Abstract
Deformities combined with shortening in 34 lower limb segments of 28 patients were treated with an Ilizarov external fixator or a Taylor spatial frame at the same level as the osteotomy. We compared an acute correction group (A) with a gradual correction group (G) in patients undergoing deformity correction followed by lengthening. We retrospectively examined the amount of deformity correction, length gained, distraction index, maturation index, and external fixation index in both groups. The mean age of subjects was 12.9 years for A, 17.9 years for G. The mean deformity correction was 17.8° for A, 25.1° for G. Mean lengthening was 5.5 cm for A, 5.0 cm for G. Mean distraction index was 16.4 days/cm for A, 10.6 days/cm for G (P<0.05). Mean maturation index was 40.5 days/cm for A, 29.5 days/cm for G (P=0.081). Mean external fixation index was 58.6 days/cm for A, 42.5 days/cm for G (P<0.05). The distraction index and external fixation index differences between the two groups were statistically significant. Gradual correction may represent a better approach than acute correction with the use of external fixators to treat deformity combined with shortening.
Résumé
Des déformations associées au raccourcissement de 34 membres inférieurs chez 28 patients étaient traités, au niveau de l’ostéotomie, avec un fixateur externe d’Ilizarof ou un cadre de Taylor. Nous avons comparés un groupe avec une correction instantanée (A) et un autre avec une correction progressive (G) de la déformation suivie de l’allongement. Nous avons mesuré rétrospectivement l’importance de la correction, le gain de longueur, les index de distraction, de maturation et de fixation externe dans les deux groupes. L’âge moyen des patients était de 12,9 ans pour le groupe A et de 17,9 ans pour le groupe G.. La correction moyenne de déformation était de 17,8° pour le groupe A et de 25,1° pour le G.. L’allongement moyen était de 5,5 cm pour le A et de 5,0 cm pour le G.. L’index de distraction était de 16,4 jours/cm pour le A et de 10,6 jours/cm pour le G. L’index de maturation était de 40,5 jours/cm pour le A et de 29,5 jours/cm pour le G. L’index de fixation externe était de 58,6 jours/cm pour le A et de 42,5 jours /cm pour le G.. La différence entre les index de distraction et de fixation externe étaient significative. La correction progressive est préférable à la correction instantanée pour traiter des déformations combinées au raccourcissement.
Introduction
Deformities combined with shortening of the lower extremities are caused by congenital anomaly, trauma, tumour, or infection. Although these deformities, when severe, can sometimes lead to disabling impairment in activities of daily life, several studies have recently reported good results of treatment [1, 2, 6, 8, 9, 10, 12]. However, there has been no study comparing acute correction with gradual correction followed by lengthening until now.
In this study we retrospectively compared an acute correction group (A) with a gradual correction group (G). Patients in both groups underwent limb lengthening at the completion of their deformity corrections, using an external fixator at the same level as the osteotomy.
Materials and methods
Patients
Between 1993 and 2004, 53 lower limb segments in 47 patients were treated at our institution. Eight segments in eight patients treated with a double-level osteotomy were excluded from this study; 11 segments in 11 patients whose length gain was less than 3 cm were also excluded because published findings show that a short lengthening distance, especially less than 3 cm, causes prolongation of the external fixation index [7]. Thus, a total of 34 segments in 28 patients were retrospectively reviewed, including 20 segments in 15 male patients and 14 segments in 13 female patients. The acute correction group contained 15 segments, and the gradual correction group contained 19 segments. The mean age of the patients was 15.1 years, ranging from 5 years to 39 years (A 12.9 years, G 17.9 years; P=0.072). The affected site was the femur in 17 segments (A 11 segments, G six segments) and the tibia in 17 segments (A four segments, G 13 segments). The osteotomy was located at the diaphysis in 21 segments (A six segments, G 15 segments) and at the metaphysis in 13 segments (A nine segments, G four segments). The aetiologies of deformity combined with shortening were as follows: growth plate injury in 14 segments (A seven segments, G seven segments); congenital anomaly in 13 segments (A six segments, G seven segments); and tumour in seven segments (A two segments, G five segments). No significant differences between the two groups were observed with respect to aetiologies.
Operating technique
Ilizarov external fixators were used for 27 segments in 21 patients from 1993 to 2001, and Taylor spatial frames were used in seven segments in seven patients from 2002 to 2004. Preoperatively, the centre of rotation of angulation (CORA) was estimated from radiographs (frontal and lateral views), using the malalignment test proposed by Paley et al. [6]. When patients were treated with an Ilizarov external fixator, deformity correction was performed with Ilizarov hinges placed at the CORA, using an image intensifier. An osteotomy for deformity correction was performed as close to the CORA as possible, and then the deformity was corrected acutely during operation or gradually after operation. The lengthening procedure was started after a full completion of deformity correction in principle. In patients treated with a Taylor spatial frame, an osteotomy was performed as close to the CORA as possible, and deformity correction and lengthening were then gradually performed after the operation, in accordance with the program posted on the website. In the cases treated with an Ilizarov external fixator, the method of deformity correction (acute or gradual) was determined by an intraoperative check of the circulatory state of the skin after completion of the osteotomy. Paleness of the skin was considered to be an indication favouring gradual correction. Generally, deformities under 20° were corrected acutely, and deformities over 20° were corrected gradually. In all the cases of the Taylor spatial frame, deformity correction and lengthening were performed gradually after the operation, regardless of the amount of deformity.
Evaluations
The following were evaluated: length gained, amount of deformity correction, distraction index (DI), maturation index (MI), external fixation index (EFI), and complications. DI was obtained by dividing the total duration of distraction by the length gained. MI was obtained by dividing the total duration of maturation by the length gained. We obtained the EFI by dividing the total duration of external fixation by the length gained [11].
Means and standard deviations were calculated for all values. Statistical testing was performed with the unpaired t- test; the level of significant difference was defined as P<0.05.
Results
The mean length gained was 5.2 cm, ranging from 2.3 cm to 10.6 cm (A 5.5 cm, G 5.0 cm), and the mean angular correction was 21.9°, ranging from 5° to 53° (A 17.8°, G 25.1°). Mean DI was 13.2 days/cm (A 16.4 days/cm, G 10.6 days/cm ; P<0.05); mean MI was 34.3 days/cm (A 40.5 days/cm, G 29.5 days/cm; P=0.081), and mean average EFI was 49.5 days/cm (A 58.6 days/cm, G 42.5 days/cm; P<0.05). DI and EFI were significantly smaller in the gradual correction group than in the acute correction group (Table 1). Good alignment of lower legs was obtained after deformity correction in all patients. Seven patients (A four patients, G three patients) had signs of superficial wire tract infection, but none developed a deep extension of the infection. Premature consolidation occurred in one patient in the acute correction group, and this patient underwent re-osteotomy. During external fixation all patients had limitations of range of motion (ROM) in adjacent joints. However, except for three patients (A one patient, G two patients), all patients recovered full ROM in the affected joints after removal of the external fixator.
Table 1.
Result from each group
| Parameter | Acute | Gradual | P |
|---|---|---|---|
| Age (years) | 12.9±1.8 | 17.9±2.0 | 0.721 |
| Tibia | 4 | 13 | |
| Femur | 11 | 6 | |
| Lengthening (cm) | 5.5±0.6 | 5.0±0.5 | 0.542 |
| Correction angle (degrees) | 17.8±2.6 | 25.1±2.8 | 0.104 |
| DI (days/cm) | 16.4±1.9 | 10.6±0.7 | 0.004 |
| MI (days/cm) | 40.5±5.5 | 29.5±3.3 | 0.081 |
| EFI (days/cm) | 58.6±6.5 | 42.5±3.6 | 0.029 |
Case presentations
Patient 1 was treated by both acute and gradual corrections at different times, using Ilizarov external fixators in all instances. Patient 2 was treated with a Taylor spatial frame.
Case 1
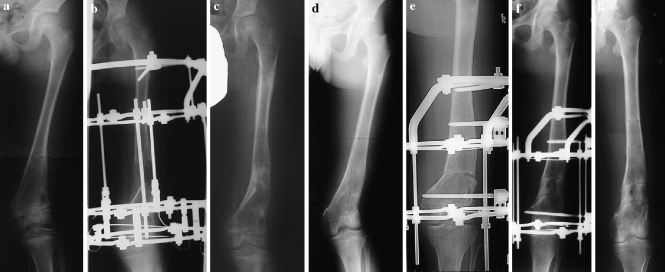
Case 1 was a male patient suffering from deformity combined with shortening caused by a distal growth plate injury of the left distal femur. He was treated with an Ilizarov external fixator at the age of 10 years (Fig. 1a). Gradual correction of his 19° deformity was performed after the operation; thereafter, a 4.0 cm lengthening was performed, resulting in good alignment and almost equal lengths of the bilateral lower limbs (Fig. 1b,c). DI was 14.0 days/cm, MI was 28.8 days/cm, and EFI was 43.8 days/cm. When he was aged 14 years, recurrent deformity with shortening was again treated with an Ilizarov external fixator (Fig. 1d). An acute correction of 22° was performed during the operation (Fig. 1e); thereafter, a 4.0 cm lengthening was performed (Fig. 1f), resulting in good alignment and almost equal lengths of the bilateral lower limbs (Fig. 1g). This time, DI was 19.3 days/cm, MI was 37.3 days/cm, and EFI was 59.8 days/cm.
Fig. 1.
Case 1. a Radiograph before the operation when the boy was aged 10 years. b Radiograph after deformity correction and lengthening. c Radiograph after removal of the Ilizarov external fixator. d Radiograph before the operation when the patient was aged 14 years. e Radiograph after acute correction during the operation. f Radiograph after lengthening. g Radiograph after removal of the Ilizarov external fixator
Case 2
Case 2 was a 5-year-old girl suffering from congenital deformity combined with shortening of her right tibia. She was treated with a Taylor spatial frame (Fig. 2a). The operation consisted of the application of a Taylor spatial frame and an osteotomy. After the operation, correction of a 5° deformity in the frontal plane and an 11° deformity in the sagittal plane were performed gradually and simultaneously with a 4.4 cm lengthening, in accordance with the program posted on the website. When it was discovered that her sagittal deformity was increasing during the lengthening procedure, her program was revised and the deformity correction with lengthening was then continued, resulting in good alignment and almost equal lengths of the bilateral lower limbs (Fig. 2b, 1,2,3). DI was 7.7 days/cm, MI was 13.0 days/cm, and EFI was 22.3 days/cm (Fig. 2c). Three years and 2 months after the operation, the patient has no leg length discrepancy and no problems with the activities of daily living (Fig. 2d).
Fig. 2.
Case 2. a Radiographs before the operation at when the girl was aged 5 years. b 1 Radiographs just after the operation. b 2 Radiographs during deformity correction and lengthening (observe the worsened deformity). b 3 Radiographs after completion of the revised deformity correction and lengthening program. c Radiographs after removal of the Taylor spatial frame. d Radiographs at the final follow up
Discussion
The results of this study comparing acute correction with gradual correction suggest that gradual correction of deformity combined with shortening should be expected to result in a smaller EFI.
Many reports have affirmed the usefulness of an external fixator in the treatment of deformity combined with shortening [1, 2, 6, 8, 9, 10, 12]. However, no clinical study has compared deformity correction and lengthening by acute versus gradual correction until now. In this study the gradual correction group had smaller DI and EFI. We suspect that these findings were the outcome of acute correction, causing more damage to surrounding soft tissues, producing a sudden gap between bone fragments and interfering with the sequence of callus formation. Consequently, lengthening speed had to be reduced because of poor callus formation, resulting in a larger DI.
Several factors influence bone formation, including age, affected site, and osteotomy site. Younger patients have faster bone formation. Bone formation is faster in the femur than in the tibia. Metaphyseal osteotomy yields faster bone formation than diaphyseal osteotomy [4].
Reviewing the patients in this study with respect to these three factors, one would expect the acute correction group to have faster bone formation than the gradual correction group, because the acute correction subjects tended to be younger and had higher percentages of affected femurs and metaphyseal osteotomies. However, the acute correction group actually had delayed bone formation, as evidenced by a significantly larger DI and EFI, compared with the gradual correction group. This result suggests that gradual correction might result in faster bone formation and shorter treatment time.
We also found that different people have different capabilities of bone formation. In this study, two patients underwent both acute and gradual corrections, followed by lengthening, at different times. Both patients had a smaller EFI when treated by gradual correction, an outcome suggesting that gradual correction was the superior approach.
Donnan et al. found that most patients with a maximum angulatory correction greater than 30° in any one plane, and many patients treated for deformities of the tibia, had unacceptable results, with poor callus formation and many complications following acute correction [1]. This observation is supported by our results, indicating that a patient with severe deformity or an affected tibia should be treated by gradual correction. On the other hand, Kamegaya et al. evaluated limb lengthening with immediate correction of the angulation deformity in 11 patients using a unilateral fixator. They observed no significant differences in healing indices between their series and a simple lengthening group [3]. Noonan et al. also examined the results of combined shortening with angulation treated by acute correction and gradual lengthening. They concluded that immediate correction and lengthening were suitable only in children and adolescents because of the poorer results observed in older patients [5]. However, these reports [3, 5] show only favourable results for children and adolescents and do not include cases requiring realignment of the lower limbs. Realignment of the mechanical axis is difficult with periarticular or multilevel deformity, using a unilateral external fixator [3, 5]. Moreover, the lengthening procedure sometimes worsens the deformity due to tension on soft tissues (Case 2), which is difficult to manage with a unilateral external fixator. Furthermore, the inability of unilateral external fixators to bear the full weight of a larger patient can lead to impairment of the activities of daily living.
Recently, a newly developed external fixator called the Taylor spatial frame has been finding increasingly wide usage. This external fixator uses the slow correction principles of the Ilizarov system combined with a six-axis deformity analysis incorporated within a computer program.
The Taylor spatial frame system treats deformities combined with shortening by correcting the angle deformities gradually and simultaneously with the lengthening procedure more easily than is possible with either the Ilizarov external fixator or a unilateral external fixator. Furthermore, the Taylor spatial frame can effectively manage deformities arising during the course of treatment due to the lengthening procedure itself. The Taylor spatial frame is proving to be a very effective tool for the treatment of deformity combined with shortening [8, 9].
Conclusions
Gradual correction may represent a better approach than acute correction in conjunction with the use of external fixators to treat deformity combined with shortening. A Taylor spatial frame is attracting increasing attention because of its ability to perform gradual correction of angle deformities and limb lengthening simultaneously.
References
- 1.Donnan LT, Saleh M, Rigby AS. Acute correction of lower limb deformity and simultaneous lengthening with a monolateral fixator. J Bone Joint Surg Br. 2003;85:254–260. doi: 10.1302/0301-620X.85B2.12645. [DOI] [PubMed] [Google Scholar]
- 2.Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005;29:125–129. doi: 10.1007/s00264-004-0611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamegaya M, Shinohara Y, Shinada Y. Limb lengthening and correction of angulation deformity: immediate correction by using a unilateral fixator. J Pediatr Orthop. 1996;16:477–479. doi: 10.1097/00004694-199607000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Noonan KJ, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80:793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Noonan KJ, Price CT, Sproul JT, Bright RW. Acute correction and distraction osteogenesis for the malaligned and shortened lower extremity. J Pediatr Orthop. 1998;18:178–186. doi: 10.1097/00004694-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 7.Sakurakichi K, Tsuchiya H, Uehara K, Kabata T, Tomita K. The relationship between distraction length and treatment indices during distraction osteogenesis. J Orthop Sci. 2002;7:298–303. doi: 10.1007/s007760200051. [DOI] [PubMed] [Google Scholar]
- 8.Sakurakichi K, Tsuchiya H, Kabata T, Yamashiro T, Watanabe K, Tomita K. Correction of juxtaarticular deformities in children using the Ilizarov apparatus. J Orthop Sci. 2005;10:360–366. doi: 10.1007/s00776-005-0908-6. [DOI] [PubMed] [Google Scholar]
- 9.Saldanha KA, Saleh M, Bell MJ, Fernandes JA. Limb lengthening and correction of deformity in the lower limbs of children with osteogenesis imperfecta. J Bone Joint Surg Br. 2004;86:259–265. doi: 10.1302/0301-620X.86B2.14393. [DOI] [PubMed] [Google Scholar]
- 10.Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop B. 2003;12:123–128. doi: 10.1097/00009957-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Tsuchiya H, Tomita K, Minematsu K, Mori Y, Asada N, Kitano S. Limb salvage using distraction osteogenesis. A classification of the technique. J Bone Joint Surg Br. 1997;79:403–411. doi: 10.1302/0301-620X.79B3.7198. [DOI] [PubMed] [Google Scholar]
- 12.Tsuchiya H, Uehara K, Tomita K. Deformity correction followed by lengthening with the Ilizarov method. Clin Orthop Relat Res. 2002;402:176–183. doi: 10.1097/00003086-200209000-00016. [DOI] [PubMed] [Google Scholar]