order to prepare a consistent paste. The femoral canal was filled with the graft, which was packed firmly down on top of the plug. A trial femoral component of the appropriate size was driven firmly into the impacted granules using a hammer in order to force the granules against the walls of the femoral canal. This procedure was repeated until endosteal defects were homogeneously covered by the graft. Once a contact between the collar of the trial stem and the calcar was obtained, trial reduction was performed. Bridging of the defects by the stem was assessed on peroperative radiographs. The trial stem was then withdrawn and the reconstructed canal sucked dry. Low viscosity antibiotic-loaded cement (Palacos-Genta) was introduced in an anterograde fashion through a tapered spout from a cement syringe, and the definitive femoral implant was inserted. The prostheses were manufactured by Ceraver (Ceraver-Osteal, Roissy, France). The stem, made of anodized Ti alloy (TiAl6V4), was smooth and collared, and was always cemented. Standard sizes and unlocked long-stem components (ranging from 170 to 190 mm) were used according to the preoperative planning. No special component was required in this series. Fourteen 32-mm alumina heads and seven 28-mm metallic heads were employed, resulting in 11 alumina-on-PE bearing couples, 7 Me-on-PE couples and 3 alumina-on-alumina couples. The mean duration of the operation was 212±79 min (range, 110 to 420 min; median, 180 min).
Mobilisation was started early and patients were allowed up within 2 or 3 days, and to walk with minimal weight-bearing on crutches for 6 to 12 weeks, followed by a graduated return to full weight bearing. A first-generation cephalosporin was routinely administered for 48 h after the operation except in the septic cases. In these cases, antibiotics were adapted to the bacteriological findings and were administered for a 6- to 12-week period. The length of hospital stay ranged from 9 to 60 days (mean, 21.5±14 days; median, 17 days).
Clinical and radiological evaluation
All patients were evaluated preoperatively and were followed up with clinical examinations and standard radiographs at regular intervals. All patients were reviewed by the same independent examiner (C.N.) at the last follow-up examination.
Hip function results were rated according to the grading system of Merle d’Aubigné [18]. This score classified the clinical results into six categories: excellent, 18 points; very good, 17 points; good, 16 points; fair, 15 points; poor, 14 points; bad, 13 points or less.
Serial AP and lateral radiographs of each hip were taken before and immediately after the operation, 6 weeks after discharge from the hospital, and 3 months, 6 months, 1 year and every 2 years postoperatively. Parameters investigating the femoral side included the evaluation of initial graft packing and cement filling using the six grades described by Gie et al. [11]. The later appearances of the graft were described according to the classification of Pierchon et al. [28] (Table 1). The presence or absence of radiolucent lines was assessed at the interfaces between the graft and the host and between the graft and the cement in the seven zones described by Gruen et al. [13]. Subsidence of the stem was analysed at the implant-cement interface and at the cement-bone interface on serial radiographs using the landmarks described by Walker et al. [30]. In view of the accuracy of manual measurement, a difference of at least 5 mm between two successive radiographs was required to establish subsidence. Loosening of the stem was defined as a continuous radiolucent line wider than 2 mm and/or a progressive migration.
Table 1.
Characteristics of the graft according to the radiological grading system of Pierchon et al. [28]
| Stage | Radiographic appearance of the graft |
|---|---|
| Stage 1 | Heterogeneous |
| Stage 2 | Homogeneous |
| Stage 3 | Condensation |
| Stage 4 | Trabecular remodelling |
| Stage 5 | Cortical repair |
On the acetabular side, the presence and progression of radiolucent lines were evaluated on AP radiographs of the pelvis and classified according to the zones described by De Lee and Charnley [5]. Heterotopic ossification, if present, was graded according to the classification of Brooker et al. [3].
Statistical analysis was done using parametric and non-parametric tests. A probability less than or equal to 0.05 was considered a significant difference.
Results
At the time of follow-up, two patients (two hips) had re-revision. One hip was revised for aseptic loosening, and one hip was revised for septic recurrence. No patients were lost to follow-up. The clinical and radiological status of the original 21 hips was known at the last follow-up evaluation, and 19 hips were available for analysis at a mean of 36±16.7 months (range, 14 to 76 months; median, 31 months). The clinical and radiological data of the patients at the time of the last follow-up evaluation are summarized in Table 2.
Table 2.
Radiographic and demographic data according to the patient and THR final status
| Case | Age (years) | Gender | Bone defect (SOFCOT) | Graft composition | Initial graft packing | FU (months) | Funct. score | Graft appearance (Pierchon et al.) | THR final status |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 60 | F | III | Allo + Biosel | Fair | 63.6 | 16 | 4 | Unrevised |
| 2 | 58 | M | III | Biosel | Exc. | 76 | 18 | 5 | Unrevised |
| 3 | 59 | M | III | Biosel | Exc. | 55 | 18 | 5 | Unrevised |
| 4 | 71 | F | III | Allo + Biosel | Exc. | 44 | 18 | 5 | Unrevised |
| 5 | 68 | M | III | Biosel | Good | 28 | 14 | 4 | Unrevised |
| 6 | 79 | F | III | Biosel | Exc. | 31 | 18 | 5 | Unrevised |
| 7 | 57 | M | II | Allo + Biosel | Exc. | 31 | 15 | 5 | Unrevised |
| 8 | 79 | F | III | Biosel | Exc. | 31 | 16 | 5 | Reop. |
| 9 | 50 | M | III | Allo + Biosel | Good | 67 | 14 | 5 | Unrevised |
| 10 | 30 | F | II | Biosel | Exc. | 39 | 15 | 5 | Unrevised |
| 11 | 71 | F | III | Biosel | Good | 27 | 15 | 5 | Unrevised |
| 12 | 71 | F | III | Allo + Biosel | Exc. | 26 | 17 | 5 | Unrevised |
| 13 | 50 | F | III | Biosel | Exc. | 26 | 15 | 5 | Unrevised |
| 14 | 73 | M | II | Biosel | Exc. | 14 | 16 | 5 | Unrevised |
| 15 | 73 | F | II | Biosel | Exc. | 31 | 18 | 5 | Unrevised |
| 16 | 73 | F | III | Biosel | Exc. | 30 | 18 | 5 | Unrevised |
| 17 | 74 | M | III | Biosel | Exc. | 18 | 17 | 5 | Unrevised |
| 18 | 66 | F | II | Auto + Biosel | Good | 36 | 16 | 5 | Unrevised |
| 19 | 78 | F | II | Biosel | Exc. | 37 | 17 | 5 | Unrevised |
| 20 | 64 | F | III | Biosel | Fair | 20 | – | – | Aseptic Loos. |
| 21 | 77 | F | II | Auto + Biosel | Exc. | 15 | – | – | Septic Recurr. |
FU= follow-up; Funct. score= functional score; Allo= allograft; Auto= autograft; Exc.= excellent; Reop.= reoperation; Loos.= loosening; Recurr.= recurrence
Complications
A diaphyseal femoral fracture occurred during surgery in two cases. The femurs were both classified preoperatively grade III according to the SOFCOT system [29]. Fractures were treated by reduction and wire, followed immediately by impaction grafting and cementing. Both of them subsequently united. At the last follow-up, functional scores were rated good and fair in these cases.
An isolated postoperative dislocation occurred in two cases. One patient required reoperation because of recurrent dislocation 5 months after revision. Acetabular expansion was performed without changing the components. At a 31-month follow-up, the functional score was rated good, and dislocation did not reoccurr.
Revisions
Revision of the femoral component was required in two patients (two hips) at a mean of 17.5 months (15 and 20 months). One hip exhibited a recurrent septic loosening at 15 months, revealed by an inflammatory syndrome and graft resorption on standard radiographs. This patient underwent a successful two-stage re-revision in another centre. One patient developed an aseptic loosening of the femoral component associated with a trochanteric non-union at 20 months postoperatively. Preoperative radiographs showed a complete femoral radiolucent line without migration of the stem. The synthetic graft was considered partially integrated at the time of re-revision. The patient underwent another femoral reconstruction with impacted MBCP granules. The trochanteric non-union was treated with plate and cerclage. At a 10-month follow-up, radiographs showed satisfying cortical repair and fibrous stabilisation of the greater trochanter.
Radiological results
One hip exhibited a non-progressive radiolucent line at the bone-cement interface, less than 2 mm in width, in Gruen zones 6, 7 and 8. Partial resorption of the calcar area was noted in one hip. None of the unrevised hips had a lytic lesion on either the femoral or the acetabular side.
Initial graft packing and cement filling were considered as excellent or as good in 19 cases, and as fair in two cases according to Gie and al. [11]. Cortical repair was achieved in 17 hips and were graded stage 5 according to Pierchon et al. [28] (Fig. 1). In this group, the mean follow-up was 36±16 months (range, 14 to 76 months; median, 31 months). Trabecular remodelling of the graft was observed in two cases (stage 4) at 28 and 63 months postoperatively. Initial graft packing was assessed as good and fair, respectively.
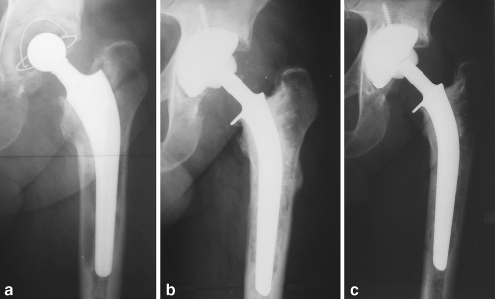
Fig. 1.
a First hip revision in a 58-year-old man. Preoperative radiographs showing aseptic loosening of the stem associated with femoral osteolysis. Bone defects were rated stage III. b Immediate postoperative anteroposterior view showing femoral reconstruction with pure synthetic graft. The graft-cement packing was considered complete and homogenous. c Radiographs taken 57 months postoperatively exhibit cortical repair and trabecular remodelling in the metaphyseal area. There is no evidence of stem subsidence and no radiolucent lines at the cement-bone interface. The functional score was rated excellent
Migration of the stem was recorded in two hips. Migration ranged from 5 to 8 mm. The latter was isolated and was not associated with any change of alignment. Maximal migration (8 mm) occurred in the hip, for which initial graft packing was considered fair (Fig. 2).
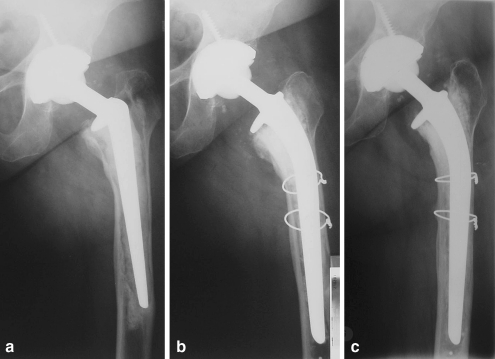
Fig. 2.
a Second hip revision in a 60-year-old woman. Preoperative radiographs show a loosening of the stem associated with a grade-III defect of the femoral shaft. b Immediate postoperative appearance after impaction grafting exhibiting a non-optimal graft packing. c An 8-mm stem subsidence occurred in the 1st postoperative months. The stem migration did not progress over 1 year (24-month view). The clinical result was rated good
At the latest follow-up examination, heterotopic ossification was observed in seven hips. Five hips were rated grade I, one hip grade II and one hip grade III according to the system of Brooker et al. [3].
Clinical evaluation
The mean Merle d’Aubigné functional hip score increased significantly from 10±2.2 (range, 5 to 14; median, 9) before surgery to 16±1.8 (range, 14 to 18; median, 16) at the last follow-up (Wilcoxon, P<0.05). Ten hips (53%) were rated as excellent or very good, seven hips (37%) as good and two hips (10%) as fair. Hip function was not restricted by pain in 16 patients (17 hips), whereas 2 patients (2 hips) had a walking capacity limited to 30 min. At the latest follow-up, the mean range of flexion was 112±16° (range, 70 to 130°) versus 91±20° (range, 20 to 140°) before operation (P<0.05).
Discussion
The use of calcium phosphate ceramics in revision replacement offers many potential advantages compared to auto- or allograft, including high purity, unlimited quantity, predictable osteointegration, time saving and the absence of immune reaction. Moreover, the use of a partially resorbable calcium phosphate ceramic encourages faster bone formation at the expense of ceramic crystals [10]. CPC have been demonstrated to bond to bone tissue under specific conditions, including close contact between the graft and host, and the achievement of primary stability. However, the main disadvantage is their poor mechanical resistance when used in bulk.
The biocompatibility and osseointegration of CPC have been well documented in experimental animal models [2, 10, 21]. CPCs appear to form a strong bond to the host bone tissue and to act as a scaffold for bone ingrowth. This property has been named osteoconduction. The use of CPC in clinical studies is more recent [4, 22]. Indications include spine arthrodesis [26], filling of cystic cavities, tibial osteotomies and treatment of periodontal osseous defects. A few studies have reported the use of bone substitutes in hip replacement revision [22], and, to the author’s knowledge, none have reported the use of CPC in femoral reconstruction in a clinical series.
Oonishi et al. [22] presented encouraging results of the impaction technique with HA granules applied to acetabular reconstruction during revision total hip replacement. The series included 40 hips, with a follow-up range from 4 to 10 years. Socket migration occurred in five hips with severe segmental and cavitary defects. The authors concluded that socket loosening and migration could be reduced when major peripheral segmental defects were stabilised by thick allografts, allowing firm packing of the HA granules. Furthermore, histological analysis on retrieved HA granules from acetabular bone defects suggested that bone ingrowth into spaces between HA could be expected [23].
In our series, a synthetic graft, used alone or in conjunction with allo- or autograft bone, was employed to reconstruct femoral peri-prosthetic defects. No specific revision prosthesis was developed, and standard titanium collared stems were used. Radiological and clinical outcomes did not differ with the nature of the graft, but no statistical analysis could be performed due to the limited number of patients in some groups. Cortical repair was achieved in the great majority. At the last examination, radiological analysis revealed no progressive radiolucent line at the bone-graft interface, suggesting direct bonding of the synthetic graft to the host. A virtual absence of osteolysis indicated good biological tolerance of the substitute. No accelerated wear of the PE was detected. One hip required further revision for aseptic loosening. This mechanical failure was related to poor graft packing, associated with the trochanteric non-union. These results compare favourably with the rates of aseptic loosening reported with the femoral reconstruction with impacted cancellous allograft, ranging from 0 to 10% [7, 11, 17, 19]. Extensive bone defect remains a high-risk situation for intra-operative fracture [19, 27]. In our series, two femoral fractures occurred during operation in patients with grade III defects. This risk appears to be independent of the technique, but rather related to the high-grade bone defect.
Subsidence and migration of components remain of concern in femoral reconstruction by impaction grafting despite the use of standardised techniques and dedicated instruments. Rates of subsidence vary from almost 0 to 90% in reports of femoral reconstruction with impacted morcellised allograft in the literature [7, 9, 11, 19]. Gie et al. [11] recorded subsidence of the stem within the cement mantle from 3 to 10 mm in 22 cases of 56 revisions. There was no negative correlation between subsidence and the clinical result. These authors concluded that some subsidence was acceptable, since there was no aseptic loosening. Eldridge et al. [7] reported an 11% incidence of subsidence over 10 mm in 79 revision hip replacements with impaction grafting of the femur. They concluded that varus positioning of the stem was correlated with failure. In a study of 34 revisions, Meding et al. [17] recorded a mean subsidence of 10.1 mm in 13 patients. In these series, no statistical association was found between subsidence and femoral bone defect grade, intraoperative fracture or the varus position of the femoral component. Pekkarinen et al. [27] reported a high incidence of stem migration (61 in 68 revisions; range from 2.7 to 5.6 mm) using cementing and non-cementing techniques with various implants. Many factors influence the subsidence of allograft within the femur, including graft preparation, the quality of the graft, particle morphology and size, impaction techniques, postoperative loading, the host’s immune response and host-graft interface. The reproducibility of the impaction technique employing pure bone allograft has been poor in experimental models [12]. An effort has been made to improve graft mechanical properties. In a radiostereometric analysis of 24 femoral revisions using improved grafting technique, Kärrholm et al. [15] reported a remarkably low rate of subsidence with a mean of 0.32 mm. In this work, the pure allograft had been washed in saline at 37°C prior to impaction. These authors concluded that low migration of the femoral stem was related to the graft preparation, leading to an increased hardness. These findings agree with experimental data reported by Dunlop et al. [6]. These authors have shown that a significant improvement of graft shear strength could be expected after the removal of fat and marrow fluids.
In our work, subsidence was identified in two hips (5 and 8 mm) according to the criteria mentioned. In these cases, subsidence was related to a technical deficiency, described as poor initial graft packing. However, migration was limited in size and did not progress over 1 year. Stability of the femoral component is said to depend on several factors, including optimal graft packing and mechanical resistance, good stem filling of the neo-canal combined with a thin cement mantle [16] and intrinsic properties of the collared stem. Nevertheless, the influence of synthetic grafting on mechanical resistance of the reconstruction still is unclear. A few experimental studies found that adding calcium phosphate ceramics to morsellised allograft bone chips significantly increased the resistance of the graft to subsidence [1, 12]. The HA volume mixes of at least 50% exhibited much more mechanical resistance than pure allograft at all loads. Therefore, it is postulated that ceramic granules of controllable properties used as extenders or as pure grafts should provide a more mechanically predictable graft material.
Conclusion
Femoral bone reconstruction with impacted MBCP in revision hip replacement provided encouraging results in the short to mid-term, which may be comparable to that of more conventional techniques using bone grafts. No adverse effect related to the use of a synthetic graft was noted. Provided that the technique is adequate and that the indications are restricted to cavitary defects of the femur, a bone stock restoration should be regularly expected. Further long-term studies are necessary to support this conclusion.
References
- 1.Blom AW, Grimm B, Cunningham J, Miles AW, Learmonth ID (2002) In vitro testing of Bonesave, a ceramic bone graft substitute for use in impaction grafting. In: Bioceramics 14, Trans Tech Publications, Zurich, pp 417–420
- 2.Braye F, Weber G, Irigaray JL, Frayssinet P. Osseointegration in cortical sheep bone of calcium phosphate implants evaluated by PIXE method and histology. J Biomed Mater Res. 1997;36:315–324. doi: 10.1002/(SICI)1097-4636(19970905)36:3<315::AID-JBM6>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg (Am) 1973;55:1629. [PubMed] [Google Scholar]
- 4.Daculsi G, Passuti N, Martin S, Deudon C, Legeros RZ, Raher S. Macroporous calcium phosphate ceramic for long bone surgery in humans and dogs. Clinical and histological study. J Biomed Mater Res. 1990;24:379–396. doi: 10.1002/jbm.820240309. [DOI] [PubMed] [Google Scholar]
- 5.Lee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;121:20–32. [PubMed] [Google Scholar]
- 6.Dunlop DG, Brewster NT, Madabhushi SPG, Usmani AS, Pankaj P, Howie CR. Techniques to improve the shear strength of impacted bone graft. J Bone Joint Surg (Am) 2003;85:639–646. doi: 10.2106/00004623-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;12:535–540. doi: 10.1016/S0883-5403(97)90176-5. [DOI] [PubMed] [Google Scholar]
- 8.Fetzer GB, Callaghan JJ, Templeton JE, Goetz DD, Sullivan PM, Johnston RC. Impaction allografting with cement for extensive femoral bone loss in revision hip surgery: a 4- to 8-year follow-up study. J Arthroplasty. 2001;16:195–202. doi: 10.1054/arth.2001.29136. [DOI] [PubMed] [Google Scholar]
- 9.Franzen H, Toksvig-Larsen S, Lidgren L, Onnerfalt R. Early migration of femoral components revised with impacted cancellous allografts and cement. A preliminary report of five patients. J Bone Joint Surg (Br) 1995;77:862–864. [PubMed] [Google Scholar]
- 10.Frayssinet P, Trouillet JL, Rouquet N, Azimus E, Autefage A. Osseointegration of macroporous calcium phosphate ceramics having a different chemical composition. Biomaterials. 1993;14:423–429. doi: 10.1016/0142-9612(93)90144-Q. [DOI] [PubMed] [Google Scholar]
- 11.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg (Br) 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 12.Grimm B, Blom AW, Miles AW, Turner IG (2002) In vitro endurance testing of bone graft materials for impaction grafting. In: Bioceramics 14, Trans Tech Publications, Zurich, pp 375–378
- 13.Gruen TA, Neice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components: A radiographic analysis of loosening. Clin Orthop. 1979;141:17–27. [PubMed] [Google Scholar]
- 14.Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg (Br) 2003;85:809–817. [PubMed] [Google Scholar]
- 15.Karrholm J, Hultmark P, Carlsson L, Malchau H. Subsidence of a non-polished stem in revisions of the hip using impaction allograft. Evaluation with radiostereometry and dual-energy X-ray absorptiometry. J Bone Joint Surg (Br) 1999;81:135–142. doi: 10.1302/0301-620X.81B1.8922. [DOI] [PubMed] [Google Scholar]
- 16.Langlais F, Kerboull M, Sedel L, Ling RS. The “French paradox”. J Bone Joint Surg (Br) 2003;85:17–20. doi: 10.1302/0301-620X.85B1.13948. [DOI] [PubMed] [Google Scholar]
- 17.Meding JB, Ritter MA, Keating EM, Faris PM. Impaction bone-grafting before insertion of a femoral stem with cement in revision total hip arthroplasty. A minimum two-year follow-up study. J Bone Joint Surg (Am) 1997;79:1834–1841. doi: 10.2106/00004623-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Merle d’Aubigné R. Cotation chiffrée de la fonction de la hanche. Rev Chir Orthop. 1970;56:481–486. [PubMed] [Google Scholar]
- 19.Migaud H, Jardin C, Fontaine C, Pierchon F, d’Herbomez O, Duquennoy A. Reconstruction fémorale par des allogreffes spongieuses impactées et protégées par un treillis métallique au cours des révisions de prothèse totale de hanche. 19 cas au recul moyen de 83 mois. Rev Chir Orthop. 1997;83:360–367. [PubMed] [Google Scholar]
- 20.Mikhail WE, Wretenberg PF, Weidenhielm LR, Mikhail MN. Complex cemented revision using polished stem and morselized allograft. Minimum 5-years follow-up. Arch Orthop Trauma Surg. 1999;119:288–291. doi: 10.1007/s004020050412. [DOI] [PubMed] [Google Scholar]
- 21.Oonishi H, Hench LL, Wilson J, Sugihara F, Tsuji E, Matsuura M, Kin S, Yamamoto T, Mizokawa S. Quantitative comparison of bone growth behavior in granules of Bioglass, A-W glass-ceramic, and hydroxyapatite. J Biomed Mater Res. 2000;51:37–46. doi: 10.1002/(SICI)1097-4636(200007)51:1<37::AID-JBM6>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 22.Oonishi H, Iwaki Y, Kin N, Kushitani S, Murata N, Wakitani S, Imoto K. Hydroxyapatite in revision of total hip replacements with massive acetabular defects: 4- to 10-year clinical results. J Bone Joint Surg (Br) 1997;79:87–92. doi: 10.1302/0301-620X.79B1.1290. [DOI] [PubMed] [Google Scholar]
- 23.Oonishi H, Kadoya Y, Iwaki H, Kin N. Hydroxyapatite granules interposed at bone-cement interface in total hip replacements: histological study of retrieved specimens. J Biomed Mater Res. 2000;53:174–180. doi: 10.1002/(SICI)1097-4636(2000)53:2<174::AID-JBM7>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 24.Ornstein E, Atroshi I, Franzen H, Johnsson R, Sandquist P, Sundberg M. Results of hip revision using the Exeter stem, impacted allograft bone, and cement. Clin Orthop. 2001;389:126–133. doi: 10.1097/00003086-200108000-00018. [DOI] [PubMed] [Google Scholar]
- 25.Ornstein E, Franzen H, Johnsson R, Sundberg M. Radiostereometric analysis in hip revision surgery–optimal time for index exafsmination: six patients revised with impacted allografts and cement followed weekly for 6 weeks. Acta Orthop Scand. 2000;71:360–364. doi: 10.1080/000164700317393349. [DOI] [PubMed] [Google Scholar]
- 26.Passuti N, Daculsi G, Rogez JM, Martin S, Bainvel JV. Macroporous calcium phosphate ceramic performance in human spine fusion. Clin Orthop. 1989;248:169–176. [PubMed] [Google Scholar]
- 27.Pekkarinen J, Alho A, Lepisto J, Ylikoski M, Ylinen P, Paavilainen T. Impaction bone grafting in revision hip surgery. A high incidence of complications. J Bone Joint Surg (Br) 2000;82:103–107. doi: 10.1302/0301-620X.82B1.9802. [DOI] [PubMed] [Google Scholar]
- 28.Pierchon F, Migaud H, Duquennoy A. Reconstitution du stock osseux fémoral dans les descellements de prothèse totale de hanche. Acta Orthop Belg. 1993;59:278–286. [PubMed] [Google Scholar]
- 29.Vives P, Lestang M, Paclot R, Cazeneuve JF. Le descellement aseptique : définitions, classification. Rev Chir Orthop. 1989;75:29–31. [Google Scholar]
- 30.Walker PS, Mai SF, Cobb AG, Bentley G, Hua J. Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems. J Bone Joint Surg (Br) 1995;77:705–714. [PubMed] [Google Scholar]